Supplemental Digital Content is available in the text.
Abstract
Background:
In light of the recent surge of media coverage and social media influence regarding breast implants, it is essential to understand patients’ concerns and misconceptions so that we can better serve them.
Methods:
The authors designed a survey study for assessing the awareness and perception of patients toward breast implant–associated anaplastic large cell lymphoma (BIA-ALCL) and breast implant illness (BII). In total, 130 patients presenting to the senior author’s breast reconstruction clinic completed the survey. The survey assessed patients’ knowledge on and their perception of BIA-ALCL and BII.
Results:
“News article” and “Television” were most often selected as sources of information for BIA-ALCL (21% and 20%, respectively) and BII (20% and 25%, respectively). A total of 100 patients (77%) had previous knowledge of BIA-ALCL. Forty-seven percent (n = 47/100) responded that they were unsure of the fate of a person diagnosed with BIA-ALCL, and 25% (n = 25/100) were unaware of the association between BIA-ALCL and specific implant type. Patients who were unaware of BIA-ALCL prognosis reported being less likely to receive breast implants in the future (P = 0.012, χ2 = 19.48). Eighty-nine patients (68%) had previous knowledge of BII. A total of 60 symptoms were mentioned by patients, with “Fatigue” (12%, n = 26) being cited the most often.
Conclusions:
The present survey highlights the importance for plastic surgeons to frequently discuss these entities with their patients. This should be done despite the obscurity of BII, in an effort to offer the best available evidence to our patients.
INTRODUCTION
Over the last few decades, silicone implants have had a back-and-forth relationship with the US Food and Drug Administration regarding their approval and with the public regarding their perception.1,2 The surge in reports of complications in women having received the first generation of implants, anecdotal reports highlighting the potential association with systemic diseases, and a large number of lawsuits from unsatisfied patients led the US Food and Drug Administration to implement a voluntary moratorium on silicone breast implants in 1992.3,4 It was not until 2006, following several longitudinal clinical studies disproving systemic sequelae secondary to silicone breast implants, that these became available once again to the general public.5–13
Recently, however, there has been media-driven attention to a new concern regarding breast implants.14 More specifically, there has been an increase in reports of nonspecific systemic symptoms with claims of a direct causation to breast implants despite ambiguity surrounding a scientifically sound association.15,16 This concept, now known as “breast implant illness” (BII), is defined as a constellation of vague physical and psychological symptoms thought to be related to implants, and is largely fueled by social media groups.4,17 Despite uncertainty surrounding the scientific basis of this issue, patients continue to consult their surgeons due to a wide range of multisystemic undifferentiated presentations. Parallel to the increase in reporting of BII, the association between textured implants and breast implant–associated anaplastic large cell lymphoma (BIA-ALCL) has also contributed to the perceived health and safety concerns regarding breast implants.18–20
In light of the recent surge of media coverage and social media influence regarding breast implants, it is essential to understand patients’ concerns and misconceptions so that we can better serve them. The authors designed a survey study assessing the awareness and perception of patients toward both BIA-ALCL and BII.
MATERIALS AND METHODS
After receiving approval from our institutional review board, a 16-question survey consisting of both multiple choice and short answer questions was distributed to all follow-up or new consultations presenting to the senior author’s breast reconstruction clinic from October 20, 2019 to February 28, 2020 at the Royal Victoria Hospital in Montreal, Canada. All patients presenting to the clinic were asked by the clinic clerk to complete the survey in the waiting room, on a voluntary basis and with complete anonymity. Patients were asked if they had already completed the survey before distribution in an effort to prevent dual responses. The survey was returned to the clinic clerk before seeing the surgeon. Patients who have completed the survey either have a history of breast reconstruction or were consulting the senior author regarding breast reconstruction. The survey included questions pertaining to knowledge or perception of both BIA-ALCL and BII. The survey was written in lay-terms, and in both French and English. Of note, before distributing the survey, a test with 20 online respondents was performed using the MTurk (Amazon Mechanical Turk, Seattle, Wash.) crowdsourcing platform. The level of difficulty and the neutrality of the questions were assessed and adjusted accordingly. The full survey can be found in survey, Supplemental Digital Content 1, which displays the breast implant survey. http://links.lww.com/PRSGO/B473). Surveys where respondents denied knowing about both BIA-ALCL and BII were excluded. Text responses in French were converted to English to facilitate data analysis. The responses were pooled across all participants that had previous knowledge on BIA-ALCL and/or BII for descriptive purposes. Responses regarding perception were also compared between patients with and without knowledge of the prognosis related to BIA-ALCL, through a chi-square analysis carried out on SPSS v.22 (IBM Corp, Armonk, N.Y.).
RESULTS
Demographics
Following the exclusion of respondents who denied knowledge about both BIA-ALCL and BII (n = 65/195), the total study population consisted of 130 patients. The mean patient age was 52 years (range 21–80, SD: 12). The primary language was English in 71% (n = 92/130) of participants. Seventy-eight percent (n = 101/130) of participants had a history of breast cancer and had already undergone reconstruction with implants.
Knowledge and perception of Breast Implant–Associated Anaplastic Large Cell Lymphoma
Seventy-seven percent of patients (n = 100/130) had previously heard of BIA-ALCL, of which 83% (n = 83/100) had a history of breast cancer. Among these patients, “News article” (21%), “Television” (20%), and “Doctor’s office” (18%) were most often selected as sources of BIA-ALCL information. Of note, multiple choices could be selected for this question. The full list of options with their respective frequencies can be found in Figure 1. Among patients who previously heard of BIA-ALCL (n = 100/130), 47% (n = 47/100) responded that they were unsure of the fate of a person with the diagnosis of BIA-ALCL, whereas 35% (n = 35/100) responded that most cases are curable. (See figure, Supplemental Digital Content 2, which displays the answers to the question “What is the fate of a person with BIA-ALCL?”, http://links.lww.com/PRSGO/B474.) Additionally, 61% (n = 61/100) correctly identified that BIA-ALCL is limited to textured implants, whereas 25% (n = 25/100) were unaware of the association between BIA-ALCL and specific implant type. (See figure, Supplemental Digital Content 2, which displays the answers to the question “What is the fate of a person with BIA-ALCL?”, http://links.lww.com/PRSGO/B474.)
Fig. 1.
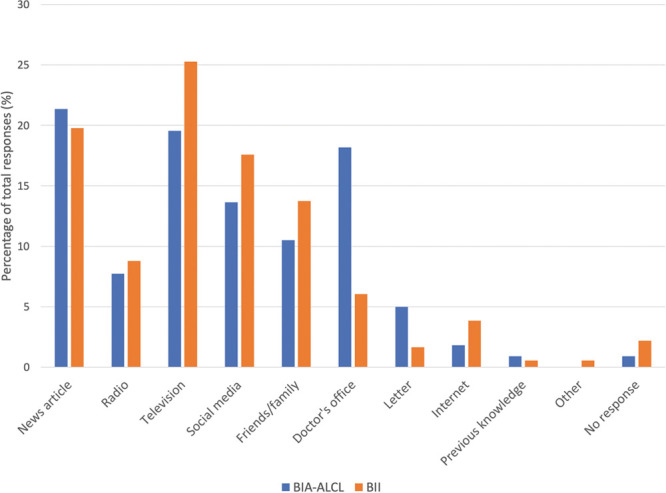
Answers to the question “Where have you heard of BIA-ALCL/BII?” (Questions 6 and 13).
When asked to describe BIA-ALCL in 3–5 words, the most commonly mentioned words were cancer (18%), implant-induced/related (13%), and lymphoma (11%). A list of the most frequent terms with their respective frequencies can be found in Table 1. When the group of patients with prior knowledge of BIA-ALCL were asked how the emergence of BIA-ALCL had affected their perception of breast implant surgery, 26% (n = 26/100) denied any effects on their willingness toward receiving breast implants, 16% (n = 16/100) reported a desire for explantation, and 10% (n = 10/100) reported being less likely to receive breast implants in the future. The full distribution of responses can be found in Figure 2. When this group of patients was asked whether they would be more or less likely to recommend breast implants to a family member or friend, 43% (n = 43/100) said they would be less likely, while 31% (n = 31/100) said they would be just as likely. The full list of responses with their relative frequencies can be found in Figure 3.
Table 1.
Terms Most Frequently Used to Describe BIA-ALCL (Question 9)
| Term | % | (n) |
|---|---|---|
| Cancer | 18 | (16) |
| Implant induced/related | 13 | (11) |
| Lymphoma | 11 | (10) |
| Risk/danger/possible complications | 8 | (7) |
| Textured implant related | 8 | (7) |
| Irritation/inflammation/rejection | 5.7 | (5) |
| Rare | 5.7 | (5) |
| Unsure | 5.7 | (5) |
| Breast cancer | 3.4 | (3) |
| Capsule | 2.3 | (2) |
| Curable | 2.3 | (2) |
| Death/fatal | 2.3 | (2) |
| Shocking | 2.3 | (2) |
Fig. 2.
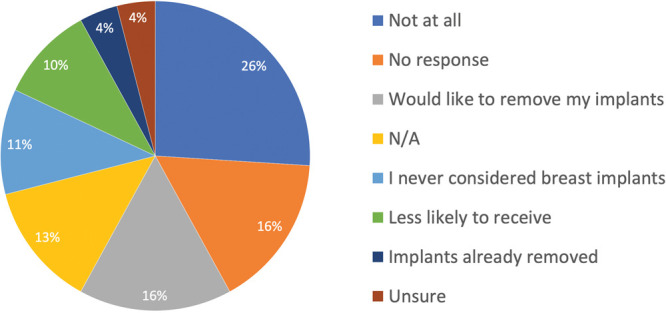
Answers to the question “How has the emergence of BIA-ALCL affected your perception of breast implant surgery?” (Question 7).
Fig. 3.
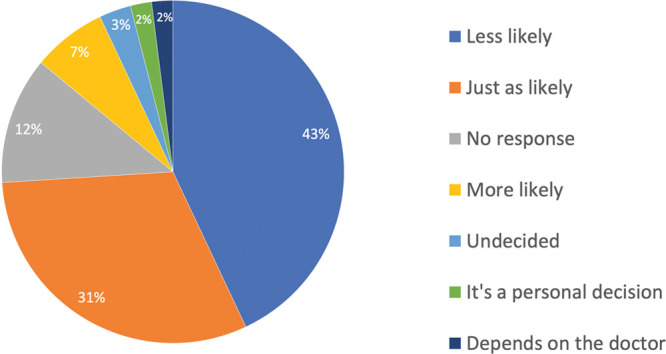
Answers to the question “Are you more or less likely to recommend breast implants to a family member or friend?” (Question 8 in the BIA-ALCL section).
Knowledge and Perception of Breast Implant Illness
Sixty-eight percent of women (n = 89/130) claimed to have previously heard of BII. “Television” (25%) and “News article” (20%) were selected most often as the source of BII information, followed by “Social Media” (18%) and “Friends/Family” (14%). Of note, multiple choices could be selected for this question. The full list of options with their respective frequencies can be found in Figure 1. The participants were also asked to name symptoms of BII (up to a maximum of 12 symptoms). Because multiple responses were allowed, a total of 219 symptoms were compiled. Fatigue (12%), Pain (11%), and Headache/migraine (5%) were cited the most often. The full list of symptoms mentioned with their relative frequencies can be found in Table 2.
Table 2.
Terms Used to Describe BII (Question 14)
| Term | % | (n) |
|---|---|---|
| Fatigue | 12 | (26) |
| Pain | 11 | (24) |
| Headache/migraine | 5 | (11) |
| Infection | 4.1 | (9) |
| Arthralgia | 4.1 | (9) |
| Depression/mood changes | 4.1 | (9) |
| Malaise | 4.1 | (9) |
| Swelling | 3.2 | (7) |
| Leaking/rupture/deflation | 3.2 | (7) |
| Brain fog/difficulty concentrating | 2.7 | (6) |
| Pain localized to breast | 2.7 | (6) |
| Hair loss | 2.3 | (5) |
| Hardness | 2.3 | (5) |
| Immune system/autoimmune | 2.3 | (5) |
| Nausea | 2.3 | (5) |
| Rash/dry skin | 2.3 | (5) |
| Myalgia | 1.8 | (4) |
| Palpitations | 1.8 | (4) |
| Anxiety | 1.4 | (3) |
| Cancer | 1.4 | (3) |
| Chest pain | 1.4 | (3) |
| Chronic inflammation | 1.4 | (3) |
| Discomfort/Soreness | 1.4 | (3) |
| Rejection | 1.4 | (3) |
| Affect subsequent diagnostic tests | 0.9 | (2) |
| Back pain | 0.9 | (2) |
| Capsulitis | 0.9 | (2) |
| Dyspepsia/dysphagia | 0.9 | (2) |
| Fever | 0.9 | (2) |
| Hormonal imbalance | 0.9 | (2) |
| Lymphedema/extremity swelling | 0.9 | (2) |
| Memory loss | 0.9 | (2) |
| Weight loss | 0.9 | (2) |
| Deformation/shape | 0.5 | (1) |
| Erythema | 0.5 | (1) |
| Body odor | 0.5 | (1) |
| Buccal ulcers | 0.5 | (1) |
| Chills | 0.5 | (1) |
| Crohn’s | 0.5 | (1) |
| Decreased breast sensation | 0.5 | (1) |
| Decreased energy | 0.5 | (1) |
| Decreased libido | 0.5 | (1) |
| Dry mucous membranes | 0.5 | (1) |
| Dull facial expression | 0.5 | (1) |
| Dyspareunia | 0.5 | (1) |
| Fibromyalgia | 0.5 | (1) |
| Heat intolerance | 0.5 | (1) |
| Increased breast sensitivity | 0.5 | (1) |
| Insomnia | 0.5 | (1) |
| Itchiness | 0.5 | (1) |
| Muscle twitches | 0.5 | (1) |
| Necrosis | 0.5 | (1) |
| Night sweats | 0.5 | (1) |
| Perspiratory issues | 0.5 | (1) |
| Premature aging | 0.5 | (1) |
| Raynaud’s | 0.5 | (1) |
| Reflux | 0.5 | (1) |
| Swollen lymph node | 0.5 | (1) |
| Tinnitus | 0.5 | (1) |
| Weight gain | 0.5 | (1) |
Participants were asked how the emergence of BII had affected their perception of breast implant surgery. In response to this, 31% (n = 28/89) of patients with prior knowledge of BII denied any effects on their willingness toward receiving breast implants, while 14% (n = 12/89) reported that they would be less likely to undergo an implant-based surgery in the future. The full distribution of responses can be found in Figure 4. Participants were also asked if they would be more or less likely to recommend breast implants to a family member or friend. Forty-two percent of respondents (n = 37/89) who were aware of BII reported being less likely to do so, while 34% (n = 30/89) felt that they would be just as likely. The full list of responses with their relative frequencies can be found in Figure 5.
Fig. 4.
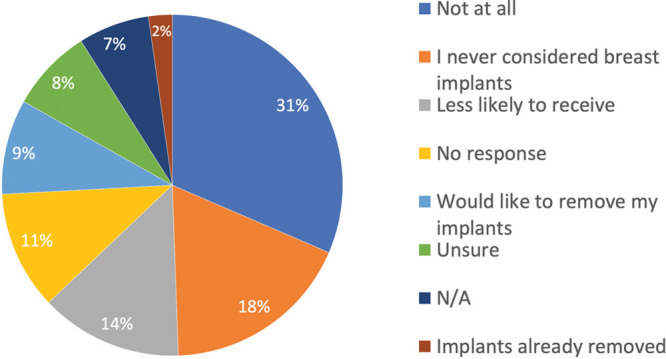
Answers to the question “How has the emergence of breast implant illness affected your perception of breast implant surgery?” (Question 15).
Fig. 5.
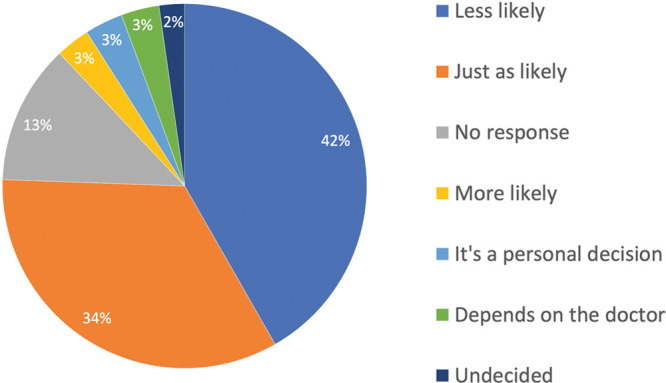
Answers to the question “Are you more or less likely to recommend breast implants to a family member or friend?” Question 16 in the BII section).
Response Stratification According to Knowledge of Prognosis
Among patients that were aware of the prognosis of BIA-ALCL (n = 35), 34% (n = 12/35) reported that their perception of breast implant surgery was not affected, whereas only 5.7% (n = 2/35) reported being less likely to receive breast implants in the future. In comparison, among the patients that were unaware of the prognosis of BIA-ALCL (n = 65), only 22% (n = 14/65) reported that their perception of BIA-ALCL was minimally affected while 12% (n = 8/65) reported being less likely to receive breast implants in the future. This difference in perception stratified by knowledge of prognosis of BIA-ALCL was found to be statistically significant by the chi-square analysis (P = 0.012, χ2 = 19.48).
DISCUSSION
While BIA-ALCL is a distinct breast implant–related disease widely studied in the plastic surgery literature, to date, BII is a vague constellation of symptoms without a scientifically sound association. With the recent wave of information and intertwined rise in concern regarding BIA-ALCL and BII, the authors felt it was important to assess the knowledge and perception of both of these entities among a cohort of breast reconstruction patients.21–23 It was of particular interest to determine their awareness and perception toward breast implants, as their opinions may have significant effects on the future of breast surgery and patients inquiring about implant-based reconstruction.
Knowledge and Perception of BIA-ALCL
Patients awaiting breast reconstruction and those who have recently undergone breast reconstruction are expected to be the most informed, as they are directly impacted by this entity and have an interest in separating fact from misconception. Regular follow-ups with their reconstructive surgeon facilitate access to evidence-based information. Interestingly, of the 101 patients who currently or previously had breast implants, 16% (n = 16/101) were unaware of BIA-ALCL. Moreover, among the cohort of patients that were aware of BIA-ALCL, a significant proportion had clear lacunae in terms of their knowledge of the fate of a person with the diagnosis of BIA-ALCL and of its association to textured implants. This further strengthens the importance of continued education, as patients that claim to be aware of BIA-ALCL may have significant knowledge gaps regarding basic pathophysiology and prognosis.
Although BIA-ALCL did not appear to negatively impact most patients’ perception, 10% (n = 10/100) of patients answered that they are now less likely to receive breast implants and 16% (n = 16/100) were seeking explantation. This is similar to the numbers provided by Lee et al,24 showing that 35% of patients with breast implants were strongly considering removing their implants when asked about BIA-ALCL. Moreover, 43% of patients (n = 43/100) replied that they would be less likely to recommend breast implants to a family member or friend. Misinformation may have contributed to negative perceptions and hence evidence-based discussions on the indications for explantation are pivotal. More specifically, patients that were aware of the prognosis of BIA-ALCL were statistically more likely to have an unaltered perception of breast implant surgery and less often reported being less likely to receive breast implants in the future, when compared with patients that were unaware of the prognosis of BIA-ALCL. This further highlights the importance of educating our patients, as it directly impacts their perception and likely countless other future patients who are considering breast implant surgery.
When survey participants with prior knowledge of BIA-ALCL were asked to describe BIA-ALCL in 3–5 words, accurate terms such as cancer (18%), implant-induced/related (13%), lymphoma (11%), risk (8%), and rare (6%) were commonly used. Interestingly, 13% used the term “implant” on its own, whereas only 8% specifically used the term “textured implant.” The link to textured implants is critical for patients to be aware of, especially in the context of the Health Canada ban on textured implants.25 A well-informed patient should know that, to date, there have been no reported cases of BIA-ALCL in a patient with a history of a smooth device only.26,27
Knowledge and Perception of BII
Overall, 28% (n = 28/101) of patients with prior breast implants were unaware of BII. Given the significant rise in discussion of BII in nonmedical platforms (eg, Facebook groups), this cohort of patients is at risk for developing potentially misinformed and unfounded preconceptions, further stressing the importance of patient education during consultation with a breast reconstructive surgeon.17,28 Among patients who claimed to know about BII (n = 89/130), 14% (n = 12/89) reported being less likely to undergo a breast implant surgery, while an even larger proportion (42%, n = 37/89) said they would be less likely to recommend breast implants to a family member or a friend. Overall, current patients in the survey seemed to be more adamant about future patients avoiding implants, contrarily to having a negative attitude toward their own implants or wanting to remove them. Misinformation or unfounded fear may lead to deterring patients’ family or friends from seeking an implant-based reconstruction on the basis of an entity that is poorly characterized and lacking scientifically robust evidence. Proper education of our current patients is thus an investment for our future patients.
The participants were also asked to name as many symptoms as possible about BII. The responses were heavily varied, resulting in 60 different terms. A few studies have highlighted patient-reported symptoms in relation to BII, with arthralgia, fatigue, and pain often mentioned, but none were as comprehensive or quantitatively detailed as the list provided in our study.4,17,29 Although very diverse, our results contribute to the endeavor of properly defining and understanding BII as caregivers.14 This is essential to properly address the media-driven rise in inquiries regarding “en bloc capsulectomies”—a term heavily misunderstood by the general public.30–32 Patient stratification based on symptomatology and pre-existing comorbidities are essential first steps at attempting to determine the likelihood for resolution of BII following explantation.4,30–32 It is also interesting to highlight the overlap in terms used to describe BII and capsular contracture or other local implant-associated phenomena. These include swelling (3.2%), rupture (3.2%), pain localized to breast (2.7%), hardness (2.3%), discomfort (1.4%), deformation (0.5%), and erythema (0.5%). This further solidifies the importance of patient education, including the spectrum of common symptoms and complications associated with breast implants. For instance, patients with the local symptoms stated above should be informed of the range of treatable causes including capsular contracture and animation deformity, rather than attributing this solely to BII.
Sources of Knowledge for BIA-ALCL and BII
With the many ways one can access information, the authors felt it would be interesting to determine where our study population received their information concerning BIA-ALCL and BII. “News article” and “Television” were most often selected as sources of information for both BIA-ALCL and BII. This is different from other authors that states most patients hear of BIA-ALCL through health professionals or media/healthcare blogs.24 In fact, albeit openly and frequently discussed in our clinic, patients who reported first being informed about BIA-ALCL and BII from their plastic surgeons were 18% and 6%, respectively. Because most patients will probably learn about these entities from sources other than their reconstructive surgeon, it is of utmost importance that plastic surgeons discuss these entities with their patients. The obscurity regarding the clinical and pathophysiological correlation of BII and the paucity of robust scientific data supporting BII should be clearly explained to patients. It is particularly important to educate patients who have heard about BII through social media posts. In fact, social media were the third most common source among patients who knew about BII (18%), with “Internet” adding an additional 4%. Regardless of the scientific certainty surrounding BII, patients are aware of this entity and are potentially being misinformed through nonmedical sources, further stressing the importance of patient education.
In fact, patients depend heavily on information found online in general, and this is especially true for health-related information.33,34 With the recent advances in research surrounding BIA-ALCL by the plastic surgery community, a recent analysis of Google and Twitter showed an exponential increase in popularity of searches regarding both BIA-ALCL and BII.23 This same analysis demonstrated that, unfortunately, misinformation regarding BII is being spread in the process.23 Confusion between the 2 terms is possible, and disentanglement between these entities is of utmost important, as information disseminated regarding BII lacks scientific evidence. The authors do not intend to minimize the symptoms experienced by BII patients; however, further scientific evidence is needed to support the various symptoms and claims. Our patients are increasingly turning toward online platforms and social media to receive their information regarding BIA-ALCL and BII. Separating evidence-based information from anecdotal evidence is a challenging task online. As a consequence, patients are prone to developing potentially misinformed and unfounded preconceptions, which may lead to fear and distress that could otherwise be mitigated by evidence-based discussions with plastic surgeons. We must therefore be aware of the potential misinformation this has created, to then properly educate our patients and society at large. In addition, there is a non-negligible portion of patients that will request explantation or avoid implant-based reconstruction in the future based on fears surrounding BIA-ALCL or BII. In fact, in a study by Peters et al,30 75% of patients requesting explantation had received their implants for aesthetic purposes. Although it is beyond the scope of this study, it would be interesting to administer this survey among aesthetic breast augmentation patients, as we suspect they might have different perceptions compared with breast reconstruction patients.35–37
Limitations
The authors do recognize the limited generalizability of our findings, given the restriction to a single-surgeon’s practice and the moderate sample size. Although these results may not be completely representative of every breast plastic surgeons’ patient population, it serves as an adequate first step toward that endeavor. Future multicenter data should be performed to expand the generalizability of this study. As well, considering the rise in inquiries regarding “en bloc capsulectomies,” it would be interesting for future studies to include questions regarding patients’ knowledge and perception regarding implant capsules, as they relate to BIA-ALCL and BII.
CONCLUSIONS
With the recent rise in awareness around BIA-ALCL and with the growing concerns regarding BII, it is our duty, as scientists and surgeons, to continue conducting frontier research on these entities to educate our patients and the public, while limiting misinformation and potentially unfounded fears. The present survey study demonstrates there is a lacuna in breast reconstruction patients’ knowledge of both BIA-ALCL and BII, leading to negatively skewed views regarding breast implants. This highlights the importance for plastic surgeons to frequently discuss these entities with their patients, which should be done despite the obscurity of BII in an effort to offer the best available evidence to our patients.
Supplementary Material
Footnotes
Published online 23 September 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Rohrich RJ, Kaplan J, Dayan E.Silicone implant illness: science versus myth? Plast Reconstr Surg. 2019;144:98–109. [DOI] [PubMed] [Google Scholar]
- 2.Spear SL, Parikh PM, Goldstein JA.History of breast implants and the food and drug administration. Clin Plast Surg. 2009;36:15–21, v. [DOI] [PubMed] [Google Scholar]
- 3.Renwick SB.Silicone breast implants: implications for society and surgeons. Med J Aust. 1996;165:338–341. [DOI] [PubMed] [Google Scholar]
- 4.Magnusson MR, Cooter RD, Rakhorst H, et al. Breast implant illness: a way forward. Plast Reconstr Surg. 2019;1433S A Review of Breast Implant-Associated Anaplastic Large Cell Lymphoma74S–81S. [DOI] [PubMed] [Google Scholar]
- 5.Gabriel SE, O’Fallon WM, Kurland LT, et al. Risk of connective-tissue diseases and other disorders after breast implantation. N Engl J Med. 1994;330:1697–1702. [DOI] [PubMed] [Google Scholar]
- 6.Sánchez-Guerrero J, Colditz GA, Karlson EW, et al. Silicone breast implants and the risk of connective-tissue diseases and symptoms. N Engl J Med. 1995;332:1666–1670. [DOI] [PubMed] [Google Scholar]
- 7.Schusterman MA, Kroll SS, Reece GP, et al. Incidence of autoimmune disease in patients after breast reconstruction with silicone gel implants versus autogenous tissue: a preliminary report. Ann Plast Surg. 1993;31:1–6. [PubMed] [Google Scholar]
- 8.Peters W, Keystone E, Snow K, et al. Is there a relationship between autoantibodies and silicone-gel implants? Ann Plast Surg. 1994;32:1–5; discussion 5-7. [DOI] [PubMed] [Google Scholar]
- 9.Blackburn WD, Jr, Everson MP.Silicone-associated rheumatic disease: an unsupported myth. Plast Reconstr Surg. 1997;99:1362–1367. [DOI] [PubMed] [Google Scholar]
- 10.Lipworth L, Tarone RE, McLaughlin JK.Silicone breast implants and connective tissue disease: an updated review of the epidemiologic evidence. Ann Plast Surg. 2004;52:598–601. [DOI] [PubMed] [Google Scholar]
- 11.Bondurant S, Ernster V, Herdman RInstitute of Medicine Committee on the Safety of Silicone Breast I. The National Academies collection: reports funded by National Institutes of Health. In: Safety of Silicone Breast Implants. 1999Washington, DC: National Academies Press (US) National Academy of Sciences; [Google Scholar]
- 12.Janowsky EC, Kupper LL, Hulka BS.Meta-analyses of the relation between silicone breast implants and the risk of connective-tissue diseases. N Engl J Med. 2000;342:781–790. [DOI] [PubMed] [Google Scholar]
- 13.Tugwell P, Wells G, Peterson J, et al. Do silicone breast implants cause rheumatologic disorders? A systematic review for a court-appointed national science panel. Arthritis Rheum. 2001;44:2477–2484. [DOI] [PubMed] [Google Scholar]
- 14.Dush DM.Breast implants and illness: a model of psychological factors. Ann Rheum Dis. 2001;60:653–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mcguire PA, Haws MJ, Nahai F.Breast implant illness: how can we help? Aesthet Surg J. 2019;39:1260–1263. [DOI] [PubMed] [Google Scholar]
- 16.Lachmansingh DA.Breast implant illness and psychiatric implications. Ir J Psychol Med. 2019:1–2 [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Tang SY, Israel JS, Afifi AM.Breast implant illness: symptoms, patient concerns, and the power of social media. Plast Reconstr Surg. 2017;140:765e–766e. [DOI] [PubMed] [Google Scholar]
- 18.Brody GS, Deapen D, Taylor CR, et al. Anaplastic large cell lymphoma occurring in women with breast implants: analysis of 173 cases. Plast Reconstr Surg. 2015;135:695–705. [DOI] [PubMed] [Google Scholar]
- 19.Leberfinger AN, Behar BJ, Williams NC, et al. Breast implant-associated anaplastic large cell lymphoma: a systematic review. JAMA Surg. 2017;152:1161–1168. [DOI] [PubMed] [Google Scholar]
- 20.Srinivasa DR, Miranda RN, Kaura A, et al. Global adverse event reports of breast implant-associated ALCL: an international review of 40 government authority databases. Plast Reconstr Surg. 2017;139:1029–1039. [DOI] [PubMed] [Google Scholar]
- 21.Clemens MW, Brody GS, Mahabir RC, et al. How to diagnose and treat breast implant-associated anaplastic large cell lymphoma. Plast Reconstr Surg. 2018;141:586e–599e. [DOI] [PubMed] [Google Scholar]
- 22.Clemens MW, Jacobsen ED, Horwitz SM.2019 NCCN consensus guidelines on the diagnosis and treatment of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL). Aesthet Surg J. 2019;39suppl_1S3–S13. [DOI] [PubMed] [Google Scholar]
- 23.Adidharma W, Latack KR, Colohan SM, et al. Breast implant illness: are social media and the internet worrying patients sick? Plast Reconstr Surg. 2020;145:225e–227e. [DOI] [PubMed] [Google Scholar]
- 24.Lee E, Khavanin N, He W, et al. Public perceptions on breast implant–associated anaplastic large cell lymphoma. Plast Reconstr Surg Glob Open. 2019;7:107–108. [Google Scholar]
- 25.Government of Canada. Summary safety review—breast implants—assessing the potential risk of cancer (Breast implant associated anaplastic large cell lymphoma). Available at https://hpr-rps.hres.ca/reg-content/summary-safety-review-detail.php?lang=en&linkID=SSR00223. Accessed April 22, 2020.
- 26.Magnusson M, Beath K, Cooter R, et al. The epidemiology of breast implant-associated anaplastic large cell lymphoma in Australia and New Zealand confirms the highest risk for grade 4 surface breast implants. Plast Reconstr Surg. 2019;143:1285–1292. [DOI] [PubMed] [Google Scholar]
- 27.Clemens MW.Discussion: the epidemiology of breast implant-associated anaplastic large cell lymphoma in Australia and New Zealand confirms the highest risk for grade 4 surface breast implants. Plast Reconstr Surg. 2019;143:1295–1297. [DOI] [PubMed] [Google Scholar]
- 28.. Available at https://healingbreastimplantillness.com. Accessed April 29, 2020.
- 29.Fryzek JP, Signorello LB, Hakelius L, et al. Self-reported symptoms among women after cosmetic breast implant and breast reduction surgery. Plast Reconstr Surg. 2001;107:206–213. [DOI] [PubMed] [Google Scholar]
- 30.Peters W, Smith D, Fornasier V, et al. An outcome analysis of 100 women after explantation of silicone gel breast implants. Ann Plast Surg. 1997;39:9–19. [DOI] [PubMed] [Google Scholar]
- 31.Rohrich RJ, Kenkel JM, Adams WP, et al. A prospective analysis of patients undergoing silicone breast implant explantation. Plast Reconstr Surg. 2000;105:2529–2537; discussion 2538-2543. [DOI] [PubMed] [Google Scholar]
- 32.Jewell ML, Jewell HL.Breast implant-associated illness: medicine by belief, so says Dr. Google. Aesthet Surg J. 2019;39:NP87–NP89. [DOI] [PubMed] [Google Scholar]
- 33.Szychta P, Zieliński T, Rykała J, et al. Role of the internet in communication between patient and surgeon before rhinoplasty. J Plast Surg Hand Surg. 2012;46:248–251. [DOI] [PubMed] [Google Scholar]
- 34.Prestin A, Vieux SN, Chou WY.Is online health activity alive and well or flatlining? Findings from 10 years of the health information national trends survey. J Health Commun. 2015;20:790–798. [DOI] [PubMed] [Google Scholar]
- 35.Clarke A, Hansen EL, White P, et al. Low priority? A cross sectional study of appearance anxiety in 500 consecutive referrals for cosmetic surgery. Psychol Health Med. 2012;17:440–446. [DOI] [PubMed] [Google Scholar]
- 36.Morioka D, Ohkubo F.Borderline personality disorder and aesthetic plastic surgery. Aesthetic Plast Surg. 2014;38:1169–1176. [DOI] [PubMed] [Google Scholar]
- 37.Ishigooka J, Iwao M, Suzuki M, et al. Demographic features of patients seeking cosmetic surgery. Psychiatry Clin Neurosci. 1998;52:283–287. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


