Abstract
There is evidence that prioritizing pets' welfare can impact the health and well-being of their owners, especially when pet owners have a strong bond with their pet. This carries public health implications, particularly in a global public health emergency such as COVID-19. The study objective was to understand pet owners' consideration of their pets' welfare when making personal healthcare decisions specific to COVID-19. A large sample (n = 1356) of adult pet owners in the U.S. completed an online survey in April and May of 2020, coinciding with the onset of social distancing measures to prevent the spread of COVID-19. Respondents were asked if they would delay or avoid testing or treatment for COVID-19 due to concern for their pets' welfare, and a follow-up question asked them to elaborate. Multinomial logistic regression models showed that attachment to pets and socioeconomic resources were important factors in pet owners' hypothetical decisions regarding testing and treatment for COVID-19. Qualitative analysis of responses to the follow-up question revealed explanations across three themes: (1) the need to find pet accommodation prior to seeking healthcare; (2) pet-related concerns; and, (3) human-related concerns. Pet owners often cited concern for their pets' welfare as a factor contributing to their decision making; participants' lack of a concrete plan for pet care was most commonly cited as the reason for their delay in seeking healthcare. Results from this study indicate that pet owners experience unique obstacles to accessing healthcare related to COVID-19, which has implications for future public health emergencies. Increased disease spread and prevalence of poor health outcomes could result if pet owners delay or avoid testing or treatment. Communities can benefit from a One Health/One Welfare approach to collaboration between human and animal health and service providers to reduce COVID-19 spread and secure the well-being of people and their pets.
Keywords: One Health, COVID-19, One Welfare, Pets, Companion animals, Healthcare
Highlights
-
•
Ten percent of pet owners indicated they might delay or avoid testing for COVID-19.
-
•
Over 10% of pet owners indicated they might delay or avoid treatment for COVID-19.
-
•
Pet attachment and socioeconomic resources predicted delay/avoidance of healthcare.
-
•
Need to secure accommodations for pets was the most cited reason for delaying care.
-
•
Inability to find care and wanting to remain with pets explained delay/avoidance.
1. Introduction
Over 60% of households in the U.S. has at least one pet (i.e., companion animal) [1], and this rate is expected to rise due to the popularity of pets during imposed social isolation from COVID-19 [2]. Though attitudes and practices toward pets vary, they are commonly thought of and treated as dependent family members in the U.S. [3]. Pet owners often form strong bonds to their pets and can experience distress upon separation [4]. Despite potential benefits [5], this bond, and the anticipated pain of separation or loss, pet-owner relationships can become a barrier to health and well-being. For example, pet-owning women experiencing intimate partner violence are sometimes reluctant to leave their abusive partner out of concern for their pet's welfare [6]. Pets can make finding and maintaining housing a challenge, particularly for those with few resources, and can lead to housing insecurity [7]. Some pet owners are unwilling to evacuate their homes during natural disasters when they are unable to bring their pet with them, risking their own health and safety, as well as that of first responders [8].
The COVID-19 pandemic has emerged as a global public health crisis, infecting tens of millions of people, and causing over one million deaths worldwide [9]. Though many COVID-19 cases were mild or asymptomatic, as of September 2020, a rate of 170.4 out of every 100,000 people infected required hospitalization [10]. At the time of writing, an infected individual is estimated to infect an average of 2–3 others [11]; therefore, it is pertinent to identify factors that contribute to delaying or forgoing testing and treatment in the interest of public health. Information is emerging and revealing barriers to care because the COVID-19 health crisis is unprecedented in recent history. Specifically, testing and treatment for COVID-19 can be cost-prohibitive, particularly for those without health insurance [12]—an issue that will likely increase as unemployment rates continue to rise. Even people who do not face cost as a barrier to healthcare often report that they find it challenging to be tested as testing shortages and delays continue into the summer [13].
Pets may impact healthcare decisions around COVID-19 for several reasons. First, there is evidence that pets can impact healthcare decision-making, generally: individuals may delay medical care due to concern for their pet, particularly when they are highly attached to their pet [14] or have low levels of social support [15]. Second, there is growing concern that pets may be susceptible to COVID-19 infection and could potentially transmit the disease to other non-human animals [16], thus complicating care plans for pets in the owners' absence. Third, as The New York Times documented, the high COVID-19 death toll in New York City left pets abandoned in apartments with no care when their owners did not return [17]. The article recounts the experience of a hospitalized person who spent days trying to arrange care for his dog—he found that facilities would not accept the dog due to concern for the spread of disease. This example poses a serious conflict for pet owners who face the prospect of arranging care for their pet(s) if they face hospitalization, and could contribute to delay of care and unnecessary risk of exposure to others.
1.1. One Health/One Welfare, pets, and COVID-19
The One Health initiative establishes that the health of people, animals, and the environment are interconnected and interdependent [18]. One Health researchers have called for consideration of the human-companion animal bond as an important factor in the interconnectedness of human and animal health [19,20]. This concept has been extended to the “One Welfare” platform, which asserts that the welfare of animals is tied to the well-being of humans [21]. We aim to understand the importance of human-animal relationships in the health and well-being of pet owners, specifically with respect to the current global public health crisis of COVID-19. Given the evidence that pets can impact their owners' healthcare decisions, we hypothesized that pets could be a potential barrier to both testing and treatment for COVID-19. Further, we hypothesized that the strength of the owner's bond to the pet, as well as the owner's access to resources would impact the likelihood of these decisions. Finally, we explored owners' explanations for potentially delaying or avoiding care to uncover opportunities for intervention.
2. Methods
2.1. Data
An anonymous, online survey was deployed to examine how relationships with pets impacted various aspects of life during the COVID-19 pandemic. The survey was distributed to interest groups and social media accounts related to companion animals, resulting in a nonprobability convenience sample (n = 2772). Respondents could participate if they agreed to the informed consent statement, were 18-years-old and over, and lived in the United States with at least one pet. Topics in the survey included questions about respondent's interactions with pets, and their household and sociodemographic characteristics. Respondents also completed two previously established scales assessing social support and pet attachment. Responses analyzed in this report were collected from April 6 – May 6, 2020.
2.2. Sample characteristics
We omitted observations that had incomplete data on any variable in the analyses, which resulted in a sample of 1356 adult pet owners residing in the United States. The majority of participants were women (89.2%) who ranged in age from 18 to 82 years (M = 39.0, SD = 13.6) and self-identified their race/ethnicity as non-Latinx White (87.8%). The sample's median annual family income range was $90,000–109,999 (M = $75,000-89,999); both mean and median level of education was a four-year college degree. Based on zip codes reported by respondents, the majority (93%) resided in metropolitan areas, defined by the USDA as an urbanized area of at least 50,000 inhabitants [22].
2.3. Measures
2.3.1. Delaying or avoiding testing and/or treatment for COVID-19
Two questions addressed intent to delay or avoid testing and treatment for COVID-19. Respondents were asked: “If you thought you had COVID-19 would you delay or avoid testing because you were worried about your pet's welfare?” and, “If you thought you had COVID-19 would you delay or avoid treatment because you were worried about your pet's welfare?” Response options for both questions were “Yes,” “Maybe,” “No,” and “I don't know.” After performing preliminary multinomial logistic regression analyses, a Wald test for combining alternatives determined that, in all models, the categories of “Maybe” and “I don't know” were not statistically different, and substantive interpretation did not differ [23]; therefore, the two categories were combined and renamed “Uncertain.”
2.3.2. Factors related to healthcare decision-making
If the respondents answered “Yes” or “Maybe” to either of the aforementioned questions regarding testing and treatment, they were filtered to an open response prompt: “Please explain more about delaying or avoiding testing or treatment for COVID-19 because you were worried about your pet.”
2.3.3. Pet attachment
Respondents completed the Lexington Attachment to Pets Scale [24], a 23-item measure designed to assess individuals' emotional attachment to their companion animal. Respondents indicated their level of agreement (on a Likert scale) with statements such as “My pet makes me feel happy.” The summated scale ranged from low to high attachment with scores of 32 to 92 (α = 0.90).
2.3.4. Number of people in household
Respondents gave a numerical response to the following question to determine population of their household: “How many people do you live with currently, not including yourself?”
2.3.5. Relationship status
Categories for relationship status were reconstructed to a binary variable: (1) “Married or permanently partnered/cohabiting” and (0) “Not married,” which included statuses of “single,” “widowed,” “divorced,” and “separated.” Conceptually, those who were married or partnered could likely depend upon a resident partner for help.
2.3.6. Caregiver to child(ren)
Status of caregiver to a child or children was determined by respondents' selection of “Yes, a child or children” to the question “Are you the primary caregiver to anyone?”
2.3.7. Worry about income loss
Given the widespread job loss across socioeconomic statuses, we asked respondents “Are you worried about losing income due to the COVID-19 situation?” Response options were “Yes”; “Somewhat”; or “No”.
2.3.8. Social support
Respondents completed the Multidimensional Scale of Perceived Social Support [25] to assess their subjective understanding of available supports from their social network. The scale consisted of a series of 12 Likert questions indicating their level of agreement with statements such as “There is a special person who is around when I am in need.” The summated scale ranged from low to high social support with scores ranging 12 to 60 (α = 0.94).
2.4. Analytic procedures
We estimated a series of multinomial logistic regression models using Stata 15.1 [26] to predict likelihood of delaying or avoiding testing and treatment for COVID-19 due to concern for companion animal welfare using closed-ended survey responses. Next, to reveal factors contributing to respondents' anticipated testing and treatment decision-making, two authors coded open-responses (n = 150) using a grounded theory approach [27]. A third coder with expertise in human-animal interaction helped reach consensus for coder disagreement.
3. Results & discussion
As shown in Table 1, nearly one-tenth (n = 122) of the sample indicated that they were either uncertain (7.2%) or would indeed (1.8%) delay or avoid testing for COVID-19 due to concern for their pet's welfare; over one-tenth (n = 168) of the sample indicated that they were either uncertain (10.2%) or would (2.1%) delay or avoid treatment for COVID-19 due to concern for their pet's welfare. See Table 1for descriptive information for all independent variables included in quantitative analyses.
Table 1.
Descriptive Statistics for all Variables (n = 1356).
| Variable | % (n) or M | Range |
|---|---|---|
| Delay/avoid testing | ||
| Yes | 1.8% (24) | |
| Uncertain | 7.2% (98) | |
| No | 91.0% (1234) | |
| Delay/avoid treatment | ||
| Yes | 2.1% (29) | |
| Uncertain | 10.3% (139) | |
| No | 87.6% (1188) | |
| Pet Attachment Scale | 80.7 | 32–92 |
| No. of People R Lives With | 1.4 | 0–7 |
| Married/Partnered | 64.8% (878) | |
| Has child(ren) | 17.3% (235) | |
| Worried about income loss | ||
| Yes | 37.5% (509) | |
| Somewhat | 31.1% (422) | |
| No | 31.3% (425) | |
| Social support scale | 49.0 | 12–60 |
Notes: Values shown in middle column are group relative frequencies or sample means.
3.1. Predicting likelihood of delaying or avoiding testing and treatment
Pet attachment was a significant predictor for intentions to delay or avoid both testing and treatment for COVID-19 in all models: likelihood of a respondent indicating they would delay or avoiding testing or treatment (“yes” response: RRRTest = 1.12, p < .01; RRRTreat = 1.07, p < .001), or that they were uncertain about what they would do (RRRTest = 1.06, p < .001; RRRTreat = 1.06, p < .001) increased slightly for each one-unit increase in the 60-point pet attachment scale, compared to a “no” response. This showed that highly attached pet owners were more likely to put their own health at risk to avoid separation from their pet than those with weaker attachment. As number of people in the household increased, likelihood of delaying or avoiding both testing and treatment decreased by about 50% (RRRTest = 0.45; RRRTreat = 0.49, p < .05). Number of people in the household also decreased the likelihood of “uncertain” responses for treatment (RRR = 0.77, p < .05), but not testing. Notably, likelihood of delaying or avoiding treatment increased substantially for those who stated that they were concerned about income loss, indicating that concern about future financial well-being due to the economic fallout of the pandemic was an important factor (RRR = 6.55, p < .01). Respondents with greater social support scores were less likely to delay or avoid testing (RRR = 0.96, p < .05) and treatment (RRR = 0.96, p < .01), highlighting the significance of one's social network. See Table 2.
Table 2.
Summary of Multinomial Logistic Regression Analysis for Variables Predicting Likelihood of Delaying or Avoiding Testing/Treatment for Covid-19 due to Concern for Pet's Welfare (base outcome = “No” response).
| Testing |
Treatment |
|||
|---|---|---|---|---|
| Predictor | Yes | Uncertain | Yes | Uncertain |
| Pet attachment | 1.12⁎⁎ | 1.06⁎⁎⁎ | 1.07⁎ | 1.06⁎⁎⁎ |
| No. of people in household | 0.45⁎ | 0.89 | 0.49⁎ | 0.77⁎ |
| Married/partnered | 0.44 | 0.72 | 0.48 | 0.76 |
| Has child | 1.13 | 0.48 | 0.66 | 0.48 |
| Worried about income loss (ref = no) | ||||
| Yes | 1.90 | 1.70⁎ | 6.55⁎⁎ | 1.31 |
| Somewhat | 0.43 | 1.24 | 2.21 | 1.33 |
| Social support | 0.96⁎ | 0.99 | 0.96⁎⁎ | 0.98⁎⁎ |
| Constants | 0.00002⁎⁎ | 0.001⁎⁎⁎ | 0.0008⁎ | 0.003⁎⁎⁎ |
| LR X2 (df) | 84.15 (14)⁎⁎⁎ | 117.91 (14)⁎⁎⁎ | ||
| N | 1356 | 1356 | ||
Notes: Values shown in cells are relative risk ratios (RRR).
p < .05.
p < .01.
p < .001.
3.2. Factors contributing to delaying or avoiding testing or treatment
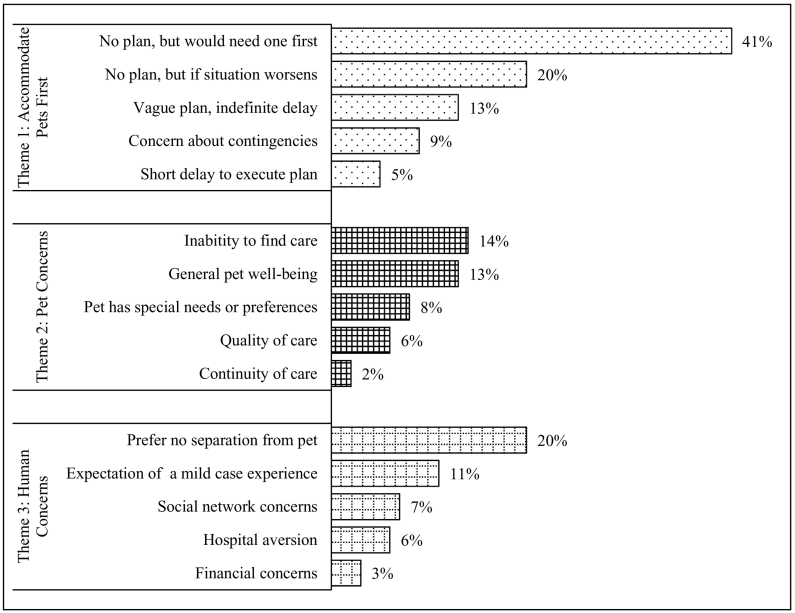
Thematic analyses of open-ended responses (n = 150) demonstrated factors explaining the probable delay or avoidance of testing and treatment for COVID-19 across three themes: (1) pet accommodations; (2) pet-related concerns; and, (3) human-related concerns. Of pet owners who considered delaying or avoiding COVID-19 testing and/or treatment, most (88%, n = 132) would do so to secure pet accommodations before seeking healthcare, indicating a delay of healthcare, rather than avoidance. More than a third (41%, n = 61) of pet owners did not have a plan in place, and many would not make arrangements until they had severe symptoms or a partner also became ill and unable to care for the pet (20%, n = 30). For example, one individual stated, “Depends on the symptoms, I may delay hospitalization until I find a reliable place to care for my pet,” (yes, no1). Another person stated “… I would be worried about finding a proper pet sitter if me and spouse [were] both sick,” (no, maybe), implying the partner is the initial pet care plan, but if things became worse, there would be delays before seeking care. The remaining responses in this theme indicated varying levels of preparation for pet care (see Fig. 1).
Fig. 1.
Explanations for Delaying or Avoiding Testing and/or Treatment for COVID-19 Among Pet Owners (n = 150) Notes: Categories were not mutually exclusive. Percentages shown represent relative frequencies of themes in qualitative responses to the open-ended question prompt “Please explain more about delaying or avoiding testing or treatment for COVID-19 because you were worried about your pet.”
About 42% (n = 64) of respondents explained delay or avoidance in seeking medical care as a concern for their pet related to someone else providing care (“Pet Concerns,” Fig. 1). General concern for the pet's welfare (13%, n = 19) and concern for the quality of pet care in the owner's absence (6%, n = 9) highlight the value of the human-animal bond in these decisions. Indications of an inability, or a fear of inability, to find care for their pet(s) (14%, n = 21), and the uneasiness about the pet having special care needs (8%, n = 12) were prevalent among considerations to delay or avoid medical care. One respondent stated, “My dog is a management case for reactivity to people and other dogs and can only be watched by very few select people. I'd be concerned they could not watch her for some reason and I would have absolutely no other option,” (maybe, maybe).
Finally, 40% (n = 61) of respondents described concerns related to people (“Human Concerns,” Fig. 1), including about 20% (n = 30) of whom expressed a strong desire to forgo medical care to avoid separation from their pet. One person asserted, “… If my husband and I both had [COVID-19] we would not leave our pets,” (maybe, maybe). Expecting to experience only mild symptoms, about 11% (n = 16) of respondents assumed they would not require testing or treatment and could remain at home caring for their pet(s). Conveying typical reliance on social support for pet care, 7% (n = 11) cited concern for their social network, most frequently with regard to potentially exposing them to COVID-19. For example, one person stated, “I would be resistant to go to the hospital [because] I don't really have anyone to take care of my pets. It feels like a burden to ask friends and expensive to hire someone. May be difficult to find someone during the pandemic,” (maybe, maybe). Eight respondents (5%) expressed concern for self or others in a hospital-setting and would avoid hospitalization, unrelated to pets. Only four respondents (3%) indicated they were concerned about finances related to pet care during or after hospitalization. This likely reflects the high-average income sample and might be more prominent among a representative sample. Given that worry about income loss predicted delay or avoidance of treatment in regression models, people may be more concerned with the financial costs of hospitalization rather than that of pet care. However, in a One Health/One Welfare perspective, these concerns are related. One single, low-income respondent notes: “I don't want to be shipped off to a hospital for 3+ weeks and them be all alone, they'll die. Also I'll be bankrupt from the medical bills afterwards and then how would I pay for their care (or a home for us to live in),” (yes, maybe).
A few respondents used the open-ended response to reveal how they did delay or avoid treatment out of concern for their pet when faced with the real-life decision. One woman reported: “I delayed going to the hospital for COVID symptoms because I was worried no one would be there for my dog. I live with my husband but he isn't very good at taking care of our dog,” (yes, yes). This respondent stated the COVID-19 testing shortage ultimately prevented her from being tested, but this experience exemplifies the interdependence of human health and animal welfare when considering access to and availability of social resources.
4. Conclusion
In this study, we examined how pets may factor into decision making for healthcare related to COVID-19. We found that 10% of pet owners might delay or avoid testing, and over 10% might delay or avoid treatment for COVID-19 due to concern for their pet's welfare. This could have major public health implications due to the popularity of pet ownership in the U.S. Level of attachment to one's pet and respondents' access to socioeconomic resources contributed to decision-making. Of particular concern are those who indicated they would not seek care for fear of diminished pet-welfare because an undiagnosed, COVID-19 positive person poses a considerable public health risk.
The contagiousness of COVID-19 and evolving information regarding routes of transmission complicate plans for pets in the event that their owner may become incapacitated or need to enter the hospital due to a severe case. As of September 2020, the vulnerability of household pets to COVID-19 was still not entirely clear, adding the additional concern of disease-spread when planning for pet care2. Pet owners may find that the people or facilities they would normally rely on for pet care are unavailable or unwilling to take a pet from a household with a known or likely positive case. Additionally, the economic toll and widespread job loss related to the pandemic may leave pet owners with even fewer options for alternative care.
An unexpected finding in this study was the prevalence of respondents who indicated they did not have a plan in place for their pet(s) if they were to require treatment. Overall, our findings indicate that pets matter in healthcare decision-making, particularly in acute emergencies like COVID-19. Therefore, it is pertinent for pet owners to make plans for their pets if they are to become hospitalized or incapacitated. Communities need to adopt a One Health/One Welfare approach for human and animal social services to work in concert to support vulnerable pet owners and their animal companions [28] while reducing risk of COVID-19 spread. This could include progressive public policy around pet companionship [29], and/or supporting pet owners financially or instrumentally to address human and pet needs together [30]. In the interest of public health, we recommend community collaboration to provide services and resources to circumvent obstacles that arise for people and their pets during public health emergencies. Fostering partnerships between human and animal health and social workers to encourage public safety and health-planning as a holistic family unit, inclusive of pets, could reduce delays in receiving healthcare by ensuring bonded owners that their pets will be cared for in their absence [31].
4.1. Limitations
Though this convenience sample is disproportionately high-SES, results suggest that low-SES pet owners may face even greater barriers to accessing healthcare as they have fewer resources to depend on for the care of their pets in their absence. It is possible that a sample of pet owners who report more variation in income and geographic location might result in a greater prevalence of economic explanations for delays in seeking health care due to concern for their pets. For example, 93% of this sample reported zip codes from urbanized areas, suggesting that both healthcare and pet care services are locally available. Rural-dwelling pet owners might explain delays due to additional transportation costs to reach areas where they can access COVID-19 testing and treatment, as well as pet boarding services. This could alter or exacerbate economic concerns related to both seeking healthcare and paying for pet care. Moreover, given the well-documented association between SES and racial and ethnic inequality in the United States, a more diverse sample of people who report non-White racial and ethnic identities could reveal other explanations for delays in seeking healthcare out of concern for animal companions, such as reduced network availability and material insecurity that are not represented in these qualitative responses. Finally, the small proportion of men in this sample limits what we know about pet owners delaying and avoiding seeking healthcare out of concern for pets. For example, women in heterosexual relationships in the U.S. take on more caregiving responsibilities when raising human children, and mothers can be skeptical of their male partners' ability to provide equal care [32]. If these gender patterns persist for pet caregiving and are related to gender differences in interactions with pets (e.g., women tend to report slightly stronger attachments to pets than men [33]), a sample including more men might reveal fewer intentions to delay or avoid healthcare, or offer different explanations for delays related to pet welfare. Despite the aforementioned limitations, we highlight the salience in empirically revealing that pet owners may delay testing and treatment out of concern for pets as this has human public health and animal welfare implications.
-
1.
The convention for reporting if a respondent being quoted would consider delaying or avoiding testing or treatment is: the first indicator is for their response to testing, and the second indicator is for their response to treatment in the close-ended questions.
-
2.
Though recent research indicates that pets may be vulnerable to COVID-19 infection [34], evidence of positive cases in animals kept as pets has been rare. For example, a study in France found no evidence of COVID-19 antibodies in a small sample of cats and dogs in close contact with confirmed COVID-19 positive humans [35].
Declaration of Competing Interest
None.
Acknowledgements
Many thanks to Camie Tomlinson, Angela Matijczak, Jennifer Murphy, and Laura Booth for their assistance in the creation of and recruitment for this survey.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Applebaum J.W., Peek C.W., Zsembik B.A. Examining U.S. pet ownership using the General Social Survey. Soc. Sci. J. 2020:1–10. doi: 10.1080/03623319.2020.1728507. [DOI] [Google Scholar]
- 2.U.S. Pet Market Outlook (2020–2021) - Impact of the Coronavirus Pandemic - ResearchAndMarkets.com | Business Wire. 2020. https://www.businesswire.com/news/home/20200409005391/en/U.S.-Pet-Market-Outlook-2020-2021-- (accessed June 30, 2020)
- 3.Irvine L., Cilia L. More-than-human families: pets, people, and practices in multispecies households. Sociol. Compass. 2017;11 doi: 10.1111/soc4.12455. [DOI] [Google Scholar]
- 4.Field N., Orsini L., Gavish R., Packman W. Role of attachment in response to pet loss. Death Stud. 2009;33:334–355. doi: 10.1080/07481180802705783. [DOI] [PubMed] [Google Scholar]
- 5.McConnell A.R., Paige Lloyd E., Humphrey B.T. We are family: viewing pets as family members improves wellbeing. Anthrozoos. 2019;32:459–470. doi: 10.1080/08927936.2019.1621516. [DOI] [Google Scholar]
- 6.Ascione F.R., Weber C.V., Thompson T.M., Heath J., Maruyama M., Hayashi K. Vol. 13. 2007. Battered Pets and Domestic Violence: Animal Abuse Reported by Women Experiencing Intimate Violence and by Nonabused Women, Violence Against Women; pp. 354–373. [DOI] [PubMed] [Google Scholar]
- 7.Power E.R. Renting with pets: a pathway to housing insecurity? Hous. Stud. 2017;32:336–360. doi: 10.1080/02673037.2016.1210095. [DOI] [Google Scholar]
- 8.Chadwin R. Evacuation of pets during disasters: a public health intervention to increase resilience. Am. J. Public Health. 2017;107:1413–1417. doi: 10.2105/AJPH.2017.303877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO Coronavirus Disease (COVID-19) Dashboard. 2020. https://covid19.who.int/ (accessed September 23, 2020) [Google Scholar]
- 10.COVIDView: A Weekly Surveillance Summary of U.S. COVID-19 Activity | CDC. 2020. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html (accessed September 23, 2020) [Google Scholar]
- 11.Mahase E. Covid-19: what is the R number? BMJ. 2020;369:m1891. doi: 10.1136/bmj.m1891. [DOI] [PubMed] [Google Scholar]
- 12.Capps R., Gelatt J. Barriers to COVID-19 Testing and Treatment: Immigrants without Health Insurance Coverage in the United States, Washington, DC. 2020. https://www.immigrationresearch.org/system/files/UninsuredNoncitizens-FS_Final.pdf
- 13.Kim E.J., Marrast L., Conigliaro J. COVID-19: magnifying the effect of health disparities. J. Gen. Intern. Med. 2020;1 doi: 10.1007/s11606-020-05881-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peacock J., Chur-Hansen A., Winefield H. Mental health implications of human attachment to companion animals. J. Clin. Psychol. 2012;68:292–303. doi: 10.1002/jclp.20866. [DOI] [PubMed] [Google Scholar]
- 15.Canady B., Sansone A. Health care decisions and delay of treatment in companion animal owners. J. Clin. Psychol. Med. Settings. 2019;26:313–320. doi: 10.1007/s10880-018-9593-4. [DOI] [PubMed] [Google Scholar]
- 16.Santini J.M., Edwards S.J.L. Host range of SARS-CoV-2 and implications for public health. Lancet Microbe. 2020;0 doi: 10.1016/S2666-5247(20)30069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nir S.M. The Pets Left behind by Covid-19, New York Times. 2020. https://www.nytimes.com/2020/06/23/nyregion/coronavirus-pets.html
- 18.Zinsstag J., Schelling E., Waltner-Toews D., Tanner M. From “one medicine” to “one health” and systemic approaches to health and well-being. Prev. Vet. Med. 2011;101:148–156. doi: 10.1016/j.prevetmed.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Takashima G.K., Day M.J. Setting the one health agenda and the human-companion animal bond. Int. J. Environ. Res. Public Health. 2014;11:11110–11120. doi: 10.3390/ijerph111111110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rock M., Blue G. Healthy publics as multi-species matters: solidarity with people’s pets in one health promotion. Humanit. Soc. Sci. Commun. 2020;7:18. doi: 10.1057/s41599-020-0509-1. [DOI] [Google Scholar]
- 21.García Pinillos R., Appleby M.C., Manteca X., Scott-Park F., Smith C., Velarde A. One welfare - a platform for improving human and animal welfare. Vet. Rec. 2016;179:412–413. doi: 10.1136/vr.i5470. [DOI] [PubMed] [Google Scholar]
- 22.USDA ERS - Rural Classifications. 2016. https://www.ers.usda.gov/topics/rural-economy-population/rural-classifications/ (accessed September 23, 2020)
- 23.Long J.S., Freese J. Third Edit. Stata Press; 2014. Regression Models for Categorical Dependent Variables Using Stata. [Google Scholar]
- 24.Johnson T.P., Garrity T.F., Stallones L. Psychometric evaluation of the Lexington attachment to pets scale (laps) Anthrozoos. 1992;5:160–175. doi: 10.2752/089279392787011395. [DOI] [Google Scholar]
- 25.Zimet G.D., Dahlem N.W., Zimet S.G., Farley G.K. The multidimensional scale of perceived social support. J. Pers. Assess. 1988;52:30–41. doi: 10.1207/s15327752jpa5201_2. [DOI] [PubMed] [Google Scholar]
- 26.StataCorp . 2017. Stata Statistical Software: Release 15. [Google Scholar]
- 27.Charmaz K. SAGE Publications; London: 2006. Constructing Grounded Theory: A Practical Guide through Qualitative Analysis. [Google Scholar]
- 28.Spencer T., Behar-Horenstein L., Aufmuth J., Hardt N., Applebaum J.W., Emanuel A., Isaza N. Factors that influence intake to one municipal animal control facility in Florida: A qualitative study. Animals. 2017;7 doi: 10.3390/ani7070048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rock M.J., Adams C.L., Degeling C., Massolo A., McCormack G.R. Policies on pets for healthy cities: a conceptual framework. Health Promot. Int. 2015;30:976–986. doi: 10.1093/HEAPRO. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rauktis M.E., Rose L., Chen Q., Martone R., Martello A. “Their pets are loved members of their family”: animal ownership, food insecurity, and the value of having pet food available in food banks. Anthrozoos. 2017;30:581–593. doi: 10.1080/08927936.2017.1370225. [DOI] [Google Scholar]
- 31.Rauktis M.E., Hoy-Gerlach J. Animal (non-human) companionship for adults aging in place during COVID-19: a critical support, a source of concern and potential for social work responses. J. Gerontol. Soc. Work. 2020 doi: 10.1080/01634372.2020.1766631. [DOI] [PubMed] [Google Scholar]
- 32.Hays S. Cult. Contraditons Mother. Yale University Press; 1996. Intensive mothering: Women’s work on behalf of the sacred child; pp. 97–130. [Google Scholar]
- 33.Herzog H.A. Gender differences in human–animal interactions: a review. Anthrozoos. 2007;20:7–21. doi: 10.2752/089279307780216687. [DOI] [Google Scholar]
- 34.Shi J., Wen Z., Zhong G., Yang H., Wang C., Huang B., Liu R., He X., Shuai L., Sun Z., Zhao Y., Liu P., Liang L., Cui P., Wang J., Zhang X., Guan Y., Tan W., Wu G., Chen H., Bu Z., Bu Z. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS-coronavirus 2. Science (80-. ) 2020;368:1016–1020. doi: 10.1126/science.abb7015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Temmam S., Barbarino A., Maso D., Behillil S., Enouf V., Huon C., Jaraud A., Chevallier L., Backovic M., Pérot P., Verwaerde P., Tiret L., van der Werf S., Eloit M. Absence of SARS-CoV-2 infection in cats and dogs in close contact with a cluster of COVID-19 patients in a veterinary campus. One Heal. 2020;10:100164. doi: 10.1016/j.onehlt.2020.100164. [DOI] [PMC free article] [PubMed] [Google Scholar]