Supplemental Digital Content is available in the text.
Summary:
Craniofacial clinics are composed of multidisciplinary teams of providers to deliver coordinated and comprehensive patient care. The coronavirus disease of 2019 (COVID-19) pandemic has disrupted this model, as social distancing guidelines have precluded in-person patient appointments and forced clinics to reconsider their method of care delivery. The University of California, San Francisco, Craniofacial Center has continued to serve patients during this acute period, adopting a hybrid model in which the vast majority of patients are seen through telehealth and a limited number of patients are evaluated in-person. Surveyed patients and families reported high rates of satisfaction, with time savings cited as a particular benefit. Furthermore, most felt comfortable using the video technology required for their appointment. This experience has demonstrated to us that multidisciplinary craniofacial evaluations can be effectively delivered in a telehealth format and has informed our conception of idealized clinic structure. Moving forward, we intend to utilize telehealth visits for selected components of craniofacial evaluations in an effort to maximize efficiency and minimize burden, including addressing barriers to accessing care. Benefits of a hybrid model will include decongestion of clinics and waiting areas, allowing social distancing, addressing clinic space limits, and increased efficiency by eliminating the need for patient and family movement. Demonstration of the safety and efficacy of telehealth visits, combined with regulatory reform that improves reimbursement and allows for appointments across state lines, will be critical for this model to persist beyond the pandemic.
INTRODUCTION
Craniofacial care involves evaluation and treatment by a coordinated interdisciplinary group of providers who typically work in close proximity, seeing common patients in the same clinic space.1–3 However, social distancing restrictions imposed during the coronavirus disease of 2019 (COVID-19) pandemic have disrupted this model of care.4,5
The University of California, San Francisco (UCSF), Craniofacial Center treats patients from throughout northern California and surrounding states. The COVID-19 pandemic prompted our clinic to continue patient care by adopting telehealth for most visits. This article describes our experience, presents preliminary patient satisfaction data, and discusses potential implications for the future of craniofacial care.
CHANGES TO CLINIC OPERATION
Patients seen in-person include those with time-sensitive diagnostic questions (eg, craniosynostosis evaluations where video was inadequate) or those with postoperative visits requiring wound care. About 1% of families did not have access to adequate internet connectivity and video technology; these patients came either to our clinic or to their local pediatrician’s office to attend their video visits.
Telehealth visits are scheduled throughout the day, intermixed with in-person visits. Before their appointments, all telehealth patients receive written reminders containing the teleconferencing hyperlink. For non-English speaking patients, interpreters are either booked in advance or invited to the virtual meeting in real time. To ensure confidentiality, all video visits take place over Zoom meetings through UCSF’s Health Insurance Portability and Accountability Act-compliant platform.
Onsite providers are each assigned a clinic room in which they see all telehealth and in-person patients. This puts providers and patients at ease by minimizing contact between individuals. For patients with at least one in-person visit, evaluations by other providers are often completed virtually using a workstation in the clinic. This promotes social distancing, but allows clinicians to examine the patient if necessary. Early in our transition, we scheduled fewer appointments and ensured that adequate technical support staff were available to address any issues that arose. However, after several clinic days, video visits took no longer to complete than in-person consultations. After all appointments are completed, care plans are finalized during the virtual, multidisciplinary craniofacial conference.
PATIENT VOLUME AND SATISFACTION
During this transition, the UCSF Craniofacial Center saw an average of 40 patients across 81 individual provider appointments each day, compared with an average of 58 patients across 138 appointments the year prior (Fig. 1). An estimated 88% of recent visits occurred over telehealth, whereas none occurred before COVID-19. Compared with the first weeks of the pandemic, the clinic volume has increased and is now at pre-COVID levels.
Fig. 1.
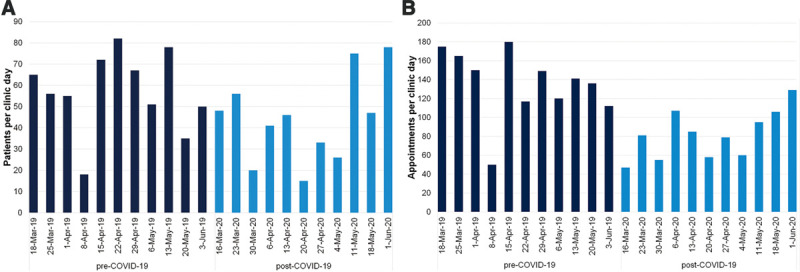
Craniofacial Center patient volume, 2019–2020. For each clinic day, the number of (A) unique patients and (B) total appointments for all Craniofacial Center providers is compared between March–June 2019 and March–June 2020. Clinic days before the COVID-19 pandemic are plotted in navy, and those after the shift to telehealth are plotted in light blue.
All English- and Spanish-speaking patients who had video visits received satisfaction surveys (see Supplemental Digital Content 1, which displays patient satisfaction survey. This patient satisfaction survey was sent to all English-speaking telehealth patients following their video visits. A Spanish version, translated by certified interpreters, was sent to all Spanish-speaking telehealth patients, http://links.lww.com/PRSGO/B483). In total, 87% of patients somewhat or strongly agreed that they were satisfied with their video visits, and nearly all felt comfortable using the telehealth technology (Fig. 2A). Furthermore, 87% of patients agreed that video visits saved time, with a median of 3 hours saved (interquartile range, 0.5–4.25 hours), and 68% reported the visits saved money. However, only 26% preferred video visits over in-person appointments, with the desire to have a physical examination cited as the most common reason among the 47% who disagreed. When prompted, many of these patients agreed that telehealth was sufficient for some visits if a regular schedule of in-person visits were maintained.
Fig. 2.
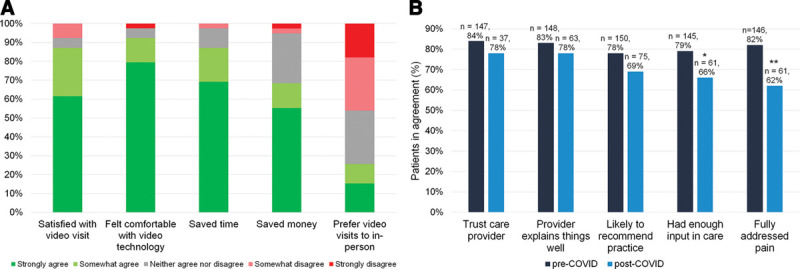
Patient experience survey data. A, Patient satisfaction surveys were sent to all English- and Spanish-speaking patients seen via telehealth between March and May 2020 (n = 123), and 39 responded. Patients indicated their level of agreement on a 5-point Likert scale (see Supplemental Digital Content 1, which displays patient satisfaction survey. This patient satisfaction survey was sent to all English-speaking telehealth patients following their video visits. A Spanish version, translated by certified interpreters, was sent to all Spanish-speaking telehealth patients, http://links.lww.com/PRSGO/B483). B, Standardized patient experience surveys are routinely administered after each appointment at UCSF. Aggregated responses from the UCSF Craniofacial Center before (navy) and after (light blue) the transition to telehealth were collected. The percentage of patients in agreement with each statement is shown. Statistically significant differences on χ2 tests are indicated with * (P < 0.05) or ** (P < 0.01).
We also compared standardized patient experience surveys between the period of the pandemic and the year before, using chi-square tests (Fig. 2B). Before and after our telehealth transition, similar proportions of patients trusted their provider (P = 0.39), found that their provider explained things well (P = 0.36), and would recommend their provider to a friend (P = 0.13). Fewer telehealth patients agreed that their pain was fully addressed (62% versus 82%; P = 0.002) and felt that they had enough input in their care (66% versus 79%; P = 0.04). These findings suggest that providers should receive specific training to ensure that patients feel heard during video visits, which is likely to improve care and satisfaction.
FUTURE CONSIDERATIONS FOR CRANIOFACIAL CARE
Prior studies have demonstrated the efficacy of telehealth in cleft care, and our experience here shows that interdisciplinary craniofacial care can be delivered virtually.6,7 This experience has led us to re-envision how ideal craniofacial clinics will be structured in the future. In our experience, many evaluations can be accomplished over video, especially annual follow-up visits unlikely to require major intervention.
Reducing in-person visits has many benefits. We have observed an improvement in clinic flow due to a decrease in late arrivals, as telehealth visits obviate physical travel. Providers were highly satisfied, noting that families were highly engaged during visit conversations, and everyone felt safer with remote visits. Many perceived the inability to examine patients in-person as a limitation but developed mitigating strategies, such as coaching parents to improve intraoral exposure using spoons as retractors.
Certain limits to the use of telehealth remain. For example, in positional plagiocephaly, equivocal history, and inability to take measurements is an indication for an in-person visit. Additionally, in-person examination is usually necessary for craniofacial evaluations by otolaryngology and ophthalmology, for feeding evaluations in patients with cleft palate, and for lip molding. Most precarious are the gray areas that arguably would be more accurate with in-person evaluations (including radiographs), such as assessment of bone graft timing in patients with clefts. Moreover, our survey data suggest that telehealth may negatively impact patient perception of care, and patients vary in their overall preference for video versus in-person visits. Finally, the technology necessary for video visits represents a barrier for some patients.
The financial viability of this model of care and whether current reforms will persist will determine whether telehealth remains sustainable. During the pandemic, reimbursement for telehealth has improved to match that of in-person services, and our institution has permitted us to perform video visits that are billable at the same level as in-person visits for the foreseeable future.8,9
The limitations of this report include response bias in our patient satisfaction surveys, which had a response rate of 32%, and our inability to collect payment data, which is generated many months after services are billed. Finally, the extent to which telehealth is viable in diverse settings will depend on access to technology and literacy that is not yet universal.
Supplementary Material
Footnotes
Published online 14 September 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Goldberg R. Standards for Approval of Cleft Palate and Cra niofacial Teams. American Cleft Palate-Craniofacial Association. https://acpa-cpf.org/wp-content/uploads/2017/06/standards.pdf. Accessed May 26, 2020.
- 2.Alleyne B, Okada HC, Leuchtag RM, et al. Cleft and craniofacial clinic formats in the United States: national and institutional survey. J Craniofac Surg. 2017;28:693. [DOI] [PubMed] [Google Scholar]
- 3.Capone RB, Sykes JM.The cleft and craniofacial team: the whole is greater than the sum of its parts. Facial Plast Surg. 2007;23:83–86. [DOI] [PubMed] [Google Scholar]
- 4.Denadai R, Lo LJ.Teleconsultation-mediated nasoalveolar molding therapy for babies with cleft lip/palate during the COVID-19 outbreak: implementing change at pandemic speed. J Plast Reconstr Aesthet Surg. 2020;73:1357–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schoenbrunner A, Sarac B, Gosman A, et al. Considerations for pediatric craniofacial surgeons during the COVID-19 outbreak. J Craniofac Surg. 2020. [E-pub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Asiri A, AlBishi S, AlMadani W, et al. The use of telemedicine in surgical care: a systematic review. Acta Inform Med. 2018;26:201–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costa MA, Yao CA, Gillenwater TJ, et al. Telemedicine in cleft care: reliability and predictability in regional and international practice settings. J Craniofac Surg. 2015;26:1116–1120. [DOI] [PubMed] [Google Scholar]
- 8.Billig JI, Sears ED.The compounding access problem for surgical care: innovations in the post-COVID era. Ann Surg. 2022;272:e47–e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loeb AE, Rao SS, Ficke JR, et al. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28:e469–e476. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


