Abstract
Background:
The extensive nature of perforator-based breast reconstructions, combined with the need for postoperative flap monitoring, often leads to long hospitalizations. We present an early report demonstrating the feasibility and advantages of a modified operative technique and recovery protocol, allowing us to perform outpatient breast reconstructions with the DIEP flap. This follow-up comprises the experience gained, which is expanded to other perforator-based flaps and not limited to DIEP breast reconstructions.
Methods:
We have implemented a general protocol in patients undergoing breast reconstruction with autologous flaps, promoting early mobilization and discharge by improving postoperative pain and decreasing opioid requirements. This protocol includes intraoperative local anesthesia, a microfascial incision for DIEP harvest with rib preservation, along with prophylactic anticoagulation.
Results:
Ninety-two consecutive patients underwent autologous tissue-based breast reconstruction with DIEP, IGAP, and PAP flaps. No intraoperative complications were reported. All patients were discharged within 23 hours, without evidence of flap compromise. One patient required operative takeback for evacuation of a hematoma on postoperative day 4. No partial or total flap losses were documented. The aim of any procedure should be to get to the patient back to the preoperative status as quickly as possible, as prolonged hospitalizations are associated with higher incidences of infection, deep venous thrombosis, overall dissatisfaction, and higher overall costs of care.
Conclusions:
By using a modified operative technique, multimodal pain control, and postoperative anticoagulant therapy, outpatient perforator-flap–based breast reconstructions can be performed with high success and low complication rates.
INTRODUCTION
The use of autologous flaps for breast reconstruction following mastectomies has become the gold standard for plastic surgeons, a testament to the long-term cosmetic results and improvements made in donor-site morbidity. Despite the wide variety of flaps available, perforator-based abdominal flaps, such as the deep inferior epigastric perforator (DIEP) or the superficial inferior epigastric artery flaps (SIEA), remain the first choice for many patients and surgeons. Other perforator-based flaps, such as the inferior and superior gluteal artery perforator (IGAP, SGAP) or the profunda artery perforator (PAP), are an option when abdominal tissue is insufficient, and yield excellent cosmetic results.
Although breast reconstruction using either of the above-mentioned flap techniques is an excellent option, their complexity and expertise required in microvascular surgery are noteworthy. The extensive nature of the procedure, combined with the need for postoperative flap monitoring, often leads to lengthy hospitalizations. In an early report of 14 consecutive patients, we demonstrated the feasibility and advantages of a modified operative technique and recovery protocol, allowing us to perform outpatient breast reconstructions with the DIEP flap.1 We present a follow-up to our early discharge protocol expanded to other perforator-based flaps for breast reconstruction.
PATIENTS AND METHODS
Following Institutional Review Board approval, we performed a retrospective review of patients who underwent autologous-based breast reconstruction by the senior author, following benign and malignant disease from April 2018 to September 2019. Demographic data, as well as intraoperative and postoperative outcomes, were collected and assessed, and a retrospective analysis was conducted. Categorical and continuous variables were expressed as frequency (%) and mean ± SD, respectively.
Preoperative
Non-diabetic patients are instructed to drink 12 ounces of carbohydrate and electrolyte-rich beverages (ie, Gatorade) the evening before surgery and an additional 12 ounces 3 hours before anesthesia induction. In addition, patients are given oral acetaminophen (1000 mg) and gabapentin (400 mg) before surgery.
Intraoperative
Intercostal peripheral nerve blocks are performed at the beginning of the procedure, utilizing a blend of 15 mL of 1.3% bupivacaine liposome (Exparel) with 40 mL of 0.25% bupivacaine hydrochloride (Marcaine) on each chest in bilateral cases, and 15 mL Exparel with 25 mL Marcaine on the ipsilateral chest in unilateral cases, with all injections performed by the surgeon.
Internal mammary vessel preparation is performed in the lowest possible interspace, where either complete or partial rib removal can be avoided (Fig. 1). For single-perforator DIEP flap harvest, a microfascial incision between 1.2 and 2.2 cm is used. For multiple-perforator DIEP flap harvest, the incision is limited to the distance between the perforators, such that the distance is <3.5 cm. For PAP and GAP flap harvest, the dissection is performed above the fascial up to the level of the perforators. The fascia is incised around the perforators and repaired after harvest of the flap.
Fig. 1.
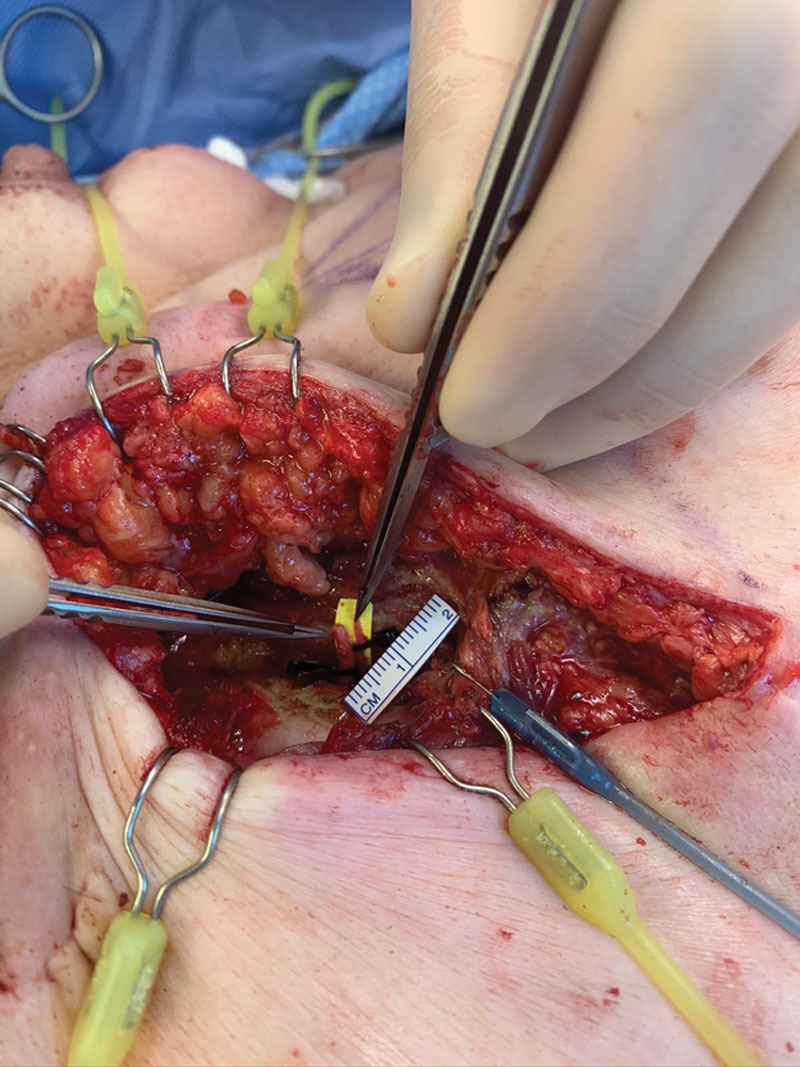
Photograph showing internal mammary vessel preparation without damage (total or partial) to the ribs.
Following DIEP flap harvest, transverse abdominis plane (TAP) blocks are performed utilizing 15 mL of the bupivacaine blend bilaterally using the same concentration as used for both unilateral and bilateral cases. In cases of stacked reconstructions with 4 flaps, 10 mL is used for TAP blocks, and 5 mL for subfascial injection around the fascial incision. Suction drains are placed in all surgical sites and every patient undergoes green-indocyanine fluoroscopy to evaluate flap perfusion.
Postoperative
Following surgery, each patient is monitored overnight and kept on bedrest. Monitoring is performed by handheld Doppler exam and clinical evaluation of the color of the flap. In the case of completely buried flaps, a small segment of the incision is partially closed with a purse-string suture, and the flap is evaluated through the purse-string with the Doppler and assessed for color. A subcutaneous dose of 30 mg enoxaparin (Lovenox) is given on the evening of their surgery. Oral and IV analgesia, acetaminophen/hydrocodone (Norco, 10/325 mg), and Hydromorphone (Dilaudid, 0.2 mg), respectively, is used for breakthrough pain. By 6 am the following morning, patients are moved to a chair and Foley catheters are removed. At this time, patients are started on 800 mg of Ibuprofen along with a proton-pump inhibitor for a minimum of 3 weeks. After 30 minutes, flaps are assessed by the surgeon and if adequate, monitoring is discontinued. Ambulation is encouraged and patients are cleared for home discharge at 7:30 am. For buried flaps, the purse string is closed before discharge. Finally, we place our patients on a daily dose of rivaroxaban (10 mg) for 9 days as anticoagulation therapy.
Patients return to the clinic for evaluation at postoperative day 4 or 5. Flaps are reassessed at that time for viability. In the case of completely buried flaps, the area of the Doppler signal is evaluated transcutaneously at the purse-string site. If there are any concerns, the purse-string is opened and the flap is directly evaluated.
RESULTS
Ninety-two consecutive patients underwent autologous tissue-based breast reconstruction in three different medical institutions by the senior author. Reconstruction techniques included DIEP, IGAP, and PAP. Also, stacked configurations of these techniques were used in cases where abdominal fat tissue was inadequate or unavailable. Demographics of the series are summarized in Table 1. None of the patients were actively smoking. Mean total operative times were calculated from anesthesia induction to thirty minutes in the recovery room. For immediate unilateral cases, it was 318 ± 38 minutes (range, 260–361), and 426 ± 24 minutes (range, 362–486) for bilateral cases, while unilateral cases with a delayed approach was 263 ± 26 minutes (range, 235–315), and 384 ± 53 minutes (range, 321–450) for bilateral. Abdominal microfascial incisions to harvest the DIEP flap pedicle ranged from 1.2 to 3.5 cm. For single perforator flaps, the fascial incision ranged from 1.2 to 2.2 cm (Fig. 2), while incisions for multiple perforators were based on the distance between the perforators (Fig. 3) with the average number of perforators per DIEP flap being 2 (range, 1–4). No intraoperative complications were reported.
Table 1.
Patient Demographics and Flap Characteristics
| Parameter | Value |
|---|---|
| Total no. patients | 92 |
| Mean age at date of operation, y | 47.8 ± 9.4 (range, 29–80) |
| Mean body mass index, kg, m2 | 25.6 ± 4.3 (range, 18–42) |
| Patients with previous abdominal surgeries, % | 37 (40) |
| Mastectomy for cancer, % | 84 (91) |
| Mastectomy for benign or premalignant disease, % | 8 (9) |
| Prereconstruction therapy | |
| Radiation, % | 31 (33) |
| Chemotherapy, % | 24 (26) |
| Radiation + chemotherapy, % | 9 (9.7) |
| Timing of breast reconstruction | |
| Immediate | 47 (51) |
| Delayed | 45 (49) |
| Type of reconstruction | |
| DIEP | 45 bilateral, 23 unilateral |
| PAP* | 4 |
| IGAP† | 1 |
| Stacked IGAP/DIEP† | 1 |
| Stacked DIEP/DIEP† | 6 |
| Stacked DIEP/PAP* | 7 |
| Stacked PAP/PAP† | 5 |
| Complications | |
| Venous thrombosis | 0 |
| Arterial thrombosis | 0 |
| Flap hematoma | 1 |
| Partial/total flap loss | 0 |
| Donor-site complications | 1 |
| Skin flap necrosis | 7 |
| Other | 1 |
| Mean follow-up, wk | 26 (range, 11–31) |
Bilateral.
Unilateral.
Fig. 2.
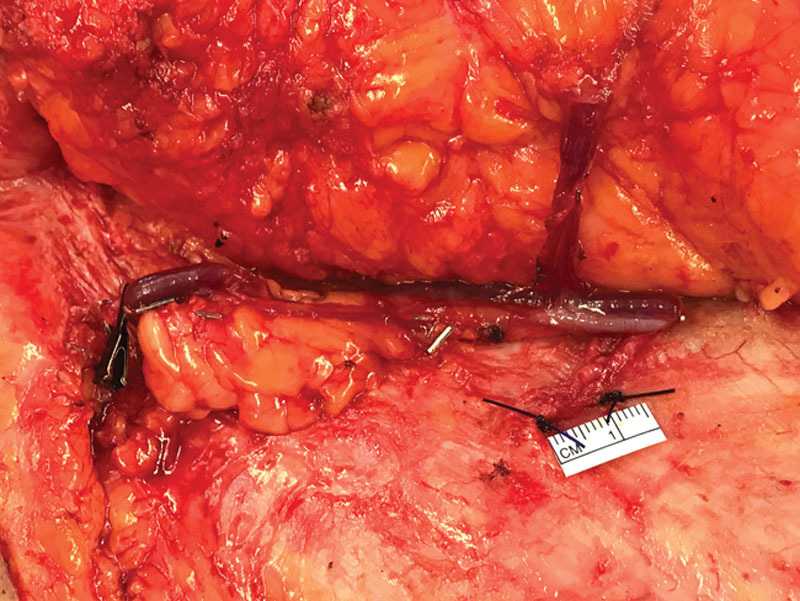
Photograph showing the microfascial incision for single perforators, ranging from 1.2 to 2.2 cm.
Fig. 3.
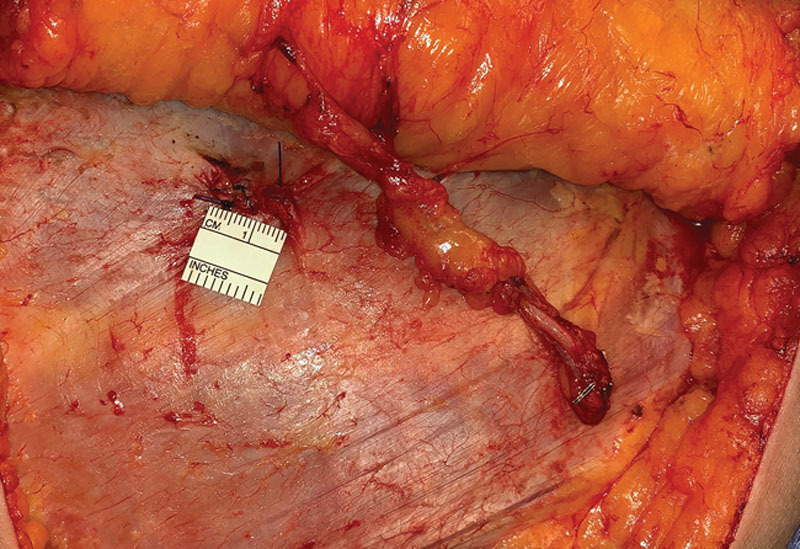
The microfascial incision is based on the distance between the perforators (2 visualized), ranging from 1.5 to 3.5 cm.
One bilateral DIEP case required operative take-back three hours postoperatively due to concerns of unilateral congestion. During exploration there was no evidence of compromise to the venous system; therefore, no further intervention was required. All patients were discharged within 23 hours with strong Doppler signals and no evidence of flap compromise. One patient in the series, with a BMI of 18.7, required bilateral mastectomies. She underwent immediate reconstruction of the prophylactic side with a gluteal flap. She subsequently underwent reconstruction of the cancerous side, which required a larger volume and skin replacements than available from her gluteal flap alone. For this reason, she underwent a delayed stacked DIEP/IGAP reconstruction on the radiated side.
Of the 92 patients, 2 required readmissions. One patient with a prior history of pulmonary embolism was admitted due to acute dyspnea on postoperative day three; however, imaging studies revealed no acute disease, and the patient was promptly discharged the next day. The second patient developed sudden inflammation of the breast on postoperative day 4 and was taken to the operating room for evacuation of a suspected expanding hematoma; arterial bleeding was found from a perforator of the internal mammary artery (IMA) in the medial chest, which was controlled without further complications. Several minor complications were noted, with 1 patient requiring drainage and curettage of a suture abscess located in the reconstructed breast, while another developed dehiscence of the abdominal incision without signs of infection. Seven patients required minor debridement (<10 cm2) of the mastectomy skin flap due to necrosis. No partial or total flap losses were documented, nor events of venous thromboembolism. Average follow-up for the series was 26 weeks.
DISCUSSION
Microvascular breast reconstruction has advanced greatly over the past several years. Rates of flap failure have decreased dramatically, as expertise in microvascular techniques has grown.2,3
Length of stay is another metric that has improved dramatically over time. Initially, patients would often stay in the hospital for periods up to 10 days following flap-based breast reconstruction. Subsequently, hospital time has decreased in most centers. The aim of any procedure should be to get the patient back to the preoperative status as quickly as possible, as prolonged hospitalizations are associated with higher incidences of infection, deep venous thrombosis, patient dissatisfaction, and higher overall costs of care.4–11
Early recovery protocols or fast-track surgeries are not a novelty, and encompass multimodal (and multidisciplinary) methods aimed at resolving problems that delay recovery and cause complications, thus extending hospitalizations. A great example is the enhanced recovery after surgery (ERAS) protocol, developed by European surgeons and published in 2005.12 This protocol described a consensus of previous reports by the ERAS authors showing reductions in length of stay by approaching different aspects of the perioperative scenario other than the surgery itself, such as nutrition and its metabolic ramifications or pain management and how it can improve postoperative mobility and bowel function.13–15 This protocol has since branched to many surgical areas, such as colorectal or orthopedic surgery, and developed particular procedures to accommodate the specific needs of their patients, albeit maintaining the essence of ERAS.
Likewise, our enhanced protocol adapts some of the ideas initially described by ERAS and includes specific procedures such as the microfascial incision or avoiding removal (partial or total) of the rib, initially demonstrated in our previous study.1 Thus, it has become a standard of care with our patients to use a combination of modified surgical techniques with complete avoidance of rib harvest along with microfascial incisions for DIEP flap vessel dissection, in addition to multimodal pain control and postoperative antithrombotic regimen. From the DIEP flap, we have learned that a limited fascial incision results in a decreased overall amount of pain and a faster overall recovery period.
With PAP and IGAP flaps, we had noticed a higher incidence of seroma formation, if the procedure is done in a subfascial manner. While subfascial dissection facilitates perforator identification, with experience, suprafascial dissection can be performed. In our experience with suprafascial dissection, the seroma and therefore complication rate is decreased. Furthermore, in our experience there is also less pain associated with this, as the maintenance of the fascia seemed to decrease patient’s postoperative pain and enhanced their overall recovery.
This study is the first to expand the outpatient DIEP flap microvascular breast reconstruction to include non-abdominal based flap, such as GAP and PAP flaps. We have an increasing trend in our practice toward the PAP flap, for which we do a vertical PAP. We found that this flap method results in an excellent overall thigh outcome with minimal issues related to long-term scar spreading.
Our rationale for outpatient flaps goes beyond decreasing the length of stay. We also believe that the main original impetus for prolonged length of stay was for flap monitoring.16–19 Arterial insufficiency, a result of a problematic microvascular anastomosis, unexpected vasospasms, or thrombogenic events, is a worrisome occurrence leading to flap compromise; however, it is venous insufficiency in perforator flaps that is the most common cause of take-backs and partial or total failure.20–25 In our experience, flap vascular complications typically happen within the first 23 hours after surgery, and are typically identified within that initial timeframe. Arterial-related vascular problems are typically encountered within the first 12 hours, with the greatest occurrence in the initial 6 hours, as opposed to venous complications, which present with more time variability.23 Furthermore, it is also our belief that postoperative vascular complications associated with flaps that are identified after 12 hours tend not to be salvageable and more often than not, will result in inevitable flap loss, as reperfusion injury and critical ischemia lead to a substantial amount of fat necrosis, although attempts to salvage flaps with extremely delayed presentation (>5 days) of vascular compromise have been successful with aggressive thrombolytic therapy,26 along with direct thrombectomy,27 or surgical approaches such as vein grafting, change of recipient vessels, and reanastomosis.28–30
Finally, we are still exploring criteria that would contraindicate patients from undergoing breast reconstruction with this protocol, such as severe radiation damage to the chest vessels or hypercoagulability states like Factor V Leiden.
CONCLUSION
With our modified operative technique, multimodal pain control, and postoperative anticoagulant therapy, we have been able to perform outpatient perforator-flap–based breast reconstructions with high success and low complication rates.
Footnotes
Published online 23 September 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Martinez CA, Reis SM, Rednam R, et al. The outpatient DIEP: safety and viability following a modified recovery protocol. Plast Reconstr Surg Glob Open. 2018;6:e1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leyngold MM.Is unipedicled transverse rectus abdominis myocutaneous flap obsolete owing to superiority of DIEP flap? Ann Plast Surg. 2018;806S suppl 6S418. [DOI] [PubMed] [Google Scholar]
- 3.Saaristo AM, Niemi TS, Viitanen TP, et al. Microvascular breast reconstruction and lymph node transfer for postmastectomy lymphedema patients. Ann Surg. 2012;255:468–473. [DOI] [PubMed] [Google Scholar]
- 4.Glicksman A, Ferder M, Casale P, et al. 1457 years of microsurgical experience. Plast Reconstr Surg. 1997;100:355–363. [DOI] [PubMed] [Google Scholar]
- 5.Fischer JP, Sieber B, Nelson JA, et al. Comprehensive outcome and cost analysis of free tissue transfer for breast reconstruction: an experience with 1303 flaps. Plast Reconstr Surg. 2013;131:195–203. [DOI] [PubMed] [Google Scholar]
- 6.Collins TC, Daley J, Henderson WH, et al. Risk factors for prolonged length of stay after major elective surgery. Ann Surg. 1999;230:251–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rowell KS, Turrentine FE, Hutter MM, et al. Use of national surgical quality improvement program data as a catalyst for quality improvement. J Am Coll Surg. 2007;204:1293–1300. [DOI] [PubMed] [Google Scholar]
- 8.Krishnan NM, Purnell C, Nahabedian MY, et al. The cost effectiveness of the DIEP flap relative to the muscle-sparing TRAM flap in postmastectomy breast reconstruction. Plast Reconstr Surg. 2015;135:948–958. [DOI] [PubMed] [Google Scholar]
- 9.Atherton DD, Hills AJ, Moradi P, et al. The economic viability of breast reconstruction in the UK: comparison of a single surgeon’s experience of implant; LD; TRAM and DIEP based reconstructions in 274 patients. J Plast Reconstr Aesthet Surg. 2011;64:710–715. [DOI] [PubMed] [Google Scholar]
- 10.Khan NA, Quan H, Bugar JM, et al. Association of postoperative complications with hospital costs and length of stay in a tertiary care center. J Gen Intern Med. 2006;21:177–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dimick JB, Chen SL, Taheri PA, et al. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199:531–537. [DOI] [PubMed] [Google Scholar]
- 12.Fearon KC, Ljungqvist O, Von Meyenfeldt M, et al. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2005;24:466–477. [DOI] [PubMed] [Google Scholar]
- 13.van der Hulst RR, van Kreel BK, von Meyenfeldt MF, et al. Glutamine and the preservation of gut integrity. Lancet. 1993;341:1363–1365. [DOI] [PubMed] [Google Scholar]
- 14.Balteskard L, Unneberg K, Mjaaland M, et al. Growth hormone and insulinlike growth factor 1 promote intestinal uptake and hepatic release of glutamine in sepsis. Ann Surg. 1998;228:131–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fearon KC, Falconer JS, Slater C, et al. Albumin synthesis rates are not decreased in hypoalbuminemic cachectic cancer patients with an ongoing acute-phase protein response. Ann Surg. 1998;227:249–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Selber JC, Angel Soto-Miranda M, Liu J, et al. The survival curve: factors impacting the outcome of free flap take-backs. Plast Reconstr Surg. 2012;130:105–113. [DOI] [PubMed] [Google Scholar]
- 17.Cai ZG, Zhang J, Zhang JG, et al. Evaluation of near infrared spectroscopy in monitoring postoperative regional tissue oxygen saturation for fibular flaps. J Plast Reconstr Aesthet Surg. 2008;61:289–296. [DOI] [PubMed] [Google Scholar]
- 18.Bui DT, Cordeiro PG, Hu QY, et al. Free flap reexploration: indications, treatment, and outcomes in 1193 free flaps. Plast Reconstr Surg. 2007;119:2092–2100. [DOI] [PubMed] [Google Scholar]
- 19.Jonas R, Schaal T, Krimmel M, et al. Monitoring in microvascular tissue transfer by measurement of oxygen partial pressure: four years experience with 125 microsurgical transplants. J Craniomaxillofac Surg. 2013;41:303–309. [DOI] [PubMed] [Google Scholar]
- 20.Chen CM, Halvorson EG, Disa JJ, et al. Immediate postoperative complications in DIEP versus free/muscle-sparing TRAM flaps. Plast Reconstr Surg. 2007;120:1477–1482. [DOI] [PubMed] [Google Scholar]
- 21.Tran NV, Buchel EW, Convery PA.Microvascular complications of DIEP flaps. Plast Reconstr Surg. 2007;119:1397–1405; discussion 1406. [DOI] [PubMed] [Google Scholar]
- 22.Chang EI, Carlsen BT, Festekjian JH, et al. Salvage rates of compromised free flap breast reconstruction after recurrent thrombosis. Ann Plast Surg. 2013;71:68–71. [DOI] [PubMed] [Google Scholar]
- 23.Ochoa O, Pisano S, Chrysopoulo M, et al. Salvage of intraoperative deep inferior epigastric perforator flap venous congestion with augmentation of venous outflow: flap morbidity and review of the literature. Plast Reconstr Surg Glob Open. 2013;1:e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blondeel PN, Arnstein M, Verstraete K, et al. Venous congestion and blood flow in free transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flaps. Plast Reconstr Surg. 2000;106:1295–1299. [DOI] [PubMed] [Google Scholar]
- 25.Enajat M, Rozen WM, Whitaker IS, et al. A single center comparison of one versus two venous anastomoses in 564 consecutive DIEP flaps: investigating the effect on venous congestion and flap survival. Microsurgery. 2010;30:185–191. [DOI] [PubMed] [Google Scholar]
- 26.Trussler AP, Watson JP, Crisera CA.Late free-flap salvage with catheter-directed thrombolysis. Microsurgery. 2008;28:217–222. [DOI] [PubMed] [Google Scholar]
- 27.Hong KY, Chang LS, Chang H, et al. Direct thrombectomy as a salvage technique in free flap breast reconstruction. Microsurgery. 2017;37:402–405. [DOI] [PubMed] [Google Scholar]
- 28.Largo RD, Selber JC, Garvey PB, et al. Outcome analysis of free flap salvage in outpatients presenting with microvascular compromise. Plast Reconstr Surg. 2018;141:20e–27e. [DOI] [PubMed] [Google Scholar]
- 29.Troeltzsch M, Troeltzsch M, Probst FA, et al. Current concepts in salvage procedures for failing microvascular flaps: is there a superior technique? Insights from a systematic review of the literature. Int J Oral Maxillofac Surg. 2016;45:1378–1387. [DOI] [PubMed] [Google Scholar]
- 30.Chang EI, Chang EI, Soto-Miranda MA, et al. Comprehensive evaluation of risk factors and management of impending flap loss in 2138 breast free flaps. Ann Plast Surg. 2016;77:67–71. [DOI] [PubMed] [Google Scholar]


