The brutalisation of Jacob Blake and murders of George Floyd, Breonna Taylor, Ahmaud Arbery, Tony McDade, and countless others—coupled with horrifying statistics about the disproportionate burden of COVID-19 on Black and Brown communities—have forced the USA and the world to reckon with how structural racism conditions survival. Although clinicians often imagine themselves as beneficent caregivers, it is increasingly clear that medicine is not a stand-alone institution immune to racial inequities, but rather is an institution of structural racism. A pervasive example of this participation is race-based medicine, the system by which research characterising race as an essential, biological variable, translates into clinical practice, leading to inequitable care. In this Viewpoint, we discuss examples of race-based medicine, how it is learned, and how it perpetuates health-care disparities. We introduce race-conscious medicine as an alternative approach that emphasises racism, rather than race, as a key determinant of illness and health, encouraging providers to focus only on the most relevant data to mitigate health inequities.
Research in clinical medicine and epidemiology requires explicit hypotheses; however, hypotheses involving race are frequently implicit and circular, relying on conventional wisdom that Black and Brown people are genetically distinct from White people.1 This common knowledge descends from European colonialisation, at which time race was developed as a tool to divide and control populations worldwide. Race is thus a social and power construct, with meanings that have shifted over time to suit political goals, including to assert biological inferiority of dark-skinned populations.2 In fact, race is a poor proxy for human variation. Physical characteristics used to identify racial groups vary with geography and do not correspond to underlying biological traits. Genetic research shows that humans cannot be divided into biologically distinct subcategories.3, 4 Furthermore, ongoing overlap and mixture between populations erodes any meaningful genetic difference.5 Despite the absence of meaningful correspondence between race and genetics, race is repeatedly used as a shortcut in clinical medicine. For instance, Black patients are presumed to have greater muscle mass than patients of other races and estimates of their renal function are accordingly adjusted.6 On the basis of the understanding that Asian patients have higher visceral body fat than do people of other races, they are considered to be at risk for diabetes at lower body-mass indices.7 Angiotensin-converting enzyme (ACE) inhibitors are considered less effective in Black patients than in White patients, and they might not be prescribed to Black patients with hypertension (table ).1, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28 We argue that such approaches are harmful and unnecessary, contributing to health-care disparities among the exact populations they are intended to help.
Table.
Examples of race-based medicine, the potential harm to patients, and race-conscious alternatives
| How race is used | Rationale for race-based management | Potential harm | Race-conscious approach | |
|---|---|---|---|---|
| eGFR6 | eGFR for Black patients is multiplied by 1·16–1·21 the eGFR for White patients, depending on the equation used | Black patients are presumed to have higher muscle mass and creatinine generation rate than patients of other races | Black patients might experience delayed dialysis and transplant referral8, 9 | Use eGFR equations that do not adjust for race (eg, CKD-EPI Cystatin C).10 |
| BMI risk for diabetes7 | Asian patients considered at risk for diabetes at BMI ≥23 vs 25 for patients of other races | Asian patients are presumed to develop more visceral than peripheral adiposity than patients of other races at similar BMI levels, increasing risk for insulin resistance7 | Asian patients screened for diabetes despite absence of other risk factors might experience increased stigma and distrust of medical providers11 | Screen patients with lower BMIs on the basis of indications of increased body fat (eg, body roundness,12 body fat percentage), not based on race |
| FRAX13 | Probability of fracture is adjusted according to geography or minority status, or both | Different geographical and ethnic minority populations are presumed to have varied relative risks for fracture on the basis of epidemiological data | Some populations, including Black women, might be less likely to be screened for osteoporosis than other populations14 | Screen patients for osteoporosis on the basis of clinical risk criteria, rather than race; counteract existing biases that place Black patients at risk because of racial essentialist beliefs about variation in bone density15 |
| PFT16 | Reference values for pulmonary function are adjusted for race and ethnicity | Racial and ethnic minority groups are presumed to have varied lung function on the basis of epidemiological data | Black patients might experience increased difficulty obtaining disability support for pulmonary disease17 | Use unadjusted measures of lung function for all patients; counteract existing biases that harm Black patients because of racial essentialist beliefs about variation in lung capacity18 |
| JNC 8 Hypertension Guidelines19 | Treatment algorithm provides alternate pathways for Black and non-Black patients | ACE-inhibitor use associated with higher risk of stroke and poorer control of blood pressure in Black patients than in patients of other races | Black patients might be less likely to achieve hypertension control and require multiple antihypertensive agents20 | Consider all antihypertensive options for blood pressure control in Black patients; adjust as needed to achieve goals and manage adverse effects |
| Paediatric UTI diagnosis21 | White race in girls and non-Black race in boys are considered independent risk factors for UTI | Study of febrile children in the emergency department found highest prevalence of UTI among White girls and non-Black boys22 | Experimental data suggests that these guidelines could affect management of UTI by race23 | Treat UTI in children on the basis of clinical presentation, regardless of race |
| ASCVD risk estimation | Race-specific equations included to estimate ASCVD risk | ASCVD events higher for Black patients than patients of other races with otherwise equivalent risk burden24 | Black patients might experience more adverse effects from recommended statin therapy, including persistent muscle damage25 | Recommend preventive therapy on the basis of clinical metrics and comorbidities; consider pathways by which structural racism might increase cardiovascular risk among Black patients and promote resources to reduce racial stress and trauma26 |
| Eltrombopag dosing | East Asian patients receive half the starting dose compared with non-east Asian patients | Limited pharmacokinetic studies suggest reduced metabolism of eltrombopag in patients of East Asian descent27 | Some East Asian patients might receive inappropriate dosing28 | Initiate same starting dose for all patients, regardless of race, and adjust as needed on the basis of platelet response |
Examples of race-based medicine were chosen to represent multiple racial groups (eg, White, Black, Asian) and domains in which race is essentialised as biological (eg, pharmacokinetics, bone density, lung capacity). ACE=angiotensin-converting enzyme. ASCVD=atherosclerotic cardiovascular disease. BMI=body-mass index. CKD-EPI=Chronic Kidney Disease Epidemiologic Collaboration equation. eGFR=estimated glomerular filtration rate. FRAX=fracture risk assessment score. JNC 8=Eighth Joint National Committee. PFT=pulmonary function test. UTI=urinary tract infection.
Emerging scholarship underscores the harms of these race-adjusted practices,29, 30 even as some continue to defend them, touting their ability to capture yet-understood differences in clinical measures between racial groups.31, 32 However, propagation of race-based medicine promotes racial stereotyping, diminishes the need for research identifying more precise biomarkers underpinning disparities, and condones false notions about the biological inferiority of Black and Brown people. Hence, even if significant findings or clinical anecdotes support the use of racially tailored practices, they should be rigorously critiqued and mediating variables, such as structural conditions, should be analysed accordingly.
Many medical students enter their training with racial biases that are unconsciously reinforced. Race is often learned as an independent risk factor for disease, rather than as a mediator of structural inequalities resulting from racist policies. Health disparities are presented without context, leading students to develop harmful stereotypes on the basis of the belief that some populations are more diseased than others. Students learn to associate race with disease conditions, such as sarcoidosis, cystic fibrosis, hypertension, and focal segmental glomerulonephritis, which upholds their implicit understandings of race as a biological trait.33, 34 Professors might misleadingly equate genetic ancestry, which could be meaningful when traced to a narrowly circumscribed population of origin (eg, Biafada people), with race (eg, African ancestry).35, 36 On the wards, students learn that race is relevant to treatment decisions and have inadequate power to question the racialised assumptions of their supervisors.37, 38, 39, 40 In this way, race-based medicine is quickly propagated.
Such racially tailored care might drive medical errors and increase health inequities. For instance, medical students who endorsed the false beliefs that Black patients had longer nerve endings and thicker skin than White patients also rated Black patients as feeling less pain and offered less accurate treatment recommendations in mock medical cases.41 This racialised belief in diminished pain sensitivity of Black patients translates to consistently inadequate pain management and their reduced likelihood of receiving opioid prescriptions for severe pain.42, 43 Furthermore, race-adjusted instruments might also affect disease management. The assessment of renal function in Black patients is based on a higher estimated glomerular filtration rate (eGFR), which might mask kidney failure, delaying dialysis and listing for transplant.9, 10 Race corrections for pulmonary lung function tests also reduce the likelihood that Black patients can obtain disability support for their lung disease.18 These examples show the necessity of transitioning from a race-based system of clinical care to race-conscious practice. Adopting the language of race-conscious policy, we accordingly provide the following recommendations for race-conscious medicine.
First, racist, racially tailored practices that propagate inequity should be avoided. Race should not be used to make inferences about physiological function in clinical practice. Race-adjusted tools should be abandoned or replaced with more precise analytics than currently used. For instance, the health systems of the University of Washington, the University of California San Francisco, the Beth Israel Deaconess, and the Vanderbilt University eliminated the race-correction for eGFR. Clinical teams should reconsider the use of race in the opening sentence of an encounter note and instead consider including relevant indicators of structural vulnerability (eg, Spanish-speaking woman aged 41 years instead of Black woman aged 41 years). Race should be used to assess for experiences of discrimination and refer to affinity-based support services. Second, it should be taught that racial health disparities are a consequence of structural racism. Beginning in preclinical education, racial disparities in disease should be explained within the framework of the structural determinants of health, defining race as a social and power construct. Awareness of institutional inequities as a root cause of ongoing racial injustice promotes structural competency in clinical practice.44 In addition, phenotypic race should be distinguished from genetic ancestry and students should be discouraged from narrowing differential diagnoses and management on the basis of perceived race. Third, resolutions denouncing race-based medicine across clinical leadership should be adopted. Effective action to eradicate race-based medicine will require cooperation across clinical leadership, including those professional societies responsible for setting practitioner standards. Societies for health-care practitioners should consider resolutions denouncing the use of race-based medicine in their trainings, guidelines, and other publications, and require that race be explicitly characterised as a social and power construct when describing disease risk factors. Black, Indigenous, and other people of colour should be included in (and rewarded for their contributions to) decision making processes to reform disease management guidelines.45 Some forward-thinking societies have already made strides to advance such resolutions. Finally, clinical research should be used to examine structural barriers, rather than using race as a proxy for biology. Clinical journals should include in their publication guidelines instructions to avoid the use of race as a proxy for biological variables, such as genetics, pharmacokinetics, and metabolism. Hypotheses using racial labels should make the authors' definition and operationalisation of race explicit. Additionally, structural barriers to health that overlap with race should be considered, including socioeconomic status, discrimination, transportation, environmental exposures, criminal history, documentation status, English proficiency, and neighbourhood violence. Models and measures of structural racism that account for policy influences can be developed and used to assess health impacts, rather than solely including race as an independent variable.46, 47, 48
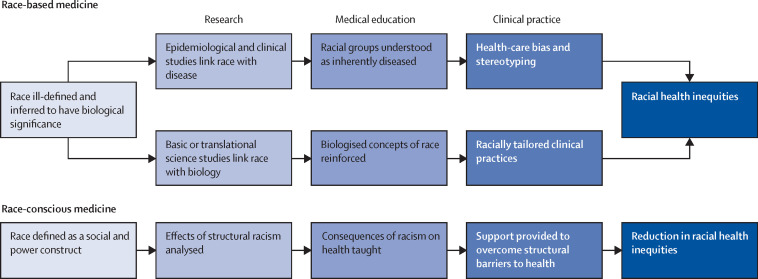
Our multi-pronged, race-conscious approach seeks to reform race-based medicine across clinical practice, education, leadership, and research (figure ). These recommendations aim to promote conscious, anti-racist practices over unchecked assumptions that uphold racial hierarchies.49 In doing so, medicine can make substantial strides toward achieving health equity.
Figure.
How race-based medicine leads to racial health inequities
An alternative approach to race-conscious medicine; defined as medical practice and pedagogy that accounts for how structural racism determines illness and health.
Health care is merely one institution plagued by structural racism: a comprehensive antidote to racial health disparities will require collaboration across sectors of housing, education, transportation, criminal justice, and environmental justice. We should encourage health-care practitioners to leverage their cultural capital to advocate for antiracist policies. Through conscious effort and collaboration, health-care providers can work towards racial equity within and beyond the walls of examination rooms.
Acknowledgments
Acknowledgments
JPC and MVP are supported by the Robert Wood Johnson Health Policy Research Scholars Program. JPC is supported by the National Institutes of Health Medical Scientist Training Program Grant T32GM13665.
Contributors
JPC and MVP conceived the idea of this Viewpoint and prepared the original manuscript draft. JT contributed to manuscript revision. JPC prepared the final version of the manuscript with input from MVP and JT.
Declaration of interests
We declare no competing interests.
References
- 1.Kaufman JS, Cooper RS. In search of the hypothesis. Public Health Rep. 1995;110:662–666. [PMC free article] [PubMed] [Google Scholar]
- 2.Roberts D. The New Press; New York and London: 2011. Fatal invention: how science, politics, and big business re-create race in the twenty-first century. [Google Scholar]
- 3.The American Society of Human Genetics ASHG denounces attempts to link genetics and racial supremacy. Am J Hum Genet. 2018;103:636. doi: 10.1016/j.ajhg.2018.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mersha TB, Abebe T. Self-reported race/ethnicity in the age of genomic research: its potential impact on understanding health disparities. Hum Genomics. 2015;9:1. doi: 10.1186/s40246-014-0023-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Association of Physical Anthropologists AAPA statement on race & racism. March 27, 2019. https://physanth.org/about/position-statements/aapa-statement-race-and-racism-2019/
- 6.National Kidney Foundation Frequently asked questions about GFR estimates. 2014. https://www.kidney.org/sites/default/files/docs/12–10–4004_abe_faqs_aboutgfrrev1b_singleb.pdf
- 7.Hsu WC, Araneta MRG, Kanaya AM, Chiang JL, Fujimoto W. BMI cut points to identify at-risk Asian Americans for Type 2 Diabetes screening. Diabetes Care. 2015;38:150–158. doi: 10.2337/dc14-2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Streja E, Nicholas SB, Norris KC. Controversies in timing of dialysis initiation and the role of race and demographics. Semin Dial. 2013;26:658–666. doi: 10.1111/sdi.12130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28:1504–1510. doi: 10.1007/s11606-013-2441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grubbs V. CJASN; 2020. Precision in GFR reporting: let's stop playing the race card. published online May 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee H, Woo BKP. Perceptions of and attitudes toward diabetes among Chinese Americans. J Am Osteopath Assoc. 2018;118:e33–e40. doi: 10.7556/jaoa.2018.087. [DOI] [PubMed] [Google Scholar]
- 12.Thomas DM, Bredlau C, Bosy-Westphal A. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity. 2013;21:2264–2271. doi: 10.1002/oby.20408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centre for Metabolic Bone Diseases FRAX fracture risk assessment tool. Welcome to FRAX. 2020. https://www.sheffield.ac.uk/FRAX/index.aspx
- 14.Silverman SL, Calderon AD. The utility and limitations of FRAX: a US perspective. Curr Osteoporos Rep. 2010;8:192–197. doi: 10.1007/s11914-010-0032-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fausto-Sterling A. The bare bones of race. Soc Stud Sci. 2008;38:657–694. doi: 10.1177/0306312708091925. [DOI] [PubMed] [Google Scholar]
- 16.Scanlon PD, Shriver MD. ‘Race correction’ in pulmonary-function testing. New Engl J Med. 2010;363:385–386. doi: 10.1056/NEJMe1005902. [DOI] [PubMed] [Google Scholar]
- 17.Braun L, Wolfgang M, Dickersin K. Defining race/ethnicity and explaining difference in research studies on lung function. Eur Respir J. 2013;41:1362–1370. doi: 10.1183/09031936.00091612. [DOI] [PubMed] [Google Scholar]
- 18.Braun L. Race, ethnicity and lung function: a brief history. Can J Respir Ther. 2015;51:99–101. [PMC free article] [PubMed] [Google Scholar]
- 19.James PA, Oparil S, Carter BL. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 20.Donato A, Brown K. In Black Africans with hypertension, amlodipine-based therapy vs perindopril–hydrochlorothiazide improved BP control. Ann Intern Med. 2019;171:JC5. doi: 10.7326/ACPJ201907160-005. [DOI] [PubMed] [Google Scholar]
- 21.Roberts KB. Revised AAP guideline on UTI in febrile infants and young children. Am Fam Physician. 2012;86:940–946. [PubMed] [Google Scholar]
- 22.Shaw KN, Gorelick M, McGowan KL, Yakscoe NM, Schwartz JS. Prevalence of urinary tract infection in febrile young children in the Emergency Department. Pediatrics. 1998;102:e16. doi: 10.1542/peds.102.2.e16. [DOI] [PubMed] [Google Scholar]
- 23.Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Med Care. 2008;46:678–685. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- 24.Bennett G, Coady S, Levy D, O'Donnell C, Shero S, Sorlie P. National Heart, Lung, and Blood Institute; 2014. 2013 Report on the assessment of cardiovascular risk: full work group report supplement. [Google Scholar]
- 25.Golomb BA, Evans MA. Statin adverse effects. Am J Cardiovasc Drugs. 2008;8:373–418. doi: 10.2165/0129784-200808060-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Williams DR, Priest N, Anderson NB. Understanding associations among race, socioeconomic status, and health: patterns and prospects. Health Psychol. 2016;35:407–411. doi: 10.1037/hea0000242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wong RS, Bussel JB, Saleh MN. Efficacy of eltrombopag in adult east Asian and non-east Asian patients with chronic immune thrombocytopenia (cITP): results from the Extend study. Blood. 2016;128 [Google Scholar]
- 28.Rajman I, Hirano M, Honma W, Zhao S. New paradigm for expediting drug development in Asia. Drug Disc Today. 2020;25:491–496. doi: 10.1016/j.drudis.2019.12.013. [DOI] [PubMed] [Google Scholar]
- 29.Vyas DA, Eisenstein LG, Jones DS. Hidden in plain sight—reconsidering the use of race correction in clinical algorithms. New Engl J Med. 2020 doi: 10.1056/NEJMms2004740. published online June 17. [DOI] [PubMed] [Google Scholar]
- 30.Eneanya ND, Yang W, Reese PP. Reconsidering the consequences of using race to estimate kidney function. JAMA. 2019;322:113–114. doi: 10.1001/jama.2019.5774. [DOI] [PubMed] [Google Scholar]
- 31.Levey AS, Titan SM, Powe NR, Coresh J, Inker LA. Kidney disease, race, and GFR estimation. CJASN. 2020 doi: 10.2215/CJN.12791019. published online May 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Powe NR. Black kidney function matters: use or misuse of race? JAMA. 2020 doi: 10.1001/jama.2020.13378. published online July 29. [DOI] [PubMed] [Google Scholar]
- 33.Tsai J, Ucik L, Baldwin N, Hasslinger C, George P. Race matters? Examining and rethinking race portrayal in preclinical medical education. Acad Med. 2016;91:916–920. doi: 10.1097/ACM.0000000000001232. [DOI] [PubMed] [Google Scholar]
- 34.Braun L, Saunders B. Avoiding racial essentialism in medical science curricula. AMA J Ethics. 2017;19:518–527. doi: 10.1001/journalofethics.2017.19.6.peer1-1706. [DOI] [PubMed] [Google Scholar]
- 35.Yudell M, Roberts D, DeSalle R, Tishkoff S. Taking race out of human genetics. Science. 2016;351:564–565. doi: 10.1126/science.aac4951. [DOI] [PubMed] [Google Scholar]
- 36.Bolnick D. Individual ancestry inference and the reification of race as a biological phenomenon. In: Koenig BA, Lee SS-J, Richardson SS, editors. Revisiting race in a genomic age. Rutgers University Press; New Brunswick, New Jersey, and London: 2008. pp. 70–85. [Google Scholar]
- 37.Snipes SA, Sellers SL, Tafawa AO, Cooper LA, Fields JC, Bonham VL. Is race medically relevant? A qualitative study of physicians' attitudes about the role of race in treatment decision-making. BMC Health Serv Res. 2011;11:183. doi: 10.1186/1472-6963-11-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lempp H, Seale C. The hidden curriculum in undergraduate medical education: qualitative study of medical students' perceptions of teaching. BMJ. 2004;329:770–773. doi: 10.1136/bmj.329.7469.770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garcia RS. The misuse of race in medical diagnosis. Pediatrics. 2004;113:1394–1395. doi: 10.1542/peds.113.5.1394. [DOI] [PubMed] [Google Scholar]
- 40.Tsai J, Brooks K, DeAndrade S. Addressing racial bias in wards. Adv Med Educ Pract. 2018;9:691–696. doi: 10.2147/AMEP.S159076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between Blacks and Whites. Proc Natl Acad Sci USA. 2016;113:4296–4301. doi: 10.1073/pnas.1516047113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anderson KO, Green CR, Payne R. Racial and ethnic disparities in pain: causes and consequences of unequal care. J Pain. 2009;10:1187–1204. doi: 10.1016/j.jpain.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 43.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299:70–78. doi: 10.1001/jama.2007.64. [DOI] [PubMed] [Google Scholar]
- 44.Metzl JM, Hansen H. Structural competency: theorizing a new medical engagement with stigma and inequality. Soc Sci Med. 2014;103:126–133. doi: 10.1016/j.socscimed.2013.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Obasi AI. Equity in excellence or just another tax on Black skin? Lancet. 2020 doi: 10.1016/S0140-6736(20)31536-1. published online July 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sewell AA. The racism–race reification process: a mesolevel political economic framework for understanding racial health disparities. Sociol Race Ethn. 2016 doi: 10.1177/2332649215626936. published online Feb 8. [DOI] [Google Scholar]
- 47.Lukachko A, Hatzenbuehler ML, Keyes KM. Structural racism and myocardial infarction in the United States. Soc Sci Med. 2014;103:42–50. doi: 10.1016/j.socscimed.2013.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chae DH, Clouston S, Hatzenbuehler ML. Association between an internet-based measure of area racism and Black mortality. PLoS One. 2015;10 doi: 10.1371/journal.pone.0122963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Crear-Perry J, Maybank A, Keeys M, Mitchell N, Godbolt D. Moving towards anti-racist praxis in medicine. Lancet. 2020;396:451–453. doi: 10.1016/S0140-6736(20)31543-9. [DOI] [PMC free article] [PubMed] [Google Scholar]