Abstract
Background
Heat exposure, which will increase with global warming, has been linked to increased risk of a range of types of cause-specific hospitalizations. However, little is known about socioeconomic disparities in vulnerability to heat. We aimed to evaluate whether there were socioeconomic disparities in vulnerability to heat-related all-cause and cause-specific hospitalization among Brazilian cities.
Methods and findings
We collected daily hospitalization and weather data in the hot season (city-specific 4 adjacent hottest months each year) during 2000–2015 from 1,814 Brazilian cities covering 78.4% of the Brazilian population. A time-stratified case-crossover design modeled by quasi-Poisson regression and a distributed lag model was used to estimate city-specific heat–hospitalization association. Then meta-analysis was used to synthesize city-specific estimates according to different socioeconomic quartiles or levels. We included 49 million hospitalizations (58.5% female; median [interquartile range] age: 33.3 [19.8–55.7] years). For cities of lower middle income (LMI), upper middle income (UMI), and high income (HI) according to the World Bank’s classification, every 5°C increase in daily mean temperature during the hot season was associated with a 5.1% (95% CI 4.4%–5.7%, P < 0.001), 3.7% (3.3%–4.0%, P < 0.001), and 2.6% (1.7%–3.4%, P < 0.001) increase in all-cause hospitalization, respectively. The inter-city socioeconomic disparities in the association were strongest for children and adolescents (0–19 years) (increased all-cause hospitalization risk with every 5°C increase [95% CI]: 9.9% [8.7%–11.1%], P < 0.001, in LMI cities versus 5.2% [4.1%–6.3%], P < 0.001, in HI cities). The disparities were particularly evident for hospitalization due to certain diseases, including ischemic heart disease (increase in cause-specific hospitalization risk with every 5°C increase [95% CI]: 5.6% [−0.2% to 11.8%], P = 0.060, in LMI cities versus 0.5% [−2.1% to 3.1%], P = 0.717, in HI cities), asthma (3.7% [0.3%–7.1%], P = 0.031, versus −6.4% [−12.1% to −0.3%], P = 0.041), pneumonia (8.0% [5.6%–10.4%], P < 0.001, versus 3.8% [1.1%–6.5%], P = 0.005), renal diseases (9.6% [6.2%–13.1%], P < 0.001, versus 4.9% [1.8%–8.0%], P = 0.002), mental health conditions (17.2% [8.4%–26.8%], P < 0.001, versus 5.5% [−1.4% to 13.0%], P = 0.121), and neoplasms (3.1% [0.7%–5.5%], P = 0.011, versus −0.1% [−2.1% to 2.0%], P = 0.939). The disparities were similar when stratifying the cities by other socioeconomic indicators (urbanization rate, literacy rate, and household income). The main limitations were lack of data on personal exposure to temperature, and that our city-level analysis did not assess intra-city or individual-level socioeconomic disparities and could not exclude confounding effects of some unmeasured variables.
Conclusions
Less developed cities displayed stronger associations between heat exposure and all-cause hospitalizations and certain types of cause-specific hospitalizations in Brazil. This may exacerbate the existing geographical health and socioeconomic inequalities under a changing climate.
In this nationwide cohort study, Rongbin Xu and colleagues investigate heat and hospitalisations in cities of different socioeconomic development.
Author summary
Why was this study done?
Heat exposure is associated with increases in mortality and morbidity, but vulnerability to heat is not evenly distributed.
It remains uncertain whether the magnitude of heat impacts on all-cause and cause-specific hospitalizations is associated with local socioeconomic characteristics.
What did the researchers do and find?
We performed case-crossover analyses based on a nationwide dataset with 49 million hospitalizations in the hot season during 2000–2015 in 1,814 Brazilian cities.
We found that less developed cities showed higher increased all-cause and cause-specific hospitalization than more developed cities when exposed to the same temperature rise during the hot season.
These inter-city socioeconomic disparities in associations of heat with health outcomes were particularly notable for hospitalizations of children and adolescents, and for hospitalizations due to ischemic heart disease, asthma, pneumonia, renal diseases, mental health conditions, and neoplasms.
What do these findings mean?
Increasing heat exposure along with global warming could be a potential driver for exacerbating inter-city health inequalities.
More attention should be paid to less developed cities in Brazil to tackle the morbidity burden of heat exposure, in order to promote health equity under global warming.
Introduction
Climate change is a major health threat in the 21st century via many pathways, including causing more heat-related mortality or morbidity [1]. Globally, although people living in low- and middle-income countries bear less responsibility for the global warming, they are actually more affected by temperature rise than residents in high-income countries [1]. Climate change has been viewed as a potential driver for exacerbating inequality. However, the modification effect of regional socioeconomic status (SES) on the heat–mortality association remains uncertain [2]. Some studies found that cities or areas with lower SES (e.g., lower urbanization [proportion of urban people], household income, education, or gross domestic product [GDP] per capita) tended to show stronger heat–mortality associations [3–9]. These associations mainly mirrored the residents’ lower adaptation capacity and higher sensitivity to heat exposure [3–9]. In contrast, other studies found that more urbanized or developed areas showed stronger heat–mortality associations [10,11]. They attributed this phenomenon to the urban heat island (UHI) effect [10,11], i.e., that people living in urbanized settings tend to experience higher temperatures due to the great thermal-storage capacity of heavily engineered environments, poor ventilation, and localized heat sources (e.g., vehicles, air conditioners) [12]. There are also some studies that found no significant modification effect of local SES on heat–mortality associations [13–16].
In addition to the conflicting findings, some limitations of previous studies should be noticed. First, the number of locations was often limited (the largest study included 340 cities [10]), which may restrict the statistical power of these studies. Second, most studies were conducted in developed countries; evidence from developing countries was relatively rare. Third, most studies only focused on heat–mortality associations [3–11,13–16], while few of them addressed inequality in heat–morbidity (e.g., hospitalization, emergency department visit) associations. The existing heat–morbidity studies also showed inconsistent findings with respect to the modification effect of regional SES [17–20], and they also had a limited number of locations (up to 158 locations [18]). Finally, most previous studies only focused on all-cause or cardiovascular mortality or morbidity; little is known about inequality in other specific potentially heat-related conditions (e.g., renal diseases, diabetes, mental illness) [21].
In this study, we aimed to evaluate whether city-level heat–hospitalization (both all-cause and cause-specific) associations are modified by local socioeconomic level (literacy rate, urbanization, average household income, and GDP per capita), using a national hospitalization dataset from Brazil during 2000–2015.
Methods
This time-stratified case-crossover study is reported following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement (see S1 STROBE Checklist). We performed all the data analyses according to a prospective analysis plan (S1 Text). Following feedback during peer review, we made some modifications to the analysis plan, as described in S1 Text.
Data collection
The hospitalization data and meteorological data sources have been described in detail in our previous publications [22–24]. Briefly, we collected all-cause hospitalization data from the Brazilian Unified Health System between 1 January 2000 and 31 December 2015. We included 1,814 cities located in 5 regions (north, northeast, central west, southeast, and south) with complete data for the entire 16 years, which covered 78.4% of the Brazilian population. In this study, a “city” (also known as a “municipality” in Brazil) refers to an administrative area with an officially defined boundary under the level of Brazilian states. Each city covers all urban and rural areas in its administrative area. The 16-year average population size of the 1,814 cities during 2000–2015 ranged from 8,014 to 11,048,690, with a median (IQR) of 29,814 (19,859 to 57,484). Generally, the population size of most cities (1,577 cities, 87.0%) was less than 100,000 (Fig A in S2 Text). The hospitalization dataset recorded sex, age, date of each admission, and the code of primary diagnosis according to the 10th revision of the International Classification of Diseases (ICD-10). According to previous reviews on heat and morbidity [21], we selected hospitalizations due to 16 specific causes, including all cardiovascular diseases, ischemic heart disease, heart failure, heart rhythm disturbances, cerebrovascular diseases, stroke, peripheral vascular disease, all respiratory diseases, chronic obstructive pulmonary disease (COPD), asthma, pneumonia, diabetes, renal diseases, mental health conditions, neoplasms, and heat illness (see their ICD-10 codes in Table A in S2 Text). This study was approved by the Monash University Human Research Ethics Committee, and individual consent was exempted because we used anonymized data.
City-specific daily mean temperatures were sourced from a 0.25° × 0.25° Brazilian meteorological dataset [25]. In order to estimate the association between hospitalization and heat exposure, we restricted our analyses to the hottest 4 consecutive months (hot season) for each city each year during the study period [26]. For each city, the hottest 4 consecutive months (e.g., November, December, January, February) were selected according to the average daily mean temperature of each specific month during 2000–2015 (e.g., the average temperature of all Januaries during the 16 years). With this method, the months of hot season held constant for a specific city during these years.
City-level socioeconomic levels were represented by 16-year (2000–2015) average literacy rate of people aged 15 years or above, 16-year average urbanization rate (proportion of urban population), average monthly household income per capita in 2010, and 16-year average GDP per capita. City-level literacy rate, urbanization rate, and population size came from the Brazilian Census 2000 and 2010; the data gaps for other years were filled by linear interpolation. City-level household income measures from the Brazilian Census 2000 and 2010 were not comparable due to different statistical criteria. We chose the latter because 2010 was in the middle of our study period; thus, the 2010 value tended to be a better surrogate of the 16-year average than the 2000 value. City-level GDP per capita for every year during 2000–2015 was reported by the Brazilian Institute of Geography and Statistics (BIGS). We adjusted all GDP per capita and household income data to 2015 US dollars, according to the Consumer Price Index during 2001–2015 and the average exchange rate in 2015. From the Brazilian Census 2010, we also collected the percentages of young population (0–19 years) and elderly population (60 years or above), as an indicator of population age structure. All these socioeconomic and demographic data were downloaded from the BIGS official website [23]. We then stratified the 1,814 cities into 4 groups (Q1–Q4) according to the quartiles (from the lowest to the highest quartile) of each socioeconomic indicator. We also classified the cities into lower middle income (LMI, GDP per capita: US$1,146–US$4,035), upper middle income (UMI, US$4,036–US$12,475), and high income (HI, >US$12,475) according to the World Bank’s 2015 standard. Because there was only 1 city with GDP per capita less than US$1,146 (US$978), we simply classified it as LMI.
Statistical analysis
We used a 2-stage analysis to quantify the associations between heat exposure and risk of all-cause and cause-specific hospitalization [23]. In the first stage, we used a time-stratified case-crossover design to evaluated the heat–hospitalization association for each city [27]. Quasi-Poisson regression with a distributed lag model was used to estimate the city-specific association with the equation below [23]:
| (1) |
where Yit represented the daily counts of hospitalization in city i on day t; α was the intercept; β, γ, and δ were the coefficients; and εit was the residual error. Stratait was a stratum variable combining year and calendar month to adjust for long-term trend and inter-month seasonal variations. DOWit was a categorical variable to adjust for hospitalization variation within 1 week. Holidayit was a binary variable (public holiday or not) to adjust for potential impacts of public holidays on hospitalization. cb(Tempit) was a 2-dimensional (exposure–response dimension and lag–response dimension) cross-basis function to model the lagged associations of daily mean temperature with hospitalizations. In each dimension, a specific smoothing function (e.g., linear function, natural cubic spline) can be used to define the shape of the relationship [26,28]. According to our preliminary analyses described before [23], we used a linear function for the temperature–response dimension, and a natural cubic spline with 3 degrees of freedom for the lag–response dimension along 0–7 lag days.
In the second stage, we pooled the city-specific estimates for all cities or cities in different socioeconomic groups (Q1–Q4 of each socioeconomic indicator, or classification according to the World Bank), using a random effect meta-analysis with maximum likelihood estimation [29]. This provided us a pooled estimation of the heat–hospitalization association at the national level and within different socioeconomic levels. Based on 1,814 city-specific effect estimates, we used random effect meta-regression with each socioeconomic variable (including literacy rate, urbanization rate, household income, and log-transformed GDP per capita) as the only meta-predictor to test whether the city-level heat–hospitalization association was significantly modified by each city-level socioeconomic variable. To capture any potential nonlinearity in the meta-regression, we tried to add each socioeconomic variable to the meta-regression model as a natural cubic spline function with 2 to 4 degrees of freedom. However, the Bayesian information criterion (BIC) values of nonlinear models were generally larger than or close to the BIC value of the linear meta-regression model (Table B in S2 Text). This suggested that the linear model outperformed the nonlinear models in the meta-regression; thus, we used the linear meta-regression model throughout the analyses. We stratified all the analyses above by sex, 4 age groups (0–19 years, 20–39 years, 40–59 years, 60 years or above), and 16 specific causes of hospitalization.
The heat–hospitalization association was reported as the cumulative relative risk (RR) of hospitalization (with 95% CIs) over lag 0–7 days associated with every 5°C increase in daily mean temperature during the hot season. The increased hospitalization risk associated with every 5°C increase in daily mean temperature was then calculated as 100% × (RR − 1).
We performed 2 sensitivity analyses to test the robustness of our results. First, we tested whether the socioeconomic disparities in heat vulnerability remained significant after adjusting for potential confounders in the meta-regression. For each socioeconomic indicator in the random effect meta-regression model, we adjusted for city-specific mean temperature in the hot seasons, temperature range (maximum temperature minus minimum temperature in the hot seasons), and the ratio of young population (0–19 years) and elderly population (60 years or above), as an indicator of population structure. Second, we repeated the above analyses based on 1,723 cities with relatively small population sizes (ranging from 8,014 to 243,270), after excluding cities with population sizes larger than the 95th percentile of all 1,814 cities. Compared to large cities, the city-level socioeconomic indicators in those small cities could be more representative of the residents’ true socioeconomic situations.
All data analyses were performed with R software (version 3.5.1). The “dlnm” and “mvmeta” packages were used for the first-stage and second-stage analyses, respectively [28,29].
Results
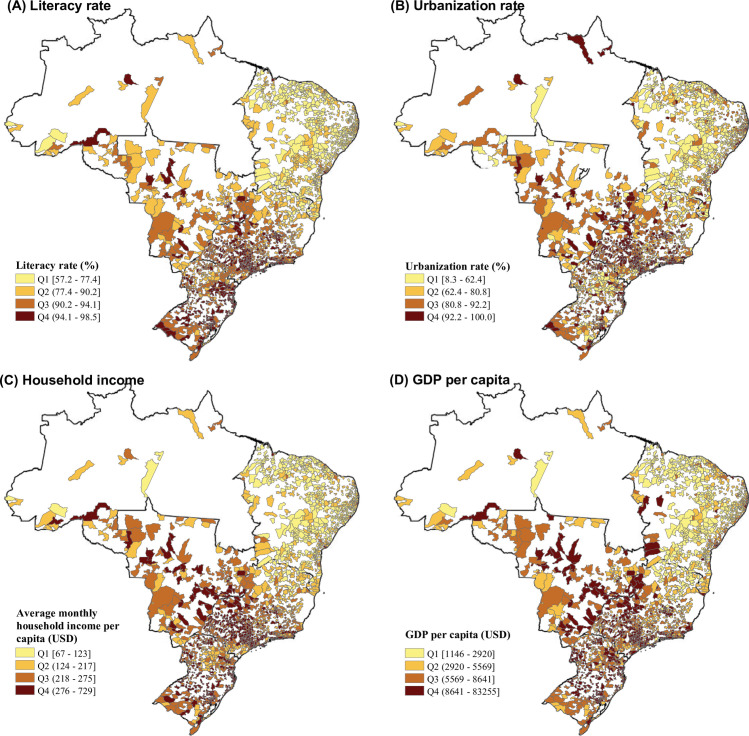
A total of 49,145,997 hospital admissions (58.5% female) from 1,814 Brazilian cities in the hot seasons between 2000 and 2015 were included in the analyses. The median age of the included hospitalized patients was 33.3 years, with an IQR of 19.8–55.7 years. The case number and age distribution of hospitalizations due to 16 specific causes are reported in Table A in S2 Text. Briefly, hospitalizations due to cardiovascular diseases, COPD, and diabetes were dominated by elderly people, while hospitalizations for pneumonia, asthma, and heat illness were dominated by children and adolescents. The daily mean temperature had a median value of 25.7°C (IQR: 23.9–27.5°C; minimum–maximum: 11.4–33.1°C) in the hot seasons during 2000–2015 in the 1,814 cities, ranging from 23.9°C (IQR: 22.1–25.5°C) in the southeast to 28.0°C (IQR: 27.0–28.8°C) in the northeast. The climatic, demographic, and socioeconomic indicators were correlated with each other (Table C in S2 Text). The northern cities were hotter than the southern cities, while the latter generally had a higher socioeconomic level (higher literacy rate, urbanization rate, household income, or GDP per capita) and older population structure than the former. There were huge socioeconomic variations across the 1,814 cities. For example, the 16-year average GDP per capita varied from US$978 to US$83,307 (Table 1; Fig 1; Fig B in S2 Text).
Table 1. Socioeconomic, demographic, and climatic characteristics of 1,814 included cities in Brazil and the hospitalization cases during the hot season, 2000–2015.
| Characteristic | Region | National | ||||
|---|---|---|---|---|---|---|
| North | Northeast | Central west | Southeast | South | ||
| Number of cities | 28 | 662 | 128 | 622 | 374 | 1,814 |
| Population coverage (%) | 26.3 | 78.0 | 80.7 | 87.0 | 83.2 | 78.4 |
| City characteristics | ||||||
| Literacy rate of people aged 15 or above (%)* | 88.1 (83.8–90.8) | 72.9 (68.2–78.0) | 89.0 (87.3–91.1) | 92.5 (90.0–94.3) | 93.5 (90.7–95.5) | 89.1 (75.5–93.3) |
| Urbanization rate (%)* | 70.5 (62.7–86.7) | 60.6 (47.7–75.8) | 84.9 (78.1–91.6) | 89.7 (78.7–95.9) | 83.7 (70.5–92.0) | 80.8 (60.7–91.5) |
| Average monthly household income per capita (USD)* | 183 (143–250) | 112 (98–135) | 245 (218–273) | 258 (216–298) | 271 (232–318) | 217 (123–275) |
| GDP per capita (USD)* | 4,077 (3,063–5,309) | 1,982 (1,594–2,748) | 5,551 (3,880–7,518) | 5,739 (4,028–8,034) | 6,602 (4,989–8,709) | 4,406 (2,205–6,878) |
| Percentage of population aged 0–19 years* | 39.9 (36.2–46.8) | 37.7 (35.6–40.3) | 33.6 (31.8–36.3) | 30.6 (28.7–32.9) | 31.0 (29.2–33.4) | 33.4 (30.2–37.5) |
| Percentage of population aged 60 years or above* | 6.9 (6.3–7.7) | 10.7 (9.3–12.3) | 9.4 (7.7–11.3) | 12.5 (10.7–14.0) | 12.1 (10.3–13.9) | 11.5 (9.7–13.3) |
| Daily mean temperature in the hot seasons (°C)* | 26.5 (25.1–27.9) | 28.0 (27.0–28.8) | 27.4 (26.1–28.8) | 23.9 (22.1–25.5) | 24.6 (23.2–25.9) | 25.7 (23.9–27.5) |
| Daily mean temperature in the hot seasons (°C), minimum–maximum | 18.2–33.3 | 18.1–33.6 | 14.3–33.5 | 14.2–32.1 | 9.2–31.8 | 11.4–33.1 |
| Hospitalization characteristics | ||||||
| Number of cases | 1,271,435 | 13,823,251 | 3,847,427 | 22,077,029 | 8,126,855 | 49,145,997 |
| Female, n (%) | 815,026 (64.1) | 8,647,071 (62.6) | 2,281,986 (59.3) | 12,563,961 (56.9) | 4,604,677 (56.7) | 28,912,721 (58.8) |
| Age, n (%) | ||||||
| 0–19 years | 426,200 (33.5) | 4,123,994 (29.8) | 1,032,481 (26.8) | 4,860,233 (22.0) | 1,847,815 (22.7) | 12,290,723 (25.0) |
| 20–39 years | 512,158 (40.3) | 4,996,318 (36.1) | 1,351,131 (35.1) | 7,125,403 (32.3) | 2,472,683 (30.4) | 16,457,693 (33.5) |
| 40–59 years | 175,960 (13.8) | 2,337,994 (16.9) | 763,057 (19.8) | 5,152,763 (23.3) | 1,880,986 (23.1) | 10,310,760 (21.0) |
| ≥60 years | 146,161 (11.5) | 2,199,275 (15.9) | 651,016 (16.9) | 4,584,110 (20.8) | 1,787,342 (22.0) | 9,367,904 (19.1) |
For daily mean temperature, the median (IQR), minimum, and maximum were based on all city-specific daily observations for the 1,814 cities in the hot seasons between 2000 and 2015. Both GDP per capita and household income have been adjusted to 2015 USD according the Consumer Price Index. The literacy rate, urbanization rate, and GDP per capita were the 16-year average values during 2000–2015. Household income and population structure were sourced from the 2010 census of Brazil. The hot season was defined as the city-specific 4 adjacent hottest months each year. The minimum and maximum temperature were represented by the 0.1% and 99.9% quantile of daily mean temperature during the study period, in order to minimize the effects of some extreme observations.
*Median (IQR) of 1,814 cities.
GDP, gross domestic product; IQR, interquartile range; USD, United States dollars.
Fig 1. Mapping the average socioeconomic characteristics during 2000–2015 in 1,814 Brazilian cities.
Literacy rate (A), urbanization rate (B), household income (C), and GDP per capita (D). Both GDP per capita and household income were adjusted to 2015 USD according to the Consumer Price Index. The literacy rate, urbanization rate, and GDP per capita were the 16-year average values during 2000–2015. Household income was sourced from the 2010 census of Brazil. Q1–Q4 were the 4 quartiles from the lowest to the highest. The base map of this figure was downloaded from the Brazilian Institute of Geography and Statistics (https://www.ibge.gov.br/); the base map was free and open-access. GDP, gross domestic product; USD, United States dollars.
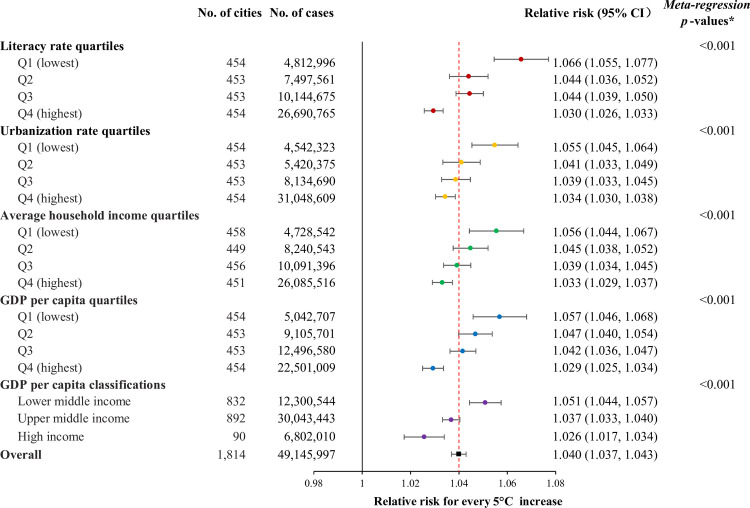
At the national level, we estimated that every 5°C increase in daily mean temperature in the hot season was associated with a 4.0% (95% CI 3.7%–4.3%; RR = 1.040, 95% CI 1.037–1.043, P < 0.001) increase in all-cause hospitalization. This association showed a clear strengthening with decreases in literacy rate, urbanization rate, average household income, and GDP per capita (Fig C in S2 Text). The RR (95% CI) for cities of LMI, UPI, and HI according to the World Bank’s classification was 1.051 (1.044–1.057, P < 0.001), 1.037 (1.033–1.040, P < 0.001), and 1.026 (1.017–1.034, P < 0.001) (meta-regression P value < 0.001), respectively (Fig 2).
Fig 2. The association between heat exposure (for every 5°C increase in daily mean temperature) and all-cause hospitalization during lag 0–7 days, stratified by socioeconomic level.
Q1–Q4 represent 4 quartiles from the lowest to the highest. GDP per capita classifications were based on the World Bank’s 2015 standard. *The meta-regression P values were derived from the meta-regressions modeling the 1,814 city-specific effect estimates against the city-level literacy rate, urbanization rate, average household income, and log(GDP per capita) separately (see Fig C in S2 Text). CI, confidence interval; GDP, gross domestic product.
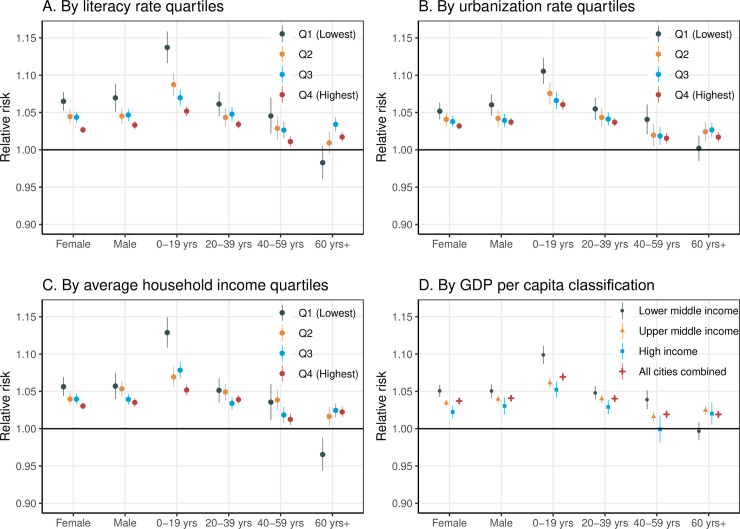
The inter-city socioeconomic disparities in heat–hospitalization association were consistent between females and males, but especially significant in the young age group (0–19 years) (increased hospitalization risk [95% CI]: 9.9% [8.7% to 11.1%], P < 0.001, in LMI cities versus 5.2% [4.1% to 6.3%], P < 0.001, in HI cities; meta-regression P value <0.001) (Fig 3; Table D in S2 Text).
Fig 3. The association between heat exposure (for every 5°C increase in daily mean temperature) and hospitalization during lag 0–7 days, stratified by socioeconomic level, sex, and age group.
Literacy rate (A), urbanization rate (B), household income (C), and GDP per capita (D). Q1–Q4 represent 4 quartiles from the lowest to the highest. GDP per capita classifications were based on the World Bank’s 2015 standard. CI, confidence interval; GDP, gross domestic product.
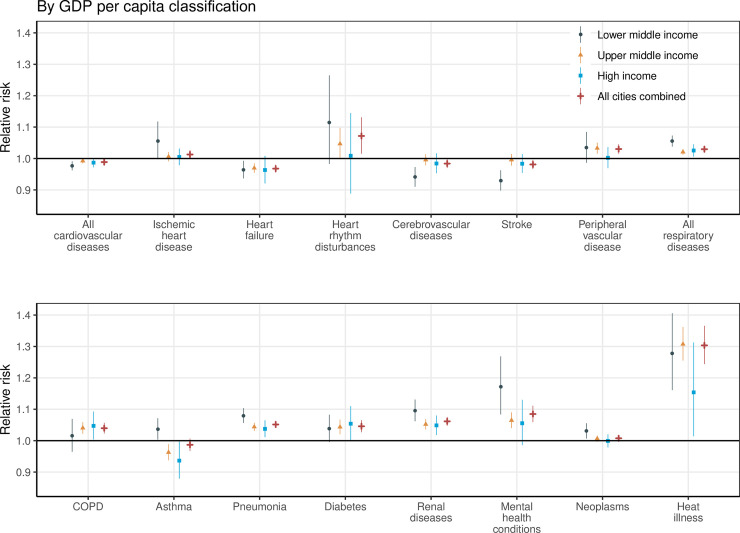
At a national level, with every 5°C increase in daily mean temperature during the hot season, the increased cause-specific hospitalization risk was 30.3% (95% CI 24.4%–36.6, P < 0.001) for heat illness, 8.5% (95% CI 5.9%–11.1%, P < 0.001) for mental health conditions, 7.2% (95% CI 1.5%–13.1%, P = 0.012) for heart rhythm disturbances, 6.2% (95% CI 4.8%–7.5%, P < 0.001) for renal diseases, 5.2% (95% CI 4.1%–6.2%, P < 0.001) for pneumonia, 4.6% (95% CI 2.7%–6.5%, P < 0.001) for diabetes, 4.0% (95% CI 2.3%–5.7%, P < 0.001) for COPD, 3.0% (95% CI 1.5%–4.5%, P < 0.001) for peripheral vascular disease, and 3.0% (95% CI 2.2%–3.7%, P < 0.001) for all respiratory diseases as a whole. The same temperature rise was associated with a reduction in hospitalizations for heart failure (−3.2%, 95% CI −4.5% to −2.0%, P < 0.001), cerebrovascular diseases (−1.6%, 95% CI −3.0% to −0.2%, P = 0.028), and stroke (−1.9%, 95% CI −3.4 to −0.4, P = 0.013), and cardiovascular diseases as a whole (−1.1%, 95% CI −1.8% to −0.5%, P < 0.001). Non-significant heat–hospitalization associations were found for hospitalizations due to neoplasms, asthma, and ischemic heart disease (Fig 4; Table D in S2 Text).
Fig 4. The association between heat exposure (for every 5°C increase in daily mean temperature) and cause-specific hospitalization during lag 0–7 days, stratified by GDP per capita classification.
GDP per capita classifications were based on the World Bank’s 2015 standard. COPD, chronic obstructive pulmonary disease; GDP, gross domestic product.
The inter-city socioeconomic disparities in heat–hospitalization association were evident for hospitalizations due to certain diseases, including ischemic heart disease (increase in cause-specific hospitalization risk with every 5°C increase [95% CI]: 5.6% [−0.2% to 11.8%], P = 0.060, in LMI cities versus 0.5% [−2.1%–3.1%], P = 0.717, in HI cities; meta-regression P value = 0.029), asthma (3.7% [0.3%–7.1%], P = 0.031, versus −6.4% [−12.1% to −0.3%], P = 0.041; meta-regression P value < 0.001), pneumonia (8.0% [5.6%–10.4%], P < 0.001, versus 3.8% [1.1%–6.5%], P = 0.005; meta-regression P value = 0.001), renal diseases (9.6% [6.2%–13.1%], P < 0.001, versus 4.9% [1.8%–8.0%], P = 0.002; meta-regression P value = 0.073), mental health conditions (17.2% [8.4%–26.8%], P < 0.001, versus 5.5% [−1.4% to 13.0%], P = 0.121; meta-regression P value = 0.034), and neoplasms (3.1% [0.7%–5.5%], P = 0.011, versus −0.1% [−2.1% to 2.0%], P = 0.939; meta-regression P value = 0.001) (Fig 4; Table D in S2 Text). The inter-city socioeconomic disparity patterns by sex, age, and specific cause of hospitalization were generally similar when stratifying the analyses by other socioeconomic indicators (literacy rate, urbanization rate, or household income) (Figs D–F and Tables E–H in S2 Text).
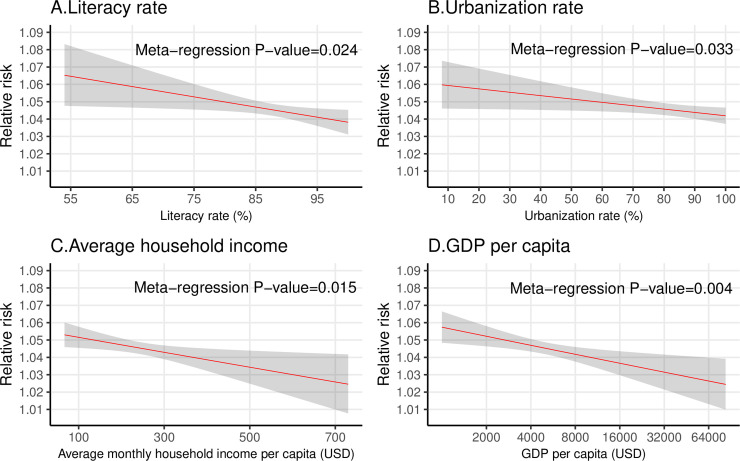
After adjusting for city-level mean temperature, temperature range, and population structure in meta-regression, the city-specific RRs were still negatively associated with literacy rate (meta-regression P value = 0.024), urbanization rate (meta-regression P value = 0.033), average family income (meta-regression P value = 0.015), and log(GDP per capita) (meta-regression P value = 0.004) (Fig 5). The modifying effects of the 4 socioeconomic indicators on city-specific heat–hospitalization association changed minimally after excluding cities with population sizes larger than the 95th percentile of the 1,814 cities (Figs G and H in S2 Text).
Fig 5. The relationship between city-level socioeconomic factors and the magnitude of heat–hospitalization association among 1,814 cities, adjusting for potential confounders.
Literacy rate (A), urbanization rate (B), household income (C), and GDP per capita (D). The RR represents the association between heat exposure (for every 5°C increase in daily mean temperature) and hospitalization during lag 0–7 days. The shadowed area represents the 95% confidence interval. The relationships between RR and the 4 socioeconomic indicators were fitted separately by meta-regression, adjusting for city-specific mean temperature, temperature range, and the ratio of elderly population (≥60 years) and young population (0–19 years). The RRs were estimated as the values when city-specific mean temperature, temperature range, and the ratio of elderly population and young population were at the average level of the 1,814 cities. The x-axis of (D) is on the log scale, because we added log(GDP per capita) rather than GDP per capita to the meta-regression model. GDP, gross domestic product; RR, relative risk; USD, United States dollars.
Discussion
This is so far the largest nationwide study to our knowledge to examine the inter-city socioeconomic disparity in the vulnerability to heat-related all-cause and cause-specific hospitalization. We found that cities with lower literacy rates, urbanization rates, average household incomes, or GDP per capita displayed stronger heat–hospitalization associations. This inter-city socioeconomic inequality was especially significant for hospitalizations of young people (0–19 years), and for hospitalizations due to ischemic heart disease, asthma, pneumonia, renal diseases, mental health conditions, and neoplasms.
The inter-city socioeconomic inequality in the vulnerability to heat could be explained by many factors under a framework of 3 aspects: heat exposure, sensitivity, and adaptation capacity [30]. Regarding heat exposure, people living in areas with low SES are not likely to work in climate-controlled settings (e.g., with air conditioning) [31]. They tend to perform outdoor work such as farming, construction, and mining [4,6]. Regarding sensitivity, people of low SES in Brazil are disproportionally affected by pre-existing non-communicable diseases such as heart disease, depression, chronic kidney diseases, and asthma [32], which could increase their vulnerability to heat [30]. The relatively poor sanitation conditions in areas with low SES might contribute to the residents’ increased vulnerability to heat-related infectious diseases (e.g., pneumonia). Regarding adaptation capacity, people of low SES usually lack the budget to buy air conditioning [33], while the cheaper electric fans are not recommended for dealing with hot weather due to the potential risk of increasing dehydration [34]. The most recent available data for household adoption rate of air conditioning at the city level was from the 2000 Brazil census, and the adoption rate was highest for wealthy, urban households in warm cities [35]. In 2010, Brazil’s national adoption rate of air conditioning was estimated to be 11.8% (up from 7.4% in 2000), with the lowest adoption rate (6.1%) seen in the northeast region (the hottest, poorest, and least urbanized region in Brazil) [35]. People with low educational levels may lack basic knowledge about heat-related health risks and how to prevent the risks [4,31]. In addition, less developed cities might lack cool public spaces such as shaded parks, or libraries, shopping centers, cinemas, or museums with air conditioning [31,36]. These places serve as important cooling shelters for residents during hot weather.
Our results were consistent with a previous study in Australia that included 158 areas within Brisbane and found that the heat–hospitalization associations attenuated in HI areas [18]. By contrast, a study in 132 districts of Vietnam found that the heat–hospitalization associations were stronger in more urbanized areas, which was likely to be explained by the UHI effect [19]. Our inconsistency with this Vietnamese study suggests that the impacts of urbanization on heat vulnerability could be 2-fold. On the one hand, urbanization is associated with UHI effects, which could increase urban residents’ magnitude and duration of heat exposure [37,38]. This could exacerbate the risk of heat-related mortality and morbidity among urban residents [10,11,19]. On the other hand, urbanization is also accompanied by socioeconomic improvements, such as improvements in education, income, access to air conditioning, housing, and sanitation conditions, and decreases in outdoor working times and pre-existing health conditions [4,6,31,32,35]. All these factors tend to reduce urban residents’ sensitivity and increase their adaptation capacity in response to heat exposure. This could explain the attenuated heat–hospitalization or heat–mortality associations in highly urbanized areas observed in our study and previous studies [3,4].
Therefore, whether urbanization is associated with increased or decreased heat vulnerability may depend on the balance between UHI effects and socioeconomic improvements. In this study, for highly urbanized cities of Brazil, the potential effects of UHI effects on heat vulnerability was likely to be offset by the socioeconomic improvements associated with urbanization. Our study and 2 previous studies in China [3,4] challenge the idea of treating high urbanization as an index of high heat vulnerability, as proposed in a recent report [1]. Without considering socioeconomic improvements along with urbanization, it would be inappropriate to conclude that high urbanization would definitely increase heat vulnerability because of UHI effects [1]. More weight should be given to socioeconomic indicators when constructing a heat vulnerability index to monitor the health impacts of heat exposure.
Although previous studies have evaluated the potential modification effect of local SES on heat–mortality [3–11,13–16] or heat–morbidity association [17–20], few of them stratified the analyses by sex, age, and specific causes of hospitalization. The similar socioeconomic disparity in heat vulnerability for females and males is consistent with 2 heat–mortality studies [4,16]. The more significant modification effect found in younger (0–19 years) than other ages could well be explained by the higher heat–hospitalization association in this age group, possibly due to the high prevalence of pneumonia and asthma compared to other ages [23]. For hospitalizations due to asthma, the finding that heat exposure was a risk factor in LMI cities while a protective factor in UMI and HI cities was not totally unexpected. A recent review also found such a discrepancy between studies from different cities [39]. Temperature rise within a certain range could have both adverse (through increasing indoor aeroallergens like spores and cockroaches) and beneficial (through enhancing lung capacity and immune system) impacts on asthma morbidity [39]. In less developed cities with poor sanitation conditions, the adverse impacts might outweigh the beneficial impacts.
The protective effect of heat exposure for hospitalization due to heart failure has also been reported by a US study [40]. It is possible that heart volume overload becomes less likely due to fluid loss in hot weather [40]. The protective effect of heat exposure for hospitalization due to stroke in LMI cities is likely to be due to a decreased rate of hemorrhagic stroke (see Fig I in S2 Text). A meta-analysis also found that high temperatures could reduce the risk of hemorrhagic stroke, which might be explained by the reduced blood pressure due to fluid loss and dilated peripheral vessels in hot temperatures [41]. Most hospitalizations due to cerebrovascular diseases (mainly stroke) and heart failure happened in elderly people (Table A in S2 Text), especially those living in LMI cities (Table I in S2 Text). This might explain the unexpected inter-city socioeconomic disparity pattern in heat vulnerability for elderly people.
The public health implications of this study are 2-fold. On the one hand, given the stronger heat–hospitalization associations in cities of lower SES, climate change could be a potential driver to exacerbate the inter-city inequality in Brazil. Less developed cities in Brazil are expected to suffer more from global warming and heat-related healthcare burden and its related economic costs [42], although they contribute less to carbon emissions than more developed cities. To tackle this unfair situation, more resources (e.g., heat warning systems, air conditioning) should be invested in less developed cities in Brazil under a changing climate. On the other hand, our study might also suggest a potential declining heat–hospitalization association along with economic growth in Brazil. In other words, there might be adaptation to heat exposure as reported in the US, Czech Republic, Spain, and Japan [43,44]. However, some other countries (e.g., Australia and South Korea [43]) did not show significant adaptation to heat. Our previous study reported a non-significant decline of heat–hospitalization association during 2000–2015 in Brazil, despite rapid economic growth during this period [23]. Therefore, more studies are needed to explore whether socioeconomic improvement could promote adaptations to heat.
The present study has several strengths. First, the 16-year-long study period, very large sample size (49 million hospitalizations), and large number of locations (1,814 cities) ensured the statistical power and robustness of our results. Second, to our knowledge, ours is the first study evaluating almost all major cause-specific heat-related hospitalizations in one study. This study could give people a comprehensive view on heat–morbidity associations. Going beyond mortality to morbidity statistics (represented by hospitalization) also adds great value to existing literature, which mainly focuses on heat–mortality associations. Third, the national hospitalization dataset covered nearly 80% of the Brazilian population, which gives good representativeness. Finally, given the great socioeconomic diversity within the 1,814 cities studied, our findings might also apply to other middle- and high-income countries.
There are also several limitations. Some limitations have been discussed by our previous publication, including the use of gridded temperature data rather than personal measurements, and being unable to adjust for relative humidity [23]. Due to the unavailability of individual-level socioeconomic data in the hospitalization records, we had to rely on city-level socioeconomic data, which meant we could not evaluate intra-city or individual-level socioeconomic inequalities [30]. However, our findings could still be quite relevant for adaptation policy at the state or national level, in terms of allocating resources between cities to deal with the increasing heat exposure under global warming. This could be an indispensable part of promoting Brazil’s within-country health equity, one of the priorities of the Sustainable Development Goals [45]. The 4 socioeconomic indicators in our study were correlated with each other, making it difficult to identify and compare the independent modification effect of each indicator [31]. However, the results from different indicators were largely similar, and all suggested the existence of inter-city socioeconomic disparities in heat vulnerability.
Finally, due to data availability, we were unable to adjust for some potential important city characteristics (e.g., air quality, green space, population health status, access to air conditioning) that could explain or confound the inter-city socioeconomic disparities. As discussed, access to air conditioning and population health status (e.g., prevalence of chronic diseases) tend to be mediators between city-level SES and heat vulnerability [30,32,33,35]. Adjusting for these potential mediators in future studies would help to test hypotheses about the potential pathways of socioeconomic disparity in heat vulnerability. Economic growth and urbanization in Brazil are generally associated with increased ambient air pollution and decreased green space (a measure of vegetation density), due to increased emissions from industries and traffic and a shift from vegetated lands to building structures [46–49].Poor outdoor air quality and low green space have been found to enhance rather than attenuate residents’ vulnerability to heat-related morbidity and mortality [50–54]. Therefore, the negative association between city-level socioeconomic factors and heat vulnerability is not likely to be explained by inter-city variations in green space and air quality.
In conclusion, less developed cities in Brazil displayed stronger heat–hospitalization associations, especially for hospitalizations of children and adolescents, and for hospitalizations due to specific conditions. This may exacerbate existing inter-city health and socioeconomic inequalities. More resources should be invested in less developed cities in Brazil to tackle the morbidity burden of heat exposure and to promote health equity under global warming.
Supporting information
STROBE, Strengthening the Reporting of Observational Studies in Epidemiology.
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We thank the Brazilian Ministry of Health and Brazilian National Institute of Meteorology for providing hospitalization and meteorological data, respectively.
Abbreviations
- COPD
chronic obstructive pulmonary disease
- GDP
gross domestic product
- HI
high income
- LMI
lower middle income
- RR
relative risk
- SES
socioeconomic status
- UHI
urban heat island
- UMI
upper middle income
Data Availability
The authors are not permitted to share the data owned by a third party. For information on data access, readers are asked to contact Dr. Pei Yu (Pei.Yu1@monash.edu).
Funding Statement
R.X. was supported by China Scholarship Council (201806010405). S.L. was supported by an Early Career Fellowship of the Australian National Health and Medical Research Council (APP1109193). Y.G. was supported by a Career Development Fellowship of the Australian National Health and Medical Research Council (APP1107107 & APP1163693). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Watts N, Amann M, Ayeb-Karlsson S, Belesova K, Bouley T, Boykoff M, et al. The Lancet Countdown on health and climate change: from 25 years of inaction to a global transformation for public health. Lancet. 2018;391(10120):581–630. 10.1016/S0140-6736(17)32464-9 [DOI] [PubMed] [Google Scholar]
- 2.Benmarhnia T, Deguen S, Kaufman JS, Smargiassi A. Review article: vulnerability to heat-related mortality: a systematic review, meta-analysis, and meta-regression analysis. Epidemiology. 2015;26(6):781–93. 10.1097/EDE.0000000000000375 [DOI] [PubMed] [Google Scholar]
- 3.Chen K, Zhou L, Chen X, Ma Z, Liu Y, Huang L, et al. Urbanization level and vulnerability to heat-related mortality in Jiangsu Province, China. Environ Health Perspect. 2016;124(12):1863–9. 10.1289/EHP204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hu K, Guo Y, Hochrainer-Stigler S, Liu W, See L, Yang X, et al. Evidence for urban–rural disparity in temperature–mortality relationships in Zhejiang Province, China. Environ Health Perspect. 2019;127(3):37001 10.1289/EHP3556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zanobetti A, O’Neill MS, Gronlund CJ, Schwartz JD. Susceptibility to mortality in weather extremes effect modification by personal and small-area characteristics. Epidemiology. 2013;24(6):809–19. 10.1097/01.ede.0000434432.06765.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kovach MM, Konrad CE II, Fuhrmann CM. Area-level risk factors for heat-related illness in rural and urban locations across North Carolina, USA. Appl Geogr. 2015;60:175–83. 10.1016/j.apgeog.2015.03.012 [DOI] [Google Scholar]
- 7.Harlan SL, Declet-Barreto JH, Stefanov WL, Petitti DB. Neighborhood effects on heat deaths: social and environmental predictors of vulnerability in Maricopa County, Arizona. Environ Health Perspect. 2012;121(2):197–204. 10.1289/ehp.1104625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berko J, Ingram DD, Saha S, Parker JD. Deaths attributed to heat, cold, and other weather events in the United States, 2006–2010. Natl Health Stat Report. 2014;(76):1–15. [PubMed] [Google Scholar]
- 9.Madrigano J, Jack D, Anderson GB, Bell ML, Kinney PL. Temperature, ozone, and mortality in urban and non-urban counties in the northeastern United States. Environ Health. 2015;14:3 10.1186/1476-069X-14-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vicedo-Cabrera AM, Gasparrini A, Armstrong B, Sera F, Guo Y, Hashizume M, et al. How urban characteristics affect vulnerability to heat and cold: a multi-country analysis. Int J Epidemiol. 2019; 48(4):1101–12. 10.1093/ije/dyz008 [DOI] [PubMed] [Google Scholar]
- 11.Burkart K, Schneider A, Breitner S, Khan MH, Krämer A, Endlicher W. The effect of atmospheric thermal conditions and urban thermal pollution on all-cause and cardiovascular mortality in Bangladesh. Environ Pollut. 2011;159(8–9):2035–43. 10.1016/j.envpol.2011.02.005 [DOI] [PubMed] [Google Scholar]
- 12.Hajat S, Kosatky T. Heat-related mortality: a review and exploration of heterogeneity. J Epidemiol Community Health. 2010;64(9):753–60. 10.1136/jech.2009.087999 [DOI] [PubMed] [Google Scholar]
- 13.Zhang YQ, Yu CH, Bao JZ, Li XD. Impact of temperature on mortality in Hubei, China: a multi-county time series analysis. Sci Rep. 2017;7:45093 10.1038/srep45093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bennett JE, Blangiardo M, Fecht D, Elliott P, Ezzati M. Vulnerability to the mortality effects of warm temperature in the districts of England and Wales. Nat Clim Chang. 2014;4(4):269 10.1038/nclimate2123 [DOI] [Google Scholar]
- 15.Hattis D, Ogneva-Himmelberger Y, Ratick S. The spatial variability of heat-related mortality in Massachusetts. Appl Geogr. 2012;33:45–52. 10.1016/j.apgeog.2011.07.008 [DOI] [Google Scholar]
- 16.Yu WW, Vaneckova P, Mengersen K, Pan XC, Tong SL. Is the association between temperature and mortality modified by age, gender and socio-economic status? Sci Total Environ. 2010;408(17):3513–8. 10.1016/j.scitotenv.2010.04.058 [DOI] [PubMed] [Google Scholar]
- 17.Phung D, Guo YM, Nguyen HTL, Rutherford S, Baum S, Chu C. High temperature and risk of hospitalizations, and effect modifying potential of socio-economic conditions: a multi-province study in the tropical Mekong Delta Region. Environ Int. 2016;92–93:77–86. 10.1016/j.envint.2015.11.003 [DOI] [PubMed] [Google Scholar]
- 18.Hondula DM, Barnett AG. Heat-related morbidity in Brisbane, Australia: spatial variation and area-level predictors. Environ Health Perspect. 2014;122(8):831–6. 10.1289/ehp.1307496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phung D, Chu C, Tran DN, Huang CR. Spatial variation of heat-related morbidity: a hierarchical Bayesian analysis in multiple districts of the Mekong Delta Region. Sci Total Environ. 2018;637:1559–65. 10.1016/j.scitotenv.2018.05.131 [DOI] [PubMed] [Google Scholar]
- 20.Urban A, Davidkovova H, Kysely J. Heat- and cold-stress effects on cardiovascular mortality and morbidity among urban and rural populations in the Czech Republic. Int J Biometeorol. 2014;58(6):1057–68. 10.1007/s00484-013-0693-4 [DOI] [PubMed] [Google Scholar]
- 21.Song X, Wang S, Hu Y, Yue M, Zhang T, Liu Y, et al. Impact of ambient temperature on morbidity and mortality: an overview of reviews. Sci Total Environ. 2017;586:241–54. 10.1016/j.scitotenv.2017.01.212 [DOI] [PubMed] [Google Scholar]
- 22.Zhao Q, Li S, Coelho M, Saldiva PHN, Hu K, Abramson MJ, et al. Assessment of intraseasonal variation in hospitalization associated with heat exposure in Brazil. JAMA Netw Open. 2019;2(2):e187901 10.1001/jamanetworkopen.2018.7901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhao Q, Li S, Coelho M, Saldiva PHN, Hu K, Arblaster JM, et al. Geographic, demographic, and temporal variations in the association between heat exposure and hospitalization in Brazil: a nationwide study between 2000 and 2015. Environ Health Perspect. 2019;127(1):17001 10.1289/EHP3889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhao Q, Coelho MSZS, Li S, Saldiva PHN, Abramson MJ, Huxley RR, et al. Trends in hospital admission rates and associated direct healthcare costs in Brazil: a nationwide retrospective study between 2000 and 2015. The Innovation. 2020;1(1):100013 10.1016/j.xinn.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xavier AC, King CW, Scanlon BR. Daily gridded meteorological variables in Brazil (1980–2013). Int J Climatol. 2016;36(6):2644–59. [Google Scholar]
- 26.Guo Y. Hourly associations between heat and ambulance calls. Environ Pollut. 2017;220:1424–8. 10.1016/j.envpol.2016.10.091 [DOI] [PubMed] [Google Scholar]
- 27.Guo Y, Barnett Adrian G, Pan X, Yu W, Tong S. The impact of temperature on mortality in Tianjin, China: a case-crossover design with a distributed lag nonlinear model. Environ Health Perspect. 2011;119(12):1719–25. 10.1289/ehp.1103598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gasparrini A. Distributed lag linear and non-linear models in R: the package dlnm. J Stat Softw. 2011;43(8):1–20. [PMC free article] [PubMed] [Google Scholar]
- 29.Gasparrini A, Armstrong B. Reducing and meta-analysing estimates from distributed lag non-linear models. BMC Med Res Methodol. 2013;13:1 10.1186/1471-2288-13-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Romero-Lankao P, Qin H, Dickinson K. Urban vulnerability to temperature-related hazards: a meta-analysis and meta-knowledge approach. Glob Environ Change. 2012;22(3):670–83. 10.1016/j.gloenvcha.2012.04.002 [DOI] [Google Scholar]
- 31.Gronlund CJ. Racial and socioeconomic disparities in heat-related health effects and their mechanisms: a review. Curr Epidemiol Rep. 2014;1(3):165–73. 10.1007/s40471-014-0014-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Malta DC, Bernal RT, de Souza MF, Szwarcwald CL, Lima MG, Barros MB. Social inequalities in the prevalence of self-reported chronic non-communicable diseases in Brazil: national health survey 2013. Int J Equity Health. 2016;15(1):153 10.1186/s12939-016-0427-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Medina-Ramon M, Schwartz J. Temperature, temperature extremes, and mortality: a study of acclimatisation and effect modification in 50 US cities. Occup Environ Med. 2007;64(12):827–33. 10.1136/oem.2007.033175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hajat S, O’Connor M, Kosatsky T. Health effects of hot weather: from awareness of risk factors to effective health protection. Lancet. 2010;375(9717):856–63. 10.1016/S0140-6736(09)61711-6 [DOI] [PubMed] [Google Scholar]
- 35.Forrester S. Residential cooling load impacts on brazil’s electricity demand [thesis]. Ann Arbor (MI): University of Michigan; 2019 [cited 2020 Sep 8]. Available from: http://hdl.handle.net/2027.42/148809.
- 36.Sampson NR, Gronlund CJ, Buxton MA, Catalano L, White-Newsome JL, Conlon KC, et al. Staying cool in a changing climate: reaching vulnerable populations during heat events. Glob Environ Change. 2013;23(2):475–84. 10.1016/j.gloenvcha.2012.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tan J, Zheng Y, Tang X, Guo C, Li L, Song G, et al. The urban heat island and its impact on heat waves and human health in Shanghai. Int J Biometeorol. 2010;54(1):75–84. 10.1007/s00484-009-0256-x [DOI] [PubMed] [Google Scholar]
- 38.Heaviside C, Macintyre H, Vardoulakis S. The urban heat island: implications for health in a changing environment. Curr Environ Health Rep. 2017;4(3):296–305. 10.1007/s40572-017-0150-3 [DOI] [PubMed] [Google Scholar]
- 39.Xu ZW, Crooks JL, Davies JM, Khan A, Hu WB, Tong SL. The association between ambient temperature and childhood asthma: a systematic review. Int J Biometeorol. 2018;62(3):471–81. 10.1007/s00484-017-1455-5 [DOI] [PubMed] [Google Scholar]
- 40.Bobb JF, Obermeyer Z, Wang Y, Dominici F. Cause-specific risk of hospital admission related to extreme heat in older adults. JAMA. 2014;312(24):2659–67. 10.1001/jama.2014.15715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kokotailo RA, Hill MD. Coding of stroke and stroke risk factors using International Classification of Diseases, revisions 9 and 10. Stroke. 2005;36(8):1776–81. 10.1161/01.STR.0000174293.17959.a1 [DOI] [PubMed] [Google Scholar]
- 42.Wondmagegn BY, Xiang JJ, Williams S, Pisaniello D, Bi P. What do we know about the healthcare costs of extreme heat exposure? A comprehensive literature review. Sci Total Environ. 2019;657:608–18. 10.1016/j.scitotenv.2018.11.479 [DOI] [PubMed] [Google Scholar]
- 43.Gasparrini A, Guo Y, Hashizume M, Kinney PL, Petkova EP, Lavigne E, et al. Temporal variation in heat-mortality associations: a multicountry study. Environ Health Perspect. 2015;123(11):1200–7. 10.1289/ehp.1409070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carson C, Hajat S, Armstrong B, Wilkinson P. Declining vulnerability to temperature-related mortality in London over the 20th century. Am J Epidemiol. 2006;164(1):77–84. 10.1093/aje/kwj147 [DOI] [PubMed] [Google Scholar]
- 45.Hosseinpoor AR, Bergen N, Magar V. Monitoring inequality: an emerging priority for health post-2015. Bull World Health Organ. 2015;93(9):591–A. 10.2471/BLT.15.162081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Manhaes MA, Loures-Ribeiro A. Spatial distribution and diversity of bird community in an urban area of Southeast Brazil. Braz Arch Biol Technol. 2005;48(2):285–94. 10.1590/S1516-89132005000200016 [DOI] [Google Scholar]
- 47.Cavalcante RM, Rocha CA, De Santiago IS, Da Silva TFA, Cattony CM, Silva MVC, et al. Influence of urbanization on air quality based on the occurrence of particle-associated polycyclic aromatic hydrocarbons in a tropical semiarid area (Fortaleza-CE, Brazil). Air Qual Atmos Health. 2017;10(4):437–45. 10.1007/s11869-016-0434-z [DOI] [Google Scholar]
- 48.Leite Silva A, Márcia Longo R. Influence of urbanization on the original vegetation cover in urban river basin: case study in Campinas/SP, Brazil. 19th EGU General Assembly; 2017 Apr 23–28; Vienna; Austria. 2017 [cited 2020 Sep 8]. Available from: https://ui.adsabs.harvard.edu/abs/2017EGUGA..19.5368L/abstract.
- 49.Requia WJ, Roig HL, Koutrakis P, Adams MD. Modeling spatial patterns of traffic emissions across 5570 municipal districts in Brazil. J Clean Prod. 2017;148:845–53. 10.1016/j.jclepro.2017.02.010 [DOI] [Google Scholar]
- 50.Gronlund CJ, Berrocal VJ, White-Newsome JL, Conlon KC, O’Neill MS. Vulnerability to extreme heat by socio-demographic characteristics and area green space among the elderly in Michigan, 1990–2007. Environ Res. 2015;136:449–61. 10.1016/j.envres.2014.08.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Burkart K, Meier F, Schneider A, Breitner S, Canario P, Alcoforado MJ, et al. Modification of heat-related mortality in an elderly urban population by vegetation (urban green) and proximity to water (urban blue): evidence from Lisbon, Portugal. Environ Health Perspect. 2016;124(7):927–34. 10.1289/ehp.1409529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schinasi LH, Benmarhnia T, De Roos AJ. Modification of the association between high ambient temperature and health by urban microclimate indicators: a systematic review and meta-analysis. Environ Res. 2018;161:168–80. 10.1016/j.envres.2017.11.004 [DOI] [PubMed] [Google Scholar]
- 53.Parry M, Green D, Zhang Y, Hayen A. Does particulate matter modify the short-term association between heat waves and hospital admissions for cardiovascular diseases in Greater Sydney, Australia? Int J Environ Res Public Health. 2019;16(18):3270 10.3390/ijerph16183270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Patel D, Jian L, Xiao J, Jansz J, Yun G, Robertson A. Joint effect of heatwaves and air quality on emergency department attendances for vulnerable population in Perth, Western Australia, 2006 to 2015. Environ Res. 2019;174:80–7. 10.1016/j.envres.2019.04.013 [DOI] [PubMed] [Google Scholar]