Abstract
Background:
Choosing the optimal mastectomy incision must account for oncologic, reconstructive, and aesthetic considerations, including nipple preservation, mastectomy skin margins and potential for skin involvement, mastectomy skin perfusion and viability, mastectomy skin excess, previous breast scars, the reconstructive plan, and inconspicuous new scar placement. In the present study, we aimed to assess breast reconstruction aesthetics, as they are influenced by mastectomy incision design.
Methods:
Nine commonly utilized mastectomy incision patterns were grouped into 3 categories: hidden scar, vertical scar, and transverse scar. Twenty plastic surgeons were asked to blindly grade before and after photographs of reconstructed breasts with regard to scar visibility and position and according to their influence on breast aesthetics.
Results:
Statistically significant differences were observed between the study groups. Mastectomies and reconstructions performed through hidden incisions yield the most aesthetic results. Vertical scars are favorable to transverse scars. In the case of bilateral reconstructions, symmetric scar placement is paramount to optimizing aesthetic outcomes.
Conclusions:
The mastectomy incision pattern significantly affects the aesthetic outcomes in breast reconstruction. Patterns borrowed from cosmetic breast surgery consistently yield highly aesthetic outcomes. Surgeons must consider oncologic factors and patient characteristics in choosing an ideal incision for each patient.
INTRODUCTION
Achieving optimal aesthetic outcomes in breast reconstruction starts with preoperative planning. Choosing a mastectomy incision is a critical decision point in this process and has a profound influence on the final appearance of the reconstructed breast. A collaborative relationship between the breast surgeon and plastic surgeons is imperative to achieving optimal results. The surgical plan must account for both the oncologic surgeon’s and reconstructive surgeon’s goals as well as their limitations. Considerations of previous breast scars, nipple preservation, oncologic margins and mastectomy skin involvement, tissue perfusion and viability, mastectomy skin excess and breast ptosis, new breast scars, and potential for adjuvant radiation therapy must be taken into account.1,2
In this study, we aimed to assess the influence of mastectomy scars on breast reconstruction aesthetics and provide a treatment algorithm for mastectomy incision selection. Nine commonly used mastectomy incision patterns were identified, which can be grouped into 3 categories (Fig. 1).
Fig. 1.
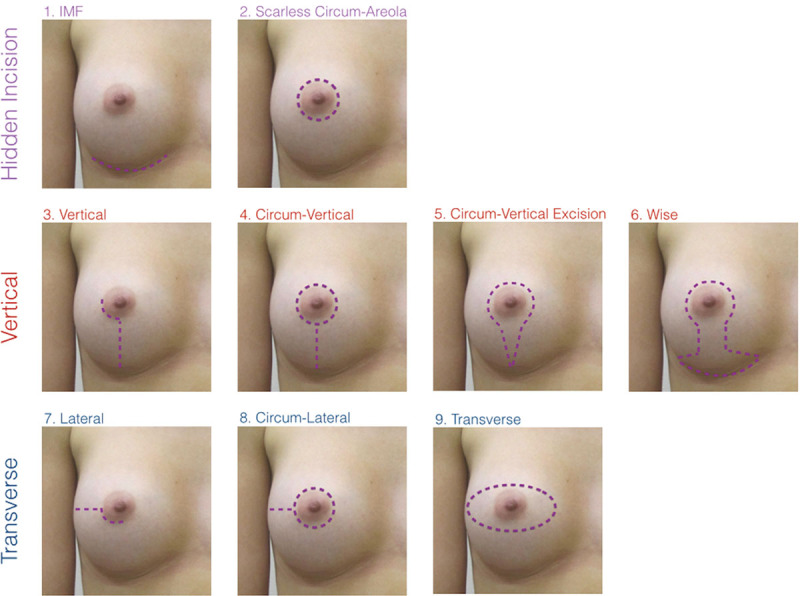
Nine commonly utilized mastectomy patterns have been identified. The patterns can be grouped into three categories: hidden scar, vertical scar, and transverse scar.
These include:
-
I. Hidden incision category:
-
II. Vertical incision category:
Of note, the Wise pattern can be applied as a first-stage breast reduction or mastopexy in preparation for second-stage nipple-sparing mastectomy in patients who are undergoing prophylactic treatment or have low-risk lesions.8,9 Alternatively, in patients who are not candidates for nipple preservation, the Wise pattern can be applied at the time of mastectomy.10
-
III. Transverse incision category:
7. Lateral incision
8. Circum-Lateral incision
9. Transverse incision
All mastectomy incision patterns can be reconstructed using implant or autologous techniques. In cases where the nipple and areola are removed, an autologous technique may be advantageous, as it can replace the missing breast surface area to avoid breast distortions.
PATIENTS AND METHODS
Study Design
This is a prospective observational study comparing the aesthetic outcomes of breast reconstructions performed with the 9 most commonly used mastectomy incisions patterns. All reconstructions were performed by a single plastic surgeon (W.D.). Twenty practicing plastic surgeons were asked to grade before and after reconstruction photographs of breasts, based on the influence of scar position on aesthetic outcome (see Fig. 2). Of note, 2 types of Wise pattern were reviewed: nipple sparing and non-nipple sparing. An absent breast and an aesthetic natural breast were used as negative and positive controls to contextualize survey participant ratings.
Fig. 2.
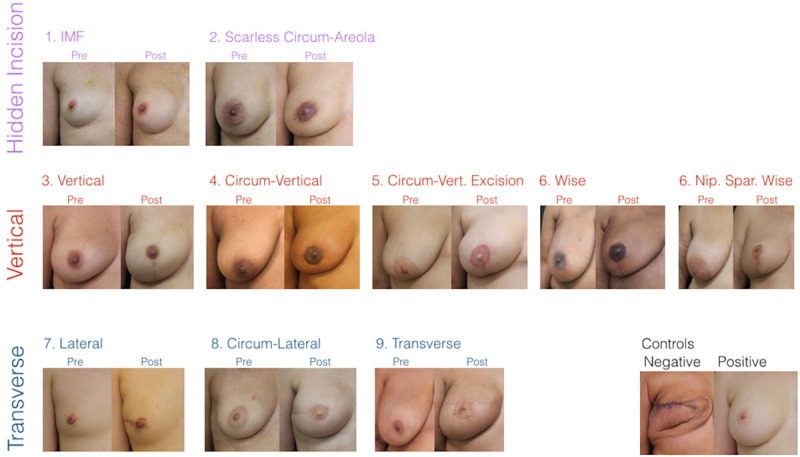
Pre- and postoperative photographs were presented in the survey, now arranged according to scar pattern as in Figure 1. Of note, two types of Wise pattern were reviewed: nipple sparing and non nipple sparing. An absent breast and an aesthetic natural breast were used as negative and positive controls to contextualize survey participant ratings.
Data were analyzed to draw conclusions and develop a treatment algorithm to guide mastectomy incision selection.
Assessments
Each participant recorded their assessment of preoperative and postoperative photographs based on the influence of scar position on aesthetic outcomes on a 5-point scale (1, Poor; 2, Fair; 3, Neutral; 4, Good; 5, Excellent). Only right breast images were used for uniformity. Preoperative and postoperative photographs were unpaired and presented in a random order.
Additionally, surgeons were asked to grade aesthetic outcomes based on scar patterns in 3 bilateral breast reconstructions using the same scale (Fig. 3). Bilateral mastectomy incisions were either symmetric (with vertical or transverse scar patterns on both breasts) or asymmetric (with a different pattern on each breast).
Fig. 3.
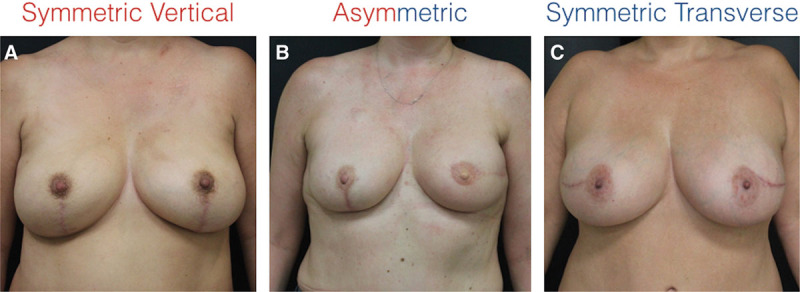
Full torso photographs of bilateral breast reconstructions presented in the survey. A, Both breasts reconstructed via vertical incisions. C, Both breasts reconstructed via transverse incisions. B, asymmetric scar pattern in the left and right breasts.
Statistical Analysis
All data were collected by a study coordinator. A 2-tailed student t test was used to compare ratings between groups. A value of P < 0.05 was used to determine statistical significance.
RESULTS
Mean aesthetic scores were calculated for each mastectomy incision pattern and then combined into 3 general groups (Fig. 4). The mean aesthetic score for hidden, vertical, and transverse incision groups were 4.48, 3.87, and 2.50, respectively. The hidden incision patterns were superior to all other incision patterns (P < 0.00001), and vertical incision patterns were superior to transverse patterns (P < 0.00001).
Fig. 4.
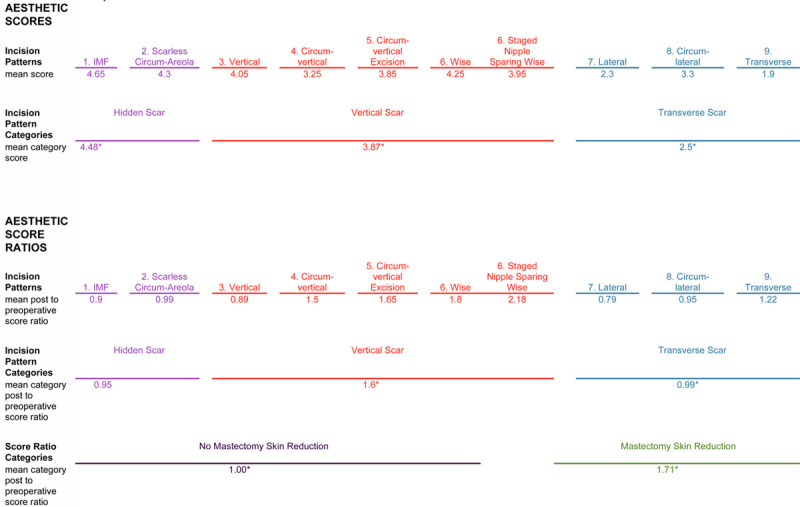
Mastectomy incision pattern scores.
The first row of numbers reports mean scores for individual mastectomy incision patterns.
The second row of numbers reports mean scores for incision pattern categories. Hidden scar incisions result in highest aesthetic ratings. Vertical incisions result in superior aesthetic ratings compared to transverse incisions. The differences between all three categories are statistically significant.
The third row of numbers reports mean post to preoperative score ratios for individual mastectomy patterns. Vertical scar patterns have significantly higher score ratios compared to transverse scar patterns.
The fourth row of numbers reports mean post to preoperative score ratios categorized based on removal of excess mastectomy skin to mitigate breast ptosis. Aesthetic improvement can be achieved in breast reconstruction patients when preoperative ptosis is corrected. The difference between the two categories is statistically significant.
*Statistically significant differences in data across a row.
When comparing scar patterns in bilateral breast reconstruction cases (symmetric vertical, symmetric transverse, and asymmetric), the mean aesthetic score for vertical, transverse, and asymmetric incisions were 4.3, 3.8, and 2.8, respectively. Symmetric breast scars (transverse or vertical) were associated with improved breast aesthetics compared with asymmetric scars (P < 0.001 and P < 0.00001). Vertical scars were associated with improved aesthetics compared with transverse scars (P < 0.03).
Postoperative to preoperative score ratios were calculated by dividing the postoperative score by the preoperative score for each breast to quantify the quality of the reconstruction vis-à-vis its starting point (Figure 4). These data demonstrated significant superiority of the vertical scar pattern over the transverse scar pattern (P < 0.00001). Data regarding score ratios for hidden scar patterns do not contribute to our conclusions because they are skewed by the high preoperative aesthetic ratings of these nonptotic patients. When the score ratios were grouped based on whether additional mastectomy skin was removed because of preoperative ptosis, patients who did not require additional skin removal had a mean score ratio of 1.0, and patients who required removal of additional skin had a mean score ratio of 1.7 (P < 0.00001).
DISCUSSION
Careful evaluation of breast reconstruction results has demonstrated that 6 mastectomy incision patterns consistently yield highly aesthetic results. These include inframammary fold incision, scarless periareoral incision,4 vertical incision, circum-vertical incision, circum-vertical excision, and Wise pattern. These patterns can be classified as being either hidden scar or vertical patterns and are modeled on tried and true incision patterns used in cosmetic surgeries. Conversely, transverse scar patterns, such as the lateral, circum-lateral, and transverse incision patterns, leave more prominent centrally located scars and limit options for second-stage revisions. Issues related to lateral nipple drift secondary to lateral scar contraction and recurrent ptosis are more difficult to correct when a transverse incision is present.
Based on these findings, we have described an algorithm for choosing mastectomy incision patterns according to patient characteristics (Fig. 5). The algorithm includes the authors’ preferred approach to 2 additional types of breast reconstruction that are not addressed by the data in this study. The first is reconstruction after additional mastectomy skin resection based on tumor skin involvement, referred to as a “geographic pattern.” This term is based on the haphazard flap skin paddle shapes that result from patching the resection defects. The second is delayed breast reconstruction, for which the algorithm has been described in a previous publication and is included in Figure 4 to present a more comprehensive algorithm.11
Fig. 5.
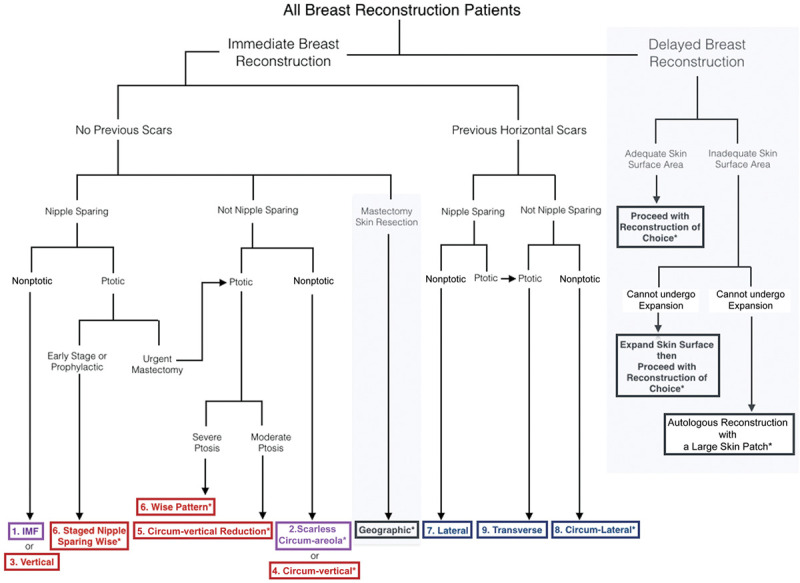
Algorithm for choosing mastectomy incision patterns based on patient characteristics and surgeon’s preference. Portions of the diagram in gray boxes (geographic scar pattern and delayed breast reconstruction) are outside the scope of this study, are based on previously published descriptions, and are included here for completeness. *Author’s preference for autologous reconstruction.
This study confirms that patients with nonptotic breasts who are likely to benefit from a nipple-sparing mastectomy are ideally treated with a hidden or vertical incision pattern such as an inframammary fold incision or vertical incision, depending on the breast surgeon’s preference. Both patterns are amenable to either implant or autologous reconstruction.
Patients who are nonptotic but are not candidates for nipple-sparing surgery are ideally treated with a scarless circum-areola approach or a circum-vertical approach. Both these reconstructions are ideally accomplished with autologous reconstruction.
Ptotic patients who are candidates for nipple-sparing mastectomy can be treated with a first-stage Wise pattern breast reduction or mastopexy, followed by second mastectomy and reconstruction. This approach is oncologically sound only in patients undergoing prophylactic mastectomy and those with small breast cancers that could have otherwise been treated with segmental resection. Although this pattern can theoretically be used both in implant and autologous reconstructions, the authors prefer to limit it to autologous reconstruction given the increased potential for partial nipple loss in these patients.
Finally, patients who are ptotic and not candidates for nipple preservation are best treated with a circum-vertical excision or Wise pattern incision depending on the degree of ptosis. This is best accomplished with autologous reconstruction to mitigate healing issues that may arise from more complex incision patterns.
All of the above-described incision patterns provide adequate access for implant reconstruction, sentinel lymph node biopsy, internal mammary vessel preparation, microvascular anastamosis, and flap inset and allow for an inconspicuous skin island that is easy to monitor and subsequently easy to remove or incorporate into a future nipple and areola reconstruction. Furthermore, using any of the vertical incision patterns facilitates correction of recurrent ptosis to improve aesthetic outcome at a later date.
Transverse incision patterns (ie, lateral, circum-lateral, and transverse) result in lesser quality aesthetics and are best reserved for cases where patients have preexisting horizontal breast scars. In the current study, transverse incision patterns were graded least favorable (P < 0.00001). Ostensibly, the transverse and vertical incision patterns create an equivalent scar burden, with perhaps a lateral extension being even more inconspicuous. In practice, the lateral extension can undergo scar contraction, which causes lateralization of the nipple. In fact, it has been shown as a significant risk factor for nipple malposition in nipple-sparing mastectomy reconstruction.12 A lateral scar also limits secondary option for adjusting the skin envelope to correct breast ptosis.6
These conclusions also apply to bilateral breast reconstruction cases; however, breast scar symmetry has an even greater effect on aesthetic outcome. Therefore, in bilateral reconstruction cases, where a transverse breast scar is already present on one of the breasts, ideal aesthetics may be achieved by violating the principles described above and completing the mastectomy and reconstruction via transverse incisions on both breasts (Fig. 3).
The primary focus of the present study relates to the influence of mastectomy incision design on aesthetic outcomes following breast reconstruction. When considering how to implement the conclusions described by the authors, the practicing plastic surgeon must contextualize the surgical plan with the individual patient’s oncologic needs, treatment plan, general state of health, breast size and shape, body mass index, and the patient’s preference and priorities.13,14 Obstacles to executing the ideal breast reconstruction will inevitably arise and the surgical plan must be modified to preserve the patient’s health and promote uneventful healing as the primary directives.
CONCLUSIONS
Mastectomy and breast reconstruction performed via hidden incisions yield highly aesthetic results. Vertically oriented scars are cosmetically favorable to transversely oriented scars in both nipple-sparing and non-nipple-sparing reconstructions. Transverse scars may be used in cases where a previous horizontal excision scar is present. Symmetric scars should be maintained in bilateral cases.
ACKNOWLEDGMENTS
These data have not been previously presented at any congress, have not been previously published, and have not been simultaneously submitted to any other journal.
Footnotes
Published online 24 September 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Frey JD, Salibian AA, Levine JP, et al. Incision choices in nipple-sparing mastectomy: a comparative analysis of outcomes and evolution of a clinical algorithm. Plast Reconstr Surg. 2018;142:826e–835e. [DOI] [PubMed] [Google Scholar]
- 2.Odom EB, Parikh RP, Um G, et al. Nipple-sparing mastectomy incisions for cancer extirpation prospective cohort trial: perfusion, complications, and patient outcomes. Plast Reconstr Surg. 2018;142:13–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blechman KM, Karp NS, Levovitz C, et al. The lateral inframammary fold incision for nipple-sparing mastectomy: outcomes from over 50 immediate implant-based breast reconstructions. Breast J. 2013;19:31–40. [DOI] [PubMed] [Google Scholar]
- 4.Dec W.Scarless breast reconstruction: indications and techniques for optimizing aesthetic outcomes in autologous breast reconstruction. Plast Reconstr Surg Glob Open. 2018;6:e1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scholz T, Kretsis V, Kobayashi MR, et al. Long-term outcomes after primary breast reconstruction using a vertical skin pattern for skin-sparing mastectomy. Plast Reconstr Surg. 2008;122:1603–1611. [DOI] [PubMed] [Google Scholar]
- 6.Becker H, Lind JG, 2nd, Hopkins EG.Immediate implant-based prepectoral breast reconstruction using a vertical incision. Plast Reconstr Surg Glob Open. 2015;3:e412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dayicioglu D, Tugertimur B, Zemina K, et al. Vertical mastectomy incision in implant breast reconstruction after skin sparing mastectomy: advantages and outcomes. Ann Plast Surg. 2016;76suppl 4S290–S294. [DOI] [PubMed] [Google Scholar]
- 8.Spear SL, Rottman SJ, Seiboth LA, et al. Breast reconstruction using a staged nipple-sparing mastectomy following mastopexy or reduction. Plast Reconstr Surg. 2012;129:572–581. [DOI] [PubMed] [Google Scholar]
- 9.Alperovich M, Tanna N, Samra F, et al. Nipple-sparing mastectomy in patients with a history of reduction mammaplasty or mastopexy: how safe is it? Plast Reconstr Surg. 2013;131:962–967. [DOI] [PubMed] [Google Scholar]
- 10.Dec W.Optimizing aesthetic outcomes for breast reconstruction in patients with significant macromastia or ptosis. JPRAS Open. 2018;16:24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dec W.Optimizing aesthetic outcomes in delayed breast reconstruction. Plast Reconstr Surg Glob Open. 2017;5:e1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Small K, Kelly KM, Swistel A, et al. Surgical treatment of nipple malposition in nipple-sparing mastectomy device-based reconstruction. Plast Reconstr Surg. 2014;133:1053–1062. [DOI] [PubMed] [Google Scholar]
- 13.Daar DA, Abdou SA, Rosario L, et al. Meta-analysis is there a preferred incision location for nipple-sparing mastectomy? A systematic review and meta-analysis. Plast Reconstr Surg. 2019;143:906e–919e. [DOI] [PubMed] [Google Scholar]
- 14.Choi M, Frey JD, Salibian AA, et al. Nipple-areola complex malposition in nipple-sparing mastectomy: a review of risk factors and corrective techniques from greater than 1000 reconstructions. Plast Reconstr Surg. 2017;140:247e–257e. [DOI] [PubMed] [Google Scholar]


