Supplemental Digital Content is available in the text.
Abstract
Background:
Long-term results and efficacy of nasoalveolar molding (NAM) on the perinasal region are reported controversially in the literature. With this study, we demonstrate our experiences, contribute to the ongoing discussion, and describe our decision-making when NAM is indicated or not.
Methods:
Conventional pre- and postinterventional photographs of patients with nonsyndromic unilateral and bilateral cleft lip and palate (UCLP and BCLP) were analyzed. The 2 independent raters were blinded to therapy (NAM versus non-NAM), and 7 parameters were measured. Intraclass correlation coefficient for intra- and interrater reliability was calculated. The Mann–Whitney U test was performed to compare therapy- and appearance-matched pairs. Finally, 30 specialists in cranio-maxillofacial surgery performed a subjective, blinded rating of matched NAM and non-NAM cases.
Results:
Thirty-six patients, 16 UCLP and 20 BCLP, were enrolled. The intraclass correlation coefficients for intra- and interrater reliability were excellent for all measurements, except for nasal sill (0.77 intrarater and 0.80 interrater). Height-to-width ratio (P = 0.012) was significantly different in the comparison of non-NAM and NAM-treated severe cases with UCLP. Thirty blinded raters evaluated NAM-treated cases with severe UCLP better than matched non-NAM cases. Non-NAM-treated cases with moderate UCLP and BCLP were rated better than matched NAM cases.
Conclusions:
Children with severe UCLP may benefit from NAM therapy in the sense of better symmetry and a more homogenous appearance. Patients with moderate UCLP and BCLP did not benefit, and the risk of the burden of care increased.
INTRODUCTION
Nasoalveolar molding (NAM) is a presurgical, orthofacial technique for the treatment of patients presenting with cleft lip and palate. This method is based on the remaining plasticity of the nasal cartilages of neonates in the first months of life.1 But NAM therapy should not be started too early and must be adapted in preterm birth because undesired force conduction to the anterior skull base might occur.2 NAM is commonly performed according to the treatment algorithm described by Grayson et al., but several modifications are also reported in the literature, including CAD/CAM solutions.3–6
Nevertheless, the usefulness, effectiveness, and long-term stability of NAM therapy have been a matter of ongoing controversial discussions in the literature.7–10 Only a small number of long-term results have been published and discussed11; so it has to be considered critical if there is an indication for NAM or not. Furthermore, this presurgical treatment modality needs regular adjustments of the NAM appliance and therefore is strongly dependent on parental compliance.12 In this context, the burden of care for NAM therapy is a well-known problem and therefore this therapy is associated with a reported noncompletion rate between 13.5% and 32.5% in the literature.13,14
Short-term results are reported to be promising, with better symmetry in patients with unilateral cleft lip and palate (UCLP) and with increased elongation of the columella in patients with bilateral cleft lip and palate (BCLP).14–16 More recently, favorable long-term results have been described, revealing a previously described assumption that NAM therapy might reduce the need for secondary corrections.7,11,17,18
Symmetry plays an important role in postoperative follow-up, facial aesthetics, and subjective perception of oneself and by others in social interaction.19 Different tools have been described to analyze symmetry, including SymNose or techniques described by Barillas et al. and Chang et al.7,20,21
The purpose of this retrospective study was to analyze photographs of therapy- and appearance-matched patients who were treated either with or without NAM and operated by only 1 surgeon. In addition, we provide a critical description of our decision-making regarding our indication for NAM therapy.
MATERIALS AND METHODS
Ethical Statement
All clinical investigations and procedures were conducted according to the principles expressed in the Declaration of Helsinki. Ethical approval for the retrospective study was granted by the Ethical Committee of the Technical University of Munich School of Medicine (Approval No. 275/18S).
Treatment Algorithm
A feeding plate was inserted within two days of birth. In the following days, the detailed, staged treatment algorithm of cleft lip and palate—including NAM therapy—was explained to all parents as part of an enlightenment and treatment talk (informed decision-making). Besides the general treatment information, we informed the parents about potential financial contributions or deterrent fees that might occur due to NAM therapy because it is not continuously covered by the insurance companies. Finally, the parents decided whether they wanted NAM therapy to be performed or not on the basis of this information.
In cases of NAM therapy, the procedure was started within the first two weeks of life and with respect to a corrected age in the case of preterm birth.2 NAM therapy consisted of alveolar molding (6–8 weeks) and subsequent nasal molding (until operation).14,22
All surgical procedures were performed by the first author and with the same techniques for primary cheilo- and palatoplasty. Primary cheiloplasty in UCLP in both non-NAM and NAM groups was performed using the technique described by Millard, with an additional subtle primary rhinoplasty at the age of 3–4 months or when a bodyweight of at least 5 kg was reached. The rhinoplasty included the mobilization along the anterior nasal spine and the nasal septum and careful preparation of the depressed lateral cartilage without additional incision, resulting in a reliable mobilization of soft tissue at the alar base. Furthermore, a complete and meticulous release of misled orbicularis oris muscle sling was performed by undermining the skin. Primary palatoplasty was performed by reconstruction of the muscle sling in combination with a simultaneous palatine and vomer flap at the age of 9–12 months.
Records and Measurements
The study includes the archived data from the Department of Oral and Maxillofacial Surgery, School of Medicine, Technical University of Munich, Klinikum rechts der Isar for comparative analyses.
Images in frontal and submental views of every child were taken. Photographs were taken in a quiet and unemotional room. Children and parents were instructed to be calm and to keep a neutral facial expression, as described by others.23 All photographs (camera body, Nikon D40; Japan; lens, Nikkor AF-S micro 600 mm 1:2.8 G ED; Nikon, Japan) were cropped in a rectangular shape, focusing on the perinasal and -oral region using Adobe Photoshop (Adobe Photoshop, CS 5.1 Version 12.1).
All measurements were performed by 2 independent investigators (L.M.R. and F.D.G.), who were blinded from the treatment history (non-NAM versus NAM). All photographic analyses were performed twice using ImageJ (ImageJ 1.410, National Institutes of Health, Bethesda, Md., USA)24 to further analyze the intrarater reliability. A second analysis was performed with an interval of 7–14 days to minimize a habitual landmark setting.
Before analysis, all cases were systematically subclassified (moderate or severe) according to the severity of the UCLP or BCLP. A UCLP case was subclassified as “severe” in cases of wide lip, alveolar and palatal clefting, deviation of the columella, and deformation of the ipsilateral nostril. A BCLP case was subclassified as “severe” in cases of short columella, deviation of the premaxilla and wide lip, alveolar, and palatal clefting (Fig. 1).
Fig. 1.

Classification according to the severity of cleft lip and palate. Representative photographs (camera body: Nikon D40; Japan; lens: Nikkor AF-S micro 600 mm 1:2.8 G ED; Nikon, Japan) of cases with moderate (A and C) and severe (B and D) subclassified unilateral (A and B) and bilateral (C and D) cleft lip palate.
The structured photographic analysis included nostril height (NH), nostril width (NW), one-fourth medial part of nostril height (¼ med. part), nostril area, inner nostril height-to-width ratio (H-t-W), and columella angle (ColAng) as described by Chang et al.21 For this purpose, an additional horizontal reference line connecting the most inward point with the outer lateral borders of the cleft and noncleft nostrils was drawn. All vertical measurements (NH, ¼ med. part, nasal sill height) were measured perpendicularly, and all horizontal measurements (NW) were measured parallel to this reference line. The above-mentioned dimensions were used to derive ratios (cleft side divided by noncleft side in UCLP, and left side divided by right in BCLP), allowing for a comparison of nostril symmetry at each time point (Fig. 2).
Fig. 2.
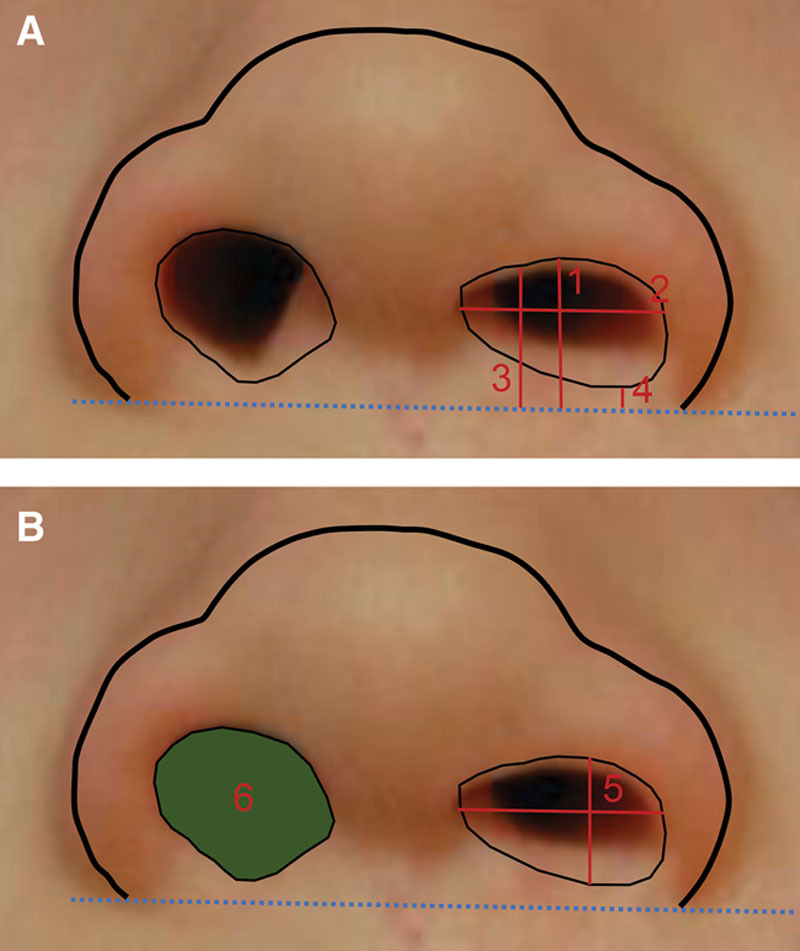
The structured photographic analysis included nostril height (NH), nostril width (NW), one-fourth medial part of nostril height (¼ med. part), nostril area, inner nostril height-to-width ratio (H-t-W), and columella angle (ColAng) as described by Chang et al.21
Blinded Rating of Therapy- and Appearance-matched Cases
Thirty specialists in cranio-maxillofacial (CMF) surgery who were blinded to treatment history rated the treatment course and aesthetical results. All enrolled cases were matched in juxtaposed pairs according to the therapy and severity in appearance (moderate or severe) in a questionnaire. In this questionnaire, only the first and second photographs of each juxtaposed, matched case were shown. The raters had to decide which of the juxtaposed cases (non-NAM versus NAM) performed better or worse aesthetically according to nasal form, nasal symmetry, and cupid’s bow. The counts were collected and summarized for all raters for each match.
Statistical Analyses
Statistical analysis was carried out by using the statistical software “Standard Package for the Social Science” (SPSS for Mac, release 22.0.0, 2013; SPSS Inc., Chicago, Ill). The intraclass correlation (ICC) coefficient was calculated to determine the intra- and interrater reliability and consistency of measurements performed by the two blinded raters (LMR and FDG) applying a 2-way mixed model. Differences between non-NAM and NAM results within the cleft-type and severity-matched groups were analyzed using the Mann–Whitney U test. A P value of <0.05 was considered statistically significant.
RESULTS
Study Population and ICC Coefficients
Descriptive results of the 36 patients are presented in Table 1. The distribution of non-NAM and NAM-treated patients was equal for both cleft entities, UCLP (each n = 8) and BCLP (each n = 10).
Table 1.
Descriptive Results and Distribution of Enrolled and Analyzed Patients with Unilateral or Bilateral Cleft Lip and Palate
| Unilateral Cleft Lip and Palate (n = 16) | Bilateral Cleft Lip and Palate (n = 20) | |||
|---|---|---|---|---|
| Non-NAM (n = 8) | NAM (n = 8) | Non-NAM (n = 10) | NAM (n = 10) | |
| Age at first photograph, d | 63 (19–98) | 21 (2–86) | 76 (14–100) | 12 (4–66) |
| Age at second photograph, d | 1121 (190–2093) | 701 (171–1967) | 665 (293–1503) | 491 (295–1692) |
| Gender, f/m | 4/4 | 0/8 | 3/7 | 5/5 |
| Appearance, m/s | 3/3 | 5/5 | 6/4 | 6/4 |
Values are given as median (range).
f/m, female/male; m/s, moderate/severe.
The ICC coefficients for the intrarater reliability of all measurements revealed very good to excellent overall results (>0.90) for the included parameters, except for nasal sill height (Table 2). Nasal sill height was associated with the lowest ICC coefficient for the intrarater reliability in the second photograph [0.84, 95% confidence interval (CI), 0.68–0.92, rater 2].
Table 2.
ICC Coefficient to Analyze the Intrarater Reliability of Measurements Performed by the 2 Blinded Raters (LMR and FDG) Applying a 2-Way Mixed Model
| Parameter | Rater 1 | Rater 2 | ||
|---|---|---|---|---|
| First Photograph, ICC (95% CI) | Second Photograph, ICC (95% CI) | First Photograph, ICC (95% CI) | Second Photograph, ICC (95% CI) | |
| NH, nc/r | 0.99 (0.98–0.99) | 0.99 (0.994–0.998) | 0.99 (0.98–0.99) | 0.98 (0.96–0.99) |
| NW, nc/r | 0.95 (0.9–0.98) | 0.98 (0.95–0.99) | 0.95 (0.90–0.98) | 0.93 (0.85–0.96) |
| ¼ med. Part, nc/r | 0.99 (0.98–0.99) | 0.99 (0.989–0.997) | 0.98 (0.95–0.99) | 0.96 (0.91–0.98) |
| Nasal sill height, nc/r | 0.91 (0.73–0.97) | 0.92 (0.84–0.96) | 0.88 (0.67–0.96) | 0.84 (0.68–0.92) |
| Nostril area, nc/r | 0.98 (0.96–0.99) | 0.97 (0.95–0.99) | 0.86 (0.71–0.93) | 0.97 (0.93–0.99) |
| Nostril H-t-W ratio, nc/r | 0.93 (0.86–0.97) | 0.97 (0.95–0.99) | 0.96 (0.92–0.98) | 0.94 (0.88–0.97) |
| Columella angle | 0.94 (0.87–0.97) | 0.92 (0.85–0.96) | 0.96 (0.92–0.98) | 0.93 (0.86–0.96) |
| NH, c/l | 0.99 (0.995–0.999) | 0.995 (0.99–0.997) | 0.97 (0.95–0.99) | 0.995 (0.99–0.998) |
| NW, c/l | 0.99 (0.98–0.995) | 0.98 (0.95–0.99) | 0.97 (0.93–0.98) | 0.977 (0.955–0.988) |
| ¼ med. Part, c/l | 0.99 (0.99–0.998) | 0.995 (0.99–0.997) | 0.98 (0.97–0.99) | 0.99 (0.978–0.99) |
| Nasal sill height, c/l | — | 0.85 (0.54–0.94) | — | 0.77 (0.54–0.88) |
| Nostril area, c/l | 0.99 (0.98–0.99) | 0.99 (0.98–0.995) | 0.97 (0.94–0.98) | 0.96 (0.92–0.98) |
| Nostril H-t-W ratio, c/l | 0.99 (0.98–0.99) | 0.99 (0.98–0.99) | 0.9 (0.80–0.95) | 0.98 (0.97–0.99) |
nc/r, noncleft or right side; c/l, cleft or left side.
The ICC coefficients for the interrater reliability of all measurements revealed overall good results for the first photograph (>0.85) (Table 3). Nasal sill height was also associated with the lowest ICC coefficient for the interrater reliability in the second photograph (0.80; 95% CI, −0.12 to 0.94).
Table 3.
ICC Coefficient to Analyze the Interrater Reliability of Measurements Performed by the 2 Blinded Raters (LMR and FDG) Applying a 2-Way Mixed Model
| Parameter | First Photograph, ICC (95% CI) | Second Photograph, ICC (95% CI) |
|---|---|---|
| NH, nc/r | 0.99 (0.96–0.99) | 0.99 (0.96–0.99) |
| NW, nc/r | 0.94 (0.89–0.97) | 0.93 (0.86–0.96) |
| ¼ med. part, nc/r | 0.97 (0.93–0.99) | 0.98 (0.97–0.99) |
| Nasal sill height, nc/r | 0.98 (0.93–0.99) | 0.80 (−0.12 to 0.94) |
| Nostril area, nc/r | 0.90 (0.78–0.95) | 0.88 (0.19–0.96) |
| Nostril H-t-W ratio, nc/r | 0.87 (0.73–0.93) | 0.97 (0.94–0.99) |
| Columella angle | 0.85 (0.60–0.93) | 0.87 (0.74–0.93) |
| NH, c/l | 0.996 (0.992–0.998) | 0.996 (.992–0.998) |
| NW, c/l | 0.96 (0.92–0.98) | 0.93 (0.85–0.97) |
| ¼ med. part, c/l | 0.995 (0.99–0.997) | 0.99 (0.98–0.996) |
| Nasal sill height, c/l | — | 0.85 (0.4–0.94) |
| Nostril area, c/l | 0.92 (0.36–0.98) | 0.96 (0.54–0.99) |
| Nostril H-t-W ratio, c/l | 0.95 (0.90–0.98) | 0.98 (0.96–0.99) |
nc/r, noncleft or right side; c/l, cleft or left side.
Descriptive Results of Analyzed Parameters According to Chang et al21
The calculated ratios (c/nc = cleft/no cleft in UCLP and l/r = left/right) of all analyzed parameters—nostril height, nostril width, one-fourth medial part of nostril height, nostril area, inner nostril H-t-W, and columella angle—before and after treatment (surgery and non-NAM or NAM therapy) are shown in Tables 4 and 5 for the first and second photograph, respectively. Before treatment, the cases showed a common and known distribution of enlarged cleft to no-cleft side ratios of NW and nostril area, and reduced NH, ¼ med. part, H-t-W, and columella angle.
Table 4.
Results [Median (Range)] of First Photograph, including Both Measurement Rounds of Both Blinded Raters According to the Analysis Reported by Chang et al21
| Ratio, c/nc or l/r | Unilateral Cleft Lip and Palate | Bilateral Cleft Lip and Palate | ||||||
|---|---|---|---|---|---|---|---|---|
| Non-NAM | NAM | Non-NAM | NAM | |||||
| Moderate | Severe | Moderate | Severe | Moderate | Severe | Moderate | Severe | |
| NH | 0.7 (0.5–0.7) | 0.5 (0.3–0.6) | 0.6 (0.5–0.8) | 0.5 (0.2–0.7) | 0.9 (0.6–2.3) | 0.5 (0.0–1.1) | 0.7 (0.4–1.7) | 0.8 (0.3–1.4) |
| NW | 2.2 (1.4–3.1) | 3.2 (2.3–3.6) | 1.6 (1.5–2.2) | 3.9 (1.7–6.2) | 1.4 (0.5–1.8) | 1.4 (0.0–3.4) | 1.6 (0.6–2.7) | 1.4 (0.8–4.8) |
| ¼ med. part | 0.6 (0.5–0.7) | 0.5 (0.2–0.6) | 0.6 (0.5–0.8) | 0.4 (0.1–0.7) | 0.9 (0.5–2.4) | 0.5 (0.0–1.0) | 0.8 (0.2–1.8) | 0.9 (0.1–1.4) |
| Nasal sill height | — | — | — | — | — | — | — | — |
| Nostril area | 1.9 (0.9–2.3) | 2.2 (1.1–3.1) | 1.2 (0.8–1.4) | 2.5 (0.4–7.6) | 1.2 (0.8–2.4) | 0.9 (0.0–3.1) | 1.2 (0.6–2.0) | 0.9 (0.6–2.9) |
| H-t-W | 0.3 (0.2–1.1) | 0.2 (0.1–0.3) | 0.4 (0.2–0.5) | 0.1 (0.1–0.2) | 0.7 (0.4–4.0) | 0.3 (0.0–0.4) | 0.5 (0.2–2.9) | 0.4 (0.2–0.9) |
| ColAng, degree | 70.6 (50.9–119.1) | 51.1 (36.3–93.1) | 86.4 (60.2–115.7) | 51.0 (31.0–79.3) | 86.9 (66.5–116.8) | 72.4 (0.0–83.7) | 78.9 (39.5–116.1) | 74.1 (0.0–91.0) |
Nasal sill height was not calculated because of missing lip and nose competence before treatment (surgery and non-NAM or NAM Therapy).
Table 5.
Results [Median (Range)] of Second Photograph, including Both Measurement Rounds of Both Blinded Raters According to the Analysis Reported by Chang et al21
| Ratio, c/nc or l/r | Unilateral Cleft Lip and Palate | Bilateral Cleft Lip and Palate | ||||||
|---|---|---|---|---|---|---|---|---|
| Non-NAM | NAM | Non-NAM | NAM | |||||
| Moderate | Severe | Moderate | Severe | Moderate | Severe | Moderate | Severe | |
| NH | 0.8 (0.6–0.9) | 0.9 (0.5–1.0) | 0.8 (0.6–0.8) | 0.7 (0.6–0.9) | 1.0 (0.8–1.1) | 0.8 (0.6–1.0) | 0.9 (0.6–1.3) | 0.9 (0.7–1.5) |
| NW | 1.1 (0.9–1.2) | 1.5 (1.1–3.2) | 1.2 (1.0–1.7) | 1.9 (1.3–3.6) | 1.0 (0.7–1.5) | 1.2 (0.9–1.4) | 1.2 (0.9–2.2) | 1.2 (0.9–1.7) |
| ¼ med. part | 0.7 (0.5–1.0) | 0.6 (0.4–1.0) | 0.8 (0.4–0.9) | 0.8 (0.5–1.0) | 1.0 (0.5–1.6) | 0.9 (0.4–1.0) | 0.9 (0.2–1.7) | 0.9 (0.6–1.9) |
| Nasal sill height | 1.0 (0.6–1.8) | 0.6 (0.3–0.9) | 0.9 (0.5–1.6) | 0.6 (0.3–1.1) | 1.0 (0.5–2.5) | 0.8 (0.4–1.3) | 0.9 (0.3–2.5) | 0.9 (0.4–1.2) |
| Nostril area | 0.8 (0.5–1.0) | 1.4 (0.6–4.3) | 0.9 (0.8–1.3) | 1.7 (0.7–2.8) | 1.1 (0.8–1.6) | 0.9 (0.4–1.2) | 1.2 (0.8–1.9) | 1.1 (0.9–1.8) |
| H-t-W | 0.8 (0.3–1.0) | 0.5 (0.2–1.0) | 0.7 (0.4–0.8) | 0.4 (0.2–0.5) | 0.9 (0.7–1.4) | 0.7 (0.4–1.2) | 0.9 (0.3–1.4) | 0.7 (0.5–1.7) |
| ColAng, degree | 87.1 (84.6–93.0) | 85.0 (74.8–94.9) | 87.0 (57.7–100.6) | 83.6 (80.9–97.1) | 88.6 (83.9–94.7) | 88.3 (72.5–91.0) | 88.9 (70.5–92.5) | 89.0 (81.0–92.2) |
After treatment, an approximation of the severe UCLP and BCLP cases to the moderate cases was registered in almost all parameters, except for nostril area and nostril width in patients with UCLP. Nostril area remained absolutely greater in all second photographs, although a negative difference was detected, irrespective of cleft type and applied treatment (Table 6). Greater nostril width ratios might have contributed to this result. The differences of the analyzed ratios between first and second photograph are illustrated in Table 6, Figure 3, and Supplemental Digital Content 1. (See figure, Supplemental Digital Content 1, which displays the boxplot diagrams representing the differences of analyzed ratios of the first and second photograph applying NAM or non-NAM therapy. The upper row displays the moderate (a) and severe (b) cases with unilateral cleft lip and palate. The lower row displays the moderate (c) and severe (d) cases with bilateral cleft lip and palate, http://links.lww.com/PRSGO/B460.) The greatest differences were registered for the NW in severe cases with UCLP in both treatment groups, non-NAM [−1.2 (−2.4 – (−0.1))] and NAM [−1.4 (−3.4 – (−0.4))]. Nostril height was associated with a low to moderate increase in all groups. The greatest increase for the ¼ med. part was observed in severe cases of UCLP NAM therapy group [0.4 (0.0–0.9)].
Table 6.
Median (Range) Differences between First and Second Photograph, including Both Measurement Rounds of Both Blinded Raters According to the Analysis Reported by Chang et al21
| Ratio, c/nc or l/r | Unilateral Cleft Lip and Palate | Bilateral Cleft Lip and Palate | ||||||
|---|---|---|---|---|---|---|---|---|
| Non-NAM | NAM | Non-NAM | NAM | |||||
| Moderate | Severe | Moderate | Severe | Moderate | Severe | Moderate | Severe | |
| NH | 0.2 (0.0–0.3) | 0.4 (0.0–0.8) | 0.1 (−0.1 to 0.3) | 0.3 (−0.1 to 0.5) | 0.1 (−1.3 to 0.3) | 0.2 (−0.2 to 0.9) | 0.2 (−0.7 to 0.5) | 0.1 (−0.2 to 0.5) |
| NW | −1.0 (−2.0 to −0.2) | −1.2 (−2.4 to −0.1) | −0.5 (−1.0 to 0.4) | −1.4 (−3.4 to 0.4) | −0.2 (−1.0 to 0.5) | 0.9 (−2.5 to 1.4) | 0.0 (−1.6 to 0.4) | −0.3 (−3.7 to 0.4) |
| ¼ med. part | 0.1 (−0.1 to 0.4) | 0.2 (−0.1 to 0.8) | 0.0 (-0.1–0.3) | 0.4 (0.0–0.9) | 0.1 (−1.5 to 0.5) | 0.2 (0.0–1.0) | 0.1 (−0.8 to 0.5) | 0.1 (−0.3 to 0.8) |
| Nasal sill height | — | — | — | — | — | — | — | — |
| Nostril area | −1.2 (−2.1 to 0.1) | −0.4 (−2.1 to 2.7) | 0.0 (−0.6 to 0.5) | −0.1 (−4.8 to 1.2) | −0.1 (−1.3 to 0.7) | 0.1 (−2.2 to 1.2) | −0.1 (−1.1 to 0.8) | 0.3 (−1.9 to 1.5) |
| H-t-W | 0.5 (−0.4 to 0.6) | 0.4 (0.0–0.9) | 0.3 (0.0–0.4) | 0.3 (0.0–0.4) | 0.2 (−3.1 to 0.8) | 0.7 (0.0–0.9) | 0.1 (−1.9 to 0.7) | 0.3 (−0.2 to 1.1) |
| ColAng, degree | 18.3 (−26.1 to 33.7) | 29.6 (−6.2 to 55.7) | 5.9 (−23.4 to 20.0) | 31.3 (2.3–77.8) | 3.0 (−26.9 to 20.4) | 6.2 (1.0–16.6) | 8.1 (−24.9 to 44.2) | 12.3 (−10.0 to 43.3) |
Fig. 3.

Treatment course. Images showing examples of clinical result applying non-NAM (A and B) and NAM (C and D) therapy according to our described treatment plan on the basis of Grayson’s technique.
Statistical Analysis
Comparison between appearance-matched non-NAM and NAM groups using the 7 analyzed parameters after treatment (second photograph) revealed significant differences of the absolute values for NH (P = 0.026), NW (P = 0.009), nostril area (P = 0.003), and H-t-W (P = 0.042) in moderate cases with UCLP (Table 7). The absolute value of the H-t-W ratio (P = 0.012) was significantly different in the comparison of non-NAM and NAM-treated severe cases with UCLP. NW (P = 0.01) was significantly different in the comparison between non-NAM and NAM-treated moderate cases with BCLP, whereas nostril area (P < 0.001) was significantly different in severe cases with BCLP.
Table 7.
Comparison of Difference between First and Second Photograph and the Absolute Value after Treatment of Appearance-matched Non-NAM and NAM Groups Using the 7 Analyzed Parameters According to Chang et al21
| Ratio, c/nc or l/r | Unilateral Cleft Lip and Palate | Bilateral Cleft Lip and Palate | ||||||
|---|---|---|---|---|---|---|---|---|
| Non-NAM vs. NAM | Non-NAM vs. NAM | |||||||
| Moderate (P) | Severe (P) | Moderate (P) | Severe (P) | |||||
| Absolute | Difference | Absolute | Difference | Absolute | Difference | Absolute | Difference | |
| NH | 0.026* | 0.371 | 0.221 | 0.424 | 0.567 | 0.079 | 0.125 | 0.316 |
| NW | 0.009* | 0.019* | 0.058 | 0.542 | 0.01* | 0.277 | 0.606 | 0.218 |
| ¼ med. part | 0.635 | 0.428 | 0.094 | 0.149 | 0.095 | 0.95 | 0.228 | 0.105 |
| Nasal sill height | 0.382 | — | 0.211 | — | 0.179 | — | 0.834 | — |
| Nostril area | 0.003* | 0.002* | 0.074 | 0.776 | 0.252 | 0.38 | <0.001* | 0.769 |
| H-t-W | 0.042* | 0.019* | 0.012* | 0.094 | 0.193 | 0.64 | 0.274 | 0.176 |
| ColAng | 0.507 | 0.053 | 0.715 | 0.818 | 0.283 | 0.071 | 0.242 | 0.869 |
Mann–Whitney U test.
P value <0.05 was considered statistically significant.
Blinded Rating of Therapy- and Appearance-matched Cases
The 30 raters, who were blinded to therapy, rated the moderate, non–NAM treated cases with UCLP better than NAM-treated cases (Table 8). Severe, NAM-treated cases with UCLP performed better in appearance than non–NAM treated cases according to the rating.
Table 8.
Results of Blinded Rating of First and Second Photograph of the 18 Therapy- and Appearance-matched Cases by 30 Specialists in Cranio-Maxillofacial Surgery
| Matched Pairs | Non-NAM | NAM | Equal | Total Count | |
|---|---|---|---|---|---|
| Moderate unilateral CLP | 3 | 64 | 9 | 17 | 90 |
| Severe unilateral CLP | 5 | 37 | 87 | 26 | 150 |
| Moderate bilateral CLP | 6 | 101 | 59 | 20 | 180 |
| Severe bilateral CLP | 4 | 49 | 54 | 17 | 120 |
| Total | 18 | 251 | 209 | 80 | 540 |
Moderate, non–NAM treated cases with BCLP were rated better than matched NAM-treated cases. Matched severe NAM-treated cases with BCLP achieved in total better results than matched non–NAM treated cases.
DISCUSSION
The presented study displays our clinical results of patients with UCLP and BCLP that have been treated according to a standardized protocol applying non-NAM or NAM therapy using Grayson’s technique in the presurgical setting as described earlier and elsewhere.4,14
Our results are based on 2 data sources, conventional photographs and a rating by 30 specialists in CMF surgery, who were blinded to treatment history. No 3-dimensional (3D) photography was used, because in many cases the first photograph was taken as a conventional 2D photograph at our department before 3D photography was available and quickly usable for our very young patients. According to the retrospective nature of this study, we avoided mixing up two different techniques of image capturing. Moreover, scoring on 2D photographs is described to be easier to perform and more applicable and intuitive in daily practice since all cleft patients are photographed throughout the course of their treatment. Additionally, conventional photography is reliably used to assess the phenotypic severity of facial anomalies and appearance and as described by others, therefore, remains the gold standard.25,26
The calculated ICC coefficients for intra- and interrater reliability were overall good to excellent. This shows a high standard and consistency of analysis for both raters. Nasal sill height was, however, the most difficult to analyze.
The rating of the 30 CMF specialists was a subjective assessment of which of the therapy- and appearance-matched pairs were aesthetically better or worse at the different stages of ongoing treatment. The quantification of any ratios, distances, or angles mentioned above or in the literature was not desired with this form of analysis. We instead wanted to achieve a feeling of unexpected and unprejudiced rating, as might occur on the street in normal social interaction. In their assessment, the raters evaluated the moderate, non–NAM treated cases with UCLP and BCLP better than matched NAM-treated cases. Severe, NAM-treated cases with UCLP performed better in the rating than non–NAM treated cases (Table 8) despite the better-measured results of, for example, the columella angle (Table 4).
According to our results clinical experience, the indication for NAM depends on the type and severity of the cleft. In our study, NAM therapy was beneficial in severe cases with UCLP. The ¼ med. part parameter was increased absolutely in comparison to the non-NAM group of severe cases with UCLP (P = 0.094). This parameter reflects, indirectly, the nasal height and H-t-W ratio and contributes to the desired long-oval nostril shape, which is often disturbed in cases of UCLP. This positive trend is advantageous for a better nose symmetry. Columella angle experienced the greatest changes in NAM-treated cases with moderate [29.6-degree angle (−6.2 to 55.7)] and severe [31.3-degree angle (2.3–77.8), Table 6] UCLP. No significant difference was registered to the matched non-NAM group, but, in this case, one must keep in mind that the severity of cleft-associated columella angle deviation was initially greater in the NAM group (first photograph, Table 4). Our results were constant for a median of at least 701 days (171–1967). This observational time interval is not a long-term result, but overall we and others achieved good short-term results.15 Mancini et al. reported improved nasal projection, nasal width and nasal symmetry, and columella length in a 3D analysis of 20 consecutively treated cases with UCLP. Barillas et al. reported that the good results were maintained at least until the age of 9 years.7 This contradicts other studies that critically question the effectiveness of NAM altogether. AlHayyan et al. described no significant impact on long-term midface symmetry of presurgical NAM in children with UCLP when compared with children treated without any form of presurgical infant orthopedics.17 Furthermore, some studies describe a relapse of initially good results. We are not able to prove or disprove these observations with our presented study but clinically agree that in some cases a relapse might be observed. Within the limitations of this study, we are not able to describe possible confounding factors that might contribute to this clinical finding. Based on our experience with NAM therapy, it will be a mixture of timing/treatment start, indication (moderate cases), compliance (neonate and parents), growth, and still unknown factors.
In addition, the indication for NAM therapy in cases of BCLP is mainly driven by the severity of appearance as well as by the consecutively shortened columella length. The latter parameter is a well-known, susceptible variable for NAM therapy in cases of BCLP.14,27,28 Garfinkle et al11 reported a long-term stability of their good results through to the age of 12 years. We did not include the columella length in this analysis. This parameter is nevertheless known to be positively influenced by NAM treatment, especially in cases of BCLP.11,27 Suri et al29 reported that infants who received NAM therapy had longer columella and better-aligned alveolar segments than those who received only feeding plate therapy. In their study, other nostril dimensions were not significantly different, comparable to our results. Finally, in cases that benefit from NAM therapy, easier primary surgery and fewer secondary corrections can be expected. Secondary columella lengthening, especially in patients with BCLP, could be reduced with a near-normal nasolabial appearance.18
On the basis of this study, as well as on our experience with this technique, we started to indicate NAM therapy more critically in our young patients presenting with an UCLP. We see more beneficial effects in severe cases. As main indicators, we will apply the following parameters in the future, to facilitate our decision-making: ¼ med. part (<0.5), H-t-W ratio (<0.2), and columella angle (<55 degree). In cases of BCLP, we generally see a great opportunity to elongate the columella and relocate a mispositioned premaxilla, which might result in easier primary surgery and could reduce secondary procedures in the future, as described by others.28 Therefore, we will continue to offer NAM therapy for all parents presenting with a newborn with a BCLP, explaining the advantages and disadvantages of the therapy.
Limitations
Although the cohort was small, we tried to make, treatment- and appearance-wise, the most homogenous matches. According to the nature of a retrospective study, the follow-up times and, as a result, the time intervals between the first and second photograph varied between the groups. Interestingly, the photograph documentation was started earlier in the NAM-treated patients. At the age of 6 months, nasal morphology should be judged with care, and estimation of the clinical course regarding relapse or good aesthetical result is not safely possible yet. Nevertheless, in the opinion of the authors, an analysis at this age is important to gauge short-term results. Another limitation is the use of 2D photograph analyses, which did not allow further evaluation of other important parameters such as columella length and lateral profile. No functionally relevant analysis was performed. We did not evaluate the effect of treatment on the dentoalveolar ridge position. But regarding this not negligible aspect of treatment in young patients with CLP, we have already described our experiences previously with the time of analysis at the end of NAM therapy.14,27 Lastly, a potential treatment bias might be evident in the analyzed patients because of the parents’ decision-making, considering the financial implications of such treatment. In Germany, NAM therapy is not (fully) covered by the health insurance providers. For this reason, we must inform the parents about the treatment itself (informed decision-making) and potential financial contributions or deterrent fees that might occur due to NAM therapy. On the basis of this information, the parents decided whether they wanted NAM therapy to be performed or not.
CONCLUSIONS
Newborns presenting with severe UCLP or BCLP may benefit from NAM, as it may give a better rated early result. Moderate severities of UCLP and BCLP did not benefit from NAM in this early phase as much as severe cases did and were not rated better than matched non-NAM cases. According to this study, NAM does not seem to be beneficial in moderate cases of BCLP.
PATIENT CONSENT
Parents or guardians provided written consent for the use of the patients' image.
Supplementary Material
Footnotes
Published online 23 September 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Matsuo K, Hirose T, Tomono T, et al. Nonsurgical correction of congenital auricular deformities in the early neonate: a preliminary report. Plast Reconstr Surg. 1984;73:38. [DOI] [PubMed] [Google Scholar]
- 2.Ritschl LM, Heinrich V, Grill FD, et al. Stress distribution patterns within viscero- and neurocranium during nasoalveolar molding: a finite element analysis. Plast Reconstr Surg Glob Open. 2018;6:e1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grill FD, Ritschl LM, Dikel H, et al. Facilitating CAD/CAM nasoalveolar molding therapy with a novel click-in system for nasal stents ensuring a quick and user-friendly chairside nasal stent exchange. Sci Rep. 2018;8:12084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grayson BH, Santiago PE, Brecht LE, et al. Presurgical nasoalveolar molding in infants with cleft lip and palate. Cleft Palate Craniofac J. 1999;36:486–498. [DOI] [PubMed] [Google Scholar]
- 5.Liao YF, Hsieh YJ, Chen IJ, et al. Comparative outcomes of two nasoalveolar molding techniques for unilateral cleft nose deformity. Plast Reconstr Surg. 2012;130:1289–1295. [DOI] [PubMed] [Google Scholar]
- 6.Yu Q, Gong X, Shen G.CAD presurgical nasoalveolar molding effects on the maxillary morphology in infants with UCLP. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:418–426. [DOI] [PubMed] [Google Scholar]
- 7.Barillas I, Dec W, Warren SM, et al. Nasoalveolar molding improves long-term nasal symmetry in complete unilateral cleft lip-cleft palate patients. Plast Reconstr Surg. 2009;123:1002–1006. [DOI] [PubMed] [Google Scholar]
- 8.van der Heijden P, Dijkstra PU, Stellingsma C, et al. Limited evidence for the effect of presurgical nasoalveolar molding in unilateral cleft on nasal symmetry: a call for unified research. Plast Reconstr Surg. 2013;131:62e–71e. [DOI] [PubMed] [Google Scholar]
- 9.Berkowitz S.Why hasn’t cutting and grayson done a longitudinal study to show why nasoalveolar molding should not be used? Cleft Palate Craniofac J. 2019;56:141. [DOI] [PubMed] [Google Scholar]
- 10.Abbott MM, Meara JG.Nasoalveolar molding in cleft care: is it efficacious? Plast Reconstr Surg. 2012;130:659–666. [DOI] [PubMed] [Google Scholar]
- 11.Garfinkle JS, King TW, Grayson BH, et al. A 12-year anthropometric evaluation of the nose in bilateral cleft lip-cleft palate patients following nasoalveolar molding and cutting bilateral cleft lip and nose reconstruction. Plast Reconstr Surg. 2011;127:1659–1667. [DOI] [PubMed] [Google Scholar]
- 12.Sischo L, Chan JW, Stein M, et al. Nasoalveolar molding: prevalence of cleft centers offering NAM and who seeks it. Cleft Palate Craniofac J. 2012;49:270–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dean RA, Wainwright DJ, Doringo IL, et al. Assessing burden of care in the patient with cleft lip and palate: factors influencing completion and noncompletion of nasoalveolar molding. Cleft Palate Craniofac J. 2019;56:759–765. [DOI] [PubMed] [Google Scholar]
- 14.Rau A, Ritschl LM, Mücke T, et al. Nasoalveolar molding in cleft care–experience in 40 patients from a single centre in Germany. PLoS One. 2015;10:e0118103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mancini L, Gibson TL, Grayson BH, et al. Three-dimensional soft tissue nasal changes after nasoalveolar molding and primary cheilorhinoplasty in infants with unilateral cleft lip and palate. Cleft Palate Craniofac J. 2019;56:31–38. [DOI] [PubMed] [Google Scholar]
- 16.Ahmed MK, Bui AH, Barnett R, et al. Quantitative evaluation of nasolabial alterations following nasoalveolar molding (NAM) therapy in patients with unilateral cleft lip. Facial Plast Surg. 2019;35:73–77. [DOI] [PubMed] [Google Scholar]
- 17.AlHayyan WA, Pani SC, AlJohar AJ, et al. The effects of presurgical nasoalveolar molding on the midface symmetry of children with unilateral cleft lip and palate: a long-term follow-up study. Plast Reconstr Surg Glob Open. 2018;6:e1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meazzini MC, Chiavenna C, Autelitano L, et al. Photometric evaluation in adolescence of patients with bilateral cleft lip and palate treated with nasoalveolar molding and primary columella lengthening. Cleft Palate Craniofac J. 2018;55:568–573. [DOI] [PubMed] [Google Scholar]
- 19.Russell JH, Kiddy HC, Mercer NS.The use of SymNose for quantitative assessment of lip symmetry following repair of complete bilateral cleft lip and palate. J Craniomaxillofac Surg. 2014;42:454–459. [DOI] [PubMed] [Google Scholar]
- 20.Pigott RW, Pigott BB.Quantitative measurement of symmetry from photographs following surgery for unilateral cleft lip and palate. Cleft Palate Craniofac J. 2010;47:363–367. [DOI] [PubMed] [Google Scholar]
- 21.Chang CS, Por YC, Liou EJ, et al. Long-term comparison of four techniques for obtaining nasal symmetry in unilateral complete cleft lip patients: a single surgeon’s experience. Plast Reconstr Surg. 2010;126:1276–1284. [DOI] [PubMed] [Google Scholar]
- 22.Grayson BH, Cutting C, Wood R.Preoperative columella lengthening in bilateral cleft lip and palate. Plast Reconstr Surg. 1993;92:1422–1423. [PubMed] [Google Scholar]
- 23.Kook MS, Jung S, Park HJ, et al. A comparison study of different facial soft tissue analysis methods. J Craniomaxillofac Surg. 2014;42:648–656. [DOI] [PubMed] [Google Scholar]
- 24.Schindelin J, Rueden CT, Hiner MC, et al. The ImageJ ecosystem: an open platform for biomedical image analysis. Mol Reprod Dev. 2015;82:518–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spolyar JL, Roldán JC.Changes in nose symmetry in unilateral cleft lip and palate treated by differing pre-surgical assistance: an objective assessment of primary repair. J Craniomaxillofac Surg. 2015;43:779–789. [DOI] [PubMed] [Google Scholar]
- 26.Asher-McDade C, Roberts C, Shaw WC, et al. Development of a method for rating nasolabial appearance in patients with clefts of the lip and palate. Cleft Palate Craniofac J. 1991;28:385–390; discussion 390. [DOI] [PubMed] [Google Scholar]
- 27.Grill FD, Wasmaier M, Mücke T, et al. Identifying perioperative volume-related risk factors in head and neck surgeries with free flap reconstructions—an investigation with focus on the influence of red blood cell concentrates and noradrenaline use. J Craniomaxillofac Surg. 2020;48:67–74. [DOI] [PubMed] [Google Scholar]
- 28.Lee CT, Garfinkle JS, Warren SM, et al. Nasoalveolar molding improves appearance of children with bilateral cleft lip-cleft palate. Plast Reconstr Surg. 2008;122:1131–1137. [DOI] [PubMed] [Google Scholar]
- 29.Suri S, Disthaporn S, Atenafu EG, et al. Presurgical presentation of columellar features, nostril anatomy, and alveolar alignment in bilateral cleft lip and palate after infant orthopedics with and without nasoalveolar molding. Cleft Palate Craniofac J. 2012;49:314–324. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


