Abstract
Obesity is associated with elevated levels of TNF-α and proinflammatory CD11c monocytes/macrophages. TNF-α mediated dysregulation in the plasticity of monocytes/macrophages is concomitant with pathogenesis of several inflammatory diseases, including metabolic syndrome, but the underlying mechanisms are incompletely understood. Since neutral sphingomyelinase-2 (nSMase2: SMPD3) is a key enzyme for ceramide production involved in inflammation, we investigated whether nSMase2 contributed to the inflammatory changes in the monocytes/macrophages induced by TNF-α. In this study, we demonstrate that the disruption of nSMase activity in monocytes/macrophages either by chemical inhibitor GW4869 or small interfering RNA (siRNA) against SMPD3 results in defects in the TNF-α mediated expression of CD11c. Furthermore, blockage of nSMase in monocytes/macrophages inhibited the secretion of inflammatory mediators IL-1β and MCP-1. In contrast, inhibition of acid SMase (aSMase) activity did not attenuate CD11c expression or secretion of IL-1β and MCP-1. TNF-α-induced phosphorylation of JNK, p38 and NF-κB was also attenuated by the inhibition of nSMase2. Moreover, NF-kB/AP-1 activity was blocked by the inhibition of nSMase2. SMPD3 was elevated in PBMCs from obese individuals and positively corelated with TNF-α gene expression. These findings indicate that nSMase2 acts, at least in part, as a master switch in the TNF-α mediated inflammatory responses in monocytes/macrophages.
Subject terms: Immunology, Biomarkers
Introduction
Obesity triggers low grade chronic inflammation in peripheral tissues such as adipose tissue and liver, which promotes various metabolic dysfunctions and thus contributes to the development of insulin resistance. In obese adipose tissue, there is an influx of immune cells, particularly monocytes (precursor cells of macrophages) and lymphocytes, which secrete inflammatory cytokines that promote inflammation1. Monocytes isolated from obese humans display an inflammatory phenotype associated with the higher expression of surface marker of inflammation CD11c and higher secretion of pro-inflammatory cytokines/chemokines such as TNF-α, IL-6, IL-1β, and MCP-1 compared to monocytes from the lean individuals2,3. Monocytes/Macrophages are predominantly involved in immune modulation in obesity and respond to environmental signals with notable plasticity and adopt different forms and functions that can be characterized as pro-inflammatory M1 and anti-inflammatory M2. Obesity is associated with adipose tissue inflammation via increasing M1 macrophage polarization4.
Obesity-driven changes of the adipose tissue monocytes/macrophages alter the secretion of the proinflammatory cytokines which contribute to the progression of inflammation and development of insulin resistance. Tumor necrosis factor-α (TNF-α) is a cytokine identified as a key regulator of inflammation and insulin resistance, and it is overexpressed in obese humans and rodents5. In settings of obesity, TNF-α has been considered mainly pro-inflammatory as it activates immune cells particularly monocytes and macrophages into inflammatory state, M1 versus M26. However, the mechanistic pathways by which TNF-α induces this pro-inflammatory shift in monocytes/macrophages remain elusive. Ceramide, a bioactive sphingolipid, has been implicated in the pathogenesis of obesity and insulin resistance7. Ceramide is produced through various pathways; however, the hydrolysis of membrane sphingomyelin by sphingomyelinases (SMases) plays a predominant role in the production of ceramide. Neutral sphingomyelinase 2 (nSMase2), the product of the sphingomyelin phosphodiesterase 3 (SMPD3) gene, is a crucial enzyme involved in multiple cell regulatory pathways such as cell cycle arrest and exosome formation8. TNF-α activates nSMase2 resulting in hydrolysis of sphingomyelin to ceramide9. Here, we report that inhibition of nSMase2 by either chemical inhibition or siRNA reduced the TNF-α-mediated expression of inflammatory marker (CD11c) on monocytes/macrophages. Furthermore, inhibition of nSMase2 attenuated the TNF-α-mediated secretion of inflammatory markers IL-1β and MCP-1. The phosphorylation of JNK, p38 and NF-κB major downstream signaling molecules of TNF-α was decreased by inhibition of nSMase2. Moreover, our data show that SMPD3 was elevated in the PBMCs of obese individuals and positively corelated with TNF-α. Collectively, our data reveal an interesting and novel role of nSMase2 in TNF-α-driven inflammation.
Results
Inhibition of the nSMase2 attenuates TNF-α induced inflammatory responses in monocytic cells
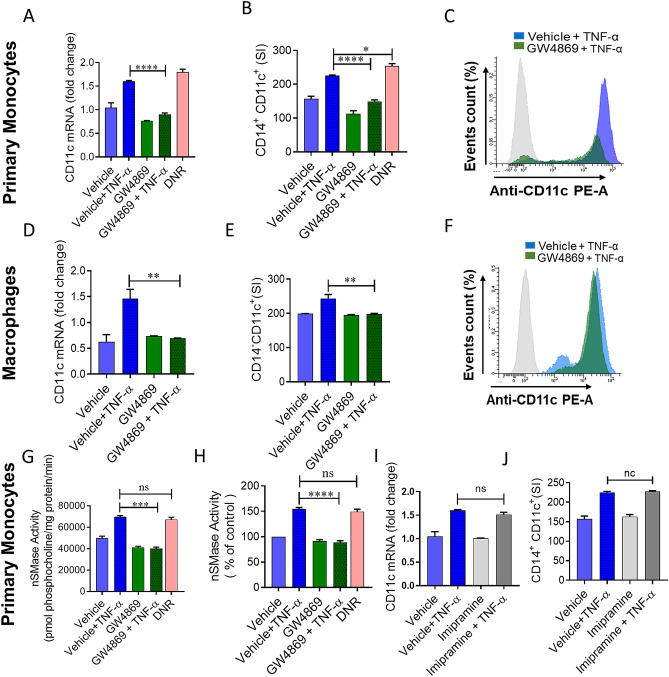
nSMase2 is involved in many pathophysiological inflammatory processes10. However, its role in the TNF-α-mediated plasticity of monocytes/macrophages is not defined yet. In the settings of obesity, CD11c is abundantly expressed in monocytes and macrophages2. Therefore, we questioned whether nSMase2 was required for TNF-α-mediated activation of primary monocytes, using GW4869 to inhibit nSMase activity. Pretreatment with the nSMase2 inhibitor GW4869, followed by exposure to TNF-α, caused a significant suppression in the expression of the phenotypic inflammatory marker (CD11c) at both mRNA and protein levels in human primary monocytes (Fig. 1A–C). Daunorubicin (DNR) has been shown to activate nSMase211; therefore, we asked whether DNR induced changes in the expression of inflammatory markers in monocytic cells. Our data show that DNR induces inflammatory change in monocytes that was comparable to TNF-α, manifested by increased CD11c expression (Fig. 1A–C).
Figure 1.
nSMase inhibition blocks TNF-α mediated pro-inflammatory changes in human monocytes/macrophages. Primary monocytes were pretreated with nSMase inhibitor (GW4869: 10 µM), nSMase agonist (DNR; 1 µM) or vehicle for 1 h and then incubated with TNF-α for 2 h. Cells were harvested, and mRNA of CD11c was determined by real time RT-PCR (A). After 6 h treatment with TNF-α, cells were stained with antibodies against CD14 and CD11c along with matched isotype controls. Surface expression of CD14+CD11c+ was assessed by flow cytometry, (B) data are presented as a bar graph of mean staining index, and (C) representative histogram. Macrophages derived from monocytes were pre-incubated with (GW4869: 10 µM) for 1 h and then treated with TNF-α. (D) CD11c mRNA expression and (E,F) surface expression of CD14+CD11c+ were assessed by flow cytometry. Monocytic cells (Primary monocytes) were pretreated with nSMase inhibitor (GW4869: 10 µM) or vehicle for 1 h and then incubated with TNF-α for 10 min. (G) nSMase activity measured in in equal amount of protein (20 µg); (H) nSMase activity as percentage of expression to vehicle. Primary monocytes were pretreated with aSMase inhibitor (lim: 10 µM) or vehicle for 1 h and then incubated with TNF-α for 2 h or 6 h. (I and J) Cells were harvested, and mRNA of CD11c and surface expression of CD14+CD11c+ cells were determined. Unstimulated cells were used as controls for different treatments. The results obtained from minimum three independent experiments with three replicates of each experiment are shown. All data are expressed as mean ± SEM (n ≥ 3). *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001, ****p ≤ 0.0001 versus vehicle.
Since macrophages are key regulators of adipose tissue functions during metabolic inflammation, we further asked whether chemical inhibition of nSMase2 attenuates macrophage expression of CD11c. Using macrophages derived from primary monocytes, we found that the presence of GW4869 inhibited TNF-α-induced CD11c upregulation in macrophages (Fig. 1D–F). A similar observation was seen in THP1 human monocytic cells (Supplemental Fig. 1A–C). Next, we determined nSMase activity in monocytic cells treated with TNF-α or DNR. In this regard, we found that nSMase activity was higher in cells treated with TNF-α or DNR compared to the cells treated with vehicle. Furthermore, GW4869 significantly inhibited TNF-α mediated nSMase activity in monocytic cells (Fig. 1G,H).
TNF-α has also been reported to upregulate aSMase activity and subsequently modulate inflammatory signaling pathways12. Therefore, we wanted to know whether there was any involvement of aSMase in the inflammatory responses induced by TNF-α. To this end, cells were treated with imipramine (a functional inhibitor of aSMase13 followed by treatment with TNF-α. The results indicated that there was no change after imipramine treatment in TNF-α mediated inflammatory responses in monocytic cells (Fig. 1I,J). These results rule out the possible involvement of aSMase in TNF-α mediated inflammatory responses. Collectively our results show that nSMase is involved in the TNF-α mediated upregulation of CD11c expression in human monocytic cells and macrophages.
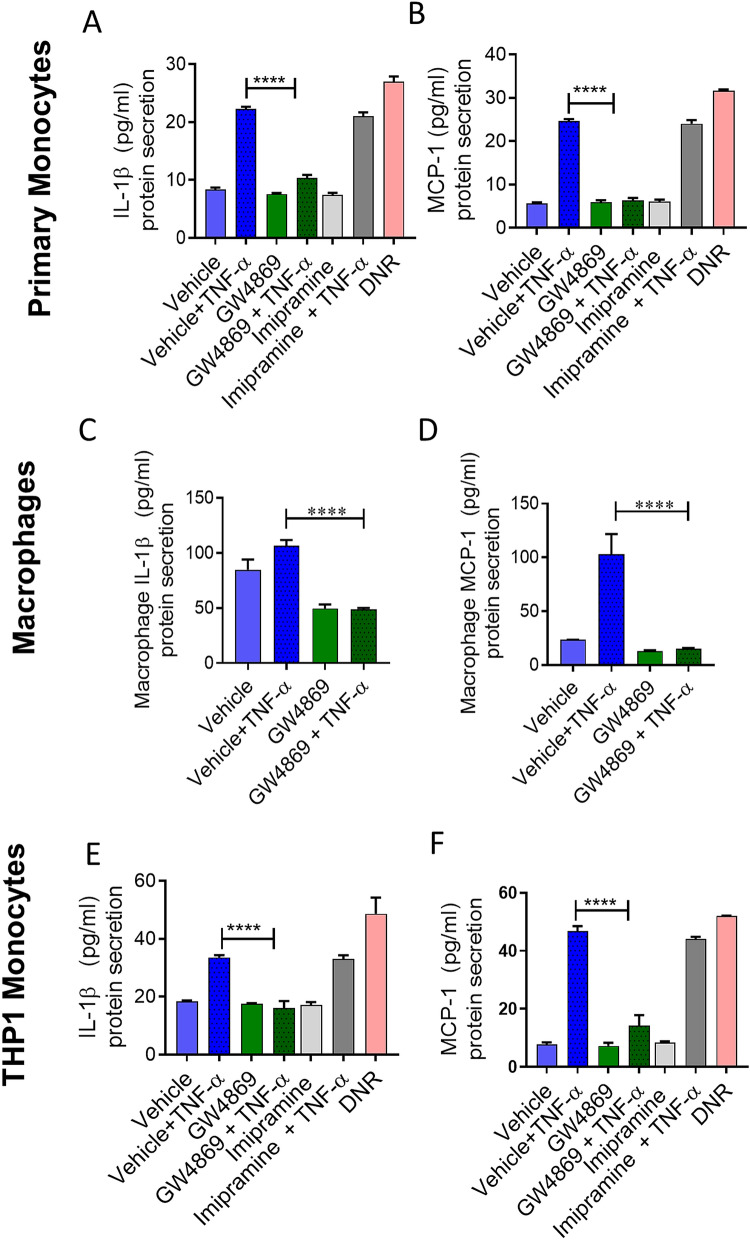
nSMase inhibition reduces TNF-α mediated IL-1β and MCP-1 production
Activated monocytes/macrophages contribute to the pathogenesis of several diseases by secreting inflammatory cytokines including IL-1β and MCP-114. Next, we asked whether IL-1β and MCP-1 production by TNF-α activated primary monocytes or THP1 monocytic cells was reduced by the inhibition of nSMase2. We found that TNF-α induced IL-1β and MCP-1 in monocytic cells (Fig. 2A–F). However, TNF-α did not show induction of IL-6 in monocytic cells in vitro setting of experiments (Supplemental Fig. 2A,B). The results showed that inhibition of nSMase2 significantly reduced the production of IL-1β and MCP-1 by TNF-α activated primary monocytes (Fig. 2A,B), macrophages (Fig. 2C,D) and THP1 monocytic cells (Fig. 2E,F). However, inhibition of aSMase activity by imipramine did not suppress TNF-α induced IL-1β and MCP-1(Fig. 2A,B,E,F). DNR, which activates nSMase2, showed similar production of cytokines as noted in case of TNF-α stimulation (Fig. 2A,B,E,F), suggesting that induction of nSMase2 is sufficient to induce these changes. Together, these results indicate that TNF-α regulates the production of key inflammatory cytokines IL-1β and MCP-1 through the activation of nSMase.
Figure 2.
IL-1β and MCP-1 secreted by TNF-α activated monocytes are suppressed by nSMase inhibition. Monocytic cells (primary monocytes, macrophages, THP-1 cells) were pretreated with nSMase inhibitor (GW4869: 10 µM), nSMase agonist (DNR: 1 µM), aSMase inhibitor (imipramine: 10 µM) or vehicle for 1 h and then incubated cells with absence or presence of TNF-α for 12 h. Secreted IL-1β and MCP-1 protein in culture media was determined by ELISA. (A,B) IL-1β and MCP1 secreted by primary monocytes, (C,D) primary macrophages and (E,F) THP-1 cells. The results obtained from minimum three independent experiments with three replicates of each experiment are shown. All data are expressed as mean ± SEM (n ≥ 3). *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001, ****p ≤ 0.0001 versus vehicle.
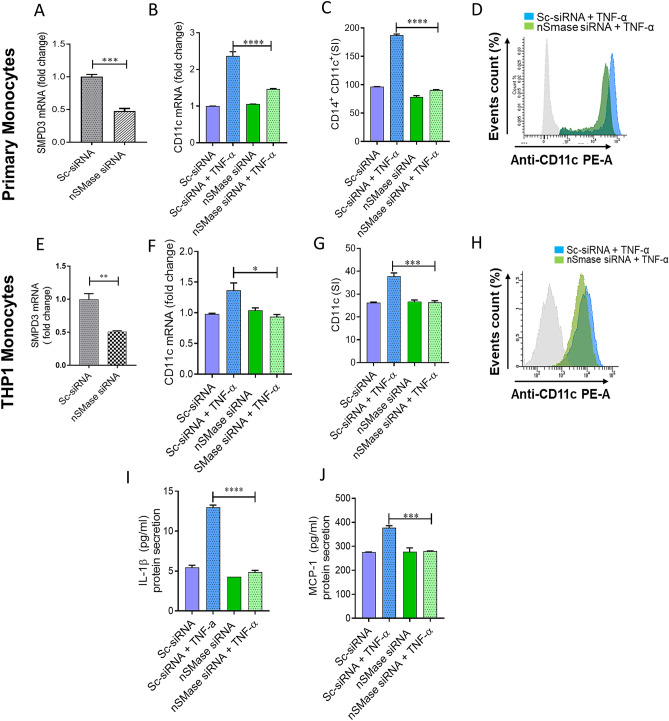
nSMase2 deficiency impairs TNF-α mediated pro-inflammatory responses in human monocytes/macrophages
To further define the role of nSMase2 in TNF-α-induced inflammatory alteration in primary monocytes and in THP1 monocytic cells, we transfected cells with siRNA against nSMase2 (SMPD3), which achieved 50 -70% reduction in nSMase2 mRNA levels compared with scramble (control) siRNA (Fig. 3A,E). Results showed that the expression of CD11c, at both the mRNA and protein levels, was significantly reduced in SMPD3 siRNA–transfected primary monocytes (Fig. 3B–D) as well as THP1 monocytes (Fig. 3F–H) after stimulation with TNF-α compared to the cells transfected with scramble siRNA. Next, we wanted to see whether nSMase2 deficiency in monocytic cells affected the TNF-α induced production of IL-1β and MCP-1. As expected, our results showed that monocytic cells deficient in nSMase2 failed to respond to TNF-α treatment for secretion of IL-1β and MCP-1 (Fig. 3I–J). Overall, the results suggest the significant involvement of nSMase2 in inflammatory responses induced by TNF-α in monocytic cells.
Figure 3.
TNF-α mediated pro-inflammatory monocytic responses requires nSMase2. Primary monocytes and THP-1 monocytes were transfected with scramble-siRNA (negative control; Sc) or SMPD3 siRNA and incubated for 36 h. Real-time PCR was performed to measure (A) SMPD3 expression in primary monocytes and (B) CD11c was determined by real time RT-PCR. Cells were stained with antibodies against CD14 and CD11c along with matched isotypes and were subjected to flow cytometry analysis. (C) Flow cytometry data are presented as a bar graph of mean staining index of CD14+CD11c+ cells as well as (D) representative histogram. nSMase deficient THP-1 cells were treated with TNF-α and vehicle. (E) SMPD3 expression in transfected THP-1 monocytic cells. (F) CD11c mRNA was determined by real time RT-PCR. Cells were stained with antibody against CD11c along with matched isotype controls and assessed by flow cytometry. (G) Flow cytometry data are presented as a bar graph of mean staining index as well as (H) representative histogram. (I–J) Secreted IL-1β and MCP-1 by nSMase2 deficient cells. The results obtained from minimum three independent experiments with three replicates of each experiment are shown. All data are expressed as mean ± SEM (n ≥ 3). *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001, ****p ≤ 0.0001 versus vehicle.
MAPKs and NF-kB activation signal downstream of nSMase2 in TNF-α mediated inflammation
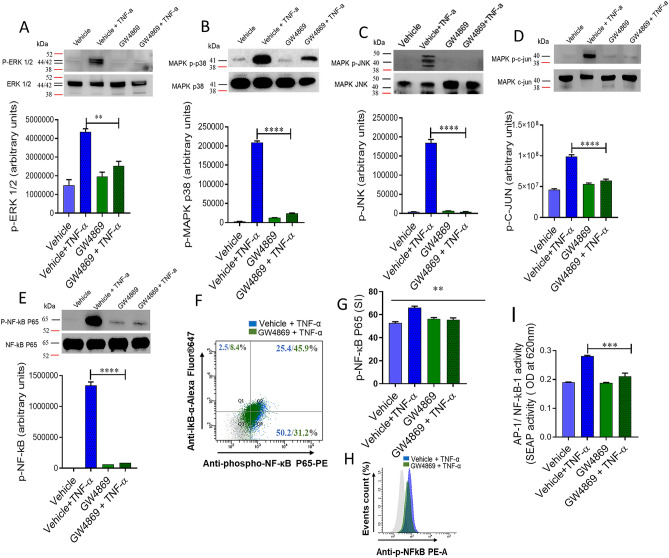
MAPK and NF-kB signaling pathways function downstream of TNFR activation. Therefore, we questioned whether nSMase2 is involved in the TNF-α mediated activation of MAPK and NF-κB signaling pathways. To gain insight into the nSMase2 function in the TNF-α-induced activation of the MAPK and NF-kB signaling pathways, we treated cells with the nSMase inhibitor (GW4869) prior to TNF-α treatment. The results showed that inhibition of nSMase2 significantly reduced the TNF-α mediated phosphorylation of ERK1/2 (Fig. 4A), p38 (Fig. 4B), JNK (Fig. 4C), c-Jun (Fig. 4D) and the p65 subunit of NF-kB (Fig. 4E–H).
Figure 4.
Inhibition of nSMase affects TNF-α activated MAPK and NF-κB signaling pathways in monocytic cells. Monocytic cells were pretreated with nSMase inhibitor (GW4869: 10 µM) and then incubated with TNF-α for 15 min. Cell lysates were prepared as described in Methods. Samples were run on denaturing gels. Immuno-reactive bands were developed using an Amersham ECL Plus Western Blotting Detection System (GE Healthcare, Chicago, IL, USA) and visualized by Molecular Imager ChemiDoc Imaging Systems (Bio-Rad Laboratories, Hercules, CA, USA). (A) Phosphorylated proteins of ERK1/2 (p42/44), (B) p38 MAPK, (C) JNK, (D) c-Jun and (E) NF-κB are depicted in the upper panels and total respective proteins are shown in the lower panels. Phosphorylation intensity of p38 MAPK, ERK1/2, and NF-κB was quantified using Image Lab software (version 6.0.1, Bio-Rad, Hercules, CA, USA) and are presented in arbitrary units. All data are expressed as mean ± SEM (n ≥ 3). **** P < 0.0001 versus TNF-α without respective inhibitor. NF-κB phosphorylation was also determined by flow cytometry. (F) Representative flow cytometry dot plots of p-NF-κB fluorescence versus total IκBα cells. (G) Flow cytometry data are presented as a bar graph of mean staining index as well as (H) representative histogram. Bar graphs depict mean values ± SEM of staining intensity (SI). P < 0.05 was considered as statistically significant (*P ≤ 0.05; **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001). The data in all Figures are representative of three independent experiments. (I) NF-κB reporter monocytic cells were pretreated with nSMase inhibitor (GW4869: 10 µM) or vehicle for 1 h and then incubated with TNF-α for 12 h. Cell culture media were assayed for SEAP reporter activity (degree of NF-κB activation).
NF-κB and AP-1 are downstream transcription factors of TNF-α activation. To further confirm the role of nSMase2 in TNF-α mediated activation of NF-κB/AP-1, we used NF-κB/AP-1 activity reporter human monocytic cells. The data showed that TNF-α induced higher NF-κB/AP-1 activity in the reporter cells and this activity was not seen in the cells treated with nSMase2 inhibitor (Fig. 4I). Together, these data support the role of nSMase2 in the TNF-α mediated activation of NF-kB and AP1 transcription factors.
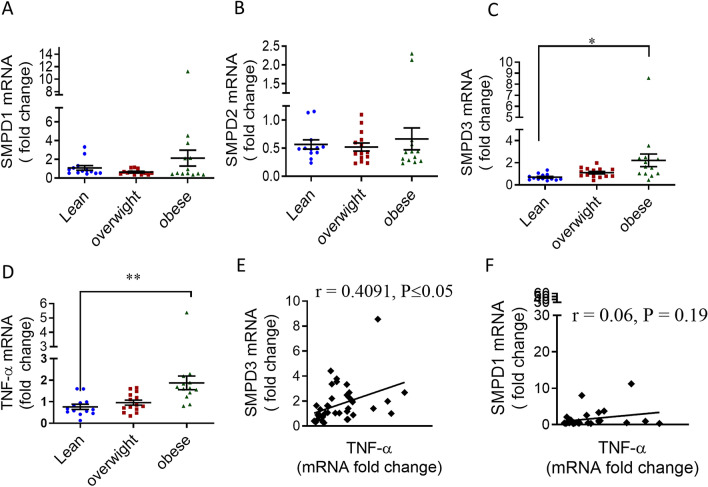
Association of TNF-α and nSMase2 expression in human PBMCs with various BMI
The in vitro data implicated the involvement of nSMase2 in the TNF-α mediated inflammatory responses in the human monocytes/macrophages. Next, we examined the role of nSMase2 and TNF-α in PBMCs of the obese individuals. To this end, we isolated RNA from the PBMCs of 40 individuals (lean, overweight, obese) and determined gene expression SMPD1(aSMase), SMPD2, SMPD3 and TNF-α (Fig. 5A–D). The data showed that nSMase2 (SMPD3) and TNF-α expression levels are elevated in obese individuals as compared to lean (Fig. 5C–D). Furthermore, nSMase2 was positively correlated with TNF-α (Fig. 5E). However, aSMase gene (SMPD1) expression was not elevated in PBMCs of the obese individuals as compared to lean individuals (Fig. 5A) and had no association with TNF-α (Fig. 5F). Likewise, the expression of nSMase1 (product of SMPD2 gene) was not elevated (Fig. 5B). Overall, nSMase2 and TNF-α show an elevated and associated expression in human PBMCs.
Figure 5.
Association of elevated TNF-α with SMPD3 levels in obese human PBMCs. PBMCs were isolated from human blood samples obtained from lean (n = 13), overweight (n = 13) and obese (n = 13) individuals. mRNA of SMPD1 (aSMase), SMPD2 (nSMase), SMPD3 (nSMase) and TNF-α were detected by real time RT-PCR and represented as fold change over controls. (A–D) Each dot represents the individual value of SMPD1, SMPD2, SMPD3 or TNF-α mRNA. Lines represented the mean values of PBMCs’ SMPD1, SMPD2, SMPD3 and TNF-α of each group. (E) Correlation of SMPD3 and (F) SMPD1 mRNA with TNF-α in PBMCs of obese individuals.
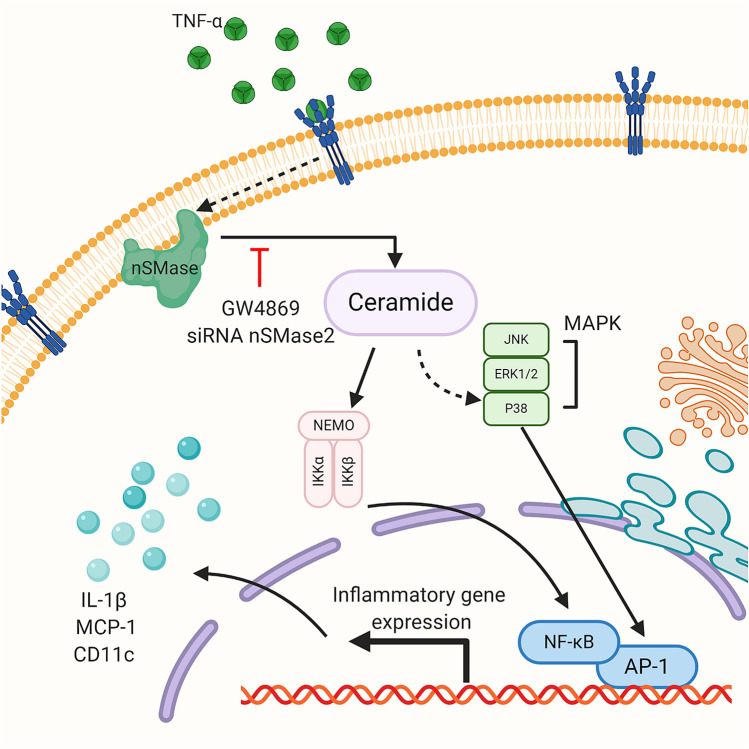
To summarize the involvement of nSMase2 in TNF-α mediated inflammatory responses in human monocytic cells, a schematic illustration is presented in Fig. 6.
Figure 6.
Schematic illustration of the role of nSMase2 in TNF-α mediated inflammatory response in monocytic cells. The pathway highlights that disruption of nSMase2 activity by GW4869 or SMPD3 suppresses TNF-α induced production of inflammatory markers (CD11c, MCP-1, IL-1β) in monocytic cells. SM, sphingomyelin.
Discussion
Obesity-driven changes of the adipose tissue monocytes/macrophages alters the secretion of proinflammatory cytokines which contributes to the progression of inflammation and the development of insulin resistance15,16. Tumor necrosis factor-α (TNF-α), which is overexpressed in obese humans and rodents, plays a central role in metabolic inflammation and insulin resistance. TNF-α in obesity has been considered mainly pro-inflammatory as it activates immune cells, particularly monocytes and macrophages into a pro-inflammatory phenotype, M1 versus M217. However, the etiology of how inflammatory monocytes/macrophages are developed and activated by TNF-α remains unclear. TNF-α activates membrane-associated nSMase2 which cleaves sphingomyelin to produce ceramide, a second messenger activated through the tumor necrosis factor (TNF) receptor18. In this study we report that nSMase2 is involved in TNF-α-mediated inflammatory responses of monocytes/macrophages which were characterized by elevated expression of CD11c, an integrin receptor recently shown to regulate adhesion to VCAM-1 on inflamed endothelium. This was accompanied by an increase in the secretion of IL-1β and MCP-1, suggesting monocytic cells activation and having inflammatory phenotype14,18,19. The current results show that inhibiting the activity of the nSMase2 by GW4869 suppressed the TNF-α induced CD11c expression on monocytes. In contrast, the inhibition of aSMase had no effect on the TNF-α mediated expression of CD11c in monocytic cells, demonstrating the participation of a specific sphingomyelinase. Moreover, nSMase2 deficiency prevented TNF-α-induced pro-inflammatory shift in monocytes, suggesting the notion that inflammatory response mediated by TNF-α is suppressed by disruption of nSMase2. Increased expression of CD11c on monocytes occurs in a wide range of inflammatory disorders such as coronary artery disease, asthma, infection, obesity, and T2D20,21. It has been reported that high fat diet-induced obesity in mice generates a high numbers of CD11c+ monocytes/macrophages and TNF-α22. Actually, TNF-α-mediated phenotypic shift of monocytes/macrophages in the adipose tissue is a central element of metabolic inflammation and insulin resistance in obese mice.
CD11c+ monocytes are actively involved in the production of inflammatory cytokines and chemokines including IL-1β, TNF-α, and MCP-1, pointing to increased migration of the inflammatory monocytes from the circulation into adipose tissue in obesity23. Our data show that the secretion of the IL-1β and MCP-1 by the TNF-α-activated monocytes was significantly suppressed by blocking of nSMase2. IL-1β and MCP-1 expression in obesity appears to be vital for phenotypic and functional M1 polarization of monocytes/macrophages in response to TNF-α24. It is evident that monocytes isolated from obese humans with diabetes display an inflammatory phenotype and secrete higher levels of pro-inflammatory mediators such as IL-6, MCP-1, and IL-1β leading in metabolic dysfunction25. Metabolic dysfunction is implicated in a wide-ranging effect on the immune cells, inflammation and lipid metabolism associated with adipocytes26. TNF-α activates the plasma membrane nSMase2 that hydrolyzes sphingomyelin to ceramide results its accumulation within the cell9. nSMase regulates inflammatory responses via ceramide production and inhibition or deficiency of nSMase2 reduces inflammation. Lallemand et al. (2018) demonstrated nSMase2 deficiency or inhibition by GW4869 reduces inflammation27 supporting our findings. Obesity elevates TNF-α expression in adipose tissues28 and it induces ceramide production via hydrolysis of SM by SMases suggesting that Ceramide is an interlink between overnutrition and the production inflammatory cytokines.
Substantial progress has been made in understanding the ability of TNF-α to activate MAPKs and NF-κB signaling pathways involved in the regulation of several inflammatory cytokines that contribute to the pathogenesis of different inflammatory conditions29. MAPK signaling molecules interact with each other along with having extensive cross-talk to other inflammatory pathways including NF-kB in orchestration of inflammatory responses30,31 . It has been reported by our group and others that ERK, JNK and NF-kB contribute to TNF-α-induced IL-8, CCL2 and CCL4 expression and secretion by monocytic cells which indicates that MAPK and NF-kB pathways regulate the gene expression of a variety of cytokines, and playing an important role in inflammation. TNF-α-induced CD11c expression, as well as IL-1β secretion in the lungs of mice was found to be dependent on p38 MAPK signaling32. Previous studies have demonstrated that p38 MAPK phosphorylation can result in nSMase2 activation and that it is associated with inflammation stress33. Consistent with previous studies14, we found that TNF-α strongly induced phosphorylation of ERK1/2, p38 MAPK, JNK, C-Jun and NF-kB in monocytic cells. Our results showed that blocking of nSMase2 activity inhibits the TNF-α mediated phosphorylation of p38 MAPK, JNK, c-Jun, NF-kB. NF-kB and AP-1 are key transcription factors downstream of TNFR signaling pathways, our results showed that activation of these two transcription factors inhibited by inhibition of nSMase2. These results suggest that nSMase2 may acts upstream of MAPK and NF-kB signaling pathways.
In conclusion, our study unveils a novel effect of nSMase2 on TNF-α mediated inflammatory responses in monocytic cells/macrophages that is dependent on the MAPK and NF-kB signaling pathways. These findings also support a possible association between TNF-α and nSMase2 in obesity that link may contribute to metabolic inflammation.
Methods
Cell culture
Monocytes, human monocytic THP-1 cells were purchased from American Type Culture Collection (ATCC) and grown in RPMI-1640 culture medium (Gibco, Life Technologies, Grand Island, USA) supplemented with 10% fetal bovine serum (Gibco, Life Technologies, Grand Island, NY, USA), 2 mM glutamine (Gibco, Invitrogen, Grand Island, NY, USA), 1 mM sodium pyruvate, 10 mM HEPES, 100 ug/ml Normocin, 50 U/ ml penicillin and 50 μg/ml streptomycin (P/S; (Gibco, Invitrogen, Grand Island, NY, USA). They were incubated at 37 °C (with humidity) in 5% CO2. NF-kB reporter monocytic cells (THP-1-XBlue) stably expressing a secreted embryonic alkaline phosphatase (SEAP) reporter inducible by NF-κB were purchased from InvivoGen (InvivoGen, San Diego, CA, USA). THP-1-XBlue cells were cultured in complete RPMI medium with the addition of zeocin (200 μg/ml) (InvivoGen, San Diego, CA, USA). Prior to stimulation, monocytes were transferred to normal medium and plated in 12-well plates (Costar, Corning Incorporated, Corning, NY, USA) at 1 × 106 cells/well cell density unless indicated otherwise.
PBMCs collection and monocyte purification
Human peripheral blood (40 ml) samples were collected from study participants in EDTA vacutainer tubes. All participants had provided written informed consent, and the study was conducted in accordance with the ethical principles of the Declaration of Helsinki and approved (04/07/2010; RA-2010-003) by the Ethical Review Committee of Dasman Diabetes Institute, Kuwait. Physical characteristics of the study participants are shown in Table 1. PBMCs were isolated by using Histo-Paque density gradient method as we described earlier34. PBMCs were plated in 6-well plates (Costar, Corning Incorporated, Corning, NY, USA) at 3 × 106 cells/well in starvation medium for 3 h at 37 °C. Non-adhered cells were removed, and monocytes that had adhered to the plate were washed with culture media without serum and incubated for 24 h in RPMI with 2% Fetal Bovine serum.
Table 1.
Physical characteristics of the study participants.
| Characteristics | Lean | Overweight | Obese | p-value |
|---|---|---|---|---|
| Age (years) | 41 ± 10.78 | 42.6 ± 14.09 | 47.9 ± 13.1 | 0.421 |
| Weight (kg) | 60.7 ± 7.37 | 74.4 ± 9.88 | 104.6 ± 16.2 | < 0.0001**** |
| Height (m) | 1.64 ± 0.05 | 1.62 ± 0.12 | 1.7 ± 0.08 | 0.13 |
| BMI (kg/m2) | 22.3 ± 2.19 | 28.05 ± 1.05 | 35.8 ± 3.54 | < 0.0001**** |
| Waist to hip circumference | 0.80 ± 0.023 | 0.87 ± 0.06 | 1.0 ± 0.08 | 0.06 |
| Body fat percentage (%) | 31.9 ± 5.9 | 37.1 ± 3.92 | 38.1 ± 3.95 | 0.114 |
Macrophage differentiation
PBMCs were plated in 6-well plates (Costar, Corning Incorporated, Corning, NY, USA) at 3 × 106 cells/well in starvation medium for 3 h at 37 °C. Non-adhered cells were removed, and monocytes that had adhered to the plate were washed with culture media without serum and incubated for 5 days in RPMI with 2% Fetal Bovine serum (FBS) and M-CSF (10 ng/ml). Differentiated cells were washed carefully and incubated in fresh RPMI (2% FBS) for 24 h. Macrophages derived from monocytes were used for different treatments. THP-1 cells(1 × 106 cells per ml) were cultured using 12-well plates (Costar, Corning Incorporated, Corning, NY) in RPMI 1640 medium (Life Technologies, Grand Island, NY) containing 10% FBS (Life Technologies), 2 mM glutamine, 1 mM sodium pyruvate, 10 mM HEPES, 100 μg/ml Normocin, 50 U/ml penicillin, and 50 μg/ml streptomycin, and cells were incubated at 37 °C in 5% CO2 under humidity. THP-1 cells were differentiated into macrophages by treatment with PMA (10 ng/ml) for 3 d in routine culturing media. Cells were washed and then incubated in RPMI (10%FBS) for 48 h. before subjected to the different treatments.
Cell stimulation
Monocytes were plated in 12-well plates (Costar, Corning Incorporated, Corning, NY, USA) at 1 × 106 cells/well concentration unless indicated otherwise. Cells were pre-treated with Neutral sphingomyelinase nSMase2 specific inhibitor (GW4869) (Sigma D1692, 10 µM/ml), then stimulated with TNF-α (10 ng/ml) or Vehicle (0.1% BSA) for 2 h at 37 °C. Cells were harvested for RNA isolation. For measuring secretion of IL-1β and MCP-1 into media, TNF-α stimulation was carried out for 12 h, and culture media were collected for analysis of IL-1β and MCP-1. For MAPK’s and NF-kB signaling pathway analysis, cultures were treated with the inhibitor as stated above then stimulated with TNF-α or BSA vehicle for 10–15 min.
Real time quantitative RT-PCR
Total RNA was extracted using RNeasy Mini Kit (Qiagen, Valencia. CA, USA) per the manufacturer’s instructions. The cDNA was synthesized using 1 μg of total RNA using high capacity cDNA reverse transcription kit (Applied Biosystems, Foster city, CA, USA). Real-time PCR was performed on 7500 Fast Real-Time PCR System (Applied Biosystems, Foster City, CA, USA) using TaqMan Gene Expression Master Mix (Applied Biosystems, Foster city). Each reaction contained 50 ng cDNA that was amplified with Inventoried TaqMan Gene Expression Assay products (SMPD3: Assay ID:Hs00920354_m1; SMPD2:Assay ID: Hs00906924_g1; SMPD1:Assay ID: Hs03679346_g1; CD11c: Assay ID: Hs00174217_m1; GAPDH: Hs03929097_g1;). The threshold cycle (Ct) values were normalized to the house-keeping gene GAPDH, and the amounts of target mRNA relative to control were calculated with ΔΔCt-method35,36. Relative mRNA expression was expressed as fold expression over average of control gene expression. The expression level in control treatment was set at 1. Values are presented as mean ± SEM. Results were analyzed statistically; P < 0.05 was considered significant.
Extracellular staining-flow cytometry
Monocytic cells were seeded in 24 well plate at 0.5 × 105 cell/ml in serum free media overnight. Cells were treated with nSMase inhibitor GW4869 (10 µM/ml) for one hour or 0.01% DMSO (vehicle) then subjected to stimulation with TNF-α (10 ng/ml) or BSA (vehicle) for 6 h. Monocytic cells (1 × 106 cells) were resuspended in FACS staining buffer (BD Biosciences) and blocked with human IgG (Sigma; 20 μg) for 30 min on ice. Cells were washed and resuspended in 100 ul of FACS buffer and incubated with CD14-Alexa Fluor 488 (5ul/test; cat# 561706; BD Biosciences), CD11c (S_HCL-3)-PE (0.25ug/20ul/test; cat# 347637; BD Biosciences) , CD11c PE-Cy7 (0.25ug/test; cat # 117317; Biolegend, San Diego, CA ) or isotype control antibody (mouse IgG2a,k-Alexa Fluor 488, cat # 558055; mouse IgG2b, κ-PE 559529; mouse IgG2b, κ-PE-Cy7 Cat # 560542: BD Biosciences) on ice for 30 min. Cells were washed three times with FACS buffer and resuspended in 2% paraformaldehyde. Cells were centrifuged and resuspended in FACS buffer for FACS analysis (FACSCanto II; BD Bioscience, San Jose, USA). FACS data analysis was performed using BD FACSDiva Software 8 (BD Biosciences, San Jose, USA). Unstained cells were used to set the quadrant of the negative versus positive gates and represented as light grey in histogram. The stain index (SI) was calculated as the difference between the mean fluorescence intensity of the positive and negative populations, divided by two times the standard deviation of the negative populations ‘unstained cells. We used unstimulated cells as controls for different treatments.
Intracellular staining-flow cytometry
Flow cytometry analysis was used to investigate the expression of signaling pathway markers. Briefly, cells were seeded in 24 well plate at 0.5 × 105 cells/ml in serum free media overnight. Cells were treated with nSMase inhibitor GW4869 or DMSO (vehicle) then subjected to stimulation with TNF-α (10 ng/ml) or BSA (vehicle) for 10 min. After stimulation, cells were collected and washed. Cells were then incubated with fixation/permeabilization buffer (cat# 00-5523-00, eBioscience, San Diego, CA, USA) for 20 min in 4 °C, followed by washing and staining with mouse anti-human p-NF-kB P65-PE (20ul/test; cat # 558423; BD Biosciences) and Alexa Fluor 647 mouse anti-IκBα (5ul/test; cat # 560817; BD Biosciences) or control isotypes (mouse IgG2b, κ-PE, Cat# 559529; Mouse IgG1-Alexa Fluor 647, Cat # 560817) for 30 min. The cells were then washed and resuspended in PBS supplemented with 2% FCS for FACS analysis (FACSCanto II; BD Bioscience, San Jose, USA). FACS data analysis was performed using BD FACSDiva Software 8 (BD Biosciences, San Jose, USA). We used unstimulated cells as controls for different treatments.
IL-1β and MCP-1 determination
Secreted IL-1β and MCP-1 proteins in supernatants of monocytic cells stimulated with TNF-α were quantified using sandwich ELISA following the manufacturer's instructions (R&D systems, Minneapolis, USA). Secreted IL-6 protein was determined by using human IL-6 DuoSet ELISA following the manufacturer’s instructions (R&D systems, Minneapolis, USA).
Small interfering RNA (siRNA) transfections
Monocytes were washed and resuspended in 100 µl of nucleofector solution provided with the Amaxa Noclecfector Kit V and transfected separately with siRNA-n-SMase (Santa Cruz Biotechnology, INK. SC-106277), scramble (control) siRNA (30 nM; OriGene Technologies, Inc. MD, USA, USA), and pmaxGFP (0.5 ug; Amaxa Nucleofector Kit V for THP-1, Lonza). All transfection experiments were performed with Amaxa Cell Line Nucleofector Kit V for monocytic cells(Lonza, Germany) by using Amaxa Electroporation System (Amaxa Inc, Germany) according to the manufacturer's protocol37. After 36 h of transfection, cells were treated with TNF-α for 2 h. For knock down of nSMase2 in human primary monocyte cultures, cells were transfected with 20 nM of the siRNA using Viromer Blue (lipocalyx, Halle, Germany) according to the manufacturer’s instructions. Cells were harvested for RNA isolation and staining study. nSMase gene knock down level was assessed by Real Time-PCR using SMPD3 gene-specific primer probes.
Measurement of NF-κB activity
NF-kB reporter monocytes (THP-1 XBlue; InvivoGen, San Diego, CA) are stably transfected with a reporter construct expressing a secreted embryonic alkaline phosphatase (SEAP) gene under the control of a promoter inducible by the transcription factors NF-κB. Upon stimulation, NF-κB is activated and subsequently the secretion of SEAP is stimulated. Cells were stimulated with TNF-α (10 ng/ml) for 6–12 h at 37 °C. Levels of SEAP were detected in the culture media after 3 h incubation of supernatants with Quanti-Blue solution (InvivoGen, San Diego, CA, USA) at 650 nm wavelength by ELISA reader.
Western blotting
After different treatments, cells were harvested and incubated for 30 min with lysis buffer (Tris 62.5 mM (pH 7.5), 1% Triton X-100, 10% glycerol). The lysates were then centrifuged at 14,000 rpm for 10 min and the supernatants were collected. Protein concentration in the lysates was measured by Quickstart Bradford Dye Reagent, 1 × Protein Assay kit (Bio-Rad Laboratories, Inc, CA). Protein (20 μg) samples were mixed with sample loading buffer, heated for 5 min at 95 °C and resolved by 12% SDS-PAGE. Cellular proteins were transferred to Immuno-Blot PVDF membrane (Bio-Rad Laboratories, USA) by electro blotting. The membranes were then blocked with 5% non-fat milk in PBS for 1 h, followed by incubation with primary antibodies against p-ERK1/2, p-p38, p-JNK, p-NF-ΚB and respective total antibodies in 1:1000 dilution at 4 °C overnight. All the primary antibodies were purchased from Cell Signaling (Cell Signaling Technology, Inc). The blots were then washed four times with TBS and incubated for 2 h with HRP-conjugated secondary antibody (Promega, Madison, WI, USA) in 1:2500 dilution. Immunoreactive bands were developed using an Amersham ECL Plus Western Blotting Detection System (GE Health Care, Buckinghamshire, UK) and visualized by Molecular Imager ChemiDoc Imaging Systems (Bio-Rad Laboratories, Hercules, CA, USA).
Statistical analysis
Statistical analysis was performed using GraphPad Prism software (La Jolla, CA, USA). Data are shown as mean ± standard error of the mean, unless otherwise indicated. Unpaired Student t-test and one-way ANOVA followed by Tukey's test were used to compare means between groups. For all analyses, data from a minimum of three sample sets were used for statistical calculation. P value < 0.05 was considered significant. Ns: no significance, *P < 0.05, ** P < 0.01, *** P < 0.001 and **** P < 0.0001).
Supplementary information
Acknowledgements
This work was supported by Kuwait Foundation for the Advancement of Sciences (KFAS) Grant RA AM 2016-007, RA 2010-003 to RA and NIH Grant GM118128 to YAH.
Author contributions
F.A., Z.A., R.T., M.M., A.S. performed experiments, analyzed data and participated in writing manuscript. L.O., F.A.M., Y.A.H. participated in designing, planning experiments and in critical review and editing manuscript, R.A. planned, designed experimental work, interpreted data and wrote the manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
is available for this paper at 10.1038/s41598-020-73912-5.
References
- 1.Pecht T, et al. Circulating blood monocyte subclasses and lipid-laden adipose tissue macrophages in human obesity. PLoS ONE. 2016;11:e0159350. doi: 10.1371/journal.pone.0159350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wouters K, et al. Circulating classical monocytes are associated with CD11c. Sci. Rep. 2017;7:42665. doi: 10.1038/srep42665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Braune J, et al. IL-6 regulates M2 polarization and local proliferation of adipose tissue macrophages in obesity. J. Immunol. 2017;198:2927–2934. doi: 10.4049/jimmunol.1600476. [DOI] [PubMed] [Google Scholar]
- 4.Kapellos TS, et al. Human monocyte subsets and phenotypes in major chronic inflammatory diseases. Front Immunol. 2019;10:2035. doi: 10.3389/fimmu.2019.02035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahmad R, et al. The synergy between palmitate and TNF-α for CCL2 production is dependent on the TRIF/IRF3 pathway: implications for metabolic inflammation. J. Immunol. 2018;200:3599–3611. doi: 10.4049/jimmunol.1701552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kang YE, et al. The roles of adipokines, proinflammatory cytokines, and adipose tissue macrophages in obesity-associated insulin resistance in modest obesity and early metabolic dysfunction. PLoS ONE. 2016;11:e0154003. doi: 10.1371/journal.pone.0154003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sokolowska E, Blachnio-Zabielska A. The role of ceramides in insulin resistance. Front Endocrinol. (Lausanne) 2019;10:577. doi: 10.3389/fendo.2019.00577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Y, Cao Y. The sphingomyelin synthase family: proteins, diseases, and inhibitors. Biol. Chem. 2017;398:1319–1325. doi: 10.1515/hsz-2017-0148. [DOI] [PubMed] [Google Scholar]
- 9.Clarke CJ, Guthrie JM, Hannun YA. Regulation of neutral sphingomyelinase-2 (nSMase2) by tumor necrosis factor-alpha involves protein kinase C-delta in lung epithelial cells. Mol. Pharmacol. 2008;74:1022–1032. doi: 10.1124/mol.108.046250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Airola MV, et al. Structure of human nSMase2 reveals an interdomain allosteric activation mechanism for ceramide generation. Proc. Natl. Acad. Sci. USA. 2017;114:E5549–E5558. doi: 10.1073/pnas.1705134114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gu L, et al. Early activation of nSMase2/ceramide pathway in astrocytes is involved in ischemia-associated neuronal damage via inflammation in rat hippocampi. J. Neuroinflam. 2013;10:109. doi: 10.1186/1742-2094-10-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Henkes LE, et al. Acid sphingomyelinase involvement in tumor necrosis factor alpha-regulated vascular and steroid disruption during luteolysis in vivo. Proc. Natl. Acad. Sci. USA. 2008;105:7670–7675. doi: 10.1073/pnas.0712260105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liangpunsakul S, et al. Imipramine blocks ethanol-induced ASMase activation, ceramide generation, and PP2A activation, and ameliorates hepatic steatosis in ethanol-fed mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2012;302:G515–523. doi: 10.1152/ajpgi.00455.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al-Rashed F, et al. TNF-α induces a pro-inflammatory phenotypic shift in monocytes through ACSL1: relevance to metabolic inflammation. Cell Physiol. Biochem. 2019;52:397–407. doi: 10.33594/000000028. [DOI] [PubMed] [Google Scholar]
- 15.Longo M, et al. Adipose tissue dysfunction as determinant of obesity-associated metabolic complications. Int. J. Mol. Sci. 2019 doi: 10.3390/ijms20092358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu R, Nikolajczyk BS. Tissue immune cells fuel obesity-associated inflammation in adipose tissue and beyond. Front Immunol. 2019;10:1587. doi: 10.3389/fimmu.2019.01587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee CH, Lam KS. Obesity-induced insulin resistance and macrophage infiltration of the adipose tissue: a vicious cycle. J. Diabetes Invest. 2019;10:29–31. doi: 10.1111/jdi.12918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clarke CJ, Truong TG, Hannun YA. Role for neutral sphingomyelinase-2 in tumor necrosis factor alpha-stimulated expression of vascular cell adhesion molecule-1 (VCAM) and intercellular adhesion molecule-1 (ICAM) in lung epithelial cells: p38 MAPK is an upstream regulator of nSMase2. J. Biol. Chem. 2007;282:1384–1396. doi: 10.1074/jbc.M609216200. [DOI] [PubMed] [Google Scholar]
- 19.Noack M, Miossec P. Selected cytokine pathways in rheumatoid arthritis. Semin. Immunopathol. 2017;39:365–383. doi: 10.1007/s00281-017-0619-z. [DOI] [PubMed] [Google Scholar]
- 20.Lewis SM, et al. Expression of CD11c and EMR2 on neutrophils: potential diagnostic biomarkers for sepsis and systemic inflammation. Clin. Exp. Immunol. 2015;182:184–194. doi: 10.1111/cei.12679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Klementowicz JE, et al. Cutting edge: origins, recruitment, and regulation of CD11c. J. Immunol. 2017;199:27–32. doi: 10.4049/jimmunol.1601062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singer K, et al. Diet-induced obesity promotes myelopoiesis in hematopoietic stem cells. Mol. Metab. 2014;3:664–675. doi: 10.1016/j.molmet.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oh DY, Morinaga H, Talukdar S, Bae EJ, Olefsky JM. Increased macrophage migration into adipose tissue in obese mice. Diabetes. 2012;61:346–354. doi: 10.2337/db11-0860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Palma A, Jarrah AS, Tieri P, Cesareni G, Castiglione F. Gene regulatory network modeling of macrophage differentiation corroborates the continuum hypothesis of polarization states. Front Physiol. 2018;9:1659. doi: 10.3389/fphys.2018.01659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alvarado-Vázquez PA, et al. Cytokine production capabilities of human primary monocyte-derived macrophages from patients with diabetes mellitus type 2 with and without diabetic peripheral neuropathy. J. Pain Res. 2019;12:69–81. doi: 10.2147/JPR.S186372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reddy P, Lent-Schochet D, Ramakrishnan N, McLaughlin M, Jialal I. Metabolic syndrome is an inflammatory disorder: a conspiracy between adipose tissue and phagocytes. Clin. Chim. Acta. 2019;496:35–44. doi: 10.1016/j.cca.2019.06.019. [DOI] [PubMed] [Google Scholar]
- 27.Lallemand T, et al. nSMase2 (type 2-neutral sphingomyelinase) deficiency or inhibition by GW4869 reduces inflammation and atherosclerosis in Apoe. Arterioscler. Thromb. Vasc. Biol. 2018;38:1479–1492. doi: 10.1161/ATVBAHA.118.311208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hotamisligil GS, Spiegelman BM. Tumor necrosis factor alpha: a key component of the obesity-diabetes link. Diabetes. 1994;43:1271–1278. doi: 10.2337/diab.43.11.1271. [DOI] [PubMed] [Google Scholar]
- 29.Shi JH, Sun SC. Tumor necrosis factor receptor-associated factor regulation of nuclear factor κB and mitogen-activated protein kinase pathways. Front Immunol. 2018;9:1849. doi: 10.3389/fimmu.2018.01849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tibbles LA, Woodgett JR. The stress-activated protein kinase pathways. Cell Mol. Life Sci. 1999;55:1230–1254. doi: 10.1007/s000180050369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kyriakis JM, Avruch J. Mammalian MAPK signal transduction pathways activated by stress and inflammation: a 10-year update. Physiol. Rev. 2012;92:689–737. doi: 10.1152/physrev.00028.2011. [DOI] [PubMed] [Google Scholar]
- 32.Gupta J, Nebreda AR. Roles of p38α mitogen-activated protein kinase in mouse models of inflammatory diseases and cancer. FEBS J. 2015;282:1841–1857. doi: 10.1111/febs.13250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Back MJ, et al. Activation of neutral sphingomyelinase 2 by starvation induces cell-protective autophagy via an increase in Golgi-localized ceramide. Cell Death Dis. 2018;9:670. doi: 10.1038/s41419-018-0709-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ahmad R, El Bassam S, Cordeiro P, Menezes J. Requirement of TLR2-mediated signaling for the induction of IL-15 gene expression in human monocytic cells by HSV-1. Blood. 2008;112:2360–2368. doi: 10.1182/blood-2008-02-137711. [DOI] [PubMed] [Google Scholar]
- 35.Wray GM, Foster SJ, Hinds CJ, Thiemermann C. A cell wall component from pathogenic and non-pathogenic gram-positive bacteria (peptidoglycan) synergises with endotoxin to cause the release of tumour necrosis factor-alpha, nitric oxide production, shock, and multiple organ injury/dysfunction in the rat. Shock. 2001;15:135–142. doi: 10.1097/00024382-200115020-00010. [DOI] [PubMed] [Google Scholar]
- 36.Al-Rashed F, Kochumon S, Usmani S, Sindhu S, Ahmad R. Pam3CSK4 induces MMP-9 expression in human monocytic THP-1 cells. Cell Physiol. Biochem. 2017;41:1993–2003. doi: 10.1159/000475298. [DOI] [PubMed] [Google Scholar]
- 37.Sindhu S, Al-Roub A, Koshy M, Thomas R, Ahmad R. Palmitate-induced MMP-9 expression in the human monocytic cells is mediated through the TLR4-MyD88 dependent mechanism. Cell Physiol. Biochem. 2016;39:889–900. doi: 10.1159/000447798. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.