Abstract
During the coronavirus disease 2019 (COVID-19) pandemic, the use of telemedicine changed from being an optional way to see patients to becoming a necessity. It has transformed primary, specialty, and mental health services by becoming incorporating into everyday practice. Because allergists have adapted to patient care using telemedicine, use of this technology is likely to continue after COVID-19. In the process of using telemedicine, lessons have been learned. We now offer 10 rules for creating a successful telemedicine practice while also ensuring that quality asthma care is provided.
Key words: Telehealth, Asthma, COVID, Connected health, Digital health, E-consults, Remote, Patient monitoring, m-Health
Abbreviations used: ACT, Asthma Control Test; CMS, Center for Medicare and Medicaid Services; COVID-19, Coronavirus disease 2019; CPT, Current Procedural Terminology; DTC, Direct to consumer; FeNO, Fractional exhaled nitric oxide; FVV, Facilitated virtual visit; HIPAA, Health Insurance Portability and Accountability Act; IMLC, Interstate Medical Licensure Compact; m-Health, Mobile health; RPM, Remote patient monitoring; TM, Telemedicine
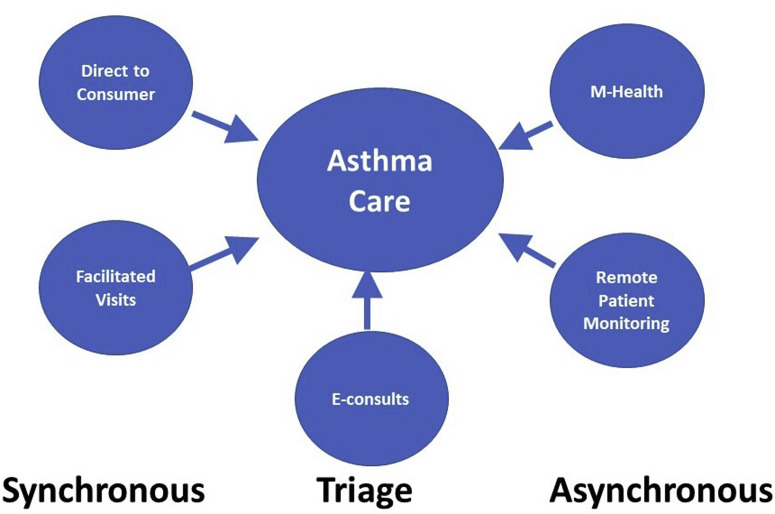
According to the American Telemedicine Association, telemedicine (TM) is the “the remote delivery of health care services and clinical information using telecommunications technology.”1 The use of TM to care for patients with asthma and allergies has increased recently, and its use has accelerated in response to coronavirus disease 2019 (COVID-19). Types of live (or synchronous) TM visits that have been used for asthma care include direct to consumer (DTC) and facilitated virtual visits (FVVs). Asynchronous methods to care for asthma have included remote patient monitoring (RPM) and use of mobile health (m-Health) applications. Asthma is a challenging condition to manage because it presents with varying severities, a multitude of triggers, and variable responsiveness to treatment. TM has been used successfully to improve asthma control, decrease its severity, and provide a better quality of life while improving medication adherence and decreasing use of health care resources.2, 3, 4, 5, 6, 7
Brown and Odenthal8 showed success in improving Asthma Control Test (ACT) scores and FEV% using TM among asthmatics during a 12-month period. However, it was not known how this compared with traditional in-person visits. Using TM, asthma control has been found to be not inferior to in-person visits in outpatient settings.4 , 9 , 10 TM also has demonstrated benefit in helping to improve proper administration of inhaled asthma medication and treatment adherence.11 , 12 A meta-analysis did not show a negative effect of using real-time TM to improve asthma education in school-aged children.13 Furthermore, a recent article of TM care delivered by an asthma specialist (allergist or pulmonologist) and a psychologist in an inner-city school demonstrated improvement in Composite Asthma Severity Index scores and medication adherence measured and reduced health care utilization via a Propeller Health web platform.3
Information and Communication Technology applications also have been helpful for the management of asthma using TM. These include use of internet-based platforms, use of e-mails and text messages, and video chats via computer or other electronic devices (eg, smartphones, tablets).14, 15, 16 Online interactions between providers and patients can be helpful in managing a patient's asthma. One study conducted in Denmark using an internet-based interactive asthma monitoring tool resulted in improvement in asthma symptoms, medication adherence, pulmonary function, and airway hyperresponsiveness.17 However, studies are still needed to show whether asthma telemonitoring with feedback from a health care professional is effective in decreasing the onset of exacerbations, visits to emergency department, or hospital stays.2 The use of traditional instruments with new telemonitoring technologies can be instrumental for improving clinical outcomes. This is important, because traditional instruments for asthma care (eg, written asthma action plans) have shown variable clinical benefit.5 , 7
According to a 2016 AMA survey of practices that use TM by specialty, an average of 15% of practices in all specialties use TM for visits between providers and patients.18 Although the use of TM has been shown to be effective for treating patients with asthma, only 6% of allergy practices used TM, making allergy/immunology the specialty with the lowest adoption rate of any of the surveyed specialties. Specialties with the highest use of TM were radiologists, primarily due to their use of asynchronous store and forward. Other specialties with high TM use included cardiologists who did a lot of RPM and psychiatrists who rely extensively on talk to manage patients. Allergists, who have traditionally relied on skin tests and allergen immunotherapy to manage patients, have not been as quick to adopt TM, though this is likely to change due to COVID-19.
The pathway to creating a successful TM program should include a thorough understanding of the different telehealth options. Providers should ask themselves what their goals are. It should be clear how their asthmatic patients will benefit from these new programs. Also, patient goals need to be incorporated into the program. A successful program will adhere to state laws and ultimately must generate a strong return on investment.
Rules for Starting a Telemedicine Program
The use of TM has increased in part because COVID-19 has encouraged patients and providers to maintain social distancing that reduces the risk of infection. After all, as mentioned in a recent editorial, the only infection that can be transferred using TM is a computer virus.19 Because of the increased need to use virtual visits for patient care, providers have needed to convert to a new technology quickly. To help with this process, we propose the following 10 rules for converting to TM.
Rule 1: understand the different types of telemedicine and use appropriate ones to treat your patients with asthma
Several types of TM can be used to provide care for patients with asthma (Figure 1 ). Depending on the goals of treatment, these can consist of DTC, FVVs, RPM, communication via patient portals, m-Health, and use of E-consults. Each of these can be used to help patients with asthma depending on what is needed. It is important to choose a platform based on whether the visit needs to be synchronous or asynchronous, ongoing or intermittent, and monitored or patient-managed.
Figure 1.
Telemedicine options to improve asthma care. M-Health, Mobile health.
Direct to consumer
During the pandemic, this has become the most commonly used type of TM. With DTC, the patient is located at an originating site (eg, personal residence, school, workplace) and the provider is located at a distant site (eg, hospital, office, provider's home). In a typical scenario, a provider located at his or her office connects to a patient who is located at his or her home using 2-way live video. The patient uses his or her own equipment making it possible for him or her to be seen at his or her home. Therefore, he or she needs to have a smart phone, tablet device, or computer with a video camera and a reliable internet connection.
A physical examination using digital examination equipment is limited to whatever can be observed using the device that the patient has available. Although patients can report their current weight, height, pulse, and respiratory rate, this usually limits the examination to the skin and general impressions of respiratory distress. Blood pressure can be documented if the patient has a blood pressure cuff at home. An example of a physical examination that can be documented using limited equipment is shown in Table I . Such visits generally are limited to evaluation of established patients where a physical examination is not required. For an initial encounter, a limited physical examination can be performed and documented; however, the most common model when seeing a new patient is to bill the patient directly and not to use Current Procedural Terminology (CPT) codes. Some of these requirements have been relaxed during COVID-19; however, the waivers are likely to expire as the pandemic continues.
Table I.
An example of documentation of a physical examination that can be done using limited digital equipment
| Examination: |
|---|
| Vital signs: Weight- Height- Resp Rate- Pulse- |
| General: No apparent distress. Awake, alert, well-appearing. |
| HEENT: Normocephalic and atraumatic. Mucous membranes are moist. No periorbital edema. Facial muscles move symmetrically. |
| Neck: Neck is symmetrical with trachea midline. |
| Eyes: Conjunctiva and eyelids normal bilaterally. Pupils equal and round bilaterally. |
| Sinuses: Patient/guardian was able to touch the face with no tenderness. No frontal or maxillary tenderness. |
| Respiratory: Breathing unlabored, no tachypnea, no nasal flaring, no coughing, use of accessory muscles, chest retractions, unable to speak in complete sentences or prolonged expiratory phase. |
| Cardiovascular: No edema, no pallor, no cyanosis. |
| Abdomen: Nondistended. |
| Skin: No concerning rash or lesions observed on exposed skin. |
| Extremities: Normal range of motion observed. No peripheral edema. |
| Neuro: Mood and behavior appropriate for age. |
| Musculoskeletal: Symmetric and appropriate movements of extremities. |
HEENT, Head, ears, eyes, nose, and throat.
Facilitated virtual visit
Some patients do not have access to the necessary infrastructure (Wi-Fi, smartphone, etc.) for a DTC visit or they have a condition that requires a physical examination. For these patients, an FVV may be needed. To have this type of visit, the patient needs to travel to an accessible location that has digital equipment required to perform a physical examination. In addition to 2-way video equipment, FVVs also require the presence of a telefacilitator and digital examination equipment. The telefacilitator should be trained to operate the video equipment and to use diagnostic equipment so that the provider can properly evaluate the patient. Depending on the type of examination required, equipment may include digital stethoscope, blood pressure cuff, thermometer, scale, otoscope, ophthalmoscope, dermascope, or even ultrasound. This type of visit usually is done synchronously; however, an asynchronous visit for a physical examination to supplement a DTC video visit is also possible.
Remote patient monitoring
RPM involves collecting personal medical data from an individual in one location and electronically transmitting that information to a provider or case worker at a distant site. It has been available in various forms for several decades and its use is now increasing with newer wearable technologies.20 For asthma care, the information may also include home spirometry results, peak flow readings, and monitoring of asthma diaries. The results are forwarded to the asthma provider for interpretation followed by recommendations.
Some key trends in RPM include monitoring the patient's temperature, oxygen saturation, pulmonary function, peak flow, blood pressure/glucose, and weight. Information obtained with a home spirometer is comparable with a standard benchtop-sized commercial spirometer for measuring parameters such as FEV1 and forced vital capacity.21 Once the diagnostic tools are identified, providers need to know about their availability/integration and interoperability and the ease of use for their patient population. Since 2018, Medicare has paid for RPM devices billed under the CPT code 99090. The benefits of using RPM include its convenience and the ability for ongoing continuous monitoring of patient response to treatment.
The use of digital inhalers for real-time monitoring of inhaled medications has the potential to improve adherence and modify behavior by using real-time feedback. The devices use Bluetooth to connect to a smartphone app that stores usage data and can alert the user if any of the programmed parameters are outside of the recommended range. The 2 most studied devices are Propeller (Propeller Health) and the ProAir Digihaler (TEVA USA, Parsippany, NJ). The Digihaler is a digital inhaler with built-in sensors that can detect, record, and store information related to the use of the inhaler and measure inspiratory flow rates (L/min). The initial inhaler contained albuterol; however, another device with an inhaled corticosteroid (fluticasone) is also in development. Digital inhalers have been shown to improve medication adherence22 , 23 and to improve asthma control or symptoms.24, 25, 26 Reduced utilization due to asthma has also been reported.27 , 28
m-Health
If there was a “silver lining” to the COVID-19 pandemic, it is that providers and patients have become familiar with m-Health applications.6 m-Health involves the use of electronic devices to bring about a health change. This can range from patient self-management of asthma using an electronic diary to use of pollen count or air quality information that might trigger asthma symptoms. m-Health does not necessarily require active monitoring by a physician. It is most commonly used to reinforce patient education, provide medication reminders, and appointment reminders.10
In 2020, there were more than 400,000 health care apps available in the app stores; however, very few of them have been shown to accomplish a targeted goal.29 Similarly, numerous types of electronic devices have been used to positively affect asthma outcomes but have not met specified objectives or have not been validated. In fact, apps are not regulated or approved by the Food and Drug Administration unless they are connected to a medical device for a specified purpose.30 However, innovative mobile asthma applications continue to try to improve on traditional asthma resources such as asthma action plans and asthma diaries.
Many apps that claim to improve asthma outcomes have not been reviewed or validated to ensure that they do indeed benefit patients with asthma. In 2013, a Cochrane review found insufficient evidence for the use of an app in routine asthma care.31 One study evaluated an m-Health application that did not decrease emergency department visits, urgent care visits, or hospitalizations.6 Another recent app, ASTHMAXcel, was found to improve asthma education as measured using the Asthma Knowledge Questionnaire. However, the authors concluded that although knowledge scores were increased, better knowledge scores were attained with the human-educator group.32 Despite this, the authors continue to improve on their app using patient engagement strategies, such as periodic updates and gamification for the pediatric population. Another app, the Scripps Asthma Coach, demonstrated improved ACT scores, decreased use of corticosteroids, and improved lung function.33 Many other apps have demonstrated improvement in different aspects of asthma care and potentially lowering the overall cost for asthma care.14 , 24 , 34, 35, 36, 37, 38
E-consults
E-consults have been used successfully to avoid unnecessary or inappropriate consults and can lead to a more efficient use of a specialist's time. E-consults can also be a good source of referrals for asthma specialists. The University of California—San Francisco and San Francisco General Hospital were successful in reducing the numbers of consults in which specialists were unsure of the reason for consultations by almost 50% in medical specialty clinics, and by almost 75% in surgical specialty clinics.39 A service like this would tend to discourage services of low value and make proper use of the specialist's time. One study conducted at Massachusetts General Hospital found that most E-consults can be completed in approximately 10 minutes, and referring providers usually received recommendations within 1 day.40 With the shortage of asthma specialists and the wait time for getting an appointment, E-consults are likely to become a very popular option.
Patients can benefit significantly if community providers use E-consults to triage referral to allergists. Allergists are experts in conditions that require their expertise. As health care transitions to value-based reimbursement, asthma specialists will be incentivized to deliver care-based services that are not redundant or of low value. Specialists can encourage management of low-acuity asthmatics by the primary care provider with the use of E-consults. Because primary care providers can get an answer regarding the appropriateness of a referral in a timely manner, the relationship between the generalist and specialist can be further strengthened.
Rule 2: stay up to date with state and federal telemedicine laws
During the COVID-19 pandemic, there have been almost daily changes in TM laws and regulations. As federal, state, and local regulatory laws and licensure requirements change, providers need to keep up to date. Organizations such as the National Telehealth Policy resource center can provide information regarding current laws and regulations for all 50 states and the District of Columbia.41 Other organizations such as the Joint Commission for Accreditation of Hospitals have agreed to allow hospitals that receive TM services to accept the credentialing and privilege status of providers who practice in another hospital.42 Furthermore, there is no requirement that TM be delineated as a separate privilege. Still, one should always check directly with the patient's health plan to determine its requirements for TM services.
The Center for Medicare and Medicaid Services (CMS) has relaxed guidelines to allow the use of noncertified Health Insurance Portability and Accountability Act (HIPAA)-compliant telehealth tools. Permitted tools included HIPAA-compliant vendors (eg, Zoom for HealthCare, Skype, Doxy.me, GoToMeeting) and non–HIPAA-compliant platforms (eg, Zoom, Teams, FaceTime, What's App, Google Hangout). Some platforms generally not allowed because of security concerns include FaceBook Live, twitch, and TikTok. It is likely that some of non–HIPAA-compliant platforms will no longer be allowed after COVID-19 because they could pose serious security risks.
States laws specify that a provider needs to be licensed in the state where the patient is located. However, The Interstate Medical Licensure Compact (IMLC) allows physicians to practice in a state without a license in that state if the state is a member of the compact agreement.43 Before physicians can participate in the compact, they must designate their State of Principal Licensure, complete an application, and then receive a formal letter of qualification from that state verifying that they meet the compact's strict eligibility requirements. The IMLC currently includes 29 states, the District of Columbia, and the territory of Guam. Other states have pending bills to join the compact that are awaiting passage.
Credentialing and privileging depend on the requirements of the facilities where the physician practices. Still, many insurance companies have specific recommendations for appropriate credentialing requirements. Furthermore, medical boards define what constitutes a proper patient-physician relationship for a telehealth encounter.
Rule 3: pick a platform
Since COVID-19 began, the number of video platform options for TM has increased. Typical platforms are web-based with video conferencing abilities. Providers are now able to connect with their patients almost anywhere if there is an adequate internet connection available. Ideally, platforms should be cloud-based making it easier to provide care from different locations. Simplicity is the key. A platform that can be used with a simple link that avoids the need for downloading an application is more likely to keep your patients satisfied. Because many patients are not digitally literate, some hand holding will be necessary in many cases.
The platform needs to be HIPAA-compliant, easy to use, and reliable with low latency. Some platforms are integrated into a TM environment that includes an electronic health record, whereas others consist of stand-alone video services. Examples of integrated platforms include American Well, Intouch Health/Teladoc Solo, and AMD Connect and Care. Examples of stand-alone platforms include Zoom, Microsoft Teams, Citrix GoToMeeting, Doximity, Polycom RealPresence, Doxy.me, and FaceTime.
Some features to consider when choosing a platform are shown in Table II .44 Examples of commercial platforms include InTouch/Teladoc, American Well, AMD, and Chiron Health. Doxy.me has been very popular during the pandemic due to ease of use. Another popular alternative includes Doximity. Many providers are using Microsoft Teams that is part of Office 365. Because there has been a temporary waiver of strict HIPAA compliance, several platforms are being used when normally they would not be permitted including What's App, Skype, and Zoom.
Table II.
Features to consider when selecting a telemedicine platform
| Feature of platform | Description | Used for which type of TM |
|---|---|---|
| 2-way video | Patient and provider can see and hear each other in real time | Synchronous DTC and facilitated visit |
| Multipresence | More than 1 provider and/or patient can participate at a time | When parents are at a different location than their child To invite a consultant to participate |
| Mobile apps available | Can permit patients and providers to participate in video conferencing using a smart phone or tablet when a computer is not available Permits tracking of biomarkers |
Synchronous DTC and facilitated visit Remote patient monitoring and e-diaries for tracking patient-generated information |
| Screen sharing | Permits providers to show information to patients including test results and instructions Permits patients to show information to providers such as pictures and symptom charts |
Synchronous DTC and facilitated visits |
| Digital examination transmission | Permits output from digital examination equipment to be viewed by a provider Can be used to send pictures and patient data to providers |
Facilitated visits DTC if the patient has examination equipment Store and forward and RPM |
| Integrated environment | The platform is integrated into the provider's electronic health record Permits scheduling of appointments, billing, and other administrative tasks |
Synchronous DTC and facilitated visits |
| HIPAA compliant | Transmits information to and from the provider in a secure manner consistent with HIPAA regulations | Any TM activity should be HIPAA compliant |
DTC, Direct to consumer; HIPAA, Health Insurance Portability and Accountability Act; RPM, remote patient monitoring; TM, telemedicine.
Some questions that should be considered when selecting a platform include:
-
•
Does it support a spike in traffic?
-
•
Are an adequate number of licenses available for all providers who need one?
-
•
How accessible is provider support? Because support can be an issue, we must stress that ease of use is vital, and products need to be simple. Providers do not want to be bogged down with technological issues. TM is a tool that needs to be almost invisible to the user while at the same time allowing good patient care.
Rule 4: build the infrastructure
Before seeing patients by TM, ensure that you have an adequate infrastructure to perform a DTC or FVV. This includes having the necessary equipment and a reliable internet connection. To most efficiently see patients by TM, it helps to use a computer with a double monitor in which one is used to communicate with the patient by video and the other is used for the electronic medical record. If a single monitor is used, it may be necessary to reduce window sizes or to switch from one application to another during the visit, which can reduce the efficiency of documentation. Some electronic medical records have an integrated TM capability so that the video window is embedded in the health information; however, greater monitor screen area is always helpful.
It also helps to use a professional-looking background to do TM. This can consist of an image of an examination room or of an office with bookshelves. Some platforms permit the background to be blurred, whereas others allow for the insertion of an image of a background. The goal is for the virtual consultation room to have a professional atmosphere so that a proper physician-patient relationship is achieved.45
Rule 5: offer telemedicine appointments
Once the TM infrastructure is in place, it is time to offer patients a choice of an in-person visit, a TM visit, or possibly even a telephone visit. Many patients who are used to being seen in-person may prefer to be seen using DTC, particularly if they have experienced it during COVID-19. It helps to ask rather than to assume that they should resume in-person visits once they become available.
After an appointment is made for a DTC visit, the patient should be provided with information about connecting to the visit. An example of this type of information using Microsoft Teams as the DTC platform is shown in Table III . This can be sent via a patient portal or by sending a direct URL link via e-mail. If e-mail is used, it is important to avoid personal health information because e-mail is not HIPAA compliant. Some patient portals can allow patients to schedule either an in-person or DTC visit depending on the provider's availability. The patients should be asked whether they have internet access and equipment to do a video visit during this preplanning phase. If patients do not have that ability, then an in-person visit or possibly a telephone visit should be offered. It also helps to verify the patient's communication preference for future visits. Staff also should update insurance information and pharmacy location during this initial contact.
Table III.
Instructions sent to patients before a meeting using Microsoft Teams
| The following are few steps to be taken before your appointment date/time that are essential: |
| ▪ Download the TEAMS APP to your smart phone/computer (https://teams.microsoft.com/downloads) |
| ▪ Click on the link below if you need assistance. Please choose instructions in language of your choice https://Domain/form |
| ▪ Click on this preregistration link provided, verifying the information on your account https://Domain/form |
| At the time of the visit do the following: |
| ▪ For a video visit, click on the Join Teams Meeting link. This is preferred |
| ▪ If you are having difficulty with the video connection, call the indicated phone number and use the access code to connect |
| ▪ Please keep in mind that this is a virtual meeting room and you may need to wait for the care team just as you would in an in-person setting |
If you plan to see patients both by TM and in-person, you should decide whether to schedule one type of visit in a block of time or whether to mix the 2 types of visit together. There are advantages and disadvantages to each strategy. A disadvantage of scheduling one type of visit per block of time is that the number of TM and in-person visits that you can offer is fixed. If more patients prefer one type of visit, your schedule may not have enough open slots to accommodate them. An advantage is that you do not have to switch from one type of visit to another during a busy clinic as you would if the types were mixed.
It is likely that one type of visit will tend to have a different duration for one type of patient than for another. In general, TM visits tend to be shorter because the visits usually are more problem-focused with less chit chat. Even though less time is spent with each visit, patients usually are as satisfied or more satisfied with TM visits than they are with in-person visits. The best approach may be to see patients using both types of encounter and determine how long each takes. Schedules can then be adjusted for the appropriate amount of time.
Rule 6: get informed consent
Medicaid rules state that the patient must consent to being seen by TM.46 This consent can be obtained either by the referring, consulting, or distant site provider. The requirement for a separate consent specific to TM is due to concerns over health information security and ensuring that the patient fully understands what takes place during a TM encounter. When obtaining consent, it is important to explain what TM is, the expected benefits and possible risks associated with it, and to explain security measures that will be used to protect patient privacy. Patients should also have the option to decline a TM visit, especially if they would prefer an in-person visit instead.
Although rules may vary with each state, most informed consents are valid for 1 year and do not need to be obtained before each visit. Informed consent may be documented either as a written consent or verbal consent. Consent is required both to provide a TM visit and for treatment using TM. Consent forms can be filled out using a patient portal if one is available. Pediatric patients may require consent from parents. Although legally it is necessary to document consent, it is more important for the patient to understand what a TM consult consists of. Sample telehealth informed consent forms can be obtained from the Telehealth Resource Center at http://telehealthresourcecenter.org/.
Rule 7: prepare for the visit in advance
Ideally, you should prepare for a TM visit in the same way that you would prepare for an in-person visit. You should review the patient's asthma history and review lab work, consultation reports, previous images, spirometry, vital signs, hospitalizations, and other data that might affect a patient's asthma status. Information from an e-device (ie, inhaler usage, asthma diary, etc.) should be reviewed before the visit if available.
Rule 8: see the patient
At the beginning of a TM visit, it helps to verify that you can be seen and heard by the patient and that you can see and hear him or her. You should state your location and verify the location of the patient at the start of a visit. Remember, you may see the patient only if he or she is located in a state where you are licensed to practice medicine (see rule 2). If the patient tells you that he or she is located in a state where you are not licensed, you will need to determine whether licensure requirements have been waived for TM in that state. If you are not able to see the patient due to license issues, it may be necessary to reschedule the visit.
When taking a history, you should ask the same questions for a TM visit as for an in-person visit. Remember to look into the camera when talking to the patient and to explain what you are looking at if you need to look away to see the electronic medical record or for another reason. Consider sending questionnaires for standardized instruments such as the ACT electronically to the patient before the visit so that the results are available when the patient is seen. During the visit, results of labs and other types of information can be reviewed with the patient using a screen share option if available.
Current guidelines recommend that patients with asthma should have measurements of pulmonary function such as spirometry or fractional exhaled nitric oxide (FeNO); however, this can be problematic during COVID-19 because these procedures can generate aerosols. In a recent update on COVID-19, the American Academy of Allergy, Asthma, and Immunology concluded that “nebulizer therapy, spirometry, sputum induction and rhinoscopy are all considered high-risk exposure.”47 The American Thoracic Society recommended that “pulmonary function testing be limited to tests that are only essential for immediate treatment decisions and that the type of pulmonary function testing be limited to the most essential tests when possible.”48 One advantage of using TM to treat asthma is that appropriate patients can be encouraged to obtain personal devices that can measure pulmonary function tests such as FEV1 and peak flow without the risk of COVID-19. The results of such home tests can be used to assist management of patients in lieu of office measurements.
The use of asthma action plans and decisions regarding what treatment to recommend does not really change when patients are seen by TM. Allergy testing can be done using in vitro tests. Similarly, measurement of total and specific IgE along with eosinophil levels, both required to determine the optimal biologic to recommend for patients with severe asthma, can be done at any laboratory equipped to perform these tests regardless of how the patient is seen.
Telehealth can be used to care for asthmatic patients who are new or in need of a follow-up visit. However, at times the diagnosis of asthma can be unclear and the patient will need to have an in-person visit to undergo objective measures. The use of office-based testing such as spirometry, oximetry, and FeNO can help to distinguish conditions that mimic asthma. In these cases, the patient will be encouraged to follow up with the asthma specialist in his or her office. Once the diagnosis of asthma is clear via history or previous objective measures, then future visits can be done via TM. Patients on home biologics can then be followed via a virtual visit.
Rule 9: perform a physical examination
One common lesson taught during medical training was to be able to determine whether a patient is well or not well simply by looking at him or her. This principle also applies when observing a patient with asthma by TM. You should be able to determine whether the patient demonstrates any signs of respiratory distress such as nasal flaring, coughing, pallor, use of accessory muscles, cyanosis, chest retractions, unable to speak in complete sentences, and prolonged expiratory phase. At times you may be able to hear wheezing with the proper speakers and microphone. Sound-reduction headphones may improve your ability to hear subtle sounds. If the patient seems unstable or is clinically worsening during the evaluation, he or she should be instructed to call 911 or go immediately to the emergency department. TM is not the proper venue for seeing patients with acute medical conditions that require immediate attention.
Virtual examinations using a facilitated TM platform can be quite simple because objective measures can be attained using digital medical equipment. Peripherals that can assist in the evaluation of an asthmatic include a digital stethoscope with which a patient's lung sounds can be heard and possibly recorded. High-resolution cameras with an otoscope or a dermascope can be used effectively with the help of a trained telefacilitator. Facilitators can also be trained to perform spirometry at the origination site if needed. Some patients might have digital equipment at home such as a blood pressure cuff, pulse oximeter, or thermometer. Although peak flows can be effectively measured at home, home spirometry is also available.21 , 49 Home spirometers can be quite helpful in providing additional objective measures but the cost might be prohibitive for many patients. Furthermore, a respiratory rate can be determined visually.
The patient's medications and pharmacy information should be confirmed by a staff member before the visit with the provider occurs. Medications can be prescribed and renewed at the time of the visit. This can be done either by a picture in picture or a double screen. Although discharge instructions should be described verbally, the patient should be provided with written instructions that can be sent ideally using a patient portal or less ideally via text, e-mail, fax, or by mail to the patient's home.
Rule 10: bill for the encounter
Changes in legislation have allowed for TM encounters to be paid for at parity with in-person visits. Although many health plans paid for TM before COVID-19, it was not necessarily at a rate that was equivalent to an in-person visit. On April 1, 2020, CMS encouraged the use of Place of Service (POS 11) to bill office visit codes 99201-99215 with modifier 95 on every telehealth visit performed with patients via audio-video. This was regardless of where the patient or the providers were located.50 Currently, facilitated, DTC, and even telephonic visits for some insurers can be billed at full parity depending on state regulation and insurance guidelines. However, CMS, Medicaid, and commercial plans have been known to have different guidance on billing. It is important to keep up to date with respect to changes in reimbursement and the use of codes necessary to obtain it.
Sample Workflows
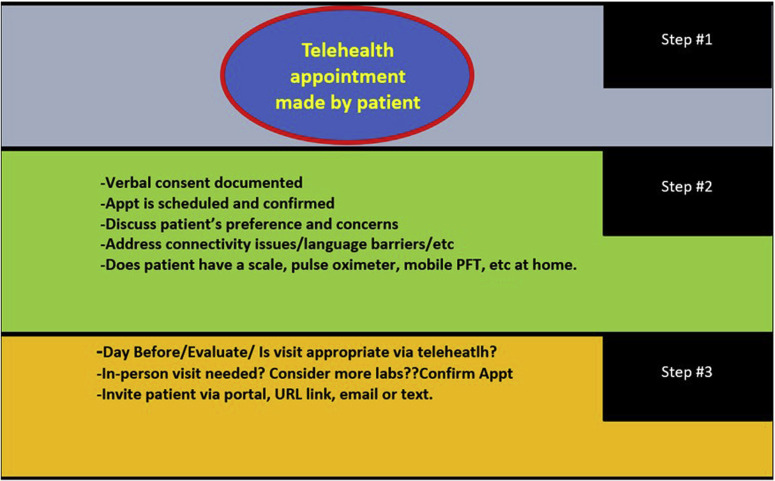
When seeing patients by TM, it helps to create a workflow similar to that used for an in-person visit (Figure 2 ). TM is not meant to change the way you currently see your patients. It has been common practice for workflows to change, staff to be retrained, and job description to change to accommodate these workflows. A simple video capability that has become popular among providers is Doxy.me, especially for private practitioners. A diagnostic TM option that is commonly used is AMD Global. Below are 2 examples of how these platforms can be used in a DTC scenario. Note that these are only examples and that many other platforms have similar capabilities. You should determine your own preferences when evaluating which platform is best for your practice.
Figure 2.
Potential workflow in private practice for a synchronous direct to consumer visit
Example 1: direct to consumer—using Doxy.me
Doxy.me has become a very popular platform for DTC TM during the COVID-19 pandemic. It comes as a free app (an optional paid clinic or professional version is available) that is easy for patients to use because it does not require them to download anything. It also is HIPAA compliant and it offers the option of signing a Business Associate Agreement. You can send a text to the patient only with a paid subscription; however, with the free version, only an e-mail can be sent which is less secure.
Originating site: patient is in his or her personal residence
- Distant site: provider is in his or her medical office
-
(1)Submit the patients e-mail or text them (paid version). You can use the free version and send the link via a free text platform (ie, textfree.us). Patient does not need to download an app.
-
(2)Patient will receive the invite and will need to permit access to his or her microphone and camera.
-
(3)Provider is notified when the patient arrives in a virtual waiting room. If the provider is available, the patient is allowed to enter the visit. If the provider is busy, the patient waits in the virtual waiting room. The provider or an assistant can send a chat to the patient letting him or her know the status of his or her visit.
-
(4)The patient is seen and a limited examination is performed as appropriate.
-
(5)Documentation can be done in the electronic medical record at the same time as the patient is seen using picture in picture or by using a double monitor.
-
(6)Prescriptions are sent to the patient's pharmacy and discharge instructions are sent to the patient.
-
(1)
Example 2: facilitated virtual visit—using a platform that supports digital examination equipment
Intouch Health/Teladoc has become a popular platform for FVVs. The provider interacts either with a stand-alone app or in some cases with an app that is integrated into their electronic medical record. The originating site with the patient usually is a satellite clinic that is closer to where the patient lives than the provider's primary clinical location. The equipment at that location can consist of a TM cart with 2-way video and a remotely controlled camera or any computer can be set up to serve as a TM sending station by installing Intouch/Teladoc's software. Digital examination equipment can be attached to either device.
Originating site: patient is at a satellite clinic
- Distant site: provider is in his or her medical office
-
(1)An appointment is made for an FVV.
-
(2)On the day of the visit, the patient arrives at the clinic.
-
(3)Routine check-in procedures occur. This includes filling out forms, obtaining vital signs, and then taking the patient to a TM sending room.
-
(4)The telefacilitator notifies the provider when the patient is ready to be seen.
-
(5)The patient is seen. A physical examination is performed with the facilitator operating digital examination equipment at the direction of the provider.
-
(6)Documentation can be done in the electronic medical record at the same time as the patient is seen using picture in picture or by using a double monitor.
-
(7)Prescriptions are sent to the patient's pharmacy.
-
(8)Discharge instructions and other information are printed to the origination site for the patient to take with him or her.
-
(9)Blood tests can be obtained in the clinic if venipuncture services are available.
-
(1)
Conclusions
Allergists are in a unique position to care for patients with asthma and allergic disorders. The use of TM offers the ability to see patients at a distance, either in a more convenient clinic or in their personal residence during COVID-19. This should be seen as another option for providing patient care that is more convenient and potentially safer than in-person visits. Although some clinical services should be reserved for in-person visits, many visits can be done using TM.
During this difficult time, TM has been instrumental in providing care to patients who were unable to be seen in-person. We should continue to build on this experience by expecting insurance carriers to continue providing appropriate coverage and payment for TM encounters. Organizations such as Association of American Medical Colleges have been in contact with CMS and state governments to ensure that legislation regarding current TM waivers, including payment and licensure, become permanent.
TM is a tool that can help enhance existing quality metrics and patient outcomes in asthma care. With its current widespread usage, TM data tools are being used to generate TM-specific metrics. Recently, the National Committee for Quality Assurance in its updates to the Healthcare Effectiveness Data and Information Set removed restrictions on the number of telehealth visits to improve the Asthma Medication Ratio.51 Health systems will be able to improve metrics like these to optimize asthma care using various forms of telehealth options. Still, other TM-specific metrics related to asthma are lacking and need to be developed. Metrics on usage, patient satisfaction, quality of technology, and so on for care provided by asthma specialists are needed. The authors of this article envision that organizations that invest in telehealth will have an advantage in improving these quality metrics and outcomes in asthma care. This will enable these organizations to show who really is providing the best care that will translate to the eventual acquisition of a greater market share.
Future research on the delivery of asthma care using TM is needed. Controlled studies are needed to evaluate how the patient-provider relationship is altered when TM is used. In addition, we have encountered that in the South Bronx, many patients with asthma and/or their parents have poor digital literacy and lack of technological infrastructure to perform an adequate TM visit. Additional investigation into ways of using different technologies to achieve these goals is important, keeping in mind that access to the internet is now a social determinant of health. We must also determine what happens to high utilizers of medical care during this pandemic. In particular, it is important to determine whether TM can provide care that is comparable with an in-person visit. After reviewing this information, we will be able to answer the simple question of whether TM can meet the standard of care in the management of asthmatic patients.
Footnotes
No funding was received for this work.
Conflicts of interest: Y. K. Persaud received an honorarium for serving on the advisory board and speaker's bureau for GlaxoSmithKline. He also participates in research with Astra Zeneca that is unrelated to this article. J. M. Portnoy declares no relevant conflicts of interest.
References
- 1.American Telemedicine Association (ATA) Telehealth Basics. https://www.americantelemed.org/resource/why-telemedicine Available from:
- 2.Kew K.M., Cates C.J. Home telemonitoring and remote feedback between clinic visits for asthma. Cochrane Database Syst Rev. 2016:CD011714. doi: 10.1002/14651858.CD011714.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin N.Y., Ramsey R.R., Miller J.L., McDowell K.M., Zhang N., Hommel K. Telehealth delivery of adherence and medication management system improves outcomes in inner-city children with asthma. Pediatr Pulmonol. 2020;55:858–865. doi: 10.1002/ppul.24623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Portnoy J.M., Waller M., De Lurgio S., Dinakar C. Telemedicine is as effective as in-person visits for patients with asthma. Ann Allergy Asthma Immunol. 2016;117:241–245. doi: 10.1016/j.anai.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 5.Sheares B.J., Mellins R.B., Dimango E., Serebrisky D., Zhang Y., Bye M.R. Do patients of subspecialist physicians benefit from written asthma action plans? Am J Respir Crit Care Med. 2015;191:1374–1383. doi: 10.1164/rccm.201407-1338OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stukus D.R., Farooqui N., Strothman K., Ryan K., Zhao S., Stevens J.H. Real-world evaluation of a mobile health application in children with asthma. Ann Allergy Asthma Immunol. 2018;120:395–400.e1. doi: 10.1016/j.anai.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 7.Toelle B.G., Ram F.S. Written individualised management plans for asthma in children and adults. Cochrane Database Syst Rev. 2004:CD002171. doi: 10.1002/14651858.CD002171.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Brown W., Odenthal D. The uses of telemedicine to improve asthma control. J Allergy Clin Immunol Pract. 2015;3:300–301. doi: 10.1016/j.jaip.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 9.Ozuah P.O., Reznik M. The role of telemedicine in the care of children in under-served communities. J Telemed Telecare. 2004;10(Suppl 1):78–80. doi: 10.1258/1357633042614294. [DOI] [PubMed] [Google Scholar]
- 10.Reznik M., Sharif I., Ozuah P.O. Use of interactive videoconferencing to deliver asthma education to inner-city immigrants. J Telemed Telecare. 2004;10:118–120. doi: 10.1258/135763304773391585. [DOI] [PubMed] [Google Scholar]
- 11.Chan D.S., Callahan C.W., Hatch-Pigott V.B., Lawless A., Proffitt H.L., Manning N.E. Internet-based home monitoring and education of children with asthma is comparable to ideal office-based care: results of a 1-year asthma in-home monitoring trial. Pediatrics. 2007;119:569–578. doi: 10.1542/peds.2006-1884. [DOI] [PubMed] [Google Scholar]
- 12.Trosini-Desert V., Lafoeste H., Regard L., Malrin R., Galarza-Jimenez M.A., Amarilla C.E. A telemedicine intervention to ensure the correct usage of inhaler devices. Telemed J E Health. 2020;26:1336–1344. doi: 10.1089/tmj.2019.0246. [DOI] [PubMed] [Google Scholar]
- 13.Culmer N., Smith T., Stager C., Wright A., Burgess K., Johns S. Telemedical asthma education and health care outcomes for school-age children: a systematic review. J Allergy Clin Immunol Pract. 2020;8:1908–1918. doi: 10.1016/j.jaip.2020.02.005. [DOI] [PubMed] [Google Scholar]
- 14.Cingi C., Yorgancioglu A., Cingi C.C., Oguzulgen K., Muluk N.B., Ulusoy S. The "physician on call patient engagement trial" (POPET): measuring the impact of a mobile patient engagement application on health outcomes and quality of life in allergic rhinitis and asthma patients. Int Forum Allergy Rhinol. 2015;5:487–497. doi: 10.1002/alr.21468. [DOI] [PubMed] [Google Scholar]
- 15.Perron B.E., Taylor H.O., Glass J.E., Margerum-Leys J. Information and communication technologies in social work. Adv Soc Work. 2010;11:67–81. [PMC free article] [PubMed] [Google Scholar]
- 16.Poowuttikul P., Seth D. New concepts and technological resources in patient education and asthma self-management. Clin Rev Allergy Immunol. 2020;59:19–37. doi: 10.1007/s12016-020-08782-w. [DOI] [PubMed] [Google Scholar]
- 17.Rasmussen L.M., Phanareth K., Nolte H., Backer V. Internet-based monitoring of asthma: a long-term, randomized clinical study of 300 asthmatic subjects. J Allergy Clin Immunol. 2005;115:1137–1142. doi: 10.1016/j.jaci.2005.03.030. [DOI] [PubMed] [Google Scholar]
- 18.Kane C.K., Gillis K. The use of telemedicine by physicians: still the exception rather than the rule. Health Aff (Millwood) 2018;37:1923–1930. doi: 10.1377/hlthaff.2018.05077. [DOI] [PubMed] [Google Scholar]
- 19.Portnoy J., Waller M., Elliott T. Telemedicine in the era of COVID-19. J Allergy Clin Immunol Pract. 2020;8:1489–1491. doi: 10.1016/j.jaip.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greiwe J., Nyenhuis S.M. Wearable technology and how this can be implemented into clinical practice. Curr Allergy Asthma Rep. 2020;20:36. doi: 10.1007/s11882-020-00927-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fung A.G., Tan L.D., Duong T.N., Schivo M., Littlefield L., Delplanque J.P. Design and benchmark testing for open architecture reconfigurable mobile spirometer and exhaled breath monitor with GPS and data telemetry. Diagnostics (Basel) 2019;9:100. doi: 10.3390/diagnostics9030100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morton R.W., Elphick H.E., Rigby A.S., Daw W.J., King D.A., Smith L.J. STAAR: a randomised controlled trial of electronic adherence monitoring with reminder alarms and feedback to improve clinical outcomes for children with asthma. Thorax. 2017;72:347–354. doi: 10.1136/thoraxjnl-2015-208171. [DOI] [PubMed] [Google Scholar]
- 23.Mosnaim G., Li H., Martin M., Richardson D., Belice P.J., Avery E. A tailored mobile health intervention to improve adherence and asthma control in minority adolescents. J Allergy Clin Immunol Pract. 2015;3:288–290.e1. doi: 10.1016/j.jaip.2014.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Merchant R.K., Inamdar R., Quade R.C. Effectiveness of population health management using the propeller health asthma platform: a randomized clinical trial. J Allergy Clin Immunol Pract. 2016;4:455–463. doi: 10.1016/j.jaip.2015.11.022. [DOI] [PubMed] [Google Scholar]
- 25.Chan Y.Y., Wang P., Rogers L., Tignor N., Zweig M., Hershman S.G. The Asthma Mobile Health Study, a large-scale clinical observational study using ResearchKit. Nat Biotechnol. 2017;35:354–362. doi: 10.1038/nbt.3826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zairina E., Abramson M.J., McDonald C.F., Li J., Dharmasiri T., Stewart K. Telehealth to improve asthma control in pregnancy: a randomized controlled trial. Respirology. 2016;21:867–874. doi: 10.1111/resp.12773. [DOI] [PubMed] [Google Scholar]
- 27.Merchant R., Szefler S.J., Bender B.G., Tuffli M., Barrett M.A., Gondalia R. Impact of a digital health intervention on asthma resource utilization. World Allergy Organ J. 2018;11:28. doi: 10.1186/s40413-018-0209-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou Y., Lu Y., Zhu H., Zhang Y., Li Y., Yu Q. Short-term effect of a smart nebulizing device on adherence to inhaled corticosteroid therapy in Asthma Predictive Index-positive wheezing children. Patient Prefer Adherence. 2018;12:861–868. doi: 10.2147/PPA.S162744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Georgiou M. Developing a healthcare app in 2020: what do patients really want? 2020. https://www.imaginovation.net/blog/developing-a-mobile-health-app-what-patients-really-want/ Available from:
- 30.Himes B.E., Leszinsky L., Walsh R., Hepner H., Wu A.C. Mobile health and inhaler-based monitoring devices for asthma management. J Allergy Clin Immunol Pract. 2019;7:2535–2543. doi: 10.1016/j.jaip.2019.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marcano Belisario J.S., Huckvale K., Greenfield G., Car J., Gunn L.H. Smartphone and tablet self-management apps for asthma. Cochrane Database Syst Rev. 2013;11:CD010013. doi: 10.1002/14651858.CD010013.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hsia B., Mowrey W., Keskin T., Wu S., Aita R., Kwak L. Developing and pilot testing ASTHMAXcel, a mobile app for adults with asthma [published online ahead of print February 19, 2020] J Asthma. [DOI] [PubMed]
- 33.Cook K.A., Modena B.D., Simon R.A. Improvement in asthma control using a minimally burdensome and proactive smartphone application. J Allergy Clin Immunol Pract. 2016;4:730–737.e1. doi: 10.1016/j.jaip.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hui C.Y., Walton R., McKinstry B., Jackson T., Parker R., Pinnock H. The use of mobile applications to support self-management for people with asthma: a systematic review of controlled studies to identify features associated with clinical effectiveness and adherence. J Am Med Inform Assoc. 2017;24:619–632. doi: 10.1093/jamia/ocw143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johnson K.B., Patterson B.L., Ho Y.X., Chen Q., Nian H., Davison C.L. The feasibility of text reminders to improve medication adherence in adolescents with asthma. J Am Med Inform Assoc. 2016;23:449–455. doi: 10.1093/jamia/ocv158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu W.T., Huang C.D., Wang C.H., Lee K.Y., Lin S.M., Kuo H.P. A mobile telephone-based interactive self-care system improves asthma control. Eur Respir J. 2011;37:310–317. doi: 10.1183/09031936.00000810. [DOI] [PubMed] [Google Scholar]
- 37.Ryan D., Price D., Musgrave S.D., Malhotra S., Lee A.J., Ayansina D. Clinical and cost effectiveness of mobile phone supported self-monitoring of asthma: multicentre randomised controlled trial. BMJ. 2012;344:e1756. doi: 10.1136/bmj.e1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tinschert P., Jakob R., Barata F., Kramer J.N., Kowatsch T. The potential of mobile apps for improving asthma self-management: a review of publicly available and well-adopted asthma apps. JMIR Mhealth Uhealth. 2017;5:e113. doi: 10.2196/mhealth.7177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen A.H., Kushel M.B., Grumbach K., Yee H.F., Jr. Practice profile. A safety-net system gains efficiencies through 'eReferrals' to specialists. Health Aff (Millwood) 2010;29:969–971. doi: 10.1377/hlthaff.2010.0027. [DOI] [PubMed] [Google Scholar]
- 40.Phadke N.A., Wolfson A.R., Mancini C., Fu X., Goldstein S.A., Ngo J. Electronic consultations in allergy/immunology. J Allergy Clin Immunol Pract. 2019;7:2594–2602. doi: 10.1016/j.jaip.2019.05.039. [DOI] [PubMed] [Google Scholar]
- 41.Center for Connected Health Policy. Credentialing and privileging. 2020. https://www.cchpca.org/telehealth-policy/credentialing-and-privileging Available from:
- 42.Joint Commission on Accreditation of Healthcare Organizations Final revisions to telemedicine standards. 2012. https://www.jointcommission.org/-/media/tjc/documents/standards/jc-requirements/revisions_telemedicine_standardspdf.pdf?db=web&hash=80DD5BCB3FE622C42BEE956C35611376 Available from: [PubMed]
- 43.2020. Interstate Medical Licensure Compact. A faster pathway to physician licensure.https://www.imlcc.org/a-faster-pathway-to-physician-licensure/ Available from: [Google Scholar]
- 44.Baker J., Stanley A. Telemedicine technology: a review of services, equipment, and other aspects. Curr Allergy Asthma Rep. 2018;18:60. doi: 10.1007/s11882-018-0814-6. [DOI] [PubMed] [Google Scholar]
- 45.Shih J., Portnoy J. Tips for seeing patients via telemedicine. Curr Allergy Asthma Rep. 2018;18:50. doi: 10.1007/s11882-018-0807-5. [DOI] [PubMed] [Google Scholar]
- 46.Center for Connected Health Policy Informed consent. 2020. https://www.cchpca.org/telehealth-policy/informed-consent Available from:
- 47.American Academy of Allergy, Asthma & Immunology . 2020. An update on COVID-19 for the practicing allergist/immunologist.https://education.aaaai.org/resources-for-a-i-clinicians/Update-for-AI_COVID-19 Available from: [Google Scholar]
- 48.McCormack M., Kaminsky D. Pulmonary function laboratories: advice regarding COVID-19. 2020. https://www.thoracic.org/professionals/clinical-resources/disease-related-resources/pulmonary-function-laboratories.php Available from:
- 49.Gibson P.G., Powell H., Coughlan J., Wilson A.J., Abramson M., Haywood P. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev. 2003;1:CD001117. doi: 10.1002/14651858.CD001117. [DOI] [PubMed] [Google Scholar]
- 50.Centers for Medicare & Medicaid Services CY 2020 Physician Fee Schedule Final Rule. 2020. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PFSlookup Available from:
- 51.National Committee on Quality Assurance Taskforce on Telehealth Policy (TTP): findings and recommendations. https://www.ncqa.org/programs/data-and-information-technology/telehealth/taskforce-on-telehealth-policy/taskforce-on-telehealth-policy-ttp-findings-and-recommendations/ Available from: