Abstract
Temporomandibular joint (TMJ) arthritis is a common cause of orofacial pain with distressing symptoms. The patients most commonly females are often anxious and worried due to the typical gritty sound produced during chewing moments. In other cases there is pain followed by decreased mouth opening. Currently the treatment is not standardised though the clinicians are treating these disorders either by oral medications; splintage or by injections. Though local injection of Triamcinolone acetonide and Hyaluronic acid is an innovative therapy yet it is elusive of much research. The main aim of the present study is to evaluate the efficacy of with Triamcinolone acetonide and Hyaluronic acid in treating temporomandibular joint arthritis. The present study is a prospective non randomized clinical trial of 100 patients in a tertiary referral centre. The patients diagnosed with temporomandibular joint arthritis were treated with local infiltration of 40 mg triamcinolone acetonide along with 20 mg of hyaluronic acid; one injection every week for 4 weeks. The pre-treatment and post-treatment data was compared using student paired t test and Mann–Whitney U test. Majority of the patients showed relief in symptoms like pain (87/96) and clicking sounds (81/88) and the difference was statistically significant (p < 0.05). Though other symptoms like restrictive mouth opening; discomfort on lateral and medial movement were also relieved in 9/15 patients and 21/23 patients respectively however the difference was not statistically significant. We highly recommend the use of Triamcinolone acetonide and hyaluronic acid injection in TMJ arthritis as it helps in relieving pain and clicking of sound in majority of the patients. The treatment is an out-patient department procedure with almost no side effects in most of the patients. The cost effectiveness of the treatment is another benefit.
Keywords: Temporomandibular joint arthritis, Triamcinolone acetonide, Hyaluronic acid, Jaw pain, Clicking sound over the jaw, Restrictive mouth opening
Introduction
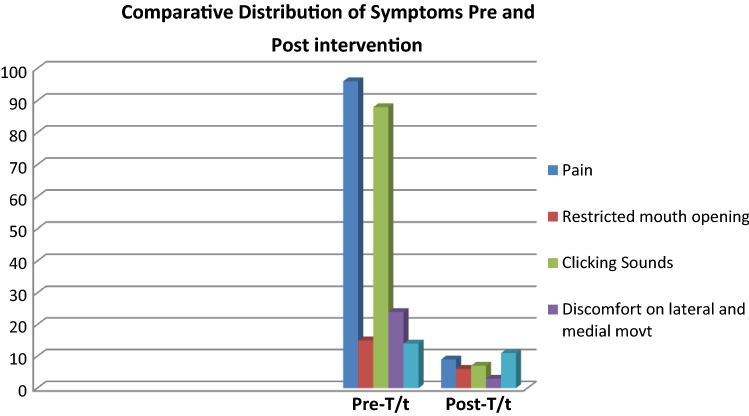
Osteoarthritis (OA) of the temporo-mandibular joint (TMJ) is a unilateral, degenerative disease of the jaw joint. It is characterized by breakdown of the articular cartilage, architectural changes in bone, and degeneration of the synovial tissues causing pain and/or dysfunction in functional movements of the jaw. In osteoarthritis, the jaw joint can be the first joint to get the disease, whereas in rheumatoid arthritis it is the last joint to be affected [1]. One of the most important events in the diagnosis of osteoarthritis was the establishment of a new specialty called oro-facial pain. The oro-facial pain specialist is familiar with the different presentations of osteoarthritis and can coordinate the different specialties necessary to manage the problem. OA is a degenerative joint disease characterized by an accumulation of mechanical stresses to joints, leading to the destruction of articular cartilage It is caused by a combination of (i) increased degradation of extracellular matrix (ECM; some members of the matrix metalloproteinase [MMP] and a disintegrin and metalloproteinase with thrombospondin motifs [ADAMTS] gene families have been correlated with the process of cartilage ECM degradation); (ii) decreased production of ECM; and (iii) chondrocyte death (Fig. 1) [2].
Fig. 1.
Risk factors for osteoarthiritis of temporal mandibular joint
The patients who develop OA present with a variety of symptoms including pain on opening, limited movement to the opposite side, coarse grinding noise on function, history of clicking that has now stopped, and deviation on opening to the affected side. An unusually large percentage of those diagnosed are women around the age of 35 [3]. In addition, substantial number of patients will have had a macrotrauma usually from a maximal voluntary contraction (MVC) force or even a blow to the mandible. The clinical findings are pain on palpation of lateral pole, decreased range of motion, flattened condyle, osteophytes on condyle, heavy occlusion on second molar on the affected side and facial asymmetry. Some other indicators include loss of condylar bone which traumatizes the posterior molar on the same side, pain referral pattern to the ear, pain on eating, talking, or function of the jaw joint, jaw locking, and pain in the front tooth of a bridge due to torque forces on two molars. In summary, a picture of pain, dysfunction, and disability is involved in osteoarthritis of jaw joint.
Triamcinolone is a potent anti-inflammatory steroid classified as synthetic glucocorticoid. It decreases tissue inflammation response by blocking phospholipase A2 in the cell membrane, causing disruption of the activity of Cyclo-oxygenase and Lipo–oxygenase. This action results in the vasodilation and reduction of vascular permeability. Triamcinolone is also a potent immune suppressant which reduces the proliferation of T lymphocytes, monocytes, eosinophils and decreases the binding of immunoglobulins with its receptors [2, 4].
Hyaluronic acid is a linear polysaccharide. It is available in the extracellular matrix of various mammalian tissues including skin, cartilage, umbilical cord, and synovial fluid [5]. Hyaluronic acid may act as a shock absorber that protects cartilage cells from shock waves, and it may also act as a barrier [6]. Hyaluronic acid also has anti-inflammatory actions such as scavenging for free radicals and reducing vascular permeability, as well as inhibition and phagocytosis of polymorphonuclear leucocytes and macrophages. It also has analgesic properties. Several reports have indicated that intra-articular injection of hyaluronic acid may be effective treatment for rheumatoid arthritis, osteoarthritis, and also disorders of the TMJ.
Until recent years, OA of the temporomandibular joint was confusing, relatively unrecognized, and difficult to diagnose and manage. Scientific research had found neither a common cause, nor a clinically useful and differentiable diagnostic test. This resulted in a diagnostic journey full of frustration, pain, and expense. Due to its multifaceted nature, the disease has no defined or linear progression of symptoms. The symptom complex is not the same from one patient to another: it can exist in a quiet state until it is set off by an array of events or it can be painful from the start, neither there is definite treatment option available for effective management of this condition. The infiltration rate of TMJ muscle is an innovative therapy that could be an alternative to traditional treatment. However, there’s not a lot of research done that shows the levels of effectiveness of this therapy, nor it is compared to other non-invasive treatments such as occlusal splints or oral anti inflammatory drug treatments [7].
Intra articular injections of 40 mg kenacort and 20 mg hyaluronic acid have been used after arthrocentesis and compared their efficacy in reducing TMD symptoms like pain, restricted mouth opening, restricted jaw movements and joint sounds. Present Study aims at finding effectiveness of local infiltration of TMJ with combination of 40 mg kenacort injection with 20 mg hyaluronic acid injection for chronic pain and other symptoms of osteoarthritis of TMJ.
Methods and Materials
The Present study was conducted at ENT OPD department of Sri Guru Ram Das University of Health Sciences, Sri Amritsar between June 2018 to June 2019 and is a prospective non-randomized, observational clinical trial conducted on 100 patients aged between 20 and 80 years who complained of oro-facial pain persisting for more than one month after conservative treatment with oral antiinflammatory drugs, local application of antiinflammatory gel and splintage. All the necessary ethical clearance were taken from ethical committee of Sri Guru Ram Das University Of Health Sciences before recruitment of subjects to study and study complied according declaration of Helsinki. All Necessary steps were taken to maintain patient confidentiality at all times. Thorough informed consent was taken from the patient and STROBE (Strengthening the Reports of Observational Studies in Epidemiology) reporting guidelines were used for reporting the study
According to the classification of the AAOP (American Academy of Oro-facial pain) The Facial pain attributed to TMJ disorders had following criteria according to International headache society [8].
-
A.
Recurrent pain in one or more regions of the head and/or face fulfilling criteria C and D
-
B.
X ray, CT scan MRI and/or bone scintigraphy demonstrate TMJ disorder
-
C.Evidence that pain can be attributed to the TMJ disorder, based on at least one of the following
- Pain is precipitated by jaw movements and/or chewing of hard or tough food
- Reduced range of or irregular jaw opening
- Noise from one or both TMJs during jaw movements
- Tenderness of the joint capsule(s) of one or both TMJs
-
D.
D. Headache resolves within 3 months, and does not recur, after successful treatment of the TMJ disorder
Inclusion Criteria Patients aged from 20 to 80 years with a chief complaint of TMJ pain, joint sounds and limited mouth opening, limited lateral, medial and propulsive movements who were not responding to conservative treatments were selected for the study. Patients who have been diagnosed with internal derangement (Anterior disc displacement with or without reduction), with moderate to severe and intractable pain in TMJ due to TMD and who have Clicking/Noises or Crepitus and who do not have any uncontrollable systemic disease were also included in the study.
Exclusion Criteria Patients with at least one of the following criteria were excluded: hypersensitivity to the components of triamcinolone, TMJ infections or surrounding structures, rheumatoid arthritis, asthma, or emphysema or pulmonary fibrosis, allergic disorders (hay fever, vasomotor rhinitis, angioneurotic edema), nephrotic syndrome or renal diseases, previous unsuccessful infiltrations, uncontrolled hypertension, patients taking anti-inflammatory medication, analgesics, muscle relaxants or anxiolytics at least in the last 7 days.
After selection of the patients as per the inclusion & exclusion criteria; a thorough history and head and neck examination was performed for every patient followed by CT imaging to confirm the diagnosis. Radiographic evaluation carefully evaluated radiographic signs of the disease like
Cortical bone erosion
Flattening of joint compartments with productive bone changes such as sclerosis and osteophytes [8].
A panoramic radiograph was obtained to rule out any possible bony pathology, such as bony tumors, that may have contributed to the limitation of mouth opening.
TMJ injection was performed in the affected joint by a senior consultant. The area lateral to the TMJ can be located by the examiner’s finger as a depression just anterior to the tragus of the ear as the patient opens the mouth wide [9]. The TMJ area was palpated by asking the patient to open and close the mouth in quick successions. The area was localised and marked. The injection of 40 mg Triamcolone acetonide (Kenacort) with 20 mg followed by hyaluronic acid (hyalase) were withdrawed from their respective vials in a 5 ml Luer-Lock syringe with a 23-gauge needle and mixed. The contents so obtained were transferred to an insulin syringe. The preauricular skin was disinfected using a 70% isopropyl alcohol pad or 10% povidone-iodine pad, and the patient was asked to open the mouth as wide as possible and needle was inserted into the superior joint space, behind the condyle and beneath the zygoma, and passed in until three fourths of the needle was in the joint space. The solution of hyaluronic acid and triamcinolone acetomide was injected into the space after negative aspiration, and an ice pack was applied to the joint after the injection. Five minutes after the procedure, the patient was assessed for any signs of facial palsy, and manual mobilization of the jaw was performed to improve mouth opening. Patients received instruction on passive stretching exercises to improve mouth opening until follow-up visit at 1st week.
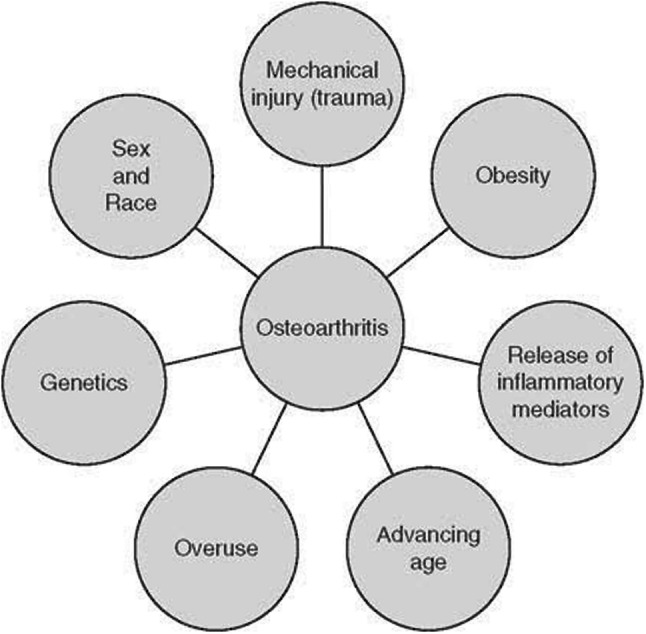
Four injections of Kenacort® and Hyalase®were given were given every 7 days at the site of pain. There was follow-up 30 days after the last infiltration. Evaluation of pre-treatment and post treatment pain on Wong Baker scale from score of 1 to 10, maximal mouth opening, clicking sound, discomfort on protrusive moments and lateral moments were recorded compared on same scale as were done pre-treatment. Any additional side-effects were also recorded. The Postoperative Pain score was recorded using Wong baker Faces Pain Scale. The Wong-Baker Faces Pain Rating Scale is a pain scale that was developed by Donna Wong and Connie Baker. The scale shows a series of faces ranging from a happy face at 0, or “no hurt”, to a crying face at 10, which represents “hurts like the worst pain imaginable”. Based on the faces and written descriptions, the patient chooses the face that best describes their level of pain [10].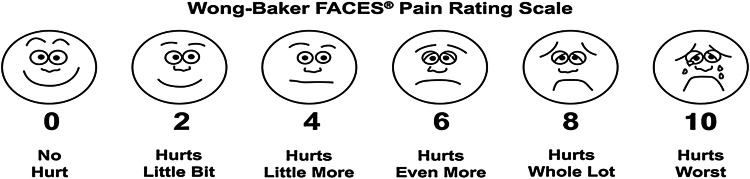
Statistical Analysis: IBM SPSS statistics version 11 was used in recording and analysing the data. Wilcoxon test for comparison of mean pain level on the Wong baker pain scale and other symptoms improvement was used. A significance level of 5% was assumed
Results
Out Of 100 Patients included in the study 33 were males while 77 were females. The age distribution in 20–40 years age group was 17 patients; 40–60 years had 51 patients while 60–80 years group had 32 patients (Table 1). The most common preoperative symptom found in our patients was pain (96% n = 100) though the score was 4 in most of the cases (52% n = 100) followed by score of 6 (40% n = 100) (Table 3). The second most common preoperative symptom in our patients was clicking of sound (88% n = 100); followed by discomfort on medial to lateral movement (24% n = 100); restrictive mouth opening (15% n = 100) and discomfort on protrusive movement (14% n = 100) (Table 2). The post-intervention pain was relieved in 87/96 patients with average pain score reducing to 2.2 compared to 4.54 pre-intervention with p value < 0.05 (Table 2; Fig. 3). Clicking of sound was relieved in 81/88(p < 0.05) patients followed by the relief in discomfort on lateral and medial movements which was reported by 21/23 patients; Though the difference in latter was not statistically significant (p > 0.05). The restrictive mouth opening was relieved in 9 patients though the other 6 felt improvement. The discomfort on protrusive movement was however relieved only in 3 patients. The t scores generated for both were however not statistically significant (Table 2; Fig. 2)
Table 1.
Demographic variables of the study
| Number | |
|---|---|
| Gender | |
| Male | 33 |
| Female | 77 |
| Age group | |
| 20–40 | 17 |
| 40–60 | 51 |
| 60–80 | 32 |
Table 3.
Comparison of pain scores pre and post intervention
| Pain score | Pre-intervention | Post-intervention |
|---|---|---|
| 2 | 3 | 4 |
| 4 | 52 | 3 |
| 6 | 40 | 2 |
| 8 | 1 | 0 |
| 10 | 0 | 0 |
Table 2.
Comparative distribution of pre and post intervention symptoms
| Symptom | Pre-intervention (n = 100) | Post-intervention (n = 100) |
|---|---|---|
| Pain | 96 | 09 |
| Restrictive mouth opening | 15 | 06 |
| Clicking sounds | 88 | 07 |
| Discomfort on lateral & medial movement | 24 | 03 |
| Discomfort on protrusive movement | 14 | 11 |
Fig. 3.
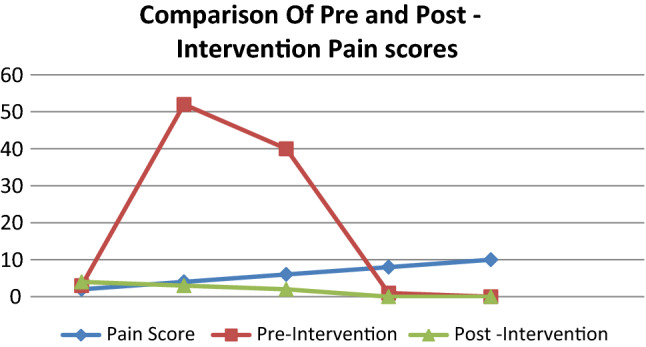
The pre and post intervention average pain scores. Average pre-intervention pain score is 2.2 while post-intervention pain score is 4.54 with p < 0.05
Fig. 2.
The pre-intervention distribution versus post-intervention distribution of the various symptoms of temporomandibular joint arthritis. The relief in pain and clicking sound is statistically significant with p < 0.05
Discussion
Patients with TMJ osteoarthritis have an increased muscle tension caused by the excessive demand of masticatory muscles. They also have an increased tendency of depression and anxiety [7]. However, it is known that 72.5% of patients, even with the presence of pain, enjoy their daily activity
Present study was conducted on carefully selected 100 patients of TM joint arthritis who presented with chief complaints of oro-facial pain, clicking sound from TM joint, restricted mouth opening, discomfort on protrusive and lateral and medial movements of jaw who were not responding to medical line and other conservative forms of treatment for at least one month. All these patients were offered injection therapy with Triamcilone acetonide (kenacort) 40 mg with Hyaluronic acid (Hyalase) 20 mg on affected side on same day of every week for at least 4 weeks. Pre-treatment symptomatology was compared with post-treatment relief of symptoms on same scale during evaluation.
It was observed that there is significant improvement of pre-treatment symptomatology (Orofacial Pain, restricted mouth opening, clicking sound, restricted lateral, medial and protrusive moments) after administration of Kenacort and Hyalase injection for 4 weeks in patients who were diagnosed with TM joint arthritis and those who were not responding to conservative treatment.
Though present study was conducted on carefully selected patients with homogenous symptomatology suggestive of primary diagnosis of TM joint osteoarthritis with well planned treatment protocols and stringent follow up according to the review of literature, there were several potential limitation of the study which included non randomisation and small cohort.
In the present study female gender was most commonly affected, 77 female patients were enrolled out of 100 patients as compared to 33 male patients with commonly affected age group of 40–60 years (51%) followed by 60–80 years (32%) followed by younger age group of 20–40 years (17%) (Table 1). Extensive literature suggests the disorder is 1.5–2 times more prevalent in women than in men, and that 80% of patients treated for TMJ disorders are women. The severity of symptoms is also related to the age of the patients. Pain onset tends to occur after puberty, and peaks in the reproductive years, with the highest prevalence occurring in women aged 20–40, and the lowest among children, adolescents, and the elderly. The gender and age distribution of TMJ disorders suggests a possible link between its pathogenesis and the female hormone axis [11].
That women make up the majority of patients treated for TMJ disorders is extensively hypothesized and documented in numerous epidemiological studies which are all in accordance to finding of present study. In the study conducted by Bagge et al. The prevalence pattern exhibits a bell shaped curve with peak prevalence in 5th and 6th decade followed by a reduction in the progression after 75 years which was also suggested by current study [12].
Orofacial pain was most common symptom 96% patients had orofacial pain (96 out of 100 patients), followed by clicking sound which was present in 88% patients (88 out of 100), discomfort in medial and lateral movement was present in 24 patients (24 out 100) while restrictive mouth opening was present in 15% (15 out of 100) and difficulty in protrusive movements was present in 14% patients (14 out 100) (Table 2). Average pain score on Wong Baker pain scale was 4 which was present in 52 out of 96 patients having pain followed by pain score of 6 which was present in 40 out of 96 patients (Table 3). The most common clinical features of TMJ osteoarthritis are pain, restriction in mouth opening, joint crepitus sounds and absence of joint warmth. Pain is generally dull aching and common during the initial phases and is due to the synovitis [13]. Some patients have morning joint stiffness and increased sensitivity to cold and damp. The pain relieving factors include rest and NSAIDs. In later stages patient may develop facial skeletal remodelling and chin deviation occurs toward the affected side. Occlusal discrepancies and unstable or fluctuating malocclusion are not uncommon. Occlusal changes include anterior open bite, reduced overbite and increased overjet [14]. In study conducted by AK. Abrahamsson et al. it was reported that facial pain and joint sounds were most common clinical symptoms reported in their study followed by restricted mouth opening [15] which were in accordance to present study.
Limited mouth opening is other common presentation of TM joint arthritis, in present study 15 patients out of 100 (15%) had restricted mouth opening which was similar to above quoted study where reported was 13% for restricted mouth opening whereas this finding was contrary to study conducted by Aveed Samiee, Daniel Sabzerou, et al. where all patients had limited mouth opening, had less than or equal to 40 mm at the time of injection. This difference can be due to patient selection criteria at time of presentation [15, 16].
The TMJ disorders are characterized by a classically described triad of clinical signs: muscle and/or TMJ pain, TMJ sounds and restriction, deviation or deflection of mouth opening. Restricted jaw function encompasses a limited range of mandibular movements in all directions. Like pain, restricted jaw function causes a great deal of anxiety for the patient who faces difficulties in everyday activities such as eating and speaking [16, 17].
In the present study significant number of patient s also complained of limitation of range of movements while chewing, like 24 out of 100 (24%) patients had difficulty in moving jaw medially and laterally while 14 out of 100 (14%) had difficulty in protrusion of jaw while chewing food and speaking.
Primary goals of the treatment for TM joint arthritis is to increase the range of motion and relieve the functional pain of the TMJ The widely accepted practice for managing TM joint osteoarthritis includes arthrocentesis followed by manual mobilization of the jaw to improve mouth opening. Several independent studies have shown that arthrocentesis is effective in improving mouth opening in patients with TM joint arthritis. A meta-analysis of surgical treatments for the temporomandibular joint (TMJ) published in 2003 reported that the most reliable evidence supports the use of arthrocentesis and arthroscopy for TM join arthritis patients [18].
In contrast, TMJ injection is a relatively uncommon means of managing the arthritis of this area. Corticosteroids have a potent anti-inflammatory effect on synovial tissue and are known to reduce effusion, decrease pain and bring about an increase in range of motion of synovial joints [19]. Intra-articular corticosteroid injection alone or after arthrocentesis provides, long-term palliative effects on subjective symptoms and clinical signs of TMJ pain [20, 21].
Similarly Several reports have indicated that intra-articular injection of hyaluronic acid may be effective treatment for rheumatoid arthritis, osteoarthritis, and also disorders of the TMJ. It was observed in study conducted by Pavan Kumar et al. arthrocentesis followed by intra articular injection of hyaluronic acid was better than hydrocortisone [22]. In the present study there was clear evidence that post treatment evaluation after administration of Kenacort and Hyalase injection there is marked improvement in symptom score of patients with respect to pain, mouth opening, lateral and medial movements, propulsive movements and clicking sounds. Post Treatment evaluation after one month of injection administration suggested that 87 patients reported improvement in pain score out of 96 patients, clicking sound was improved 81 patients out of 88 patients, 21 patients out 24 patients reported improvement in medial and lateral movement of jaw, restrictive mouth opening was improved in 9 out of 15 patients while just 3 patients improved out of 14 in protusive movements (Table 2; Fig. 2). Post treatment evaluation suggested that out of 9 patient who were having persistent pain after injection therapy 4 patients were having just mild pain on Wong Baker pain scale (average 2) who further responded to oral anti-inflammatory treatment of 2 weeks and 3 patients were having pain score of 4 on Wong Baker pain scale (Table 3; Fig. 3).
Role of Corticosteroids and hyaluronic acid injection has been extensively studied in knee joint arthritis. A study published by The Cochrane Collaboration in 2009, with a sample of 1973 patients divided into 28 groups, evaluated the efficacy of infiltrations in the knee joint with corticosteroids, hyaluronic acid and betamethasone to reduce pain, swelling and disability in patients with osteoarthritis. It was demonstrated that corticosteroids and Hylaruonic acid (HA) were superior for pain reduction compared with betamethasone, a visual analog scale-VAS at treatment completion, the effect of this therapy lasted 4 weeks after the last infiltration; the confidence interval was 95% [23].
The endogenous nature of triamcinolone acetonide and its ability to act locally and protect tissues from damage, are the premises that are based therapeutic applications. Potent anti-inflammatory, anti-allergic and anti-pruritic affect of triamcinolone allows use for treating chronic inflammatory processes as TM joint arthritis [24]. Similarly injection of exogenous HA into a joint may restore the articular viscoelastic properties [25]. A possible mechanism that describes HA therapeutic action in OA has been proposed macroscopically, HA restores the synovium and the organization of healthy cartilage so that the joint can react visco elastically to force application [26, 27]. HA exerts a beneficial effect on the cartilage integrity and response to OA damage, which may be related to a primary effect of HA on the cartilage surface HA may also act on the synovial membrane by limiting the synovial reaction HA exerts a chondro-protective action, which can be explained at different levels. It seems to have a trophic effect on chondrocytes, enhancing their metabolism. Moreover, HA inhibits the development of the fibroblast-like cells in damaged joints [28]. HA protects chondrocytes from oxidative stress through preservation of mitochondrial function, and it inhibits apoptotic and de-differentiative effects of nitric oxide (NO) on chondrocytes, reverting the block of protein kinase C-α [29, 30].
Further recent reports have pointed out the importance of joint lubrication for a correct joint function, also hypothesizing that abnormalities of the joint lubrication system may play a role in the onset of TMJ dysfunctions [31]. An efficient lubrication system in the TMJ is absolutely necessary so the disc can slide along the slope of the eminence. Hyaluronic acid probably plays an important indirect role in joint lubrication by adhering to surface-active phospholipids. It was found that the mechanical lysis of adhesions and lavage of the TMJ was often successful in treating various internal derangements [32].
The infiltration of TMJ with kenacort and hyaluronic acid is an innovative therapy that could be an alternative to traditional treatment which takes the strong advantage of anti-inflammatory action of kenacort and viscoelastic properties of hyalase and this approach has shown significant improvement in pre and post treatment symptom score in present study. However, there’s not a lot of research done that shows the levels of effectiveness of this therapy, nor it is compared to other non-invasive treatments such as occlusal splints or oral drug treatments.
Though this study was prospective non randomised controlled trial, but We hope that the data from this study will lead to such a study comparing TMJ injection with corticosteroid and hyalase to other conservative form of treatment for TM joint osteoarthritis. Such a prospective trial is necessary to compare and contrast the efficacy of these procedures for treatment of TMJ osteoarthritis.
Conclusion
TMJ arthritis is a common cause of orofacial pain. Triamcinolone and Hyaluronic acid injections at the local site are highly effective in treating this disorder. The only caution required is the site of injection should be palpated accurately so that the medication reaches specifically the joint area. It’s a simple OPD procedure with low treatment cost and majority of the patients respond extremely well to this treatment. We highly recommend the use of this treatment by our fellow colleagues and encourage for data collection and analysis so that a standardised regimen can be initiated.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Standards
Before starting the study Ethical Clearance was taken from the institutional ETHICAL Committee as per DECLARATION OF HELSINKI. Informed consent was duly taken from patients.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jaskaran Singh, Email: jassigill001@gmail.com.
Bhanu Bhardwaj, Email: entwithdrbhanu@gmail.com.
References
- 1.Toller P. Osteoarthritis of the mandibular condyle. Brit Dent J. 1973;134:223–231. doi: 10.1038/sj.bdj.4802982. [DOI] [PubMed] [Google Scholar]
- 2.Abramson SB, Attur M (2009) Developments in the scientific understanding of osteoarthritis. Arthritis Res Ther 11(3):227 [DOI] [PMC free article] [PubMed]
- 3.Gremillion H, Bates R, Stewart C. Degenerative joint disease. Part I: Diagnosis & management considerations. J Cranio Prac. 1993;11(4):284–290. doi: 10.1080/08869634.1993.11677980. [DOI] [PubMed] [Google Scholar]
- 4.Bellamy N, Campbell J, Welch V, et al. Intraarticular corticosteroid for treatment of osteoarthritis of the knee (review) Cochrane Database Syst Rev. 2006;19(2):CD005328. doi: 10.1002/14651858.CD005328.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Sharma A, Rana AS, Jain G, Kalra P, Gupta D, Sharma S. Evaluation of efficacy of arthrocentesis (with normal saline) with or without sodium hyaluronate in treatment of internal derangement of TMJ. A prospective randomized study in 20 patients. J Oral Boil Craniofac Res. 2013;3(3):112–119. doi: 10.1016/j.jobcr.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meyer K, Smyth EM, Dawson MH. The isolation of mucopolysaccharide from synovial fluid. J Biol Chem. 1939;128:319–327. [Google Scholar]
- 7.Correa PE, Ríos CD, Porras TDA et al (2019) Infiltration with triamcinolone in patients with temporomandibular disorders. J Dent Maxillofacial Res 2(2):49–52
- 8.Olesen J, Bousser MG, Diener HC, Dodick D, First M, Goadsby PJ, et al. The international classification of headache disorders. Cephalalgia. 2004;24(Suppl. 1):24–150. [Google Scholar]
- 9.Polley HF, Hunder GG. Rheumatologic interviewing and physical examination of the joints. 2. Philadelphia: W. B. Saunders; 1978. p. 48. [Google Scholar]
- 10.Drendel AL, Kelly BT, Ali S. Pain assessment for children overcoming challenges and optimizing care. Pediatric Emerg Care. 2011;27(8):773–781. doi: 10.1097/PEC.0b013e31822877f7. [DOI] [PubMed] [Google Scholar]
- 11.Warren MP, Fried JL. Temporomandibular disorders and hormones in women. Cells Tissues Organs. 2001;169(3):187–192. doi: 10.1159/000047881. [DOI] [PubMed] [Google Scholar]
- 12.Bagge E, Bjelle A, Edén S, Svanborg A. Osteoarthritis in the elderly: clinical and radiological findings in 79 and 85 year olds. Ann Rheum Dis. 1991;50(8):535–539. doi: 10.1136/ard.50.8.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okesan JP (2003) Management of temporomandibular disorders and occlusion, 5th edn, 0-323-01477-1, Mosby Publication (2003) pp 355–356 and pp 465–466
- 14.Buckwalter JA. The role of mechanical forces in the initiation and progression of osteoarthritis. HSS J. 2012;8(1):37–38. doi: 10.1007/s11420-011-9251-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stegenga B, de Bont LG, Boering G, van Willige JD. Tissue responses to degenerative changes in the temporomandibular joint: a review. J Oral Maxillofac Surg. 1991;49(10):1079–1088. doi: 10.1016/0278-2391(91)90143-A. [DOI] [PubMed] [Google Scholar]
- 16.Abrahamsson A-K, Kristensen M, Arvidsson LZ, Kvien TK, Larheim TA, Haugen IK. Frequency of temporomandibular osteoarthritis and related symptoms in a hand osteoarthritis cohort. Osteoarthr Cartil. 2017 doi: 10.1016/j.joca.2016.12.028. [DOI] [PubMed] [Google Scholar]
- 17.Glaros AG, Marszalek JM, Williams KB. Longitudinal multilevel modeling of facial pain, muscle tension, and stress. J Dent Res. 2016;95:416–422. doi: 10.1177/0022034515625216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Auerbach SM, Laskin DM, Frantsve LM, Orr T. Depression, pain, exposure to stressful life events, and long-term outcomes in temporomandibular disorder patients. J Oral Maxillofac Surg. 2001;59:628–633. doi: 10.1053/joms.2001.23371. [DOI] [PubMed] [Google Scholar]
- 19.Reston JT, Turkelson CM. Meta-analysis of surgical treatments for temporomandibular articular disorders. J Oral Maxillofac Surg. 2003;61:3–10. doi: 10.1053/joms.2003.50000. [DOI] [PubMed] [Google Scholar]
- 20.Giraddi GD, Siddaraju A, Kumar B, Singh C. Internal derangement of temporomandibular joint: an evaluation of effect of corticosteroid injection compared with injection of sodium hyaluronate after arthrocentesis. J Maxillofac Oral Surg. 2012;11(3):258–260. doi: 10.1007/s12663-011-0324-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kopp S, Wenneberg B, Haraldson T, Carlsson GE. The short-term effect of intra-articular injections of sodium hyaluronate and corticosteroid on temporomandibular joint pain and dysfunction. J Oral Maxillofac Surg. 1985;43(6):429–435. doi: 10.1016/S0278-2391(85)80050-1. [DOI] [PubMed] [Google Scholar]
- 22.Kopp S, Carlsson GE, Haraldson T, Wenneberg B. Long-term effect of intra-articular injections of sodium hyaluronate and corticosteroid on temporomandibular joint arthritis. J Oral Maxillofac Surg. 1987;45(11):929–935. doi: 10.1016/0278-2391(87)90443-5. [DOI] [PubMed] [Google Scholar]
- 23.Pavan Kumar B, Chari H, et al. A clinical study of efficacy of hydrocortisone compared with hyaluronic acid after arthrocentesis in TMJ disorders. Dent Issue. 2016;8(3):141–147. [Google Scholar]
- 24.Pereda CA, Uson JJ, Carmona L (2006) Systematic revision: is it advisable to use botulinum toxin as a treatment of pain in Myofascial syndrome? Rheumatol Clin 2(4):173–182 [DOI] [PubMed]
- 25.Kreger ST, Voytik-Harbin SL. Hyaluronan concentration within a 3D collagen matrix modulates matrix viscoelasticity, but not fibroblast response. Matrix Biol. 2009;28(6):336–346. doi: 10.1016/j.matbio.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghosh P, Guidolin D. Potential mechanism of action of intra-articular hyaluronan therapy in osteoarthritis: are the effects molecular weight dependent? Semin Arthritis Rheum. 2002;32:10–37. doi: 10.1053/sarh.2002.33720. [DOI] [PubMed] [Google Scholar]
- 27.Pelletier JP, Martel-Pelletier J. The pathophysiology of osteoarthritis and the implication of the use of hyaluronan and hylan as therapeutic agents in visco supplementation. J Rheumatol Suppl. 1993;39:19–24. [PubMed] [Google Scholar]
- 28.Schiavinato A, Lini E, Guidolin D, et al. Intraarticular sodium hyaluronate injections in the Pond-Nuki experimental model of osteoarthritis in dogs. II: Morphological findings. Clin Orthop Relat Res. 1989;241:286–299. [PubMed] [Google Scholar]
- 29.Grishko V, Xu M, Ho R, et al. Effects of hyaluronic acid on mitochondrial function and mitochondria-driven apoptosis following oxidative stress in human chondrocytes. J Biol Chem. 2009;284(14):9132–9139. doi: 10.1074/jbc.M804178200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Takahashi K, Hashimoto S, Kubo T, et al. Effect of hyaluronan on chondrocyte apoptosis and nitric oxide production in experimentally induced osteoarthritis. J Rheumatol. 2000;27(7):1713–1720. [PubMed] [Google Scholar]
- 31.Guarda-Nardini L, Stifano M, Brombin C, Salmaso L, Manfredini D. A one-year case series of arthrocentesis with hyaluronic acid injections for temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(6):14–22. doi: 10.1016/j.tripleo.2006.12.021. [DOI] [PubMed] [Google Scholar]
- 32.Nitzan DW. Arthrocentesis—incentives for using this minimally invasive approach for temporomandibular disorders. Oral Maxillofac Surg Clin N Am. 2006;18(3):311–328. doi: 10.1016/j.coms.2006.03.005. [DOI] [PubMed] [Google Scholar]