Abstract
The origin of the novel human coronavirus (SARS-CoV-2) and its potential for harm increased face mask and medical waste in the environment, thereby necessitating the urgent prevention and control of the pandemic. The article estimates the face mask and medical waste generation in Asia during the pandemic to convince the waste management and scientific communities to find ways to address the negative impact that the waste disposal has on the environment. Standardisation, procedures, guidelines and strict implementation of medical waste management related to COVID-19, community habitats and public areas should be carefully considered to reduce pandemic risks in hospitals, as proper medical waste disposal effectively controls infection sources.
Keywords: Infectious waste, SARS-CoV-2, Transmission, Waste management, Outbreak, Disposal
Graphical abstract
1. Introduction
The emergence of the novel coronavirus (COVID-19) disease has attracted global attention [1] since December 2019. The first outbreak of coronavirus disease 2019 (COVID-19), which is caused by a novel severe acute respiratory syndrome, namely, coronavirus 2 (SARS-CoV-2), occurred in Wuhan, Hubei Province, China [2]. Although most countries have closed their borders to prevent unnecessary travel and immigration, the possibility of confirmed cases and deaths is still increasing due to increased community transmission and increased capacity for testing [3]. World Health Organisation (WHO) and the US Centers for Disease Control and Prevention, the National Centers for Disease Control and local governments have announced various guidelines, including frequent handwashing, social distancing and quarantine (home, local and state quarantine), to reduce the spread and health risks associated with COVID-19. These institutions have also recommended medical personnel and the general population to use personal protective equipment (PPE) such as surgical or medical masks, non-medical face masks (including various forms of self-made or commercial masks of cloth, cotton or other textiles), face shields, aprons and gloves. More and more countries have recommended wearing masks when going out in public places. The press conference study of the Joint Prevention and Control Mechanism of the State Council of China found that approximately 468.9 tons of medical waste are generated every day in association with COVID-19 [4,5]. On the other hand, it was found in Indonesia (Jakarta) that the medical waste scale had reached 12,740 tons approximately 60 days after people were first infected by coronavirus in the area [6,7]. Infectious waste is characterised as any material that is suspected to contain pathogens (bacteria, viruses, parasites or fungi) in sufficient concentration or quantity to cause disease in susceptible hosts. It also comprises waste contaminated with blood, bodily fluids, tissues, organs and sharp objects from treatment and, therefore, also includes diagnosis, swabs, medical devices and so on [8,9]. Therefore, it is harmful to health. In particular, infectious waste generated by the COVID-19 outbreak has posed a major environmental and health concern in many countries [1]. In particular, inadequate solid waste management may increase the spread of coronavirus, especially in developing countries [10].
Currently, millions of contaminated face masks, gloves and materials for diagnosing, detecting and treating SARS-CoV-2 and other human pathogens are undergoing the irreversible process of becoming infectious waste. This, in turn, will cause environmental and health problems if they are stored, transported and handled improperly [3]. Moreover, due to the increased healthcare waste owing to the COVID-19 pandemic, the threat that unsafe disposal of medical waste will spill over into environmental pollution is palpable and immediate [11]. A recent study Kampf et al. [12] found that human coronaviruses can remain active on inanimate hard surfaces (such as metal, glass or plastic) for up to nine days. Although some Asian countries still do not follow proper management strategies and insufficient solid waste containers are one of the major problems that lead to the contamination of infectious waste in solid waste containers in the general community, the threat will be greater in developing countries that do not have sufficient resources for solid waste management. In particular, most developing countries, such as Cambodia, Philippines, Thailand, India, Malaysia, Indonesia, Bangladesh, Vietnam and Palestine are widely perceived to be dump solid waste in poorly managed and open landfills [13,14]. This is another example where improper management of contaminated PPEs and healthcare waste may increase the spread of viral disease in the environment [3].
Consequently, one of the many problems that will inevitably occur is contagious waste, which, if not managed properly, may be the root cause of severe diseases and environmental problems. Hence, the purpose of this work is to estimate face mask use and medical waste during the COVID-19 pandemic, thereby calling on the waste management and scientific communities to express their concerns and take the requisite actions for the formulation of appropriate solid waste management policies and strategies to governments at all levels.
2. Materials and methods
2.1. Population, urban population (percentage) and COVID-19 cases confirmed on databases
Data on the population and the total number of confirmed COVID-19 cases were collected from 49 countries in Asia from https://www.worldometers.info/coronavirus/, [15]. In addition, information about the urban population (percentage of the total population) was collected from https://www.worldometers.info/population/asia/, [16]. This method was used to highlight the spatial variation of the pandemic, which not only exists between different countries but also, more importantly, exists within each country. These data are important to estimate COVID-19 related face mask and medical waste generation in Asia.
2.2. Estimation of daily face mask usage and medical waste
2.2.1. Estimation of daily face mask usage of general population
The quantity of daily face mask is estimated using an equation adapted from Nzediegwu and Chang [3] as follows:
where.
2.2.2. Estimation of medical waste
The amount of medical waste generated at different hospitals is proportional to the number of infected persons and the average waste generation per bed. An early study reveals that the daily generation of medical waste in Jordan is 2.69 kg/bed/day [18]. Meanwhile, estimated values and analysis of medical waste in the city of Istanbul showcased that the yearly average values of daily unit medical waste per hospital bed have increased from 0.43 kg/bed/day in 2000 to 1.68 kg/bed/day in 2017 [19]. In April 2020, the highest rate of medical waste was estimated at around 14,500 tons during the COVID-19 pandemic. This has undoubtedly increased since then due to the increasing infection rate [20]. For instance, the amount of medical waste peaked to 240 tons per day [6,7] in Wuhan City. At the same time, the medical waste amounted to the average value of 206 tons per day in Dhaka, Bangladesh [20]. Recently, in Jordan, the study conducted by Abu-Qdais et al. [21] found that the average medical waste generated in King Abdullah University Hospital as a result of COVID-19 treatment was 3.95 kg/bed/day. In general, in the context of the COVID-19 pandemic, medical waste related with diagnoses and patients’ treatment is expected to be higher than the general average of infectious disease and the detected upper limit [7]. Therefore, the estimation of medical waste provided by previous studies in Jordan (3.95 kg/bed/day) has been further considered in the medical waste analysis as follows:
where.
MW = Medical waste (tons/day)
NCC = Number of COVID-19 cases (infected persons)
MWGR = Medical waste generation rate, that is, 3.95 kg/bed/day
The number of confirmed cases is available at https://www.worldometers.info/coronavirus/ for the Asia region. The total number of confirmed cases represents the infected persons who were treated in hospitals without recovering or those who were declared dead after being infected with COVID-19. Consequently, the total confirmed COVID-19 cases comprise the ones wherein patients were treated in hospitals during the emergency state.
2.3. Limitation of the study
This is a cross-sectional study that aims to provide a rapid estimation of potential face mask and medical waste associated with the COVID-19 pandemic in Asia. This examination depends on the reliability of COVID-19 case statistics and available information in this regard, as mentioned in Sections 2.1 and 2.2 [number of confirmed cases, number of populations, urban population (per cent), and so on]. On the other hand, the medical waste generation rates (kg/bed/day) and waste generation rates are taken into consideration and supported by previous studies [7].
3. Results and discussions
3.1. Daily face mask usage and medical waste in Asia during COVID-19 pandemic
This study estimates the number of face masks used in self-defence and medical waste generated by the total COVID-19 cases in developed and developing countries in Asia during the crisis. The result showed that more than one hundred thousand people were infected in Asian countries, such as India, Iran, Pakistan, Saudi Arabia, Turkey, Bangladesh, Qatar and Indonesia. The number of masks used in 49 Asian countries was estimated from the COVID-19 pandemic database on July 31, 2020. Subsequently, it was found that 2,228,170,832 face masks were used in Asia in total. In particular, the selected countries that use the most daily face masks are China (989,103,299 pieces), followed by India, Indonesia, Bangladesh, Japan, Pakistan, Iran, Philippines and Vietnam with 381,179,657, 159,214,791, 99,155,739, 92,758,754, 61,762,860, 50,648,022, 48,967,769 and 46,288,632 pieces, respectively (see Table 1 ). The maximum face mask use by the general population in Asian regions was found in Eastern Asia (1,110,472,794 pieces), followed by Southern Asia, Southeastern Asia, Western Asia and Central Asia, thereby amounting to 648,945,814, 295,458,617, 142,162,166 and 31,131,442 pieces, respectively (Fig. 1 ). The research conducted by Nzediegwu and Chang [3] perceived the apparent fact that the total number of face masks used every day has increased during the COVID-19 outbreak. This study used mathematic calculation to estimate the numerical value of face mask usage across Asian countries. Consequently, it was found that the quantity of daily face mask usage depends on the number of people residing in a certain country, urban population (per cent), face masks acceptance rate (per cent) and average daily face masks per capita. Thus, this equation can be applied to the estimation of face mask scenarios during the COVID-19 pandemic for healthcare waste management (HWM).
Table 1.
Estimated daily face mask use and medical waste in Asia with confirmed COVID-19 cases.
| Country | aPopulation | aTotal COVID-19 cases | bUrban population (%) | Face masks acceptance rate (%) | Number of face mask need of each general population each day | Total daily face mask use (pieces) | Medical waste (tons/day) |
|---|---|---|---|---|---|---|---|
| India | 1,381,085,714 | 1,643,416 | 35 | 80 | 1 | 381,179,657 | 6,491.49 |
| Iran | 84,077,062 | 301,530 | 75 | 80 | 1 | 50,648,022 | 1,191.04 |
| Pakistan | 221,213,683 | 278,305 | 35 | 80 | 1 | 61,762,860 | 1,099.30 |
| Saudi Arabia | 34,855,542 | 274,219 | 84 | 80 | 1 | 23,367,155 | 1,083.17 |
| Bangladesh | 164,820,045 | 234,889 | 75 | 80 | 1 | 99,155,739 | 927.81 |
| Turkey | 84,410,984 | 229,891 | 39 | 80 | 1 | 26,066,112 | 908.07 |
| Iraq | 40,288,721 | 121,263 | 96 | 80 | 1 | 30,973,969 | 478.99 |
| Qatar | 2,807,805 | 110,460 | 60 | 80 | 1 | 1,341,008 | 436.32 |
| Indonesia | 273,753,080 | 106,336 | 73 | 80 | 1 | 159,214,791 | 420.03 |
| Philippines | 109,694,822 | 89,374 | 56 | 80 | 1 | 48,967,769 | 353.03 |
| Kazakhstan | 18,794,372 | 89,078 | 58 | 80 | 1 | 8,675,482 | 351.86 |
| China | 1,439,323,776 | 84,292 | 86 | 80 | 1 | 989,103,299 | 332.95 |
| Oman | 5,115,955 | 79,159 | 47 | 80 | 1 | 1,927,692 | 312.68 |
| Israel | 91,97,590 | 70,379 | 100 | 80 | 1 | 7,358,072 | 278.00 |
| Kuwait | 4,275,450 | 66,529 | 86 | 80 | 1 | 2,941,510 | 262.79 |
| United Arab Emirates | 9,899,794 | 60,223 | 100 | 80 | 1 | 7,919,835 | 237.88 |
| Singapore | 5,854,053 | 51,809 | 93 | 80 | 1 | 4,364,782 | 204.65 |
| Bahrain | 1,705,531 | 40,755 | 25 | 80 | 1 | 343,835 | 160.98 |
| Armenia | 2,963,706 | 38,196 | 89 | 80 | 1 | 2,114,901 | 150.87 |
| Afghanistan | 38,992,638 | 36,542 | 63 | 80 | 1 | 19,589,901 | 144.34 |
| Kyrgyzstan | 6,532,418 | 35,619 | 56 | 80 | 1 | 2,916,071 | 140.70 |
| Japan | 126,443,231 | 33,049 | 92 | 80 | 1 | 92,758,754 | 130.54 |
| Azerbaijan | 10,146,497 | 31,560 | 21 | 80 | 1 | 1,712,729 | 124.66 |
| Uzbekistan | 33,506,746 | 23,558 | 50 | 80 | 1 | 13,456,309 | 93.05 |
| Nepal | 29,176,450 | 19,547 | 82 | 80 | 1 | 19,046,387 | 77.21 |
| South Korea | 51,272,891 | 14,305 | 36 | 80 | 1 | 14,561,501 | 56.50 |
| Palestine | 5,110,066 | 11,548 | 78 | 80 | 1 | 3,180,505 | 45.61 |
| Malaysia | 32,398,441 | 8,964 | 27 | 80 | 1 | 7,049,901 | 35.41 |
| Tajikistan | 9,553,361 | 7,366 | 80 | 80 | 1 | 6,083,580 | 29.10 |
| Lebanon | 6,822,802 | 4,334 | 51 | 80 | 1 | 2,756,412 | 17.12 |
| Maldives | 541,266 | 3,719 | 34 | 80 | 1 | 148,090 | 14.69 |
| Thailand | 69,814,554 | 3,310 | 18 | 80 | 1 | 10,220,851 | 13.07 |
| Hong Kong | 7,501,879 | 3,152 | 79 | 80 | 1 | 4,711,180 | 12.45 |
| Sri Lanka | 21,420,649 | 2,814 | 100 | 80 | 1 | 17,136,519 | 11.12 |
| Yemen | 29,874,304 | 1,726 | 38 | 80 | 1 | 9,033,990 | 6.82 |
| Jordan | 10,211,202 | 1,191 | 91 | 80 | 1 | 7,425,586 | 4.70 |
| Georgia | 3,988,514 | 1,168 | 67 | 80 | 1 | 2,131,462 | 4.61 |
| Cyprus | 1,208,070 | 1090 | 58 | 80 | 1 | 557,645 | 4.31 |
| Syria | 17,531,446 | 738 | 79 | 80 | 1 | 11,009,748 | 2.92 |
| Vietnam | 97,408,737 | 509 | 59 | 80 | 1 | 46,288,632 | 2.01 |
| Taiwan | 23,820,377 | 467 | 37 | 80 | 1 | 7,050,832 | 1.84 |
| Myanmar | 54,439,424 | 353 | 31 | 80 | 1 | 13,500,977 | 1.39 |
| Mongolia | 3,282,334 | 291 | 67 | 80 | 1 | 1,767,209 | 1.15 |
| Cambodia | 16,736,949 | 234 | 24 | 80 | 1 | 3,186,715 | 0.92 |
| Brunei | 437,813 | 141 | 79 | 80 | 1 | 276,698 | 0.56 |
| Bhutan | 772,280 | 101 | 45 | 80 | 1 | 278,639 | 0.40 |
| Macao | 650,024 | 46 | 100 | 80 | 1 | 520,019 | 0.18 |
| Timor-Leste | 1,320,331 | 24 | 32 | 80 | 1 | 342,230 | 0.09 |
| Laos | 7,283,730 | 20 | 35 | 80 | 1 | 2,045,271 | 0.08 |
| Total | 4,612,337,109 | 4,217,589 | 2,228,170,832 | 16,659.48 |
Data source: retrieved on July 31, 2020 from: https://www.worldometers.info/coronavirus/.
Data source: retrieved on July 31, 2020 from: https://www.worldometers.info/population/asia/.
Fig. 1.
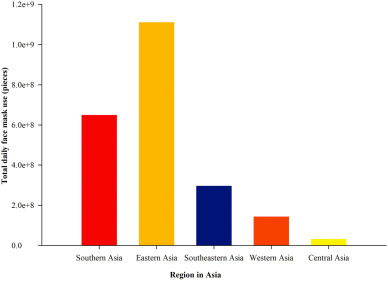
Face mask usage of general population in Asia region.
It was found while conducting this study that the total medical waste generated in Asia is around 16,659.48 tons/day. The countries with the highest medical waste are India (6,491.49 tons/day), followed by Iran (1,191.04 tons/day), Pakistan (1,099.30 tons/day), Saudi Arabia (1,083.17 tons/day), Bangladesh (927.81 tons/day) and Turkey (908.07 tons/day). Information about the medical waste of other countries has been included in Table 1. Indeed, due to the rapid increase in the number of confirmed cases, the amount of medical waste related to COVID-19 has also significantly increased. The use of medical gloves, surgical face masks and aprons has been recommended for essential healthcare service staff such as physicians, nurses, medical technologists and nurses’ aides. Moreover, face mask use has been mandated for citizens [3,5].
3.2. Infection control special team and medical waste management frame during the COVID-19 pandemic
A special infection prevention and control team was established to discuss potential problems and countermeasures. The administrative and operating boards include the nosocomial infection control expert, director of infectious disease department, respiratory disease department, nursing department, local government organisations, multi-level quarantine departments, environmental health and safety, logistics departments (special waste management in the private sector or partnerships) and administrative leaders. Each department has specific personnel who are allocated to coordinate and improve the management of medical and household waste during COVID-19 outbreak (Fig. 2 ).
Fig. 2.
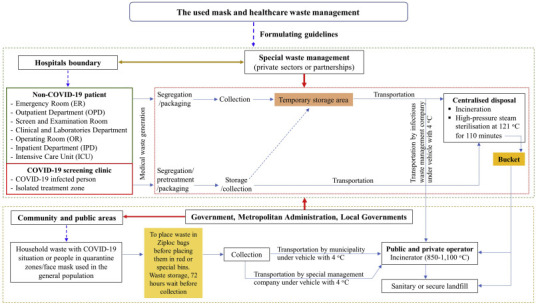
Scheme of medical and households waste management frame during COVID-19 outbreak.
3.3. Managing infectious waste for final disposal during the COVID-19 pandemic
The COVID-19 outbreak has increased medical waste all across the world. The results of this study showed that it has also led to a huge amount of face mask and medical waste. The SARS-CoV-2 pandemic has caused a global emergency and aroused social and economic concerns in addition to excessive medical and household waste, which adversely affects municipal waste management, thereby spilling over into environmental issues [22]. In particular, another aspect of the spread of COVID-19 is improper solid waste management. If waste is not managed properly, it may lead to the spread of the virus. Consequently, the number of confirmed cases has rapidly increased and the amount of medical waste associated with COVID-19 has also significantly increased [5]. In addition, existing operational protocols for HWM and municipal solid waste (MSW) management should be continued for SARS-CoV-2 waste, with specific precautionary measures, adjustments and arrangements applied to reduce any potential risk of SARS-CoV-2 infection due to the improper waste management process. The following sections describe the used mask and medical waste management in detail.
3.3.1. Categorised containers or packaging and pre-treatment
Medical waste includes those elements that have been contaminated by blood, body fluids and cultures produced in laboratories, stockpiles of infectious agents or waste generated through medical wards and equipment [23]. During the COVID-19 pandemic, the disposal capacity of medical waste is seriously insufficient [24]. This is because the use of protective masks has greatly increased the possibility of carrying pathogens. Therefore, some medical waste buckets with obvious mark points are placed in the public areas of hospitals and communities to collect abandoned masks. They are packaged in double-layered medical waste bags and treated as general medical waste by specific personnel, municipal solid waste workers and the company’s special waste management department [25]. Meanwhile, by stratifying patients on the basis of risk, special care facilities can be facilitated with appropriate health care personnel, procedures and PPEs (long-sleeved gowns, gloves, boots, masks and goggles or face masks) to provide maximum protection against nosocomial infections and optimise patient care [26], thereby effectively managing infectious waste in hospitals.
Therefore, the medical waste generated by clinics, wards, specialised examination rooms and medical laboratories (especially, nucleic acid testing laboratories) should be regarded as medical waste related to COVID-19 and should be labelled as ‘COVID-19 infectious waste’. This label should be attached by special personnel during the packaging phase. Subsequently, this waste is placed into double yellow or red medical waste bags. Finally, before placing the bag in the medical waste bucket for temporary storage on site, 0.5% (5000 ppm) chlorine disinfectant should be sprayed on the surface of the bag [27]. Alternately, chlorine-based products (for example, hypochlorite) at 0.1% (1000 ppm) can be used for general environmental disinfection [28]. However, chlorine solutions at lower pH have much shorter shelf lives [29]. Thus, chlorine solutions (0.1% or 0.5%) should ideally be freshly prepared every day [28]. Therefore, after isolation and packaging in another double-layered medical waste bag, a chlorine-rich disinfectant was sprayed again to disinfect the waste. The specimens or preservation solutions containing pathogens in laboratories or clinics should be sealed and packaged first. Subsequently, they should be autoclaved at 121 °C for 110 min [5] or maintained at a high temperature (more than 70 °C) for over 5 min. This process is reported to be extremely effective in inactivating SARS-CoV-2 [30] from the waste. The bag should then be placed in a medical waste bucket and incinerated in hospitals until the storage period is less than 24 h [5]. This quickly and efficiently reduces the potential for contamination of medical waste, which may have the potential to spread COVID-19, and protects patients who are in sickbeds and medical personnel during COVID-19 outbreak within hospitals. Thus, the facts have proved that timely, orderly, effective and harmless treatment of medical waste related to COVID-19 has also become an important part of the fight against the pandemic [5]. In addition, public areas and households are advised to place used face masks in Ziploc bags or bags that are sealed with ropes or rubber bands before placing them in red or special bins, which are subsequently collected for proper disposal.
3.3.2. Segregation and storage
Screening and examination from hospitals and COVID-19 in outpatient treatment areas directly generate infectious waste. These wastes must be immediately separated from the general wastes, packaged and then stored and collected for transportation to the hospital for centralised disposal. A separate temporary storage area has been established for COVID-19-related medical waste with easily visible warning signs. Medical waste buckets from clinics, observation wards, isolation wards and nucleic acid testing laboratories are placed in this area to prevent mixing with other wastes in the general wards. The temporary storage time of COVID-19-related medical waste in hospitals should not exceed 24–48 h [5] while waste related with COVID-19 generated by people should undergo mandatory quarantine sorting at home and the authorities should wait for 72 h before collection [31]. The inorganic part of most municipal solid wastes in developed and developing countries is mainly composed of plastic, rubber, metal and glass [32]. This suggests that waste materials generated from households and quarantine facilities with infected or suspected patients may possibly contain traces of COVID-19 and could be a source of infection for people outside the facility [31]. As recently discovered, SARS-CoV-2 can stay on hard surfaces for long periods of time, specifically, 72 h on plastic, 48 h on stainless steel [33] and 24 h on paper and cardboard [25]. Therefore, a 72-h-delay in the collection does not seem to be sufficient to ensure safety and may lead to COVID-19 infection amongst waste workers [31,34]. Moreover, poor management can possibly increase the chances of COVID-19 spread in the environment due to transmission of the SARS-CoV-2 through two channels, namely, respiratory channels and physical touch [35]. Respiratory droplets are generated when an infected person coughs or sneezes. Apart from human-to-human transmission, droplets may also stay active on surfaces where the virus could remain viable. Thus, the immediate environment of an infected individual can serve as a source of transmission [35]. This, in turn, may affect the spread of the infection in urban areas and similar set-ups through inadequate management of municipal solid waste [22]. Therefore, MSW management implemented under the government in local governments or private sector’s partnership should include the provision of infectious or special waste containers for used masks and other infectious waste in communities and public areas to ensure proper collection operations.
3.3.3. Collection and transportation
Additional vehicles should have a non-absorbent, sealed loading area, which can be locked, disinfected and separated from the main vehicle. The vehicle identification or chassis number should be recorded for future control [36]. In addition, the disposal of medical waste related to COVID-19 should be arranged by specially trained workers and special vehicles, which should be different from general medical waste collection vehicles. A specific logbook is used to maintain detailed records of the time spent by waste and quantity of waste in internal and external carriers. In addition, the transportation routes should avoid crowds as much as possible, and the time should avoid morning and evening rush hours. The vehicles for medical waste should be installed with closed loading box and maintained at 4 °C when transporting the medical waste storage from hospitals [37]. If there is no dedicated special waste collection mechanism in place for masks used in households and generated in public areas, then the waste should be double-packaged and disposed by following the general waste management strategies during the COVID-19 outbreak by increasing collection frequency to incineration or secure landfills. These transportation vehicles should be disinfected immediately after loading and unloading. Thus, considering the risk exposure level in the working environment of waste collectors, they need to be provided with PPEs for collecting and transferring waste and wearing medical masks, gloves, protective clothing and waterproof shoes should be mandated for them. Moreover, alcohol solution should be prepared in the plastic bottles, which are provided to collectors and transporters. This should be used for disinfecting the vehicles with 70% alcohol solution before and after waste collection and end operations so that proper hygiene is maintained during such disposal [35].
3.3.4. Disposal
Most countries that generate excessive waste should evaluate their management systems to properly incorporate medical waste disposal during the COVID-19 pandemic. Therefore, waste management through its different phases (that is, pre-treatment, segregation, storage, delivery, collection, transportation and disposal) can represent another way for SARS-CoV-2 to spread, mainly through contact with contaminated surfaces and objects. Hence, all necessary precautions must be taken to prevent the potential spread of infectious viruses and feasible guidelines should be put forward. The guidelines should also consider socio-economic conditions and technologies available in specific environments [34]. However, healthcare waste must be treated by incineration and secure landfill. Thus, priority is given to high-temperature incineration to dispose medical waste related to COVID-19. This is the most common, biologically safe [38] and suitable method to destroy traces of the virus with high furnace temperature, and the incineration temperature and duration are set to 1100 °C for 3 min. In these facilities, combustion efficiency is ensured by using specific equipment capable of maintaining a minimum temperature of more than 850 °C and a residence time of waste in the furnace of more than 1 h [39]. For example, emergency incineration of medical waste in China during COVID-19 includes the use of municipal solid waste incinerators to co-process medical waste for medical waste disposal in rotary kilns whose temperature is controlled above 850 °C [24]. However, in some areas without incineration capacity, medical waste can be also treated with high-temperature sterilisation (autoclave) and boiling before entrance into the sanitary landfills. Nevertheless, the overall capacity for medical waste disposal during the COVID-19 pandemic is seriously inadequate. For instance, in developing countries in Asia such as India, Bangladesh, Thailand, Indonesia, Myanmar and Malaysia, landfills continue to be one of the most common MSW management options [40]. Thus, the management of mask use and medical waste needs strict operations such as segregation, sorting, storage, collection, transport and final disposal. This, in turn, should reduce the spread of COVID-19 in the environment and in several countries. Mostly, each country recognises and attaches great importance to preventing the spread of the pandemic amongst its citizens. The recommended practice that is widely used is wearing a mask to reduce COVID-19 infection and spread. Consequently, there has been a dramatical increase in face mask and medical waste during the COVID-19 pandemic. However, every country is aware that waste management and proper disposal of face masks and medical waste play a critical role in preventing the spread of COVID-19 in the neighbouring communities and healthcare service sectors. Moreover, the author gathered guidelines and recommendations for management and disposal of used face masks in certain Asian nations, as illustrated in Table 2 , and practices for related COVID-19 waste management generated from healthcare facilities, which have been adopted by some countries during COVID-19 pandemic (Table 3 ).
Table 2.
Disposal management of face masks during the COVID-19 pandemic in Asian countries.
| Country | Recommended for Face Masks’ Waste Management | References |
|---|---|---|
| Thailand (Bangkok and local government) |
|
[[41], [42], [43]] |
| China |
|
[44,45] |
| India |
|
[46] |
| Singapore |
|
[47] |
| South Korea |
|
[37] |
| Malaysia |
|
[48] |
| Taiwan |
|
[49,50] |
Table 3.
Existing practices for infectious waste separation, storage, transportation and disposal in Asian countries.
| Country | Practices for COVID-19 Waste Generated from Healthcare Facilities | COVID-19 Waste Treatment and Disposal |
|---|---|---|
| India |
|
|
| China |
|
|
| Bangladesh |
|
Incineration |
| Indonesia |
|
Mostly incineration, disinfecting at source and transporting to the disposal site, open burning (if no incinerator) or hazardous waste landfill. |
| Japan |
|
Incineration, melting, steam sterilisation (autoclave), dry sterilisation and disinfection followed by shredding and disposal to sanitary landfills. |
| Malaysia |
|
Mostly incineration |
| Nepal |
|
Mostly burned, small-scale incineration or dumped in backyards, municipal landfills |
| Thailand |
|
Incineration, autoclave, WMSP, sanitary landfill. |
3.4. New challenge in plastics waste management
This comprises disposable gowns made from polyester or polyethylene such as a surgical masks, gloves, N95 respirators, face shields (polycarbonate or polyvinyl chloride) as well as hand sanitisation products with packaging made with polyethylene terephthalate (PET) for alcohol and other disinfectant solutions [[52], [53]]. The COVID-19 pandemic presents growing environmental consequences related to plastic use and follow-up waste. In this context, PPEs are critically needed. Most of these PPEs comprise single-use plastic. Therefore, it was found that, during the peak of the outbreak, hospitals in Wuhan produced more than 240 tons of waste per day in comparison to the 40 tons that was earlier produced during normal circumstances with most of the waste comprising plastic PPEs [53]. Furthermore, COVID-19 face masks are a potentially high source of microplastic fibres, which have the possibility of being released into the environment [54]. These emerging challenges in solid waste management during and after the pandemic have been discussed from the perspective of novel study and environmental policies. Thus, it is necessary to plan and consider separation, storage and collection for recycling and disposing face masks and medical waste to reduce plastic waste and adopt alternative technology in the form of waste with a view to facilitating energy recovery.
4. Conclusion
This is the first study to estimate the face mask and medical waste use in the context of the COVID-19 pandemic in Asia. The finding shows that the number of face masks used and medical waste has increased with the steady increase in the number of confirmed SARS-CoV-2 cases. COVID-19 is pathogenic virus, and the concerned authorities should pay significant attention to all aspects of prevention and control. Standardisation, procedures, guidelines and strict implementation of medical waste management for the COVID-19 pandemic should be carefully considered to reduce the risk of the pandemic spreading to the environment within hospitals, community residences and public areas.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Saadat S., Rawtani D., Hussain C.M. Environmental perspective of COVID-19. Sci. Total Environ. 2020;728:138870. doi: 10.1016/j.scitotenv.2020.138870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harapan H., Itoh N., Yufika A., Winardi W., Keam S., Te H., Megawati D., Hayati Z., Wagner A.L., Mudatsir M. Coronavirus disease 2019 (COVID-19): A literature review. J. Infect. Public. Health. 2020;13(5):667–673. doi: 10.1016/j.jiph.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nzediegwu C., Chang S.X. Improper solid waste management increases potential for COVID-19 spread in developing countries. Resour. Conserv. Recycl. 2020;161:104947. doi: 10.1016/j.resconrec.2020.104947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The State Council Information Office of the People’s Republic of China, Press Conference on Strengthening Comprehensive Treatment of Medical Waste and Environmental Protection. 2020. http://www.scio.gov.cn/xwfbh/gbwxwfbh/xwfbh/wsb/Document/1675174/1675174.htm (Chinese translate to English) [Google Scholar]
- 5.Peng J., Wu X., Wang R., Li C., Zhang Q., Wei D. Medical waste management practice during the 2019-2020 novel coronavirus pandemic: Experience in a general hospital. Am. J. Infect. Contr. 2020;48(8):918–921. doi: 10.1016/j.ajic.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eria . 2020. Strengthening Waste Management Policies to Mitigate the COVID-19 Pandemic.https://www.eria.org/uploads/media/policy-brief/Strengthening-Waste-Management-Policies-to-Mitigate-the-COVID19-Pandemic-.pdf [Google Scholar]
- 7.Mihai F.-C. Assessment of COVID-19 waste flows during the emergency State in Romania and related public health and environmental concerns. Int. J. Environ. Res. Publ. Health. 2020;17:5439. doi: 10.3390/ijerph17155439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yong Z., Gang X., Guanxing W., Tao Z., Dawei J. Medical waste management in China: A case study of Nanjing. Waste Manag. 2009;29(4):1376–1382. doi: 10.1016/j.wasman.2008.10.023. [DOI] [PubMed] [Google Scholar]
- 9.WHO . 2017. Safe Management of Wastes from Health-Care Activities: A Summary.https://apps.who.int/iris/bitstream/handle/10665/259491/WHO-FWC-WSH-17.05-eng.pdf?sequence=1 [Google Scholar]
- 10.Mol M.P.G., Caldas S. Can the human coronavirus epidemic also spread through solid waste? Waste Manag. Res. 2020;38(5):485–486. doi: 10.1177/0734242X20918312. [DOI] [PubMed] [Google Scholar]
- 11.Singh N., Tang Y., Zhang Z., Zheng C. COVID-19 waste management: Effective and successful measures in Wuhan, China. Resour. Conserv. Recycl. 2020;163:105071. doi: 10.1016/j.resconrec.2020.105071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Bank . 2019. Solid Waste Management.https://www.worldbank.org/en/topic/urbandevelopment/brief/solid-waste-management [Google Scholar]
- 14.Ferronato N., Torretta V. Waste mismanagement in developing countries: A review of global issues. Int. J. Environ. Res. Publ. Health. 2019;16(6):1060. doi: 10.3390/ijerph16061060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Worldometers COVID-19 coronavirus pandemic 2020. 2020. https://www.worldometers.info/coronavirus/
- 16.Worldometers Population: Asia. 2020. https://www.worldometers.info/population/asia/ 2020.
- 17.Wu H.-L., Huang J., Zhang C.J.P., He Z., Ming W.-K. Facemask shortage and the novel coronavirus disease (COVID-19) outbreak: Reflections on public health measures. EClinicalMedicine. 2020;21:100329. doi: 10.1016/j.eclinm.2020.100329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Minoglou M., Gerassimidou S., Komilis D. Healthcare waste generation worldwide and its dependence on socio-economic and environmental factors. Sustainability. 2017;9:220. [Google Scholar]
- 19.Korkut E.N. Estimations and analysis of medical waste amounts in the city of Istanbul and proposing a new approach for the estimation of future medical waste amounts. Waste Manag. 2020;81:168–176. doi: 10.1016/j.wasman.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 20.Rahman M.M., Bodrud-Doza M., Griffiths M.D., Mamun M.A. Biomedical waste amid COVID-19: perspectives from Bangladesh. Lancet Global Health. 2020;8 doi: 10.1016/S2214-109X(20)30349-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abu-Qdais H.A., Al-Ghazo M.A., Al-Ghazo E.M. Statistical analysis and characteristics of hospital medical waste under novel Coronavirus outbreak. Global J. Environ. Sci. Manage. 2020;6:21–30. [Google Scholar]
- 22.Kulkarni B.N., Anantharama V. Repercussions of COVID-19 pandemic on municipal solid waste management: Challenges and opportunities. Sci. Total Environ. 2020;743:140693. doi: 10.1016/j.scitotenv.2020.140693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zamparas M., Kapsalis V.C., Kyriakopoulos G.L., Aravossis K.G., Kanteraki A.E., Vantarakis A., Kalavrouziotis I.K. Medical waste management and environmental assessment in the Rio University hospital, Western Greece. Sust. Chem. Pharm. 2019;13:100163. [Google Scholar]
- 24.Ma Y., Lin X., Wu A., Huang Q., Li X., Yan J. Suggested guidelines for emergency treatment of medical waste during COVID-19: Chinese experience. Environ. Prog. Sustain. Energy. 2020;2:81–84. doi: 10.1007/s42768-020-00039-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.UNEP . 2020. Waste Management during the COVID-19 Pandemic.http://wedocs.unep.org/bitstream/handle/20.500.11822/33416/WMC-19.pdf?sequence=1&isAllowed=y [Google Scholar]
- 26.Kim J.-H., An J.A.-R., Min P.-k., Bitton A., Gawande A.A. How South Korea responded to the Covid-19 outbreak in Daegu. NEJM Catalyst. 2020;1(4) [Google Scholar]
- 27.Yves C., Jorge E., Ute P., Annette P., Philip R., Ruth S., William T., Susan W., Raki Z., editors. Safe Management of Wastes from Health-Care Activities. 2014. https://www.who.int/water_sanitation_health/publications/wastemanag/en/ [Google Scholar]
- 28.WHO Cleaning and disinfection of environmental surfaces in the context of COVID-19. 2020. https://www.who.int/publications/i/item/cleaning-and-disinfection-of-environmental-surfaces-inthe-context-of-covid-19
- 29.Iqbal Q., Lubeck-Schricker M., Wells E., Wolfe M.K., Lantagne D. Shelf-life of chlorine solutions recommended in Ebola virus disease response. PloS One. 2016;11(5) doi: 10.1371/journal.pone.0156136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chin A.W.H., Chu J.T.S., Perera M.R.A., Hui K.P.Y., Yen H.-L., Chan M.C.M.C.W., Peiris M., Poon L.L.M. Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe. 2020;1(1) doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nghiem L.D., Morgan B., Donner E., Short M.S. The COVID-19 pandemic: Considerations for the waste and wastewater services sector. Case Studies in Chemical and Environmental Engineering. 2020;1:100006. doi: 10.1016/j.cscee.2020.100006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kumar A., Samadder S.R. A review on technological options of waste to energy for effective management of municipal solid waste. Waste Manag. 2017;69:407–422. doi: 10.1016/j.wasman.2017.08.046. [DOI] [PubMed] [Google Scholar]
- 33.van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., Lloyd-Smith J.O., de Wit E., Munster V.J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maria F.D., Beccaloni E., Bonadonna L., Cini C., Confalonieri E., Rosa G.L., Milana M.R., Testaib E., Scaini F. Minimization of spreading of SARS-CoV-2 via household waste produced by subjects affected by COVID-19 or in quarantine. Sci. Total Environ. 2020;743:140803. doi: 10.1016/j.scitotenv.2020.140803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.WHO . 2020. Water, Sanitation, Hygiene, and Waste Management for the COVID-19 Virus.https://apps.who.int/iris/bitstream/handle/10665/331846/WHO-2019-nCoV-IPC_WASH-2020.3-eng.pdf [Google Scholar]
- 36.Ute P. Technical Guidelines: transport of infectious clinical waste (UN 3291) 2013. https://www.washinhcf.org/wp-content/uploads/2019/03/Guidelines-Transport-of-%20infectious-waste-UN3291.pdf/
- 37.Rhee S.-W. Management of used personal protective equipment and wastes related to COVID-19 in South Korea. Waste Manag. Res. 2020;38(8):820–824. doi: 10.1177/0734242X20933343. [DOI] [PubMed] [Google Scholar]
- 38.Kanemitsu K., Inden K., Kunishima H., Ueno K., Hatta M., Gunji Y., Watanabe I., Kaku M. Does incineration turn infectious waste aseptic? J. Hosp. Infect. 2005;60(4):304–306. doi: 10.1016/j.jhin.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 39.Di Maria F., Bidini G., Lasagni M., Boncompagni A. On time measurement of the efficiency of a waste-to-energy plant and evaluation of the associated uncertainty. Appl. Therm. Eng. 2018;129:338–344. [Google Scholar]
- 40.Kulkarni B.N. Environmental sustainability assessment of land disposal of municipal solid waste generated in Indian cities-A review. Environ Dev. 2020;33:100490. [Google Scholar]
- 41.Ministry of Public Health Recommendation on Disposal of a Used Mask in Situations of Coronavirus Infection (COVID-19) 2020. https://www.anamai.moph.go.th/ewt_dl_link.php?nid=1672 8 September 2020.
- 42.Pollution Control Department . 2020. MONRE Has Given Suggestion for Managing Used Sanitary Masks during the COVID-19 Situation.http://www.pcd.go.th/file/MaskManagement%20COVID-19.pdf [Google Scholar]
- 43.Thampanishvong K., Wibulpolprasert W. 2020. Face Mask Crisis of Another Design.https://tdri.or.th/en/2020/05/face-mask-crisis-of-another-design/ [Google Scholar]
- 44.Rongmeng J., Jianguo J. 2020. Discarded Masks Must Be Properly Disposed of: China Daily Contributors.https://www.straitstimes.com/asia/discarded-masks-must-be-properly-disposed-of-china-daily-contributors?fbclid=IwAR3gYoymzqZ0aQ%200roE58xeNI8uM7Ejswygyh8h9CRtxYnI9YuWgmLqqt6k [Google Scholar]
- 45.Wang J. 2020. How Does Chongqing Dispose of Discarded Masks during the Coronavirus Outbreak?https://www.ichongqing.info/2020/02/04/how-does-chongqing-dispose-of-discarded-masks-during-the-coronavirus%20outbreak/?fbclid=IwAR3ceYhGZkiyrAF2tMowGRlbJY8-b02uhVTwXlPuIK4k05kMsLyjnabnjmA [Google Scholar]
- 46.Bandela D.R. COVID-19: Here is what you should do to safely dispose your used mask. 2020. https://www.downtoearth.org.in/news/waste/covid-19-here-is-what-you-should-do-to-safely-dispose-your-used-mask-71006
- 47.ISWA Q&A: Waste management & COVID-19 in Singapore. 2020. https://www.iswa.org/fileadmin/galleries/0001_COVID/Singapore_Waste_Management_during_Covid19.pdf?fbclid=IwAR3gYoymzqZ0aQ-0roE58xeNI8uM7Ejswygyh8h9CRtxYnI9YuWgmLqqt6k
- 48.Bavani M. 2020. Hazard in Rubbish Bin.https://www.thestar.com.my/metro/metro-news/2020/03/25/hazard-in-rubbish-bin [Google Scholar]
- 49.Taiwan News Taipei City Government to reward those who report mask litterers. 2020. https://www.taiwannews.com.tw/en/news/3909264?fbclid=IwAR3gYoymzqZ0aQ-0roE58xeNI8uM7Ejswygyh8h9CRtxYnI9YuWgmLqqt6k
- 50.Lee W.-C. Mask usage. 2020. https://fightcovid.edu.tw/specific-topics/mask-usage?fbclid=IwAR3ceYhGZkiyrAF2tMowGRlbJY8-b02uhVTwXlPuIK4k05kMsLyjnabnjmA
- 51.Yang L., Yu X., Wu X., Wang J., Yan X., Jiang S., Chen Z. Emergency response to the explosive growth of health care wastes during COVID-19 pandemic in Wuhan, China. Resour. Conserv. Recycl. 2021;164:105074. doi: 10.1016/j.resconrec.2020.105074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Klemeš J.J., Fan Y.V., Tan R.R., Jiang P. Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew. Sustain. Energy Rev. 2020;127:109883. doi: 10.1016/j.rser.2020.109883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sonia A., Kumar R. 2020. The COVID-19 Plastic Pandemic.https://www.nepalitimes.com/banner/the-covid-19-plastic-pandemic/ [Google Scholar]
- 54.Fadare O.O., Okoffo E.D. Covid-19 face masks: A potential source of microplastic fibers in the environment. Sci. Total Environ. 2020;737:140279. doi: 10.1016/j.scitotenv.2020.140279. [DOI] [PMC free article] [PubMed] [Google Scholar]


