Abstract
Objective:
Parents often report guilt about what they feed their child, but no studies have examined how this guilt might affect their child-feeding or own eating behavior. Some studies suggest that guilt motivates healthy behaviors, yet others show that guilt impairs the self-control needed to abstain from unhealthy behaviors.
Method:
One hundred and ninety parents reported how guilty they feel about their current child-feeding habits. Parents then chose food for their child in a virtual reality (VR) buffet and reported their intentions to improve child-feeding and own eating behavior in the future. Finally, parents were offered candy while they completed an unrelated survey.
Results:
Parents with greater guilt reported stronger intentions to improve both feeding (b=.27, p=.010) and eating (b=.21, p=.019) in the future. However, among parents with higher (but not lower) BMI, those who reported greater guilt served more unhealthy foods for their child in the buffet (b=.32, p=.010) and were more likely to eat candy at the end of the study (b=.92, p=.004). Further analyses revealed that guilt only predicted greater feeding intentions when parents had served relatively more unhealthy foods in the buffet (b=.43, p<.001).
Conclusions:
Findings echo the mixed conceptualization of guilt shown in previous literature on health behavior. More research is necessary to understand the long-term influence of guilt on eating and feeding behavior and the circumstances under which guilt is associated with detrimental versus healthy behavior.
Keywords: guilt, obesity, child-feeding, eating, virtual reality
Introduction
Projections suggest that 57.3% of today’s children in the United States will have obesity by age 35 (Ward et al., 2017). Obesity is associated with a host of negative consequences, including lower quality of life; increased risk for non-communicable diseases such as Type 2 Diabetes, cancer, and cardiovascular disease; and early mortality (Centers for Disease Control, 2017). One important predictor of obesity is eating behavior during childhood (Sahoo et al., 2015), for which parents play a significant role (Savage, Fisher, & Birch, 2007).
U.S. culture facilitates unhealthy diets (Rosenkranz & Dzewaltowski, 2008) and simultaneously stigmatizes obesity (Ambwani, Thomas, Hopwood, Moss, & Grilo, 2014). As such, it is unsurprising that parents often express guilt about their feeding practices (Pescud & Pettigrew, 2014; Pocock, Trivedi, Wills, Bunn, & Magnusson, 2010). Parental guilt is ubiquitous and considered inherent to parenting (Sutherland, 2010; Liss, Schiffrin, & Rizzo, 2013), yet scant research has explored how this guilt might be related to parents’ eating or child feeding behavior.
Guilt is the experience of negative affect following a personal failure or transgression (Tangney, Stuewig, & Mashek, 2007). Research suggests that guilt serves an adaptive function by motivating reparative action (Tangney et al., 2007). Indeed, several studies have found that “guilt-proneness,” an individual tendency to experience guilt in response to transgressions, is associated with increased efforts to correct such transgressions (Sheikh & Janoff-Bulman, 2010). Similarly, one meta-analysis shows that individuals who feel guilty about their unhealthy behavior report greater intentions to improve their behavior in the future (Xu & Guo, 2018). Cognitive Dissonance Theory would suggest that guilt is especially motivating when past transgressions are salient (Fointiat, Morisot, & Pakuszewski, 2008). Indeed, when the salience of hypocrisy is experimentally induced, participants are more likely to change their behavior or report stronger intentions to change in the future (McKimmie et al., 2003).
Still, within literature on health behavior, guilt has also been linked to impaired self-control. Several studies demonstrate that greater feelings of guilt actually lead to an inability to withstand temptation (Hofmann & Fisher, 2012; Muraven, Collins, Shiffman, & Paty, 2005; Kuijer, Boyce, & Marshall, 2015, Kuijer & Boyce, 2014). For instance, Muraven et al. (2005) found that greater guilt about an episode of drinking too much alcohol led to increased subsequent alcohol consumption and greater intoxication. The link between guilt and impaired self-control may be due to maladaptive emotion regulation (DeSteno, Gross, & Kubzansky, 2013). Although guilt can inspire intentions to improve, intentions do not always translate into behavior because behavior change is often quite difficult (Sheeran & Webb, 2016). If individuals do not have the resources to engage in the healthy behavior change that might attenuate guilt, they may instead seek gratification to soothe their negative, guilty feelings. Counterintuitively, this gratification often occurs in the form of increases in the guilt-inducing behavior (or other unhealthy behaviors), because these behaviors are hedonically pleasing (DeSteno et al., 2013; Salovey, Rothman, Detweiler, Steward, & Wayne, 2000).
In this case, guilt need not be derived from a failure to perform health behaviors in order to facilitate emotion regulation through hedonically pleasing, unhealthy behaviors (Ferrer, Klein, Lerner, Reyna, & Kelter, 2016). That is, individuals experiencing guilt completely unrelated to health behavior may also find comfort in these hedonic behaviors (DeSteno et al., 2013; Ferrer, Green, & Barrett, 2015). This is consistent with literature showing that incidental emotions, i.e., emotions that are not relevant to the behavioral decision at hand, can influence unrelated behaviors (Ferrer et al., 2016).
There is an abundance of literature on guilt and eating behavior, yet most studies examine guilt as an outcome, rather than a predictor, of eating (e.g., Macht & Dettmer, 2006; Steenhuis, 2009). The limited literature examining the effect of guilt on eating reflects the contradictory theories of guilt, linking this emotion to both healthy and unhealthy eating behavior. In one study, greater anticipated guilt about failing to eat fruit was associated with greater intentions to eat fruit in the future (Onwezen, Bartels, & Antonides, 2014). Conradt et al. (2008) found that current feelings of guilt also motivated healthier eating. In this longitudinal study of individuals with obesity, weight-related guilt at baseline predicted problem-focused engagement strategies and greater dietary restraint six months later (Conradt et al., 2008).
Other studies support the link between guilt and impaired self-control, showing that when guilt is more salient, it is associated with less healthful eating. Kuijer et al. (2015) found that those who associate chocolate cake with guilt (versus celebration) reported poorer eating habits and lower levels of perceived behavioral control over eating during times of stress. Similarly, Kuijer & Boyce (2014) found that those who associated chocolate cake with guilt were less successful at maintaining or losing weight 18 months later. Relatedly, ecological momentary assessment data showed that a current experience of guilt about a self-control failure (including but not limited to unhealthy eating) led to worse self-control at the next similar temptation. However, this guilt also indirectly led to better self-control via greater perceived goal importance (Hofmann & Fisher, 2012). These paradoxical findings illuminate the complex nature of guilt in relation to health behavior.
In the clinical literature, guilt is consistently linked to disordered eating. In a large study of undergraduates, feelings of general guilt (i.e., guilt related to any issue) over the past week were related to more binge eating episodes and disordered eating (Davis-Becker, Peterson, & Fischer, 2014). Ecological momentary assessment data with participants with obesity also showed that general feelings of guilt increase in the four hours before a binge eating episode (Berg et al., 2015). Similarly, an abundance of literature supports the notion of “comfort food,” demonstrating that individuals eat palatable but unhealthy foods to quell negative emotions (Garg & Lerner, 2013; Dallman, 2010), such as guilt.
Despite the prevalence of guilt in parenting (Sutherland, 2010; Liss et al., 2013), little research has focused on how these feelings might be related to child feeding, or other parenting behaviors. One study found that parents who feel guiltier about a child’s wrongdoing make more of an effort to address and correct the behavior (Scarnier, Schmader, & Lickel, 2009), which may extend to feeding behavior. Bouhlal, Abrams, McBride, and Persky (2018) found that among women with overweight, those having greater body-related guilt reported more restriction of their child’s diet (i.e., restricting their child’s access to palatable but calorically dense foods). Restricted feeding is, counterintuitively, associated with childhood overweight (Faith, Scanlon, Birch, Francis, & Sherry, 2004; Faith & Kerns, 2005), suggesting that guilt about one’s own body might be counterproductive to promoting the health of one’s children.
The Bouhlal et al. (2018) findings also suggest that parent and child eating behavior are inextricably linked. Parents’ own eating behavior is highly predictive of how their children eat, as parents model eating behavior and make important decisions such as what foods to keep in the house (Savage et al., 2007; Mitchell, Farrow, Haycraft, & Meyer, 2013). Likewise, Best et al. (2016) found that, following family-based behavioral treatment for obesity, parent and child (ages 7–12) dyads had highly similar patterns of weight maintenance, which were explained by congruent dietary changes (Best et al., 2016). This correlation in eating behavior may be partially, but not entirely, due to parents’ feeding practices, as children ages 7–12 may have more autonomy over eating choices than younger children. Therefore, it is not clear whether a similar correspondence would occur between parents and younger children, whose eating behavior is more strongly determined by parental feeding. Further, although studies have examined these trends over time, no research has examined whether an isolated experience (such as an experience of guilt) will exert a similar influence on parents and children’s consumption.
Due to genetic and environmental factors, children who have parents with overweight or obesity have increased likelihood of developing obesity themselves (Birbilis, Moschonis, Mougios, & Manios, 2013). Accordingly, Persky, McBride, Faith, Wagner, and Ward (2015) found that parents with higher body mass index (BMI) experience greater guilt about the genetic risk they passed to their child. Importantly, this study did not find a relationship between BMI and “lifestyle guilt” (i.e., guilt about feeding and child’s physical activity; Persky et al., 2015). Given the dearth of research on how guilt about feeding or eating is associated with behavioral outcomes, no studies have examined whether the experience of guilt might be different for parents with higher BMI versus leaner parents. Leaner parents may find it easier to ignore or dismiss their feeding-related guilt, because their children have a lower risk for obesity (Birbilis et al., 2013). Further, guilt may be especially problematic for parents with higher BMIs because this population is more likely to eat in response to stress and negative affect (Ozier et al., 2008).
Overall, more research is necessary to understand how parents’ guilt about feeding is related to actual feeding and eating practices, and how factors such as BMI might moderate these relationships. The current study examines these cross-sectional associations among parents of children ages 3–7. After receiving an educational message about healthy feeding, parents reported their levels of guilt about feeding and about the genetic risk for disease they may have passed to their child. They then chose food for their child in a virtual reality (VR) buffet, and subsequently reported their intentions to improve feeding and eating in the future. Parents were then offered M&Ms while they responded to an unrelated questionnaire.
Hypotheses
The following hypotheses were tested:
Hypothesis 1. Greater guilt about feeding will be associated with healthier feeding behavior; specifically, a) more servings of healthy foods and b) fewer servings of unhealthy foods on the final plate in the VR buffet, especially among parents with higher BMI.
Hypothesis 2. Greater guilt about feeding will be associated with greater intentions to feed their child more fruits and vegetables in the future, especially among parents with higher BMI.
Hypothesis 3. Greater guilt about feeding will be associated with greater intentions to increase one’s own fruit and vegetable consumption in the future, especially among parents with higher BMI.
Hypothesis 4. Parents with greater guilt about feeding whose poor feeding behavior is salient (i.e., who feed their child more servings of unhealthy food and fewer servings of healthy food in the VR buffet) will have the highest intentions to increase their child’s fruit and vegetable consumption in the future.
Hypothesis 5. Greater guilt about feeding will be associated with a greater likelihood of eating M&Ms at the end of the study, especially among parents with higher BMI.
Method
Participants
Participants were 190 parents (126 mothers) from the Washington, DC area with a biological child between the ages of 4 and 7. Parents were recruited through several different methods, including online advertisements, flyers, and word of mouth. Participants were considered ineligible if another parent had already completed the study on behalf of the index child, if their child had any major allergies or dietary restrictions, or if their child did not live with them. Parents had a mean age of 37.71 (SD=5.73) and a mean BMI of 27.73 (SD=7.82). The sample was 46.30% White, 25.80% Black, 14.20% Asian, 9.50% Latinx, 3.20% biracial, and 0.50% American Indian. Participants had high socioeconomic status (SES); 27.90% held a college degree and an additional 51.60% held a graduate degree. Most parents were employed full time (67.4%). See Table 1 for study characteristics by participant weight status.
Table 1.
Study Characteristics by Participant Weight Status
| Lean (BMI<25) | Overweight/Obese (BMI≥25) | |
|---|---|---|
| Past Feeding | 2.36 (.89) | 2.22 (.69) |
| Past Perception of Feeding | 3.45 (1.02) | 3.26 (1.07) |
| Guilt about Feeding | 2.81 (1.68) | 3.25 (1.70) |
| Guilt about Genetic Risk* | 1.92 (1.16) | 2.97 (1.72) |
p<.05
Procedure
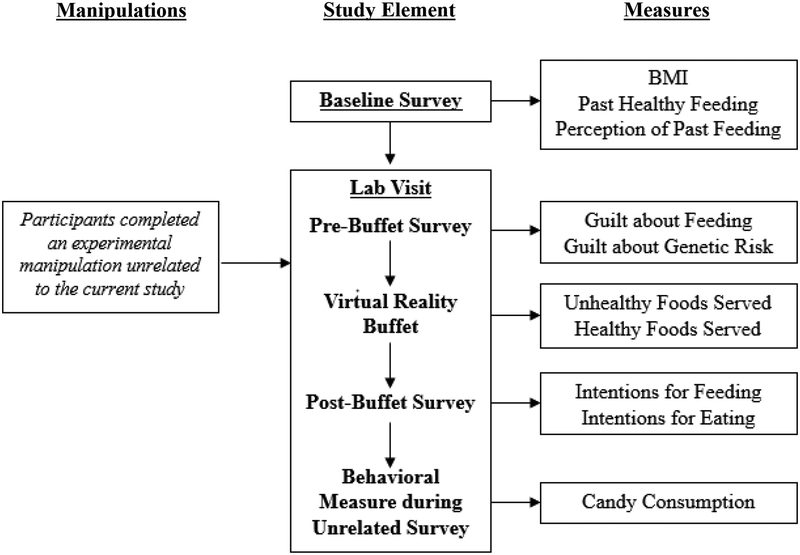
Data were collected in the course of a larger experimental study testing how an emotion manipulation paired with a health message manipulation affects parents’ feeding behavior (Persky et al., 2018a). The study was approved by the Institutional Review Board of the National Human Genome Research Institute. See Figure 1 for a timeline of study procedures. After providing informed consent, parents completed an online questionnaire of baseline measures and scheduled a time to visit the lab. Upon arrival, parents re-consented and completed a brief training and practice session for the VR buffet. The goal of the practice session was to acclimate participants to the technology and ensure that the regular session would run smoothly. In this training session, the only food option was pasta with tomato sauce, and parents were instructed to practice placing the pasta on their plate and finalizing their plate by “checking out” with the virtual cashier. Parents then completed the experimental manipulations to which they had been randomly assigned. Although the presentation of the message differed among experimental groups, all parents received information about the importance of feeding children fruits and vegetables. This paper will not focus on the effects of the manipulations, and therefore the experimental conditions are controlled for in all analyses. After the manipulations, parents completed a follow-up survey which included their current feelings of guilt. Importantly, self-reported guilt did not differ by experimental condition.
Figure 1.
Study Timeline
Next, participants were placed in the VR buffet, in which they were asked to create a lunch for their child. A VR buffet provides precise measures of the amount of food chosen and reduces the possibility of confounding variables by measuring behavior in an entirely controlled environment (Persky, Goldring, Turner, Cohen, & Kistler, 2018b). Previous research has demonstrated that feeding in a VR buffet is a valid proxy for real-life feeding behavior (Persky et al., 2018b) and is sensitive to interventions (McBride, Persky, Wagner, Faith, & Ward, 2013). Specifically, the amount of pasta, apple juice, and overall number of calories that parents serve in a VR buffet is highly correlated with the amounts they serve in real-life feeding situations. Parents also report that they would feed the virtual meal they created to their child in real life (Persky et al., 2018b). Foods chosen for inclusion in the VR buffet were palatable and frequently served to children, but represented a range of caloric and nutrient densities. For a detailed explanation of how foods were selected to be included in the VR buffet, see Persky et al., 2018b.
Parents received the following instructions, which were intended to increase the ecological validity of the experience and reduce experimental demand. The instructions were designed to discourage parents from simply choosing the healthiest foods and encourage them to include a range of foods to comprise a typical meal that their child might eat. Instructions were received in text form and through audio when they first entered the VR buffet:
When picking foods for your child’s plate, please create a whole meal during each session, just as you would in real life if you were at a buffet. This is a one-trip buffet with only one plate, so pick what you would choose if you only made one trip for the whole meal. Please select the type of meal you would choose if your child would not eat again afterward for several hours. You should select foods that you believe your child would eat. When you make your choices, please consider only the child that is a part of this study. You will be able to add as many or as few spoonfuls of each food as you would like. You may fill the plate completely, or you may leave parts empty. If you change your mind, you are allowed to put items back on the buffet. There is no time limit; take as much time as you need.
The food options in the buffet included: carrots, grapes, grilled chicken, chicken nuggets, oranges, fries, pizza bagels, sliders, apple sauce, corn, green beans, macaroni and cheese, black beans, yogurt, white rice, cookies, and brownies. Parents also chose among several drinks. After creating a plate for their child in the VR buffet, parents completed a follow-up survey that assessed their intentions to feed their child and to eat more fruits and vegetables in the future.
Finally, all participants viewed an unrelated, brief presentation about epigenetics (how the environment influences gene expression) and completed a questionnaire on the topic. Findings from this questionnaire are not presented in this paper; however, this time was used as an opportunity to measure parents’ own eating behavior. A researcher recorded how much candy the participant ate from an M&M dispenser on the desk where they completed the survey.
Measures
Independent Variables.
Body Mass Index (BMI)
During the baseline survey, participants were asked to report their current height and weight, which was used to calculate their BMI.
Guilt about Feeding
Two items (r=.79) assessed how guilty parents felt about their child’s current eating and physical activity habits: “I feel guilty about the amount of fruits and vegetables [child] eats on an average day” and “I feel guilty about [child’s] current eating and physical activity habits.” Response options were 1 (strongly disagree) to 7 (strongly agree).
Guilt about another Parenting Issue (Genetic Risk)
To determine whether parental guilt about another health threat for the child would affect feeding and eating behavior, two items assessed how guilty parents felt about the genetic risks that their child may have inherited from them: “I feel guilty about the genetic risk for disease that I may have passed down to [child]” and “I feel guilty about the genetic risk for overweight that I may have passed down to [child]” Response options ranged from 1 (strongly disagree) to 7 (strongly agree). Although the correlation between the two items was relatively low (r=.59), the pattern of results remained the same when each item was examined as an individual predictor.
Covariates.
Experimental Conditions
To control for any variance in the dependent variables that may be explained by the manipulation, the two experimental condition variables (emotion frame and message frame) are included as covariates in all analyses. The interactions of both experimental conditions with guilt were tested as predictors of all dependent variables. There was a significant interaction between experimental condition and guilt on the number of slow/whoa foods served in the VR buffet (p=.002). However, neither experimental condition moderated association of guilt with any other dependent variable.
Past Fruit and Vegetable Feeding
Past feeding behavior may confound the relationship between guilt and eating/feeding behavior and intentions (i.e., poor past feeding behavior may cause both greater guilt and greater intentions to improve in the future). As such, analyses controlled for reports of past feeding behavior using two separate items regarding fruit and vegetable feeding, respectively. Parents reported how many times the index child ate vegetables and fruits in the past week on a scale from 0 (child did not eat this food in the past 7 days) to 7 (3 or more times per day; Dwyer et al., 2017).
Perception of Past Feeding
To further control for past feeding behavior, a single item assessed parents’ perception of their child’s healthy eating habits: “Use the scale below to indicate how often you think your child eats the recommended amount of fruits and vegetables in a given day” on a scale from 1 (never) to 5 (always).
Outcome Variables
Feeding Behavior
To assess feeding behavior, the total number of healthy and unhealthy servings of food on the final plate that parents created in the VR buffet was measured. One serving was defined as a single “click” of the VR controller, which adds a single portion of the food to the plate. As in Persky et al. (2015), foods were defined according to the Coordinated Approach to Child Health guide, which categorizes foods as “go” (healthy), “slow” (less healthy), and “whoa” (unhealthy) options (U.S. Department of Health and Human Service, National Heart, Lung, and Blood Institute, 2013).
Slow/Whoa Foods
As in Persky et al. (2015), the number of servings of slow and whoa foods in the VR buffet were combined into a single variable. Slow/whoa foods were the sum of servings of chicken nuggets, pizza bagels, sliders, fries, brownies, cookies, macaroni and cheese, white rice, apple sauce, and strawberry yogurt.
Go Foods
Go foods were the sum of servings of healthy foods in the VR buffet, including grilled chicken, carrots, oranges, grapes, corn, green beans, and black beans.
Intentions for Feeding Fruits and Vegetables
Four items (α =.91) assessed parents’ intentions to feed their child more fruits and vegetables in the next six months (e.g., “I intend to increase the amount of vegetables [child] eats in the next six months”) on a scale from 1 (strongly disagree/very unlikely) to 7 (strongly agree/very likely).
Intentions for Eating Fruits and Vegetables
Four items (α =.93) assessed parents’ intentions to eat more fruits and vegetables in the next six months (e.g., “I intend to increase the amount of fruits and vegetables I eat in the next six months”). Response options ranged from 1 (strongly disagree/very unlikely) to 7 (strongly agree/very likely).
Candy Consumption
While parents completed the final, unrelated survey about epigenetics, the experimenter told them to help themselves to the M&Ms from a dispenser on the desk. The number of grams of M&Ms that participants ate from the dispenser was recorded. Because this variable was non-normally distributed (56.8% of parents did not eat any candy), candy consumption was dichotomized into a yes/no variable.
Statistical Analysis
Statistical analyses were conducted through SPSS Statistics Version 25. All analyses controlled for experimental condition, past fruit feeding, past vegetable feeding, perception of past feeding behavior, and parent gender. Multiple linear regressions were used to predict continuous variables and logistic regressions were used for categorical dependent variables. Continuous variables were centered; interactions were calculated using these centered variables. For any significant interactions, simple slopes analyses explored the association of each variable with the outcome at one standard deviation above and below the mean of the other variable.
Results
See Table 2 for correlations among study variables. Of note, the number of Go foods served in the VR buffet was negatively correlated with the number of Slow/Whoa foods served (r=−.27, p<.001). Candy consumption was positively correlated with the number of Slow/Whoa foods (r=.22, p=.002) but not associated with the number of Go foods (r=.02, p=.836).
Table 2.
Correlations between study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Guilt about Feeding | -- | |||||||
| 2. Guilt about Genetic Risk | .43** | -- | ||||||
| 3. BMI | −.03 | .31** | -- | |||||
| 4. Slow/Whoa Food Servings | .21** | .10 | .18* | -- | ||||
| 5. Go Food Servings | −.18* | −.05 | .10 | −.27** | -- | |||
| 6. Healthy Feeding Intentions | .33** | .16* | .19** | .05 | .01 | -- | ||
| 7. Healthy Eating Intentions | .25** | .21** | .24** | .05 | .04 | .75** | -- | |
| 8. Candy Consumption† | .13 | .15* | .22** | .22** | .02 | .34** | .35** | -- |
| Means | 3.04 | 2.49 | 27.70 | 2.69 | 4.20 | 5.14 | 5.11 | .43 |
| SD | 1.70 | 1.57 | 7.82 | 1.59 | 2.16 | 1.45 | 1.51 | .50 |
0=no, 1=yes,
<.01,
<.05
Associations of Guilt about Feeding
Guilt and Feeding Behavior.
Neither feeding guilt, BMI, nor the interaction of guilt and BMI was associated with Go food servings in the VR buffet (see Table 3). Thus, Hypothesis 1a was not supported.
Table 3.
Results from multiple linear regression models
| Variable | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | p-value | β | p-value | β | p-value | β | p-value | |||||
| Intercept | 6.689 | <.001 | 3.58 | <.001 | 11.65 | <.001 | 10.28 | <.001 | ||||
| Experimental Condition 1 | −.04 | −.51 | .612 | .05 | .70 | .484 | .09 | 1.32 | .188 | .05 | .66 | .512 |
| Experimental Condition 2 | .10 | 1.36 | .176 | .15 | 2.10 | .037 | .02 | .24 | .811 | .03 | .45 | .652 |
| Gender | −.05 | −.72 | .471 | −.08 | −1.08 | .281 | .10 | 1.45 | .148 | .17 | 2.50 | .013 |
| Past Fruit Feeding | −.01 | −.05 | .957 | .03 | .38 | .701 | −.20 | −2.31 | .022 | −.16 | −1.89 | .061 |
| Past Vegetable Feeding | −.06 | −.65 | .520 | −.01 | −.10 | .919 | −.05 | −.55 | .584 | −.16 | −1.77 | .079 |
| Perception of Past Feeding | −.13 | −1.32 | .189 | .17 | 1.75 | .08 | .04 | .45 | .656 | .14 | 1.47 | .143 |
| Parental BMI | .24 | 3.21 | .002 | .11 | 1.42 | .156 | .19 | 2.62 | .010 | .24 | 3.27 | .001 |
| Guilt | .14 | 1.54 | .125 | −.05 | −.56 | .577 | .27 | 3.15 | .002 | .21 | 2.37 | .019 |
| Parental BMI x Guilt | .17 | 2.23 | .027 | .00 | .05 | .963 | −.02 | −.31 | .757 | −.00 | −.05 | .959 |
Note: Final steps in regression analyses.
Parents with a higher BMI served more Slow/Whoa (less healthy/unhealthy) servings in the VR buffet. There was no main effect of feeding guilt, but more importantly, there was a significant interaction between guilt and BMI (see Table 3). Simple slopes analyses revealed that greater guilt was associated with more servings of Slow/Whoa food, but only among parents with higher BMI (+1 SD, b=.32, p=.010), not among those with lower BMI (−1 SD, b=−.04, p=.758). Thus, the results were significant in the opposite direction of Hypothesis 1b.1
Guilt and Feeding Intentions.
Parents with higher BMI, as well as those with greater feeding guilt, had greater intentions to increase the amount of fruit and vegetables they feed their child in the next six months. There was no interaction between BMI and guilt (see Table 3). Hypothesis 2 was therefore partially supported.
Guilt and Eating Intentions.
Parents with higher BMI, as well as those with greater feeding guilt, reported greater intentions to eat more fruits and vegetables themselves in the next six months. There was no interaction between BMI and guilt (See Table 3). Hypothesis 3 was thus partially supported.
Moderating Effect of Feeding Behavior
Slow/Whoa food servings in the VR buffet were not associated with future feeding intentions. However, greater feeding guilt was associated with greater healthy feeding intentions, and there was a significant interaction between guilt and Slow/Whoa servings chosen in the buffet (see Table 4). Simple slopes analyses revealed that greater feeding guilt was associated with greater healthy feeding intentions among parents who chose a large amount of Slow/Whoa food in the buffet (+ 1 SD, b=.43, p<.001), but not those who chose a small amount of Slow/Whoa foods (−1 SD, b=.15, p=.160). However, among parents with lower levels of guilt (−1 SD), those who chose more Slow/Whoa foods in the buffet had significantly lower intentions to increase their fruit and vegetable feeding (b=−.25, p=.022). Among those with higher levels of guilt (+1 SD), this relationship was not significant (b=.03, p=.706). The total number of Go food servings and its interaction with feeding guilt were not significantly related to healthy eating intentions. Thus, the number of unhealthy foods served in the VR buffet exacerbated the relationship between parental guilt and subsequent feeding intentions, but the number of healthy foods served did not moderate this relationship. Therefore, Hypothesis 4 was partially supported (See Table 4).
Table 4.
Results from multiple linear regression models.
| Variable | |||
|---|---|---|---|
| β | p-value | ||
| Intercept | 11.72 | <.001 | |
| Experimental Condition 1 | .10 | 1.45 | .150 |
| Experimental Condition 2 | −.01 | −.08 | .939 |
| Gender | .08 | 1.20 | .233 |
| Past Fruit Feeding | −.21 | −.19 | .024 |
| Past Vegetable Feeding | −.05 | −.51 | .609 |
| Perception of Past Feeding | .04 | .42 | .673 |
| Parental BMI | .20 | 2.91 | .004 |
| Guilt | .29 | 3.38 | .001 |
| Slow Servings | −.11 | −1.46 | .146 |
| Guilt x Slow Servings | .15 | 2.14 | .034 |
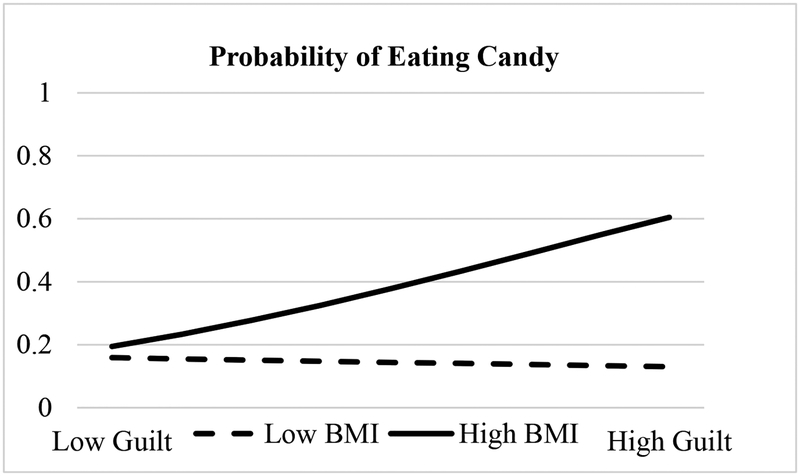
Guilt and Candy Consumption
Parents with a higher BMI were more likely to eat candy during a questionnaire at the end of the study, and there was not a main effect of feeding guilt with eating behavior. However, there was a significant interaction between feeding guilt and BMI (see Figure 2 and Table 5). Simple slopes analyses revealed that greater guilt was associated with a greater likelihood of eating candy, but only among parents with a higher BMI (+1 SD, b=.92, p=.004), not those with a lower BMI (−1 SD, b=−.12, p=.682). Hypothesis 5 was therefore supported.
Figure 2.
This figure displays the association of parents’ guilt about feeding with their likelihood of eating candy during the study among parents with higher (+1 SD) and lower (−1 SD) BMIs. BMI=body mass index
Table 5.
Results from logistic regression model predicting whether the parent ate candy
| Variable | Candy Consumption | ||
|---|---|---|---|
| β | OR [95% CI] | ||
| Constant | −.71 | .365 | |
| Experimental Condition 1 | .11 | .743 | 1.11 [0.58–2.13] |
| Experimental Condition 2 | .11 | .750 | 1.11 [0.58–2.14] |
| Gender | .40 | .258 | 1.50 [0.74–3.01] |
| Past Fruit Feeding | −.37 | .026 | 0.69 [0.50-.096] |
| Past Vegetable Feeding | −.10 | .559 | 0.91 [0.66–1.25] |
| Perception of Past Feeding | .44 | .041 | 1.56 [1.02–2.38] |
| Parental BMI | .64 | .002 | 1.90 [1.26–2.86] |
| Guilt | .40 | .061 | 1.49 [0.98–2.28] |
| Parental BMI x Guilt | .52 | .016 | 1.68 [1.10–2.57] |
Note: Final Step in logistic regression analysis.
Analyses Using Guilt about Genetic Risk
Participants reported lower guilt about genetic risk than they did guilt about feeding (M=2.49 vs. M=3.04, t=−4.34, p<.001). Guilt about genetic risk was also tested as to its association with all outcome variables all the reported analyses. However, there were no significant relationships between guilt about genetic risk nor its interaction with BMI and any of the outcome variables.
Discussion
The current study found that parental guilt about feeding was associated with less healthy behavior among parents with higher BMI, yet healthier intentions for parents overall. The association of guilt with both healthy and unhealthy behavior is consistent with previous literature showing that guilt has mixed consequences (Hofmann & Fisher, 2012; Tangney et al., 2007), suggesting that although guilt can be motivational, it can also impair self-control or trigger emotion regulatory processes in the form of hedonic eating (Ferrer et al., 2016). Alongside Hofmann and Fisher (2012), this is one of the first studies to demonstrate how guilt can be associated with both beneficial and detrimental outcomes, even within a single sample.
As hypothesized, guilt was associated with greater likelihood of eating candy, but only among parents with higher BMI. This result is consistent with previous studies demonstrating that guilt inhibits self-control (Hofmann & Fisher, 2012) and can elicit emotion regulation through hedonic behavior (DeSteno et al., 2013; Salovey et al., 2000). This finding echoes the literature demonstrating that individuals who have higher weights are more likely to eat in response to negative emotions and stress (Ozier et al., 2008), suggesting that parents with overweight who also feel guiltier may be especially prone to such hedonic behavior to cope with negative affect.
Contrary to hypotheses, among parents with higher BMI, guilt was associated with selecting more Slow/Whoa food servings in the VR buffet. This result contradicts previous findings that guilt motivates efforts to correct previous transgressions (Sheikh & Janoff-Bulman, 2010) and facilitates adaptive parenting responses (Scarnier et al., 2009). These results also bring into question the legitimacy of conceptualizing guilt as a purely adaptive emotion. Furthermore, the association of guilt with unhealthy feeding behavior is surprising because previous literature suggests that any deleterious effect of guilt should be due to impaired self-control (Hofmann & Fisher, 2012; Muraven et al., 2005) and emotion regulation (DeSteno et al., 2013; Ferrer et al., 2016). Impaired self-control and emotion regulation through hedonic behaviors are typically associated with an inability to resist impulses toward self-gratification (DeSteno et al., 2013; Ferrer et al., 2016), and therefore was not expected to affect food choices for another person.
However, perhaps unhealthy feeding is the more self-gratifying option, especially when parents know that feeding certain foods typically appeases their children. Resisting a child’s demands for unhealthy foods and coaxing him or her to eat healthier options can be a frustrating experience (Nepper & Chai, 2016). Moreover, unhealthy feeding may have pleasant consequences for parents’ moods. In qualitative interviews, parents explain that giving their child “treats” increases the affection they receive from the child (Pescud & Pettigrew, 2014). When experiencing guilt, parents may seek this affection to improve their currently negative mood (Adamo & Brett, 2014). Indeed, a recent study shows that work-family guilt is associated with more permissive parenting (Borelli, Nelson-Coffey, River, Birken, & Moss-Racusin, 2017), suggesting that parents may indulge their children to assuage parental guilt. Further, feeding children palatable foods may also regulate the more affective component of guilt by offering a vicarious experience of pleasure, similar to the pleasure experienced through viewing videos and pictures of food (Spence, Okajima, Cheok, Petit, & Michel, 2016).
Despite its associations with unhealthy behavior among parents with higher BMI, guilt about feeding was associated with greater intentions to feed children more fruits and vegetables in the future. Parents also had greater intentions to eat more fruits and vegetables themselves. These results echo previous studies that show how guilt motivates healthy cognitions (Xu & Guo, 2018; Onwezen et al., 2014) and that parent and child eating behavior are interdependent (Best et al., 2016).
Future studies should consider whether parents who feel more guilt follow through on these healthier intentions, particularly given the conflicting behavioral findings in (as well as the cross-sectional nature of) this study. Most of the research demonstrating the adaptive function of guilt has measured intentions or attitudes as the outcome (Xu & Guo, 2018). Unfortunately, the link between intentions and health behavior is sometimes weak (Sheeran & Webb, 2016), and only one study has demonstrated that guilt is associated with healthier eating behavior (Onwezen et al., 2014). Thus, parents who feel guilty may resolve to improve, sufficiently assuaging their dissonant feelings, but may not actually change behavior—due to the many barriers that prevent healthy feeding, including the need to regulate negative affect. This temporary discounting of a future goal in lieu of immediate gratification is related to delayed discounting (Weller, Cook, Avsar, & Cox, 2008). That is, parents experiencing greater guilt may immediately regulate their negative feelings though food while simultaneously planning to improve in the future.
The fact that guilt had no overall association with healthy feeding in the VR buffet—and was associated with more unhealthy feeding among parents with higher BMI—could imply that parents who feel guiltier do not follow through on their healthier intentions. However, parents created a plate in the VR buffet before setting their intentions to change in the future. Taking this VR feeding experience into account, guilt was only associated with greater intentions to improve feeding if the parent had served a large amount of Slow/Whoa foods in the buffet. Thus, perhaps parents who feel guiltier do not have greater intentions to improve until their poor feeding behavior is salient. If so, the unhealthy feeding in the VR buffet would not be evidence of failed intentions, but rather indicate the lack of intention in the first place.
The interaction between guilt and feeding behavior also revealed that, among parents with low levels of guilt, those who served a larger number of unhealthy servings had lower intentions to improve. This interaction points to a potential advantage of guilt, suggesting that individuals may be motivated to improve their behavior when unhealthy feeding behavior is salient, but only if they feel guilty about this behavior.
Only guilt about feeding, not guilt about genetic risk, was associated with feeding intentions and behavior. Thus, it appears that domain-specific guilt, rather than feelings of guilt about a different topic, are relevant to health behavior. These results are similar to de Hooge, Breugelmans, and Zeelenberg’s (2008) finding that shame motivates prosocial behavior, but only when the prosocial behavior is relevant to the source of their shame. However, this finding contradicts the idea that individuals eat unhealthily when experiencing guilt in order to regulate their negative affect (DeSteno et al., 2013; Ferrer et al., 2016), because this relationship should exist whenever guilt is experienced, regardless of its source. One possible explanation is that guilt about genetic risk was not a significant predictor of any outcome variable because parents simply experienced low levels of guilt about genetic risk. Indeed, because the experimental manipulations discussed feeding behavior specifically, child feeding was salient throughout the study, and genetics were never mentioned.
No conclusions about causality can be drawn from these data given that guilt was measured, not induced experimentally. Therefore, it is possible that some of these relationships are bidirectional or even reversed. This possibility is the strongest for the analyses examining slow/whoa food servings in the VR buffet, as the data set also did not include a measure of past unhealthy feeding to include as a covariate. However, all analyses controlled for past fruit and vegetable feeding, and it is likely that past healthy feeding captures some portion of the variance in past unhealthy feeding. Servings of slow/whoa foods and go foods in the VR buffet were negatively correlated in the current study, and healthy and unhealthy feeding and have been correlated in other research (Kroller & Warschburger, 2009). Parents were instructed to choose “only foods that [their] child would actually eat,” so it is possible that they avoided the healthier buffet options that they expected their child might refuse. However, in a survey after the VR buffet, only 18.5% of parents said that their child would eat the entire meal, suggesting that parents did not feel constrained to create a plate that their child would eat in its entirety.
Further, guilt was measured using only two items, given space limitations. Other work does suggest that single item measures can be as reliable and valid as longer, multi-item measures (e.g., Ferrer et al., 2018), but more comprehensive measures of parental guilt about feeding, child’s nutrition, and genetic risk may be useful for future studies—especially in light of the finding that domain-specific guilt is important. Further, although the use of the word “guilt” in the current measure increases its face validity, responses to this measure may also reflect the experience of shame, as participants may be unable to differentiate between these two emotions (Tangney et al., 2007). However, whereas some studies have distinguished guilt as adaptive and shame as maladaptive (Tangney et al., 2007), recent research cautions against this sharp distinction and suggests that the effects of these two emotions are more similar than previously believed (Leach & Cidam, 2015; Leach, 2017). Future research may consider whether guilt and shame uniquely affect parents’ eating and feeding behavior.
There were other limitations posed by variable measurement. Intentions for feeding were not measured before the VR buffet, which would have helped assess whether parents follow through on their healthy intentions. This would also have allowed us to determine any change in intentions due to parents’ performance in the buffet. Unfortunately, stating one’s intentions could have unduly influenced buffet behavior as well as later intentions, so it is not clear that pre-measures of intentions would have been prudent. Additionally, parents’ past eating behavior was not assessed at baseline and therefore none of the analyses controlled for this variable. Lastly, the study did not examine parents’ healthy eating; therefore, it is unclear how guilt might be associated with immediate healthy eating as opposed to unhealthy eating (i.e., candy consumption).
All findings should be considered in light of the broader context of environmental factors that influence eating and feeding behavior (Rosenkranz & Dzewaltoswki, 2008), such as socioeconomic status (SES) and cultural norms. Although the current sample was fairly racially and ethnically diverse, parents had high SES. These findings may not be generalizable to lower SES communities, who may have less access to healthy foods (Rosenkranz & Dzewaltoswki, 2008). Because children in low SES communities are more likely to experience weight-related problems (Barriuso et al., 2015), it is especially important to understand whether parents experience such guilt in the context of more pressing health and financial burdens, and if so, how such guilt is associated with feeding behavior. Further, the VR buffet content in this study may be culture-specific.
Despite these limitations, the current study sheds light on how the ubiquitous experience of parental guilt may be associated with the family’s diet. Although guilt about feeding habits was associated with intentions to engage in healthier feeding and eating behaviors, it was also related to feeding and eating more unhealthy foods among parents with higher BMI. Future studies should consider the longer-term impact of guilt on feeding and eating behavior. Further research is necessary to understand the best ways to communicate potentially guilt-inducing health messages to parents, and how these guilty feelings affect their health behaviors.
Footnotes
Sensitivity analyses were conducted to ensure that these results were not influenced by a lack of foods that parents would typically feed their child in the VR buffet. After the buffet, parents reported the extent to which the foods in the buffet were ones that they serve their child on a scale from 1 (not at all) to 5 (very much). Both of the analyses examining feeding outcomes were re-run with only the 74.6% of parents who reported a 4 or 5 on this scale. The pattern of results remained the same.
References
- Adamo KB, & Brett KE (2014). Parental perceptions and childhood dietary quality. Maternal and Child Health Journal, 18(4), 978–995. [DOI] [PubMed] [Google Scholar]
- Ambwani S, Thomas KM, Hopwood CJ, Moss SA, & Grilo CM (2014). Obesity stigmatization as the status quo: Structural considerations and prevalence among young adults in the US. Eating Behaviors, 15(3), 366–370. [DOI] [PubMed] [Google Scholar]
- Barriuso L, Miqueleiz E, Albaladejo R, Villanueva R, Santos JM, & Regidor E (2015). Socioeconomic position and childhood-adolescent weight status in rich countries: a systematic review, 1990–2013. BMC Pediatrics, 15(1), 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg KC, Crosby RD, Cao L, Crow SJ, Engel SG, Wonderlich SA, & Peterson CB (2015). Negative affect prior to and following overeating-only, loss of control eating-only, and binge eating episodes in obese adults. International Journal of Eating Disorders, 48(6), 641–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Best JR, Goldschmidt AB, Mockus-Valenzuela DS, Stein RI, Epstein LH, & Wilfley DE (2016). Shared weight and dietary changes in parent–child dyads following family-based obesity treatment. Health Psychology, 35(1), 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birbilis M, Moschonis G, Mougios V, & Manios Y (2013). Obesity in adolescence is associated with perinatal risk factors, parental BMI and sociodemographic characteristics. European Journal of Clinical Nutrition, 67(1), 115. [DOI] [PubMed] [Google Scholar]
- Borelli JL, Nelson-Coffey SK, River LM, Birken SA, & Moss-Racusin C (2017). Bringing work home: Gender and parenting correlates of work-family guilt among parents of toddlers. Journal of Child and Family Studies, 26(6), 1734–1745. [Google Scholar]
- Bouhlal S, Abrams LR, McBride CM, & Persky S (2018). Cognitive and affective factors linking mothers’ perceived weight history to child feeding. European Journal of Clinical Nutrition, 72, 1583–1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2017, August). Adult Obesity Causes & Consequences. Retrieved from https://www.cdc.gov/obesity/adult/causes.html. [Google Scholar]
- Conradt M, Dierk JM, Schlumberger P, Rauh E, Hebebrand J, & Rief W (2008). Who copes well? Obesity-related coping and its associations with shame, guilt, and weight loss. Journal of Clinical Psychology, 64(10), 1129–1144. [DOI] [PubMed] [Google Scholar]
- Cotte J, Coulter RA, & Moore M (2005). Enhancing or disrupting guilt: The role of ad credibility and perceived manipulative intent. Journal of Business Research, 58(3), 361–368. [Google Scholar]
- Dallman MF (2010). Stress-induced obesity and the emotional nervous system. Trends in Endocrinology & Metabolism, 21(3), 159–165. 10.1016/j.tem.2009.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis-Becker K, Peterson CM, & Fischer S (2014). The relationship of trait negative urgency and negative affect to disordered eating in men and women. Personality and Individual Differences, 56, 9–14. [Google Scholar]
- de Hooge IE, Breugelmans SM, & Zeelenberg M (2008). Not so ugly after all: when shame acts as a commitment device. Journal of Personality and Social Psychology, 95(4), 933. [DOI] [PubMed] [Google Scholar]
- DeSteno D, Gross JJ, & Kubzansky L (2013). Affective science and health: The importance of emotion and emotion regulation. Health Psychology, 32(5), 474. [DOI] [PubMed] [Google Scholar]
- Dwyer LA, Bolger N, Laurenceau JP, Patrick H, Oh AY, Nebeling LC, & Hennessy E (2017). Autonomous motivation and fruit/vegetable intake in parent–adolescent dyads. American Journal of Preventive Medicine, 52(6), 863–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faith MS, & Kerns J (2005). Infant and child feeding practices and childhood overweight: the role of restriction. Maternal & Child Nutrition, 1(3), 164–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faith MS, Scanlon KS, Birch LL, Francis LA, & Sherry B (2004). Parent-child feeding strategies and their relationships to child eating and weight status. Obesity Research, 12(11), 1711–1722. [DOI] [PubMed] [Google Scholar]
- Ferrer RA, Green PA, & Barrett LF (2015). Affective science perspectives on cancer control: Strategically crafting a mutually beneficial research agenda. Perspectives on Psychological Science, 10(3), 328–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer RA, Klein WMP, Lerner JS, Reyna V, & Keltner D (2016). Emotions and health decision making: Extending the Appraisal Tendency Framework to improve health and health care Roberto C & Kawachi I (Eds.), Behavioral economics and public health (pp. 101–131). Cambridge, MA; Harvard University Press. [Google Scholar]
- Ferrer RA, Klein WMP, Avishai A, Jones K, Villegas M & Sheeran P (2018). When does risk perception predict protection motivation? A person-by-situation analysis. PLoS ONE, 13(3), e0191994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fointiat V, Morisot V, & Pakuszewski M (2008). Effects of past transgressions in an induced hypocrisy paradigm. Psychological Reports, 103(2), 625–633. [DOI] [PubMed] [Google Scholar]
- Garg N, & Lerner JS (2013). Sadness and consumption. Journal of Consumer Psychology, 23(1), 106–113. 10.1016/j.jcps.2012.05.009 [DOI] [Google Scholar]
- Hofmann W, & Fisher RR (2012). How guilt and pride shape subsequent self-control. Social Psychological and Personality Science, 3(6), 682–690. [Google Scholar]
- Kuijer RG & Boyce JA (2014). Chocolate cake. Guilt or celebration? Associations with healthy eating attitudes, perceived behavioural control, intentions and weight-loss. Appetite, 74, 48–54. [DOI] [PubMed] [Google Scholar]
- Kuijer RG, Boyce JA, & Marshall EM (2015). Associating a prototypical forbidden food item with guilt or celebration: Relationships with indicators of (un) healthy eating and the moderating role of stress and depressive symptoms. Psychology & Health, 30(2), 203–217. [DOI] [PubMed] [Google Scholar]
- Kröller K, & Warschburger P (2009). Maternal feeding strategies and child’s food intake: considering weight and demographic influences using structural equation modeling. International Journal of Behavioral Nutrition and Physical Activity, 6(1), 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leach CW (2017). Understanding shame and guilt In Woodyatt L, Worthington E, Wenzel M, & Griffin B (Eds.) Handbook of the Psychology of Self-Forgiveness (pp. 17–28). New York: Springer [Google Scholar]
- Leach CW, & Cidam A (2015). When is shame linked to constructive approach orientation? A meta-analysis. Journal of Personality and Social Psychology, 109(6), 983. [DOI] [PubMed] [Google Scholar]
- Liss M, Schiffrin HH, & Rizzo KM (2013). Maternal guilt and shame: The role of self-discrepancy and fear of negative evaluation. Journal of Child and Family Studies, 22(8), 1112–1119. [Google Scholar]
- Macht M, & Dettmer D (2006). Everyday mood and emotions after eating a chocolate bar or an apple. Appetite, 46(3), 332–336. 10.1016/j.appet.2006.01.014 [DOI] [PubMed] [Google Scholar]
- McBride CM, Persky S, Wagner LK, Faith MS, & Ward DS (2013). Effects of providing personalized feedback of child’s obesity risk on mothers’ food choices using a virtual reality buffet. International Journal of Obesity, 37(10), 1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKimmie BM, Terry DJ, Hogg MA, Manstead AS, Spears R, & Doosje B (2003). I’m a hypocrite, but so is everyone else: Group support and the reduction of cognitive dissonance. Group Dynamics: Theory, Research, and Practice, 7(3), 214. [Google Scholar]
- Mitchell GL, Farrow C, Haycraft E, & Meyer C (2013). Parental influences on children’s eating behaviour and characteristics of successful parent-focussed interventions. Appetite, 60, 85–94. [DOI] [PubMed] [Google Scholar]
- Muraven M, Collins RL, Shiffman S, & Paty JA (2005). Daily fluctuations in self-control demands and alcohol intake. Psychology of Addictive Behaviors, 19(2), 140. [DOI] [PubMed] [Google Scholar]
- Nepper MJ, & Chai W (2016). Parents’ barriers and strategies to promote healthy eating among school-age children. Appetite, 103, 157–164. [DOI] [PubMed] [Google Scholar]
- Onwezen MC, Bartels J, & Antonides G (2014). The self-regulatory function of anticipated pride and guilt in a sustainable and healthy consumption context. European Journal of Social Psychology, 44(1), 53–68. [Google Scholar]
- Ozier AD, Kendrick OW, Leeper JD, Knol LL, Perko M, & Burnham J (2008). Overweight and obesity are associated with emotion-and stress-related eating as measured by the eating and appraisal due to emotions and stress questionnaire. Journal of the American Dietetic Association, 108(1), 49–56. [DOI] [PubMed] [Google Scholar]
- Persky S, McBride CM, Faith MS, Wagner LK, & Ward DS (2015). Mothers’ guilt responses to children’s obesity risk feedback. Journal of Health Psychology, 20(5), 649–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persky S, Ferrer RA, Klein WMP, Goldring MR, Cohen RW, Kistler WD, Yaremych H, Bouhlal S (2018a). Effects of fruit and vegetable feeding messages on mothers and fathers: Interactions between emotional state and health message framing. Annals of Behavioral Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persky S, Goldring MR, Turner SA, Cohen RW, & Kistler WD (2018b). Validity of assessing child feeding with virtual reality. Appetite, 123, 201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pescud M & Pettigrew S (2014). ‘I know it’s wrong, but…’: A qualitative investigation of low-income parents’ feelings of guilt about their child-feeding practices. Maternal & Child Nutrition, 10(3), 422–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pocock M, Trivedi D, Wills W, Bunn F, & Magnusson J (2010). Parental perceptions regarding healthy behaviours for preventing overweight and obesity in young children: a systematic review of qualitative studies. Obesity Reviews, 11(5), 338–353. [DOI] [PubMed] [Google Scholar]
- Rosenkranz RR, & Dzewaltowski DA (2008). Model of the home food environment pertaining to childhood obesity. Nutrition Reviews, 66(3), 123–140. [DOI] [PubMed] [Google Scholar]
- Salovey P, Rothman AJ, Detweiler JB, & Steward JB, & Wayne T (2000). Emotional states and physical health. American Psychologist, 55(1), 110. [DOI] [PubMed] [Google Scholar]
- Savage JS, Fisher JO, & Birch LL (2007). Parental influence on eating behavior: conception to adolescence. The Journal of Law, Medicine & Ethics, 35(1), 22–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, & Bhadoria AS (2015). Childhood obesity: Causes and consequences. Journal of Family Medicine and Primary care, 4(2), 187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarnier M, Schmader T, & Lickel B (2009). Parental shame and guilt: Distinguishing emotional responses to a child’s wrongdoings. Personal Relationships, 16(2), 205–220. [Google Scholar]
- Sheeran P, & Webb TL (2016). The intention–behavior gap. Social and Personality Psychology Compass, 10(9), 503–518. [Google Scholar]
- Sheikh S, & Janoff-Bulman R (2010). The “shoulds” and “should nots” of moral emotions: A self-regulatory perspective on shame and guilt. Personality and Social Psychology Bulletin, 36(2), 213–224. [DOI] [PubMed] [Google Scholar]
- Spence C, Okajima K, Cheok AD, Petit O, & Michel C (2016). Eating with our eyes: From visual hunger to digital satiation. Brain and Cognition, 110, 53–63. [DOI] [PubMed] [Google Scholar]
- Steenhuis I (2009). Guilty or not? Feelings of guilt about food among college women. Appetite, 52(2), 531–534. [DOI] [PubMed] [Google Scholar]
- Stice E (1992). The similarities between cognitive dissonance and guilt: Confession as a relief of dissonance. Current Psychology, 11(1), 69–77. [Google Scholar]
- Sutherland JA (2010). Mothering, guilt and shame. Sociology Compass, 4(5), 310–321. [Google Scholar]
- Tangney JP, Stuewig J, & Mashek DJ (2007). Moral emotions and moral behavior. Annual Review of Psychology, 58, 345–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services, National Heart, Lung and Blood Institute (2013). We Can! GO, SLOW, and WHOA Foods. Retrieved from https://www.nhlbi.nih.gov/health/educational/wecan/downloads/go-slow-whoa.pdf
- Ward ZJ, Long MW, Resch SC, Giles CM, Cradock AL, & Gortmaker SL (2017). Simulation of growth trajectories of childhood obesity into adulthood. New England Journal of Medicine, 377(22), 2145–2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardle J (1995). Parental influences on children’s diets. Proceedings of the Nutrition Society, 54(3), 747–758. [DOI] [PubMed] [Google Scholar]
- Weller RE, Cook III EW, Avsar KB, & Cox JE (2008). Obese women show greater delay discounting than healthy-weight women. Appetite, 51(3), 563–569. [DOI] [PubMed] [Google Scholar]
- Wicker FW, Payne GC, & Morgan RD (1983). Participant descriptions of guilt and shame. Motivation and Emotion, 7(1), 25–39. [Google Scholar]
- Xu Z, & Guo H (2018). A meta-analysis of the effectiveness of guilt on health-related attitudes and intentions. Health Communication, 33(5), 519–525. [DOI] [PubMed] [Google Scholar]