Supplemental Digital Content is available in the text.
Abstract
Background:
Increasing evidence suggests that open reduction and internal fixation of condylar base fractures in adults results in improved outcomes in regard to interincisal opening, jaw movement, pain, and malocclusion. However, most of the condylar fractures are managed by maxillomandibular fixation alone due to the need for specialized training and equipment. Our aim was to present an algorithm for condylar base fractures to simplify surgical management.
Methods:
A retrospective review was performed of patients (n = 22) with condylar base fractures treated from 2016 to 2020. Patients who presented with operative fractures that require open treatment underwent 1 of 2 different techniques depending on the fracture type: a preauricular approach with a transoral approach if the condyle was dislocated (n = 2) or a transoral only approach (n = 20) in nondislocated cases. Operative time, occlusion, range of motion, and postoperative complications were assessed.
Results:
Condylar base fractures were combined with other mandibular fractures in 16 of 22 patients. Patients with condylar dislocation were managed with a preauricular approach with a secondary transoral incision (n = 2, median 147 minutes). Those without dislocation were treated with a transoral approach (n = 20, median 159 minutes). Most patients were restored to their preoperative occlusion without long-term complications.
Conclusions:
We present a simplified algorithm for treating condylar base fractures. Our case series suggests that reduction in operative time and clinical success can be achieved with open reduction and internal fixation using a transoral approach alone or in combination with a preauricular approach for dislocated fractures.
INTRODUCTION
Fractures of the mandible commonly involve the condylar head, neck, or base (subcondylar region).1–10 Despite a large and growing literature base focused on treatment options for these fractures, controversy remains on the indications for closed treatment versus open reduction and internal fixation (ORIF).1,7,9,11–18 In the past, traditional treatment for condylar base fractures was closed, due to simple application of maxillomandibular fixation (MMF) and low risk for surgical complications.1,12 Proponents of this approach cite acceptable results with decreased operative costs, no visible scars, or risk of damage to the facial nerve.15,18,19 Opponents state that closed treatment can lead to chronic malocclusion, pain, changes in jaw mobility, and need for secondary procedures.13,17,20,21
As surgical techniques and equipment have advanced, there has been a shift with more surgeons favoring ORIF.13,15,16,20,22–24 Supporters commonly state that ORIF is a safe alternative that improves ramus height with quicker return of jaw function.3,7,20,24 A recent meta-analysis, including 23 studies, looked at clinical outcomes comparing ORIF with closed treatment for condylar fractures and showed improved outcomes with open treatment in regards to interincisal opening, jaw movement, pain, and malocclusion.1 Similar findings were noted in a multicenter randomized controlled trial by Eckelt et al9 showing improved functional outcomes of moderately displaced condylar base, neck, and head fractures. However, facial nerve injury (temporary or permanent), infection, hematoma, sialocele, Frey’s syndrome, salivary fistula, and visible scar are reported complications of open treatment.3,5,11,24–26
Suggested indications for ORIF of condylar base fractures in the literature vary and often include loss of ramus height, inability to restore occlusion through closed management, foreign body in the mandible, dislocation, severe displacement, and edentulous patients.1,2,15,16,21,24 ORIF for condylar fractures encompasses a wide range of operative incisions, techniques, and plating options. Common approaches include retromandibular, submandibular, preauricular, and transoral. The choice of incision is often determined by surgeon preference and location of the fracture.2
Introduction of 3-dimensional (3D) condylar plates greatly aids the transoral approach by simplifying fixation using a single plate without compromising biomechanical strength when compared with 2-plate fixation.27 The transoral approach has the benefit of reducing the risk of facial nerve injury and scarring.2,6,7,11,12,17,26,28–30 However, despite availability of technology to facilitate transoral fixation and fracture visualization using an endoscope and lighted retractors, the technique is not widely accepted.26,31 There remains concern over the steep learning curve and potential increase in operative time with this method.2,5,24,26,30,32
With such a wide range of operative treatments, it can be challenging for surgeons to decide which patients would benefit most from each surgical option. Herein, we present our case series using a simplified algorithm for management of condylar base fractures with or without dislocation.
MATERIALS AND METHODS
Patients and Study Design
An Institutional Review Board approved retrospective chart review was performed at a single tertiary academic medical center from March 2016 to January 2020 of patients (n = 22) with operative condylar base fractures of the mandible. Location of fractures were classified based on the AO craniomaxillofacial (AOCMF) classification system.23 Additional patient characteristics, mandible fractures, operative time (from incision to closure), postoperative occlusion, maximum interincisal opening, and postoperative complications were obtained from the electronic medical record. The patients were divided into 2 groups; patients without condylar dislocation (n = 20) were managed via transoral approach only, while the dislocated group (n = 2) were treated using a preauricular incision with the transoral approach.
Surgical Algorithm
An algorithm was created for condylar base fractures starting with assessment of occlusion (Fig. 1). Patients without malocclusion or displacement (no loss of vertical ramus height) were treated nonoperatively with a soft diet for 4–6 weeks. Condylar base fractures with maintenance of ramus height and malocclusion due to a second mandibular fracture were managed with ORIF of the second fracture and MMF until the condylar fracture was clinically healed. Displaced condylar base fractures causing a loss of vertical height and malocclusion were treated with a transoral approach with percutaneous screw placement via a transbuccal trocar. Condylar base fractures with a dislocated condylar head were managed with a combined preauricular and transoral approach. 3D condylar plates (KLS Martin [Jacksonville, Fla.] or Stryker Craniomaxillofacial [Kalamazoo, Mich.]) were used to aid in the reduction and fixation of the fracture (Fig. 2). In patients with secondary mandible fractures, vertical ramus height was assessed by computed tomography and occlusion was assessed intraoperatively after fixation of the non-condylar base fractures to determine management per the algorithm.
Fig. 1.
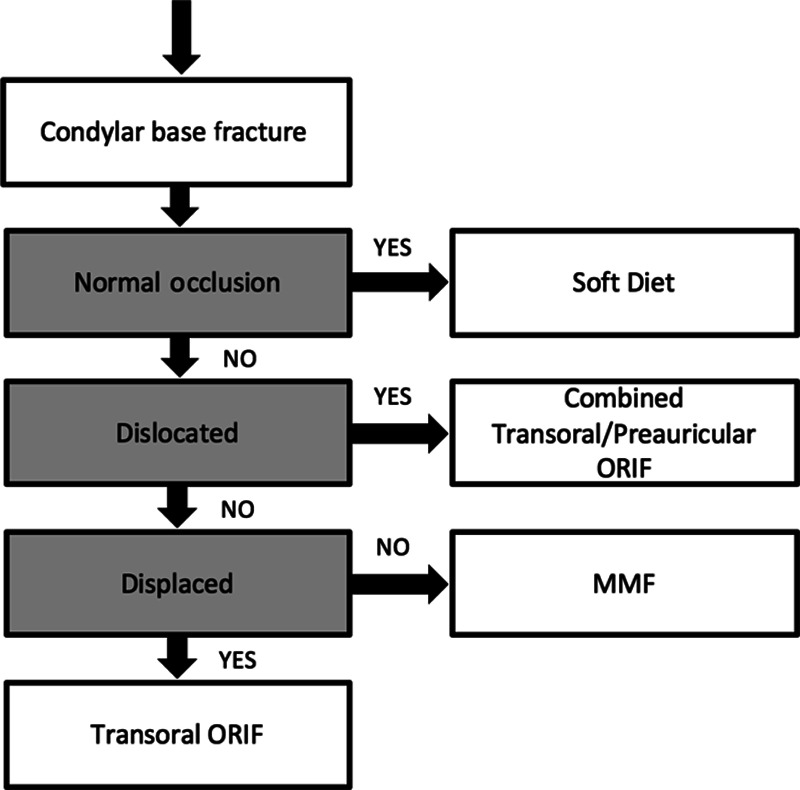
Algorithm for patients with condylar base fractures assessing occlusion, dislocation, and fracture displacement.
Fig. 2.
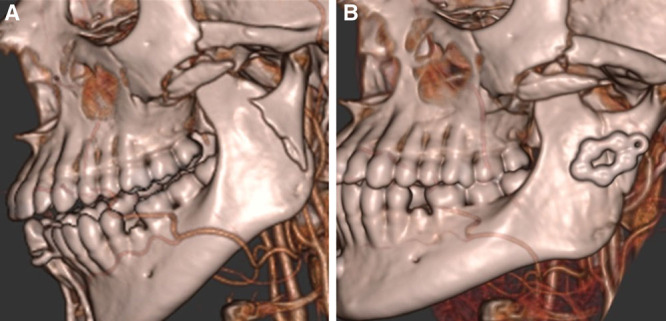
Preoperative (A) and postoperative (B) lateral view computed tomography images after open reduction and internal fixation using transoral approach and a 3D condylar plate. This patient had a displaced condylar base fracture without condylar dislocation in conjunction with a symphyseal fracture.
Surgical Technique
Condylar base fractures were diagnosed radiographically using the AOCMF classification system.23 Condylar head and neck fractures without a concurrent condylar base fracture were excluded from this study. Dislocation was identified radiographically where the entire condylar head is displaced out of the fossa limits.
Surgical approaches included the preauricular and transoral techniques. Per the condylar base algorithm (Fig. 1), the preauricular approach as previously described by Ellis and Zide33 was used if the proximal condylar segment was dislocated. Once the temporomandibular joint and proximal condylar segment was identified, reduction of the temporomandibular dislocation was aided by simultaneous manual downward pressure on the mandible. An MMF screw was positioned in the condylar head and a wire was placed through the screw to help maintain reduction before fixation. The MMF screw was removed from the condylar head after fixation of the mandibular fractures and the temporomandibular joint capsule and the superficial musculoaponeurotic system were closed. Alternative options for controlling the condylar head during reduction that do not require placing an additional MMF screw include temporary suture or wire around the condylar head.
The transoral approach, as previously described by Kanno et al7 and the AO Foundation, was used in the presence of displacement, resulting in loss of vertical ramus height and malocclusion.34 The patient was placed in centric occlusion using MMF. The mucosal incision along the oblique line was placed inferior to the occlusal plane to avoid the buccal fat pad and buccal nerve, and lateral to the mucogingival junction to facilitate mucosal closure. Subperiosteal dissection was performed up the anterior edge of the ascending ramus with an Obwegeser ramus retractor and blunt periosteal elevators in the plane between the anterior temporalis fibers and the bone. A lighted Bauer sigmoid notch retractor (Electrosurgical Instrument, Rochester, N.Y.) was placed in the sigmoid notch to provide visualization of the fracture. A transbuccal system was used with the trocar coming through at the level of the fracture line. The plate was fixed into the proximal condylar segment. The transbuccal trocar handle with drill sleeve was placed in one of the distal screw holes of the plate to allow for manipulation of the condylar segment. Reduction can be checked with a 4-mm 30-degree endoscope. (See figure, Supplemental Digital Content 1, which displays endoscopic view of percutaneous screw placement during open reduction internal fixation of condylar base fractures, http://links.lww.com/PRSGO/B475.) After reduction was obtained of the condylar base fracture, 2–3 screws were placed in the distal segment. Our goal was to place at minimum two screws on either side of the fracture, but if access was easy to the third screw hole, an additional screw was placed.
Statistical Analysis
Descriptive statistics and figures were generated using Excel 2013 (Microsoft, Redmond Wash.) with a 1-tail. A 1-tailed bivariate Pearson’s correlation test was performed to compare the time of surgery to the order in which patients underwent repair. The correlation coefficient and significance were calculated using IBM SPSS Statistics v 26 (IBM Corp., Armonk, N.Y.) Significance was set a priori at P < 0.05.
RESULTS
Preoperative Factors and Demographics
Preoperative patient factors and demographics are described in Table 1. Most patients were young (median 33 years) assaulted (64%) men (73%) with high rates of tobacco smoking (59%). Patient ages ranged from 16 to 49 years. Most condylar base fractures were combined with other mandible fractures (73%).
Table 1.
Patient Demographics
| Patients (n = 22) | |
|---|---|
| Age (median), y | 33 |
| IQR 24.3–37.8 | |
| Sex | 16 (73%) man |
| 6 (27%) woman | |
| Co-morbidities | 5 (23%) psychiatric diagnoses |
| 4 (18%) polysubstance abuse | |
| Smoking status | 13 (59%) smoker |
| 9 (41%) nonsmoker | |
| Injury mechanism | 14 (64%) assault |
| 3 (14%) MVC | |
| 2 (9%) fall | |
| 2 (9%) sports | |
| 1 (5%) GSW | |
| Other mandible fractures | 13 (59%) para/symphyseal |
| 3 (14%) body/angle | |
| 1 (5%) coronoid |
GSW, gunshot wound; IQR, interquartile range; MVC, motor vehicle collision.
Injury Pattern and Operative Time
Injury pattern and operative times are listed by the operative technique in Table 2. The median time interval between injury and surgery was 7 days, with a range of 1–18 days. Operative times based on dislocated and isolated condylar base fractures are shown in Figure 3.
Table 2.
Operative Times and Surgical Approaches for Each Patient Case
| Patient | Sex/Age, y | Fracture Side | Associated Mandibular Fracture | Operative Time, min | Approach | Complications |
|---|---|---|---|---|---|---|
| 1 | M/33 | R | L vertical ramus, L parasymphyseal | 260 | Transoral, perc. trocar | |
| 2 | M/48 | L | R parasymphyseal, L angle | 153 | Transoral, perc. trocar | |
| 3 | M/31 | R | L parasymphyseal | 164 | Transoral, perc. trocar | Malocclusion |
| 4 | M/49 | R | L body | 199 | Transoral, perc. trocar | |
| 5 | M/33 | R | R parasymphyseal | 133 | Transoral, perc. trocar | |
| 6 | F/24 | L | R parasymphyseal | 165 | Transoral, perc. trocar | |
| 7 | M/33 | L | 111 | Transoral, perc. trocar | ||
| 8 | M/38 | L | R parasymphyseal | 171 | Transoral, perc. trocar | |
| 9 | M/31 | R | L symphyseal | 100 | Transoral, perc. trocar | |
| 10 | F/25 | L | R symphyseal | 111 | Transoral, endoscope | |
| 11 | M/22 | R | L parasymphyseal | 166 | Transoral, perc. trocar | Cellulitis |
| 12 | M/39 | L | L parasymphyseal | 167 | Transoral, perc. trocar | |
| 13 | M/41 | L | 77 | Transoral, perc. trocar, endoscope | ||
| 14 | M/35 | R | L parasymphyseal | 214 | Transoral, perc. trocar, endoscope | Limited jaw opening |
| 15 | F/35 | L | R condylar head, R parasymphyseal | 148 | Transoral, perc. trocar | |
| 16 | M/43 | BL | L coronoid | 139 | Transoral, perc. trocar | Mild jaw deviation, limited jaw opening |
| 17 | F/16 | R | 169 | Transoral, perc. trocar | Mild jaw deviation | |
| 18 | F/22 | R | L parasymphyseal | 277 | Transoral, perc. trocar | |
| 19 | M/29 | R | 76 | Transoral, perc. trocar | ||
| 20 | M/37 | L | 127 | Transoral, perc. trocar, endoscope | Mild jaw deviation | |
| 21* | M/20 | L | 116 | Preauricular, transoral | Mild jaw deviation | |
| 22* | F/17 | L | R angle | 178 | Preauricular, transoral, endoscope |
Dislocated condylar head.
BL, bilateral; L, left; Perc, percutaneous; R, right.
Fig. 3.
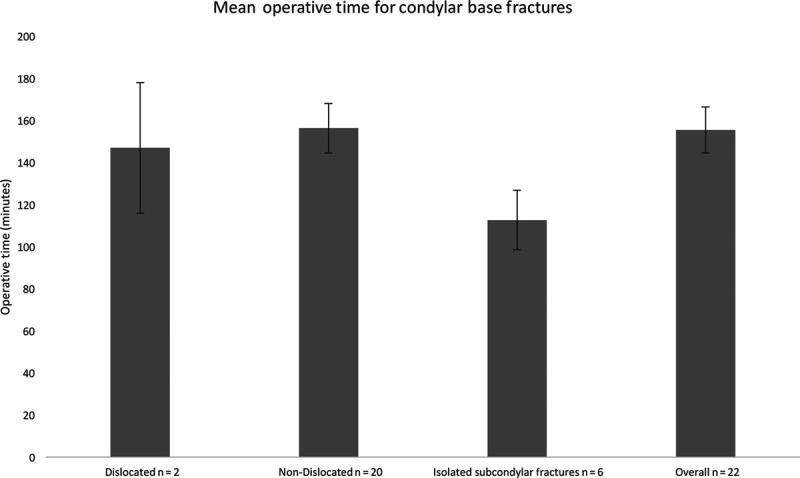
Graphs showing mean operative times for patients presenting with condylar base fractures.
After implementation of the condylar base fracture algorithm, the average operating time from incision to closure was 156 minutes (n = 22, median 159 minutes, range, 76–277 minutes). For dislocated fractures the operative times were 116 and 178 minutes. Patients with nondislocated fractures were managed with a transoral incision with an average operating time of 156 minutes (n = 20, median 159 minutes; range, 76–277 minutes).
There were 6 patients who had an isolated condylar base fracture without a second mandibular fracture. The average operating time for these cases was 113 minutes (n = 6, median 114 minutes; range, 76–169 minutes). One of the isolated condylar base fractures was dislocated (operating time, 116 minutes) and 5 were nondislocated (average operating time, 112 minutes).
The transoral only operative approach was used in 20 cases between 2016 and 2020. The change in operating time over the time course of this study was from an average of 187 minutes in 2016, to 161 minutes in 2017–2018, to 136 minutes in 2019–2020 (Fig. 4).
Fig. 4.
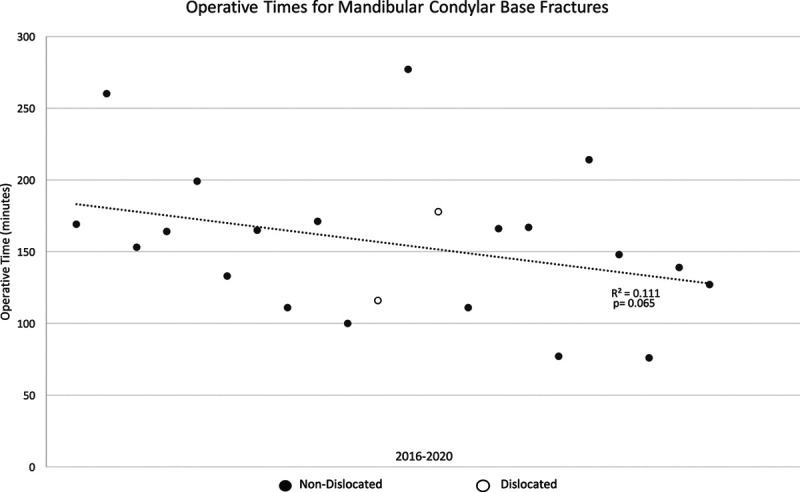
Scatter plot showing change in operative times operative times over the time course of this study.
Most patients with combined mandibular fractures required MMF. Median duration of MMF was 2 weeks (range of 1.5–4 weeks) All patients were prescribed a soft diet for 6 weeks. Physiotherapy to encourage maximal jaw excursion was offered in the form of home exercises.
Outcomes and Adverse Events
Most of the patients postoperatively were restored to prefracture occlusion and range of motion. Median follow-up was 38 days postoperatively, which ranged from 11 to 83 days. Complications included 4 cases of mild jaw deviation on mouth opening, 1 case of cellulitis around an external incision, and 1 case of malocclusion. Malocclusion documented as 1 mm contralateral posterior open bite at 6 weeks postoperative was caused by bone resorption concerning for osteomyelitis of the concurrent parasymphyseal fracture. In total, 14 patients had documented postoperative maximal interincisal opening. Of the measurements that occurred at least 2 weeks after MMF was removed, 3 of 14 patients were documented as less than full jaw opening. One patient had a jaw opening of 25 mm at 9 weeks postoperatively, one of 25 mm at 6 weeks, and the other 10 mm at 8 weeks. These patients were given a home exercise program to help with their range of motion, and they did not return to clinic to document improved jaw opening.
DISCUSSION
The results of this study suggest that in our experience, patients with condylar base fractures can be managed safely with implementation of a simplified algorithm to aid surgeon decision-making. We found that patients with condylar dislocations could be managed with a combined preauricular and transoral approach, while displaced condylar base fractures could be managed with a transoral approach. With these techniques, the majority of patients were restored to premorbid occlusion and range of motion postoperatively. After implementation of the algorithm, condylar base operative time has decreased and simplified the decision-making process.
Patients with displaced, but nondislocated fractures underwent surgery through a transoral approach (n = 20). The authors prefer this surgical incision as it minimizes the risk of facial nerve palsy.6,11,12,26,28–30 Some surgeons find this approach difficult due to limited exposure of the fracture.5,6,17,31 The authors overcome this issue by using a lighted sigmoid notch retractor (Electrosurgical Instrument) for improved visualization and a transbuccal trocar for plate placement. In 2 patients who preceded this study, fixation was performed with a right angle drill and screwdriver via the transoral approach. In each case, operative time was prolonged (285 and 196 minutes). Despite studies stating the ease of use of an angulated system,7,17,31 we found the drill hole to be of poor quality and the screwdrivers difficult to handle. In 5 of the cases (between 2018 and 2020), we utilized an endoscope to aid in fracture visualization; however, an endoscope is not required. There is often cited concern about the learning curve of a transoral endoscopic-assisted approach with the possibility of increased operative times.6,26,30 Operative times in our study trended toward shorter operations over time, but did not reach statistical significance in our patient cohort. Endoscope use did not negatively affect operating time (average 141 minutes versus 160 minutes without an endoscope).
Dislocated fractures were treated with a combined preauricular and transoral approach. It is very difficult to reduce a medially dislocated condyle with a purely transoral approach2,11,29 and the preauricular approach provides great access to the temporomandibular joint.2,5 In this patient population, 2 of 22 patients had a dislocated condylar base fracture. Dislocation is discussed less in the literature than displacement. It is an important group of fractures to study, as this group is associated with greater overall morbidity.16 Zachariades et al21 found that 19% of all condylar fracture types were dislocated. Zhang et al35 studied a population of severely dislocated pediatric condyle fractures who underwent ORIF with bioabsorbable plates and a preauricular incision approach. All patients did well postoperatively without any complications.35 While this study only includes our surgeons’ experience and preferences in a small patient population, it still provides a detailed surgical approach for consideration when encountering dislocated condylar base fractures.
A variety of plates were utilized in this study, and numerous fixation methods have been described in the literature, such as single or double miniplates, 3D shapes, compression plates, or dissolving plates.4,14,36 Several studies show increased complication rates, including loosening of screws and fracturing plates when a single miniplate is used, but this has to be balanced with the limited space on the condylar surface for fixation.4,20,21,36 Three-dimensional plates combine the ease of applying one plate with the additional fracture stability similar to a 2-plate system.27,37 There were no cases of plate fracturing in our patient population. The ultimate goal of fixation is to obtain anatomic reduction of the condylar base fracture using the appropriate plating system (Fig. 2). In contrast, the key principle in closed treatment using MMF only is to obtain appropriate ramus height using dental occlusion as a guide without direct bony manipulation to reduce the fracture. We believe this principle also guides treatment when performing ORIF of a condylar base fracture via the transoral approach. Figures 5 and 6 illustrates normalization of occlusion and incisal opening with restoration of ramus height, but without complete anatomic reduction of the fracture.
Fig. 5.
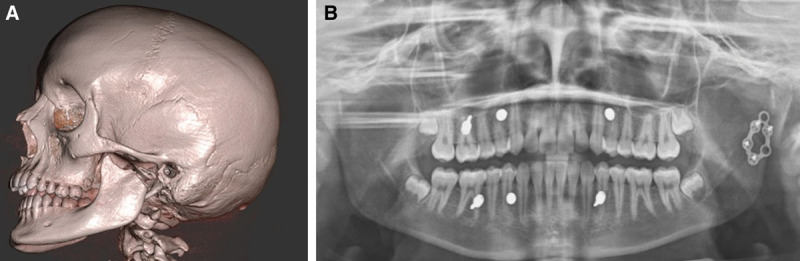
(A) Preoperative computed tomography image showing dislocated condylar fracture; (B) 4-weeks postoperative x-ray after open reduction and internal fixation.
Fig. 6.
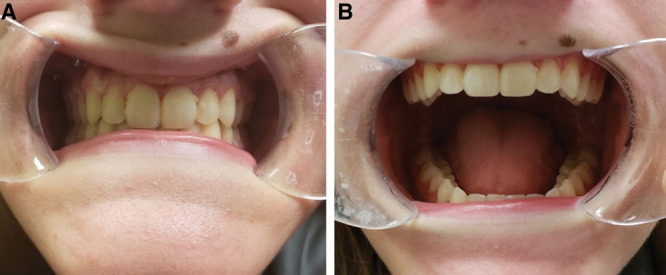
Four weeks after fixation of a left dislocated condylar base fracture (A) in centric occlusion; (B) maximal incisal opening.
Several other studies have published algorithms for similar condylar base fracture populations. Hackenberg et al’s12 published algorithm divided patients by occlusion, displacement, and several other factors between closed, open, and endoscopic treatment. We expanded on this study with the inclusion of dislocated fractures and the discussion of operative times between groups. Haug and Brandt13 have also published treatment guidelines using closed treatment for cases without malocclusion, pain, or restricted range of motion and open treatment for those with unstable occlusion, loss of rami height, and displacement. They do not advocate for endoscopic use due to increased operative times.13 Lee et al’s16 group provided a treatment algorithm based on higher versus lower condylar fractures, but also did not include dislocation in the algorithm. Landes and Lipphardt15 determined that displacement and dislocation were better markers for open treatment than malocclusion when there were other mandible fractures. We chose to include all 3 measures in our treatment algorithm, but agree that the high rate of other mandibular fractures in this patient population makes determining occlusion based solely on the condylar base fracture difficult. Reddy et al38 also published a treatment guideline separating patients first by age and then condylar fracture location. Their group used a similar guideline with displaced and dislocated fractures of the condylar base in adults receiving ORIF. In their study, they used a retromandibular approach and cited a 24% rate of temporary facial nerve palsy.38 We hoped to improve on this percentage of facial nerve palsy and the potential for poor external scarring with a transoral approach.
This algorithm was designed to help ease the surgical decision making for condylar base fractures whose treatment remains controversial in the literature. Our approach is unique in its inclusion of a separate arm for dislocated fractures and its surgical approaches. This study also incorporates a percutaneous trocar with or without an endoscope, which allows surgeons the ability to use either method depending on their comfort with the equipment. We feel that the simplicity of the algorithm makes it easy for other surgeons to adopt in their practice.
This study is not without limitations and the patients represent only 1 surgical center’s data and surgeons’ experience. This retrospective case series did not randomize patients before the use of the algorithm; so it is unclear what outcomes the surgically treated patients would have had with other approaches. The median follow-up was 38 days, but several patients were only seen postoperatively for the first 1–2 weeks. While the authors feel that the follow-up period was adequate to assess outcomes and occlusion in most patients, there may be complications missed owing to a lack of patient long-term follow-up. Ideally, these patients would return for follow-up for at least 4 months or until complications such as limited jaw opening resolved. Despite several phone calls, we were unable to reach several of the patients after the early postoperative period. There were also several patients missing information on range of motion and incisal opening. This study included a majority of patients with additional mandibular fractures, which complicates assessing operative time and difficulty of some of the cases. While our study’s results suggest the ease of use of this algorithm, every condylar base fracture and patient is unique, and still require surgeon decision making on an individual patient basis. The decision to perform ORIF versus closed reduction with or without MMF needs to take into account the anatomy of the condylar base fracture, surgeon preference, and patient preference.
Supplementary Material
Footnotes
Published online 24 September 2020.
Disclosure: Dr. Patel is a consultant for Stryker CMF; Drs. Chi and Patel are course faculty member for AOCMF. All the other authors have no financial interest to declare.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Al-Moraissi EA, Ellis E., IIISurgical treatment of adult mandibular condylar fractures provides better outcomes than closed treatment: a systematic review and meta-analysis. J Oral Maxillofac Surg. 2015;73:482–493. [DOI] [PubMed] [Google Scholar]
- 2.Cranford J, Kadakia S, Sawhney R, et al. Contemporary issues in the open management of subcondylar fractures of the mandible. Facial Plast Surg. 2016;32:424–430. [DOI] [PubMed] [Google Scholar]
- 3.Bindra S, Choudhary K, Sharma P, et al. Management of mandibular sub condylar and condylar fractures using retromandibular approach and assessment of associated surgical complications. J Maxillofac Oral Surg. 2010;9:355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bischoff EL, Carmichael R, Reddy LV.Plating options for fixation of condylar neck and base fractures. Atlas Oral Maxillofac Surg Clin North Am. 2017;25:69–73. [DOI] [PubMed] [Google Scholar]
- 5.D’Agostino A, Trevisiol L, Procacci P, et al. Is the retromandibular transparotid approach a reliable option for the surgical treatment of condylar fractures? J Oral Maxillofac Surg. 2017;75:348–356. [DOI] [PubMed] [Google Scholar]
- 6.Emam HA, Jatana CA, Ness GM.Matching surgical approach to condylar fracture type. Atlas Oral Maxillofac Surg Clin North Am. 2017;25:55–61. [DOI] [PubMed] [Google Scholar]
- 7.Kanno T, Sukegawa S, Fujioka M, et al. Transoral open reduction with rigid internal fixation for subcondylar fractures of the mandible using a small angulated screwdriver system: is endoscopic assistance necessary? J Oral Maxillofac Surg. 2011;69:e372–e384. [DOI] [PubMed] [Google Scholar]
- 8.Marker P, Nielsen A, Bastian HL.Fractures of the mandibular condyle. Part 1: patterns of distribution of types and causes of fractures in 348 patients. Br J Oral Maxillofac Surg. 2000;38:417–421. [DOI] [PubMed] [Google Scholar]
- 9.Eckelt U, Schneider M, Erasmus F, et al. Open versus closed treatment of fractures of the mandibular condylar process—a prospective randomized multi-centre study. J Cranio Maxillofac Surg. 2006;34:306–314. [DOI] [PubMed] [Google Scholar]
- 10.Sharif MO, Fedorowicz Z, Drews P, et al. Interventions for the treatment of fractures of the mandibular condyle. Cochrane Database Syst Rev. 2010:CD006538. [DOI] [PubMed] [Google Scholar]
- 11.Anehosur V, Kulkarni K, Shetty S, et al. Clinical outcomes of endoscopic vs retromandibular approach for the treatment of condylar fractures—a randomized clinical trial. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;128:479–484. [DOI] [PubMed] [Google Scholar]
- 12.Hackenberg B, Lee C, Caterson EJ.Management of subcondylar mandible fractures in the adult patient. J Craniofac Surg. 2014;25:166–171. [DOI] [PubMed] [Google Scholar]
- 13.Haug RH, Brandt MT.Closed reduction, open reduction, and endoscopic assistance: current thoughts on the management of mandibular condyle fractures. Plast Reconstr Surg. 2007;1207 suppl 290S–102S. [DOI] [PubMed] [Google Scholar]
- 14.Lechler C, Probst F, Cornelius CP, et al. Open reduction and internal fixation of mandibular condylar base and neck fractures using strut plates. J Oral Maxillofac Surg. 2018;76:1494–1503. [DOI] [PubMed] [Google Scholar]
- 15.Landes CA, Lipphardt R.Prospective evaluation of a pragmatic treatment rationale: open reduction and internal fixation of displaced and dislocated condyle and condylar head fractures and closed reduction of non-displaced, non-dislocated fractures. Part I: condyle and subcondylar fractures. Int J Oral Maxillofac Surg. 2005;34:859–870. [DOI] [PubMed] [Google Scholar]
- 16.Lee JW, Lee YC, Kuo YL.Reappraisal of the surgical strategy in treatment of mandibular condylar fractures. Plast Reconstr Surg. 2010;125:609–619. [DOI] [PubMed] [Google Scholar]
- 17.Nam SM, Kim YB, Cha HG, et al. Transoral open reduction for subcondylar fractures of the mandible using an angulated screwdriver system. Ann Plast Surg. 2015;75:295–301. [DOI] [PubMed] [Google Scholar]
- 18.Danda AK, Muthusekhar MR, Narayanan V, et al. Open versus closed treatment of unilateral subcondylar and condylar neck fractures: a prospective, randomized clinical study. J Oral Maxillofac Surg. 2010;68:1238–1241. [DOI] [PubMed] [Google Scholar]
- 19.Rozeboom AVJ, Dubois L, Bos RRM, et al. Closed treatment of unilateral mandibular condyle fractures in adults: a systematic review. Int J Oral Maxillofac Surg. 2017;46:456–464. [DOI] [PubMed] [Google Scholar]
- 20.Choi BH, Yi CK, Yoo JH.Clinical evaluation of 3 types of plate osteosynthesis for fixation of condylar neck fractures. J Oral Maxillofac Surg. 2001;59:734–737; discussion 738. [DOI] [PubMed] [Google Scholar]
- 21.Zachariades N, Mezitis M, Mourouzis C, et al. Fractures of the mandibular condyle: a review of 466 cases. Literature review, reflections on treatment and proposals. J Craniomaxillofac Surg. 2006;34:421–432. [DOI] [PubMed] [Google Scholar]
- 22.Ellis E., IIIMethod to determine when open treatment of condylar process fractures is not necessary. J Oral Maxillofac Surg. 2009;67:1685–1690. [DOI] [PubMed] [Google Scholar]
- 23.Neff A, Cornelius CP, Rasse M, et al. The comprehensive AOCMF classification system: condylar process fractures—level 3 tutorial. Craniomaxillofac Trauma Reconstr. 2014;7suppl 1S044–S058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rozeboom A, Dubois L, Bos R, et al. Open treatment of unilateral mandibular condyle fractures in adults: a systematic review. Int J Oral Maxillofac Surg. 2017;46:1257–1266. [DOI] [PubMed] [Google Scholar]
- 25.Ellis E, III, McFadden D, Simon P, et al. Surgical complications with open treatment of mandibular condylar process fractures. J Oral Maxillofac Surg. 2000;58:950–958. [DOI] [PubMed] [Google Scholar]
- 26.Pau M, Navisany K, Reinbacher KE, et al. Use of a modified high submandibular approach to treat condylar base fractures: experience with 44 consecutive cases treated in a single institution. J Craniomaxillofac Surg. 2016;44:1641–1645. [DOI] [PubMed] [Google Scholar]
- 27.Lauer G, Pradel W, Schneider M, et al. A new 3-dimensional plate for transoral endoscopic-assisted osteosynthesis of condylar neck fractures. J Oral Maxillofac Surg. 2007;65:964–971. [DOI] [PubMed] [Google Scholar]
- 28.Schiel S, Mayer P, Probst F, et al. Transoral open reduction and fixation of mandibular condylar base and neck fractures in children and young teenagers—a beneficial treatment option? J Oral Maxillofac Surg. 2013;71:1220–1230. [DOI] [PubMed] [Google Scholar]
- 29.Schön R, Gutwald R, Schramm A, et al. Endoscopy-assisted open treatment of condylar fractures of the mandible: extraoral vs intraoral approach. Int J Oral Maxillofac Surg. 2002;31:237–243. [DOI] [PubMed] [Google Scholar]
- 30.Loukota RA.Endoscopically assisted reduction and fixation of condylar neck/base fractures—the learning curve. Br J Oral Maxillofac Surg. 2006;44:480–481. [DOI] [PubMed] [Google Scholar]
- 31.Vajgel A, Santos Tde S, Camargo IB, et al. Treatment of condylar fractures with an intraoral approach using an angulated screwdriver: results of a multicentre study. J Craniomaxillofac Surg. 2015;43:34–42. [DOI] [PubMed] [Google Scholar]
- 32.Kim BK, Kwon YD, Ohe JY, et al. Usefulness of the retromandibular transparotid approach for condylar neck and condylar base fractures. J Craniofac Surg. 2012;23:712–715. [DOI] [PubMed] [Google Scholar]
- 33.Ellis E, Zide MF.Surgical Approaches to the Facial Skeleton. 2005Philidelphia, Pa.: LWW; [Google Scholar]
- 34.Scott Bartlett M, Ehrenfeld GM, Sugar AAO Surgery Reference. Transoral approach to the mandible angle. AO Surgery Reference:2012. Available at https://surgeryreference.aofoundation.org. Accessed February 9, 2020.
- 35.Zhang B, Liu ZH, Li J, et al. Open reduction and internal fixation of severely dislocated fractures of condylar neck and base using bioabsorbable miniplate in children: a 3–10 years follow-up study. Int J Pediatr Otorhinolaryngol. 2014;78:1987–1992. [DOI] [PubMed] [Google Scholar]
- 36.Marwan H, Sawatari Y.What is the most stable fixation technique for mandibular condyle fracture? J Oral Maxillofac Surg. 2019;77:2522.e1–2522.e12. [DOI] [PubMed] [Google Scholar]
- 37.Ahuja SA, Galinde J, Asnani U, et al. Comparative evaluation of clinical outcomes using delta plates and conventional miniplates for internal fixation of mandibular condylar fractures in adults. J Oral Maxillofac Surg. 2018;76:1255–1266. [DOI] [PubMed] [Google Scholar]
- 38.Reddy NV, Reddy PB, Rajan R, et al. Analysis of patterns and treatment strategies for mandibular condyle fractures: review of 175 condyle fractures with review of literature. J Maxillofac Oral Surg. 2013;12:315–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


