Abstract
Background:
Clinical treatment of plaque psoriasis typically involves a comprehensive therapy, which is expensive and unsatisfactory, and some medications have serious side effects. Moving cupping therapy has shown good clinical efficacy in the treatment of plaque psoriasis; it can significantly relieve skin inflammation and excessive thickening of plaque psoriasis and has fewer side effects. However, a comprehensive evaluation of the current clinical evidence regarding its use is lacking.
Methods:
Several databases were systematically searched from inception to March 2, 2020, including PubMed, Embase, Cochrane Central Register of Controlled Trials, China Network Knowledge Infrastructure, and Wan Fang. This review included randomized controlled trials on plaque psoriasis treatment with the use of moving cupping and in combination with Chinese herbs or conventional Western medicine therapy. These trial findings were compared with the treatment results using placebo, pharmaceutical medications, or Chinese herbs. Moving cupping treatment frequency was also compared.
Results:
Sixteen trials with 1164 participants met the inclusion criteria. Meta-analysis showed that the intervention group (moving cupping therapy) had a significant effect compared with the no-moving cupping therapy group (weighted mean difference = –1.22, 95% confidence interval [CI] [–1.58, –0.85], P < .00001 random model; I2 = 85%). Furthermore, moving cupping (weighted mean difference = –1.19, 95% CI [–1.98, –0.39], P = .003 random model; I2 = 85%) or combined with pharmaceutical medications (weighted mean difference = –1.55, 95% CI [–1.89, –1.20], P < .00001 random model; I2 = 0%) were better than pharmaceutical medications alone in treating plaque psoriasis. Cupping therapy significantly improved psoriasis recurrence rate (risk ratio = 0.33, 95% CI [0.16, 0.68], P = .003 fixed model; I2 = 28%). However, for the visual analogue score, moving cupping showed no obvious advantages (weighted mean difference = –0.27, 95% CI [–0.71, 0.17], P = .22 random model; I2 = 64%). Moreover, studies reported that moving cupping reduced serum tumor necrosis factor-α and vascular endothelial growth factor levels more significantly than pharmaceutical medications. Moving cupping was associated with few transient adverse reactions, such as redness, itching, and local skin burning.
Conclusion:
Moving cupping therapy could be an effective treatment either alone or as a combination therapy for plaque psoriasis. However, further large-scale, rigorously designed trials are needed to confirm these findings.
Keywords: moving cupping, plaque psoriasis, pharmaceutical medications
1. Introduction
Psoriasis vulgaris is a common and often chronic inflammatory skin disease. The incidence of psoriasis in Western industrialized countries ranges from 1.5% to 2%,[1] with approximately 80% of patients with psoriasis having the plaque form of the disease. For most patients, the disease means decades-long restriction of various aspects of everyday life, resulting in enormous personal costs and mental stress.[2] In addition, studies have shown that patients with psoriasis have a significantly higher risk of metabolic syndrome and cardiovascular disease than the general population.[3,4] Our previous studies have confirmed that psoriasis may be closely related to hyperuricemia and chronic obstructive pulmonary disease.[5,6]
As per the Guidelines on the treatment of psoriasis vulgaris,[7–10] the recommended treatment of plaque psoriasis should be based on the classification of the psoriasis area and severity index (PASI) scores, which determine the different treatments and drugs, such as calcineurin inhibitors, dithranol, corticosteroids, laser therapy, ultraviolet B, vitamin D3, methotrexate, and biological agents. However, these examples could not achieve the desired clinical effect, which could be attributed to poor tolerability, fear, lacking information on potential side effects, low efficacy, and complicated usage.[11,12] Thus, treatment that is cost-effective and has few side effects is needed. Moreover, current recommended treatments for plaque psoriasis should be improved and alternative treatment options considered.
In recent years, complementary and alternative medicine (CAM) therapies have become an increasingly important area of dermatology. Cupping is becoming an important therapy in CAM. Cupping therapy has the effect of regulating the T subsets of lymphocyte and reducing inflammation.[13] In addition, cupping therapy can also increase the expression of anti-inflammatory lipids (such as PGE1, 5, 6-EET, 14, 15-EET, 10S, 17S-DiHDoHE), while reducing inflammatory lipids (such as 12-HETE and thromboxane B2) in the skin and plasma.[14] Moving cupping therapy, which is a kind of cupping therapy that involves repeated movements of cups on the skin with the aid of lubrication, is safe and cost-effective. It integrates the functions of warm moxibustion, cupping, scraping, massage, and drug therapy and has a wide range of clinical applications. Lubrication in this therapy also could achieve a certain drug treatment effect. The therapeutic effects make moving cupping therapy especially suitable for treating erythematous scaly skin diseases.
In China, moving cupping therapy has been widely used as a cost-effective treatment for plaque psoriasis. Although 2 studies[15,16] have systematically reviewed cupping therapy, the results showed that it has mainly been used in herpes zoster, facial paralysis (Bell palsy), cough, dyspnea, etc., and has potential benefits for painful diseases. However, to the best of our knowledge, no systematic review evaluating the clinical evidence pertaining to the efficacy of moving cupping therapy for plaque psoriasis exists. Hence, we conducted a systematic review to evaluate the effectiveness of moving cupping therapy for plaque psoriasis.
2. Methods
The review protocol was registered in the PROSPERO database before the start of the review process (CRD42018114896). This study was performed according to the Cochrane Handbook for Systematic Reviews of Interventions[17] and is presented in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (additional file 2: PRISMA 2009 Checklist).[18]
The Cochrane Central Register of Controlled Trials, PubMed, Embase, China Network Knowledge Infrastructure (1979–2018), and Wanfang Data (1985–2018) were searched until March 2, 2020. We performed a systematic review and meta-analysis to evaluate the efficacy and safety using moving cupping therapy for plaque psoriasis. This study is based on existing literature, and therefore does not require approval from the ethics committee. The search terms included “moving cupping” and “plaque psoriasis.” Unpublished postgraduate theses in Chinese databases also were searched (Fig. 1). Randomized controlled trials (RCTs) where interventions for the treatment of plaque psoriasis included the use of moving cupping, or in combination with Chinese herbs or conventional Western medicine therapy, were included in this review. Findings from these trials were compared with the results of treatment using placebo, conventional Western medicine therapy, or Chinese herbs. Trials were excluded if any of the following factors were identified: insufficient information concerning evaluation rates, lack of moving cupping therapy data, combined moving cupping therapy appeared in the control group, and animal trials. Responses to interventions were classified as follows: cure (at least 90% PASI score reduction, leaving only mild pigmentation), markedly effective (60–89% PASI score reduction), effective (30–59% PASI score reduction), and ineffective (<30% PASI score reduction or if the condition worsened). To calculate the recovery rate (primary outcome), the sum of the cure and markedly effective responses were divided by the total cases between weeks 4 and 8. The secondary outcomes included the visual analogue score (VAS), Dermatology Quality of Life Index (DLQI), laboratory index, recurrence rates (>2 weeks after treatment), and adverse events.
Figure 1.
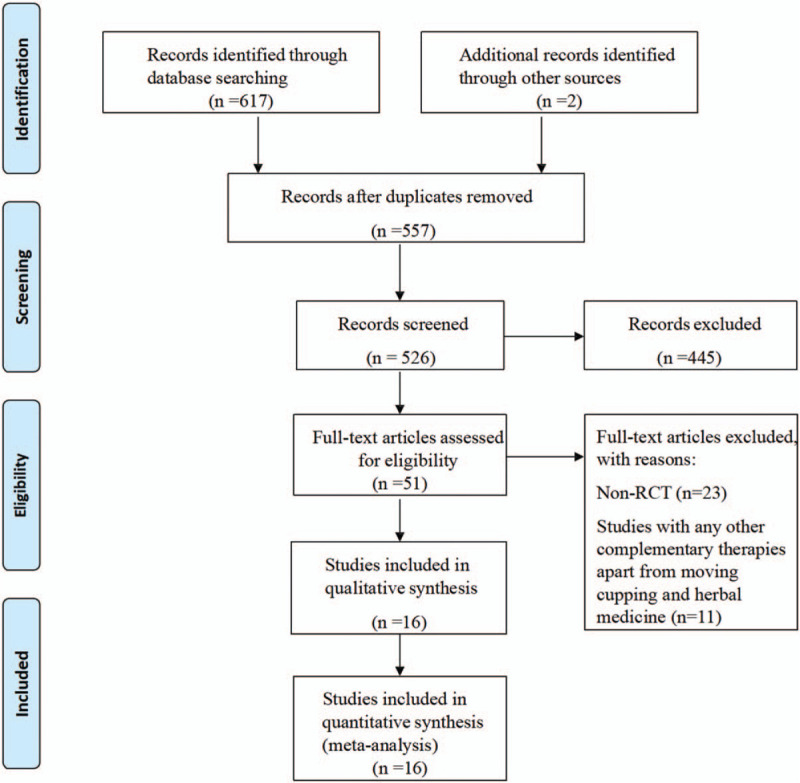
Literature identification and selection process. RCT = randomized controlled trial.
As performed in our previous work, 2 authors (MX and XD) were responsible for the screening of the titles and abstracts of the retrieved references. In the next step, the full texts of the included references were assessed based on the eligibility criteria. One author (MX) extracted the data from the included trials and assessed the risk of bias of the included RCTs using the Cochrane collaboration tool, while the other (XD) verified the extracted data and evaluated the risk of bias. Discrepancies were resolved by consulting a third author (XL).
The risk of bias for each study was evaluated in accordance with the Cochrane Handbook for Systematic Reviews of Intervention.[17] The following 6 criteria were applied: selection bias (random sequence generation and allocation concealment), performance bias (blinding of participants and personnel), detection bias (blinding of outcome assessment), attrition bias (incomplete outcome data), reporting bias (selective reporting), and any other bias. Three potential bias judgments were identified: low risk, high risk, and unclear risk. A study was classified as having an unclear risk when insufficient details regarding the methods and outcome were reported, the risk of bias was unknown, a metric was not relevant to the study (particularly for assessing blinding and incomplete outcome data), or the outcome assessed by the metric had not been measured in the study.
Dichotomous data were expressed as risk ratios (RR) with a 95% confidence interval (CI). Continuous data were expressed as mean differences with 95% CIs. Statistical heterogeneity was tested for the 16 trials. RevMan 5.3 software (Cochrane Collaboration) was used for data analyses. Meta-analyses were performed if the trials had acceptable homogeneity (I2 < 85%) concerning the study design, participants, interventions, controls, and outcome measures. Fixed-effect models (I2 < 25%) were used for homogeneous studies and random-effects methods were employed prior to the fixed-effect models in studies with substantial heterogeneity (25% < I2 < 85%).[18]
3. Results
3.1. Characteristics of included studies
After the primary searches of the 6 databases, 617 citations were identified. We excluded 557 studies because they did not meet the inclusion criteria. Full-text articles of 51 studies were retrieved. Finally, 16 studies with a total of 1164 participants were included in this systematic review and meta-analysis (Fig. 1). Characteristics of the included trials are listed in Table 1 . Among the included trials, 3 studies[19–21] were unpublished master's theses.
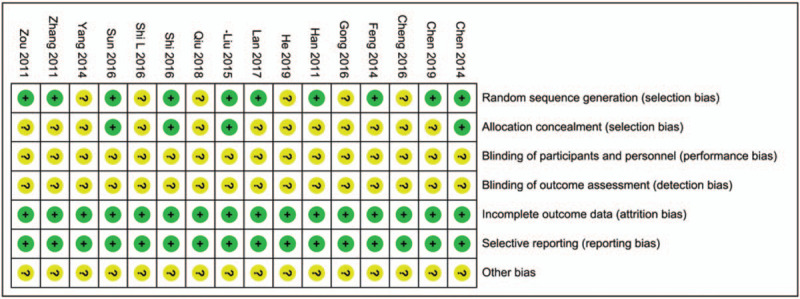
Table 1.
Characteristics of the 13 included trials.
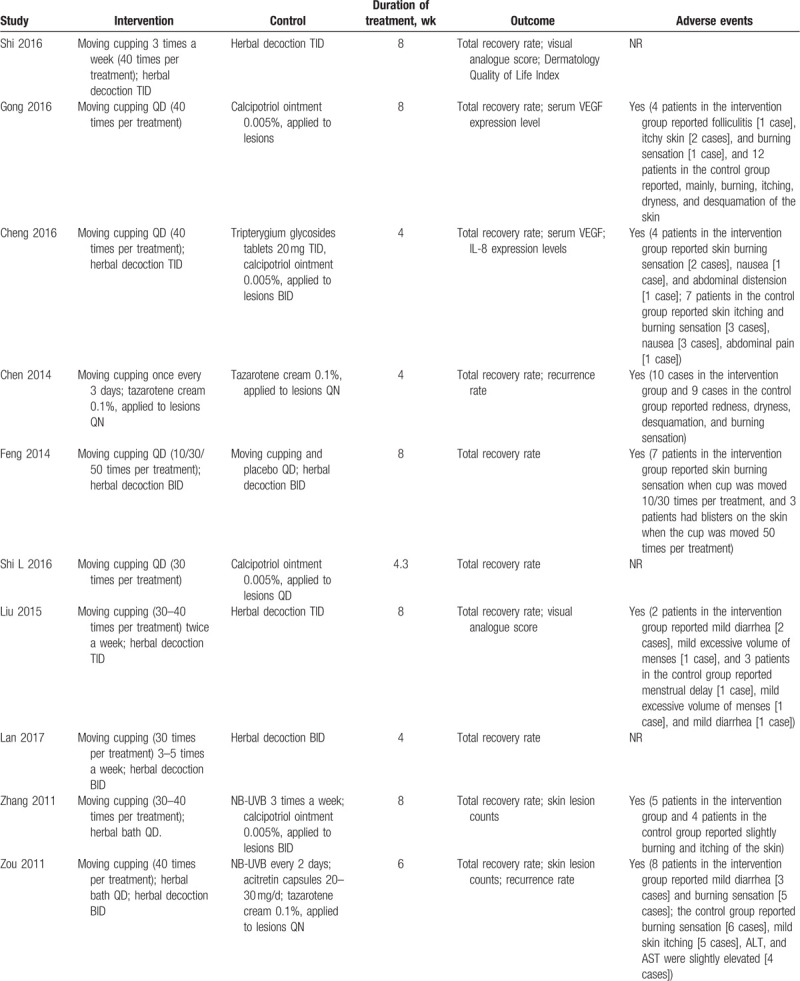
Table 1 (Continued).
Characteristics of the 13 included trials.
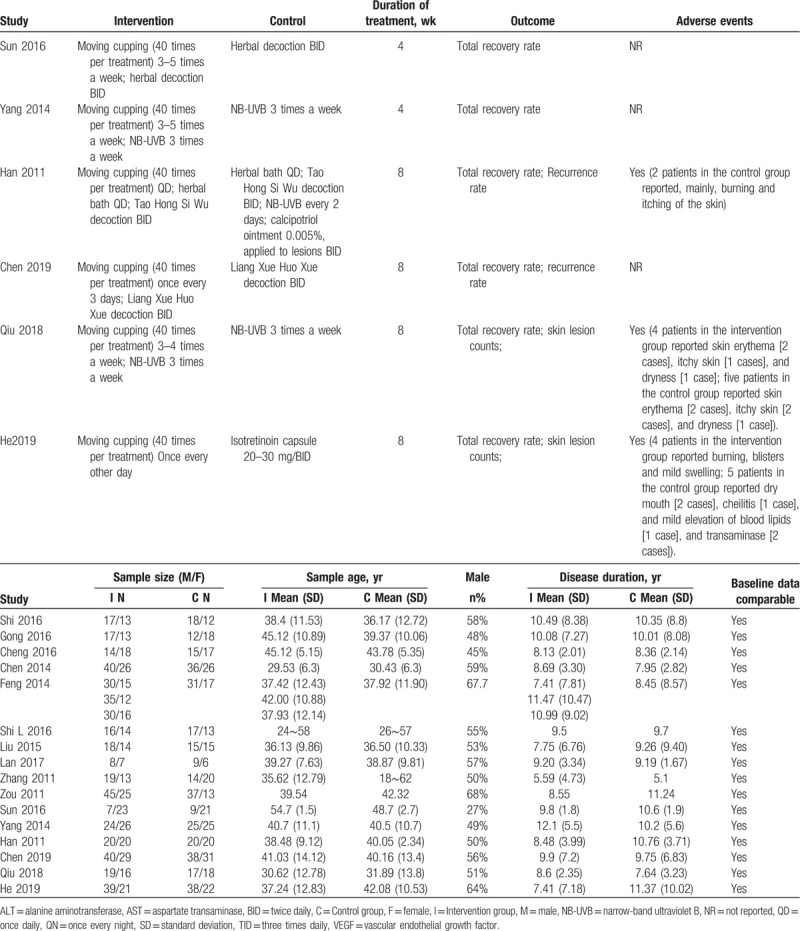
The risk of bias is shown in Fig. 2. The methodological quality of all included studies was not very satisfactory. Although all the analyzed trials reported randomization, only 9 adequately described the randomization method: 7 with a random number table[19,21–24] and 2 using a computerized method.[20,27] Moreover, only 2 studies reported allocation concealment,[19,25] and none of the included studies reported implementation of a blinded outcome assessment. All the trials adequately addressed incomplete outcome data and selective reporting. We found no other biases in these trials; however, considering their unsatisfactory methodological quality, we determined that all the included trials had an unclear risk of bias.
Figure 2.
Risk of bias graph.
3.2. Meta-analysis outcomes
3.2.1. Primary outcomes
3.2.1.1. Psoriasis area and severity index
Thirteen included RCTs[19–21,23–25,27–30,32] reported on the primary end point (Fig. 3). These studies used moving cupping therapy in intervention groups. The results showed a better therapeutic effect in the intervention group with moving cupping (weighted mean difference = –1.22, 95% CI [–1.58, –0.85], P < .00001 random model; I2 = 85%).
Figure 3.
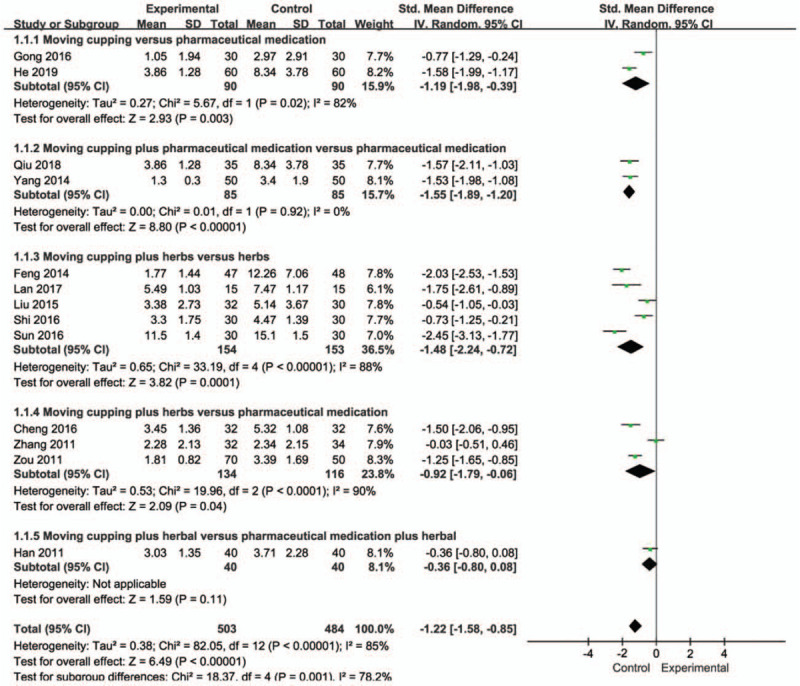
Meta-analysis of psoriasis area and severity index. CI = confidence interval; df = degree of freedom; IV = independent variable; SD = standard deviation.
We performed a subgroups analysis based on the difference in treatment methods. We found that whether comparing moving cupping with pharmaceutical medication, or moving cupping and combined pharmaceutical medication with pharmaceutical medication alone, moving cupping intervention was associated with a significantly better PASI score (P < .003). In addition, moving cupping combined with herbs had a better therapeutic effect than herbs alone (weighted mean difference = –1.48, 95% CI [–2.24, –0.72], P < .00001 random model; I2 = 88%). Moving cupping combined with herbs also was superior to pharmaceutical medications in treating plaque psoriasis (weighted mean difference = –0.92, 95% CI [–1.79, –0.06], P < .0001 random model; I2 = 90%). However, the efficacy of moving cupping combined with herbs was not statistically different from that of pharmaceutical medication combined with herbal medicines (P = .11).
In view of the high heterogeneity in this review, we conducted a sensitivity analysis (Fig. 4); in the subgroup analysis of acupuncture combined with traditional Chinese medicine compared with traditional Chinese medicine alone, eliminating the 2 studies solved the heterogeneity problem (weighted mean difference = –2.10, 95% CI [–2.46, –1.74], P < .0001 random model; I2 = 0%). In these 2 studies, the frequency of use of cans was ≤2 times per week, whereas in the other 3 studies, the frequency of treatment was used 3 to 4 times a week. Therefore, the difference in treatment frequency may be the reason for higher heterogeneity. In the subgroup analysis of acupuncture combined with traditional Chinese medicine compared with Western medicine, the heterogeneity decreased significantly after one study was excluded (weighted mean difference = –1.33, 95% CI [–1.66, –1.01], P < .00001 random model; I2 = 0%). Our analysis showed that the study did not use herbs decoction in the intervention group that was used in the other studies, which may explain the heterogeneity.
Figure 4.
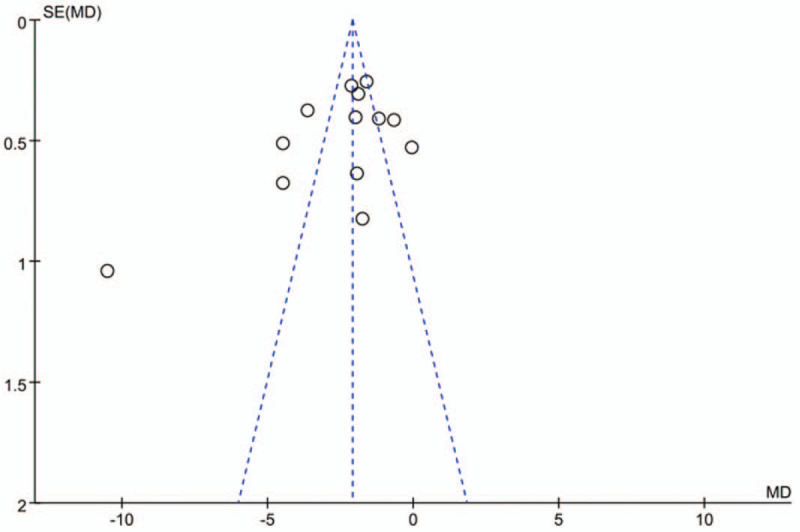
Funnel plot. MD = mean difference; SE = standard error.
3.2.1.2. Efficacy of psoriasis area and severity index >60%
Fifteen included RCTs[19–28,30–34] reported a 60% reduction in the PASI score after treatment. The results also showed a better efficacy in the moving cupping-treated group than in the control group without moving cupping (RR = 1.43, 95% CI [1.31, 1.57], P < .00001 fixed model; I2 = 22%) (Fig. 5).
Figure 5.
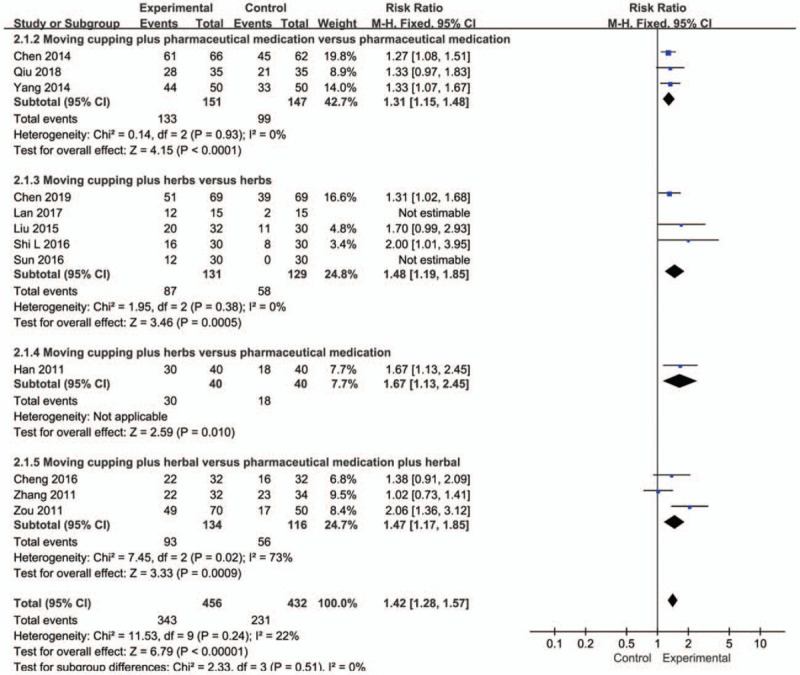
Meta-analysis of psoriasis area and severity index > 60%. CI = confidence interval; df = degree of freedom; M-H = Mantel-Haenszel.
A subgroup analysis also was performed based on different treatment methods. The results suggested that moving cupping combined with either pharmaceutical medications or herbs is more effective than pharmaceutical medications (RR = 1.31, 95% CI [1.15, 1.48], P < .0001 fixed model; I2 = 0%) or herbs (RR = 1.48, 95% CI [1.19, 1.85], P = .0005 fixed model; I2 = 0%) alone. The therapeutic effect of moving cupping combined with herbs was significantly better than that of pharmaceutical medication combined with herbs (RR = 1.47, 95% CI [1.17, 1.85], P = .0009 fixed model; I2 = 73%). In addition, other studies have shown that the efficacy of moving cupping combined with herbal is better than that of pharmaceutical medication alone (P = .01).
3.2.2. Secondary outcomes
3.2.2.1. Visual analogue score
VAS is a patient's subjective assessment method for measuring itching from 0 (no itching) to 100 (maximum itching) at each visit. Three studies[19,20,24] analyzed the VAS. The results showed no difference in VAS between moving cupping combined with herbs and herbal medicines or pharmaceutical medications (weighted mean difference = –0.27, 95% CI [–0.71, 0.17], P = .22 random model; I2 = 64%) (Fig. 6).
Figure 6.
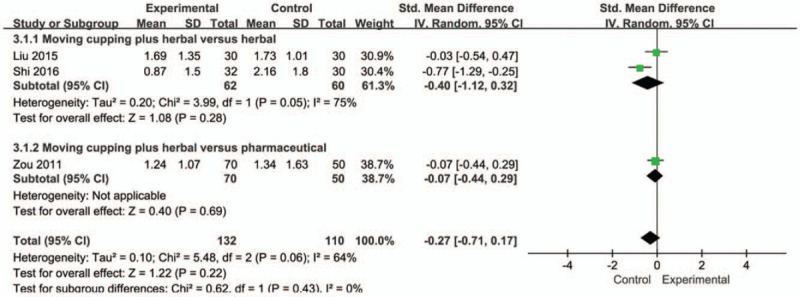
Meta-analysis of visual analogue score. CI = confidence interval; df = degree of freedom; IV = independent variable; SD = standard deviation.
3.2.2.2. Dermatology Quality of Life Index
One[20] study showed that moving cupping combined with herbs was significantly better than herbal medicines alone in terms of DQLI of patients with plaque psoriasis (P < .05).
3.2.2.3. Psoriasis-associated cytokine levels
Two[32,34] studies assessed the levels of cytokines associated with plaque psoriasis. One[34] study showed that serum vascular endothelial growth factor (VEGF) levels were significantly lower in patients treated with moving cupping than in those who had topical calcipotriol therapy. The other study[31] compared moving cupping combined with herbs and pharmaceutical medications and reported that moving cupping reduced serum tumor necrosis factor (TNF-α) and VEGF levels more significantly than pharmaceutical medications.
3.2.2.4. Recurrence rate
Four studies[21,22,24,26] analyzed the recurrence rates and showed that the moving cupping group had a significant improvement (RR = 0.33, 95% CI [0.16, 0.68], P = .003; I2 = 28%), suggesting that moving cupping treatment of plaque psoriasis has long-term effects (Fig. 7).
Figure 7.
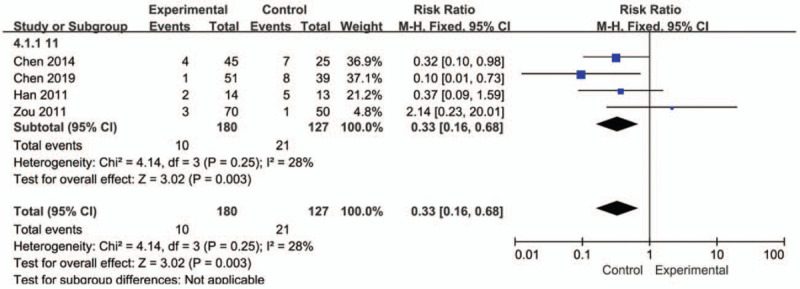
Meta-analysis of recurrence rate. CI = confidence interval; M-H = Mantel-Haenszel.
3.2.2.5. Adverse events
Ten studies[20,21,24,27–29,31,34] in total demonstrated that moving cupping therapy had a good safety and tolerability profile. The most common adverse reaction to moving cupping is redness, itching, and burning of local skin. However, in one study,[29] blisters appeared because of excessively frequent moving cupping therapy but healed quickly after treatment. Two studies reported adverse reactions for Chinese herbs[20,32]; the main symptoms were gastric discomfort and diarrhea. One study[24] reported the following side effects of a combination of tazarotene, narrow-band ultraviolet B (NB-UVB), and acitretin capsules: dryness, desquamation, and mild local skin irritation. The main adverse reactions observed with calcipotriol[34] were mild irritation and itching of the skin. In addition, another study reported a slight increase in dry mouth, cheilitis, blood lipids, and transaminase caused by isotretinoin.[31]
4. Discussion
This systematic review evaluated the efficacy and safety of moving cupping therapy in the treatment of plaque psoriasis. Although the quality of the studies reviewed was not satisfactory, the results showed that moving cupping therapy is superior to pharmaceutical medications such as calcipotriol or isotretinoin in the treatment of psoriasis, and combined with other therapies can significantly improve the clinical symptoms of plaque psoriasis. At the same time, it has obvious advantages in relieving the recurrence rate, in particular when cost-effectiveness and drug saving strategies such as drug dose-tapering, are considered.[35] Moreover, moving cupping therapy could significantly reduce TNF-α and VEGF levels compared with calcipotriol. However, this therapy has no greater advantage in reducing the VAS and DLQI. In addition, moving cupping therapy is not considered to be associated with adverse reactions. The only adverse effects of the treatment are redness, itching, and burning of local skin, which disappear quickly and thus are not considered to be severe. Therefore, moving cupping therapy is a viable clinical treatment option for plaque psoriasis.
In Chinese public hospitals, moving cupping therapy has become extremely popular as an effective method for treating plaque psoriasis, and it has been included in the 2017 Chinese expert consensus on special treatment of psoriasis vulgaris.[36] Moving cupping therapy has strong adsorption force, and the operator could quickly move the cup to the skin lesion, thereby promoting blood flow, improving the circulation of qi, eliminating pathogenic factors, detoxifying the body, and ultimately resulting in a therapeutic effect. Moreover, psoriasis involves inflammation and disorder of lipid metabolism. Cupping therapy can upregulate anti-inflammatory lipids, downregulate the function of pro-inflammatory lipids, improve the balance of lipid metabolites, and alleviate the inflammatory response.[37]
Although this study demonstrated that moving cupping therapy is a suitable treatment option for plaque psoriasis, a few limitations to this systematic review exist, such as the inclusion of unpublished master's theses, the small sample size of the trials, and the unclear risk of bias. Moreover, a few studies did not mention the methods of randomization, and the lack of allocation concealment and blinding in most of the studies could lead to potential performance bias and detection bias. Emollients play an important role in the basic treatment of psoriasis. As a matrix, the use of moving cupping treatment is also different. More importantly, the included studies lack a meticulous design, and the quality of the methodology of the studies included in this review was generally unsatisfactory, indicating a possible high risk of bias.
The clinical efficacy of moving cupping therapy is worthy of recognition; however, high quality and large-scale research that systematically confirms its effectiveness is lacking. To improve the quality of future studies, researchers need to regulate the intensity of moving cupping, the frequency of moving cupping, and the course of treatment, while also considering whether the difference in the type of substrate applied to the body during moving cupping will also affect the corresponding therapeutic effect. Randomization methods need to be described clearly and reported fully. Moreover, blinding of the outcome assessors should be attempted, to minimize performance and assessment biases; analyses of outcomes based on the intention-to-treat principle and accurate sample-size calculation are vital. Furthermore, future systematic reviews and meta-analyses should adhere to the PRISMA guidelines to ensure clarity and completeness of reporting.
5. Conclusions
In summary, moving cupping therapy combined with herbs or pharmaceutical medications could be an important part of combination therapy for the treatment of plaque psoriasis. However, this is not conclusive because of the unsatisfactory methodological quality of the available relevant RCTs. Therefore, more high-quality RCTs, with low risk of bias and adequate sample sizes, are required to demonstrate the effectiveness of moving cupping therapy.
Author contributions
Meng Xing, Xiaojie Ding, Jinjing Zhang, Le Kuai, YL, Yi Ru, Xiaoying Sun, Tian Ma, Xiao Miao, Liu Liu, Yanjiao Wang, Bin Li, and Xin Li had full access to all the study data and take full responsibility for the integrity and accuracy of the analysis. Meng Xing, Xiaojie Ding, Jinjing Zhang, and Le Kuai were responsible for the study concept and design. Meng Xing and Yi Ru were responsible for data acquisition, and Xiaoying Sun and Tian Ma were responsible for data extraction. The assessment of bias risk was performed by Xiao Miao and Liu Liu, Yanjiao Wang, and Xin Li completed the data analysis and interpretation. Xin Li and Meng Xing drafted the manuscript, and Xiaojie Ding and Yi Ru provided critical review of the manuscript for important intellectual content. Xin Li performed the statistical analyses and Bin Li supervised the study. Everyone mentioned above has provided permission to be named.
Glossary
Abbreviations: CI = confidence interval, DLQI = Dermatology Quality of Life Index, NB-UVB = narrow-band ultraviolet B, PASI = psoriasis area and severity index, PRISMA = preferred reporting items for systematic reviews and meta-analyses, RCT = randomized controlled trials, RR = risk ratios, TNF-α = tumor necrosis factor-α, VAS = visual analogue score, VEGF = vascular endothelial growth factor.
References
- [1].Nevitt GJ, Hutchinson PE. Psoriasis in the community: prevalence, severity and patients’ beliefs and attitudes towards the disease. Br J Dermatol 1996;135:533–7. [PubMed] [Google Scholar]
- [2].Schöffski O, Augustin M, Prinz J, et al. Costs and quality of life in patients with moderate to severe plaque-type psoriasis in Germany: a multi-center study. J Dtsch Dermatol Ges 2007;5:209–18. [DOI] [PubMed] [Google Scholar]
- [3].Gisondi P, Tessari G, Conti A, et al. Prevalence of metabolic syndrome in patients with psoriasis: a hospital-based case-control study. Br J Dermatol 2007;157:68–73. [DOI] [PubMed] [Google Scholar]
- [4].Gelfand JM, Troxel AB, Lewis JD, et al. The risk of mortality in patients with psoriasis: results from a population-based study. Arch Dermatol 2007;143:1493–9. [DOI] [PubMed] [Google Scholar]
- [5].Xin Li, Lingjun Kong, Fulun Li, et al. Association between psoriasis and chronic obstructive pulmonary disease: a systematic review and meta-analysis. PLoS ONE 2015;10:e0145221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Xin Li, Qing-Qing Xiao, Fu-Lun Li, et al. Immune signatures in patients with psoriasis vulgaris of blood-heat syndrome: a systematic review and meta-analysis. Evid Based Complement Alternat Med 2016;2016:9503652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Nast A, Boehncke WH, Mrowietz U, et al. German S3-guidelines on the treatment of psoriasis vulgaris (short version). Arch Dermatol Res 2012;304:87–113. [DOI] [PubMed] [Google Scholar]
- [8].Menter A, Gelfand JM, Connor C, et al. Joint American Academy of Dermatology-National Psoriasis Foundation guidelines of care for the management of psoriasis with systemic nonbiologic therapies. J Am Acad Dermatol 2020;82:1445–86. [DOI] [PubMed] [Google Scholar]
- [9].Kogan N, Raimondo N, Gusis SE, et al. Latin American Clinical Practice Guidelines on the Systemic Treatment of Psoriasis SOLAPSO - Sociedad Latinoamericana de Psoriasis (Latin American Psoriasis Society). Int J Dermatol 2019;58: (suppl): 4–28. [DOI] [PubMed] [Google Scholar]
- [10].Gisondi P, Altomare G, Ayala F, et al. Italian guidelines on the systemic treatments of moderate-to-severe plaque psoriasis. J Eur Acad Dermatol Venereol 2017;31:774–90. [DOI] [PubMed] [Google Scholar]
- [11].Zaghloul SS, Goodfield MJ. Objective assessment of compliance with psoriasis treatment. Arch Dermatol 2004;140:408–14. [DOI] [PubMed] [Google Scholar]
- [12].Beach MC, Sugarman J, Johnson RL, et al. Do patients treated with dignity report higher satisfaction, adherence, and receipt of preventive care? Ann Fam Med 2016;3:331–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Reza S, Mojgan M, Seyed S, et al. Comparison of Th1/Th2 and Treg/Th17 ratios between wet and dry cupping therapies in Persian medicine. Avicenna J Phytomed 2020;10:24–34. [PMC free article] [PubMed] [Google Scholar]
- [14].Zhang Q, Wang X, Yan G, et al. Anti-versus pro-inflammatory metabololipidome upon cupping treatment. Cell Physiol Biochem 2018;45:1377–89. [DOI] [PubMed] [Google Scholar]
- [15].Wang Q, Shang Y, Dong S, et al. Clinical research evidence of cupping therapy in China: a systematic literature review. BMC Complement Altern Med 2010;10:1–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Cao H, Li X, Liu J. An updated review of the efficacy of cupping therapy. PLoS One 2012;7:e31793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Higgins, JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 (updated March 2011). Cochrane Collaboration website. Available from: training. cochrane.org/handbook. Accessed February 15, 2012. [Google Scholar]
- [18].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;21:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Anhui University of TCM, Shi LL. Clinical Observation of Compound Ze Qi Granule Combined With Moving Cupping Therapy in the Treatment of Plaque Psoriasis. 2016. [Google Scholar]
- [20].Chengdu University of TCM, Liu YB. Clinical Study on Traditional Chinese Medicine Combined With Cupping Therapy for Psoriasis Vulgaris With Blood Stasis Type. 2015. [Google Scholar]
- [21].Xinjiang Medical University, Han HJ. Clinical Observation of Moving Cupping Therapy in the Treatment of Plaque Psoriasis. 2013. [Google Scholar]
- [22].Chen LN, Chen HC. Efficacy of Tazarotene Cream combined with moving cupping in the treatment of plaque psoriasis. J Dermatol Venereal Dis 2014;21:395–7. [Google Scholar]
- [23].Lan HR, Wu YB, Lian WY. Treatment of 15 cases of plaque psoriasis vulgaris (blood stasis syndrome) with Chinese medicine oil moving cupping and oral Chinese Medicine. J Jiangxi Univ TCM 2017;29:24–7. [Google Scholar]
- [24].Zou L, Liu HX, Yao SP. Clinical study of traditional Chinese medicine in the treatment of plaque psoriasis. Guangming Trad Chin Med 2011;26:926–9. [Google Scholar]
- [25].Sun SY, Zai X, Li LL. Clinical study on treatment of plaque psoriasis with herbal extract of Radix Shikonin. Mod Chin Med Clin J 2016;23:29–32. [Google Scholar]
- [26].Chen SL, Liu JF, Shan W. Therapeutic effect of Liangxue Huoxue decoction combined with canning therapy on plaque psoriasis. Chin J Clin Pharm Therap 2019;24:86–91. [Google Scholar]
- [27].He B, Lin ZF. Clinical study on 60 cases of blood stasis syndrome of psoriasis vulgaris treated by walking cans. New J Trad Chin Med 2019;51:236–8. [Google Scholar]
- [28].Qiu GR, Wu YB, Lan HG, et al. Treatment of 35 cases of plaque psoriasis vulgaris with traditional Chinese medicine medicinal oil and NB-UVB irradiation. J Jiangxi Univ Trad Chin Med 2018;4:26–9. [Google Scholar]
- [29].Feng L, Guo F, Ji Y. Clinical study on the treatment of plaque psoriasis with blood stasis syndrome based on moving cupping therapy. China J Trad Chin Med Pharm 2014;29:3343–5. [Google Scholar]
- [30].Anhui University of Traditional Chinese Medicine, Shi LL. Therapeutic Effect of Compound Lacquer Granules Combined With Canning Therapy On Plaque Psoriasis. 2016. [Google Scholar]
- [31].Zhang CH, Li B, Feng W, et al. Clinical observation of traditional Chinese medicine treatment for plaque psoriasis vulgaris. China J Trad Chin Med Pharm 2011;26:2470–2. [Google Scholar]
- [32].Cheng L, Cheng H, Qian Y. Effects of Qingyin Jiedu Decoction combined with canning therapy on VEGF and TNF-α in patients with psoriasis vulgaris. Mod J Integr Trad Chin Western Med 2016;25:3060–2. [Google Scholar]
- [33].Yang XX, Liu XL, Yan Li, et al. Clinical observation of BC-UVB in the treatment of plaque psoriasis. Guangxi J Trad Chin Med 2014;37:53–4. [Google Scholar]
- [34].Gong LP, Huang G, Zhu Q, et al. Treatment of 30 cases of plaque psoriasis with golden cream combined with canning therapy. J Jiangxi Coll Trad Chin Med 2016;28:38–9. [Google Scholar]
- [35].Hansel K, Bianchi L, Lanza F, et al. Adalimumab dose tapering in psoriasis: predictive factors for maintenance of complete clearance. Acta Derm Venereol 2017;97:346–50. [DOI] [PubMed] [Google Scholar]
- [36].Chinese Academy of integrated traditional Chinese and Western medicine dermatology Venerology Specialized Committee special therapeutics group. Expert consensus on TCM treatment of psoriasis vulgaris (2017 year). Chin J Integr Trad Chinese Western Med Dermatol Venerol 2017;2017:547–50. [Google Scholar]
- [37].Zhang Q, Wang X, Yan G, et al. Anti- versus pro-inflammatory metabololipidome upon cupping treatment. Cell Physiol Biochem 2018;45:1377–89. [DOI] [PubMed] [Google Scholar]


