Abstract
To study the age & sex distribution, etiology, formulate most suitable management protocol and evaluate the results of our study and compare our data with similarly published studies to look for any changing trends. All the patients presenting with epistaxis who came to our institute, a tertiary care centre of central India were included in the study. The diagnostic confirmation was done with clinical along with radiological and endoscopic evaluation. Various parameters categorized accordingly. Total 304 patients were included in the study. Epistaxis was found prevalent in 1st to 3rd decade, more common in males, frequently seen in cold, anterior epistaxis more common. Trauma and infection being more common in children and young adults, whereas hypertension in the elderly. Although the treatment of epistaxis hasn’t change much, we found cauterization to be a very efficient and effective method to control epistaxis and required less hospitalization.
Keywords: Epistaxis, Nose bleed, Etiology, Trauma, Management
Introduction
According to Stedman’s medical dictionary, ‘epistaxis’ term means ‘bleeding from the nose’ in which, ‘epi’ means ‘on’ and ‘stazo’ means ‘to fall in drops’ [1]. Although this definition is so simple but it becomes most difficult to treat when it comes as an emergency to an otorhinolaryngologist. There are many references to epistaxis in our literature of history. The most unique thing about epistaxis is that it can be treated just by pinching the ala nasi which is known as the Hippocratic method [2].
Epistaxis is one of the most commonly encountered hemorrhages to an ENT surgeon. About 60% of the public have episode of nasal bleed once in their lifetime while only 6% comes to hospital to get treatment [3].It is perhaps one of the most common cause of emergency admission into the ENT department.
It affects all age groups and has two peaks in the age of onset of epistaxis. The condition is common in childhood, becomes less common in early adult life and then peaks in the sixth decade. Children are mainly susceptible to nose bleed due to the rich vascular supply to the nasal mucosa and since they develop more upper respiratory tract infections [4].
Most of the epistaxis patients get relieved just by observation and medical management and do not require admission. The study was done to study the pattern and changing trends in occurrence and management of epistaxis.
Material and Methods
This Observational/Cross Sectional study has been carried out on all patients who presented with epistaxis at a tertiary care hospital of Central India from Nov 2017 to April 2019. A total of 304 patients of both sexes & all age group were taken into the study. Epistaxis resulting from recent septal or paranasal sinus surgery (within 3 weeks) & patients’ not giving consent for the study were excluded.
Before including in the study, each patient was explained about need and purpose of study; and ascent & consent for study was taken as per standard guidelines. All patients with epistaxis at our hospital were evaluated by taking detailed history followed by general and ENT examination followed by diagnostic and treatment evaluation. In cases of mild epistaxis and stable patient, detailed history was noted along with management of the bleeding. In case of severe bleeding, history was taken after the control of bleeding.
Patients were subjected to investigations of hematological baseline parameters (haemoglobin, bleeding time, clotting time, platelet count, blood grouping and cross matching etc.). Diagnosis was based on detail clinical history, physical findings and laboratory investigations with examination of the nose and nasopharynx by nasal endoscopy. This whole data was collected in a performa and data analyzed.
Observation
Total study patients taken were 304, out of which 210 (69.08%) were male and 94 (30.92%) were female. The male to female ratio was found to be 2.23. maximum number of patients with epistaxis were of age group 21–30 years i.e. 66 (21.71%) and least number of patients were of age group 71–80 years and 81–90 years i.e. 1 (0.33%). In this study, patients of age group, 0–30 years consists of 62.5% of patients of epistaxis. We found maximum patients of epistaxis in summer season i.e. 143 (47.04%) followed by winter i.e. 104 (34.21%) and least in monsoon i.e. 20 (6.58%).
Maximum patients according to involvement of type of nasal bleed were having anterior epistaxis i.e. 277 (91.12%) as compared to posterior epistaxis which were only 27 (8.88%) (Fig. 1). According to etiology found in patients of epistaxis, maximum patients were of nose picking i.e. 113 (37.17%) followed by trauma via accident, assault and fall i.e. 77 (25.33%) followed by hypertension i.e. 49 (16.12%) (Table 1).
Fig. 1.
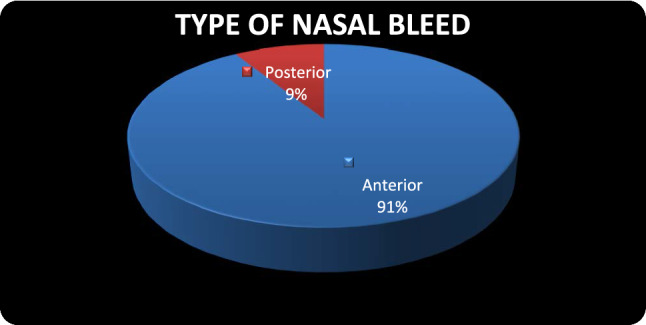
Type of nasal bleed
Table 1.
Etiologies of epistaxis
| Etiology | Number of patients | Percentage |
|---|---|---|
| Local | ||
| Nose picking | 113 | 37.17% |
| RTA/assualt/fall | 77 | 25.33% |
| Foreign body | 21 | 6.91% |
| Maggots | 5 | 1.64% |
| DNS with spur | 2 | 0.66% |
| Infections | 12 | 3.85% |
| Neoplasms | 2 | 0.66% |
| Hypertension | 49 | 16.12% |
| Infections | 6 | 1.97% |
| Bleeding disorders | 3 | 0.99% |
| Drugs | 2 | 0.66% |
| Chronic alcohol/liver failure | 2 | 0.66% |
| Vicarious menstruation | 1 | 0.33% |
| Idiopathic | 9 | 2.96% |
| Total | 304 | 100.00% |
In this study, maximum patients i.e. 250 (82.23%) had good recovery after observation with medical management or spontaneously stopped (Table 2). in 22 patients we had to do cautery which was found to be very effective and efficient and these patients required less hospitalization.
Table 2.
Methods of management of epistaxis performed
| Treatment | Total |
|---|---|
| Spontaneously stopped/Observation with medical management | 267 |
| Anterior nasal packing | 6 |
| Posterior nasal packing | 1 |
| Cautery | 22 |
| Septoplasty/FESS | 2 |
| Nasal bone fracture reduction | 3 |
| Surgical excision of mass / tumor | 2 |
| > 1 procedure | 1 |
| Total | 304 |
Discussion
In our study, total patients taken were 304, out of which 210 (69.08%) were male and 94 (30.92%) were female. According to Hussain G et al.’s study on 313 patients, epistaxis was found 2 times more common in males as compared to females which is favourable to our study in which male to female ratio was 2.23 approximately just double and similar to this study [5]. Juselies [6] has also stated that males are little more commonly affected as compared to females which are almost similar to our study.
In present study, out of 304 participants, mean age of epistaxis found in our study was 26.5 years, maximum number of patients with epistaxis were of age group 21–30 years i.e. 66 (21.71%) and least number of patients were of age group 71–80 years and 81–90 years i.e. 1 (0.33%).
In this study, maximum bulks of patients were within the age group of 0–30 years, which consists of 62.5% of patients of epistaxis. Juselies [6] also noted higher incidence of epistaxis in older age groups as they found more cases of hypertension which is in contrast to our study. Hussain G et al. also found epistaxis in all age groups as most common emergency. They found two peaks in age group i.e. young and adult although in our study maximum were in age group 21–30 years and comparatively less in adult group [5].
In this study, we found maximum patients of epistaxis in summer season i.e. 143 (47.04%) followed by winter i.e. 104 (34.21%) and least in monsoon i.e. 20 (6.58%). This is supported by study which was conducted by Leena Jain [7] (2015), which showed more cases of epistaxis in summer season (50%).
According to type of nasal bleed, maximum patients were having anterior epistaxis i.e. 277 (91.12%) as compared to posterior epistaxis which was found in only 27 (8.88%). Similar findings were also seen in study of Juselius H. [6], Emanuel J M. [8]
According to etiology found in patients of epistaxis, maximum patients were of nose picking i.e. 113 (37.17%) followed by trauma via accident, assault and fall i.e. 77 (25.33%), followed by hypertension i.e. 49 (16.12%). Findings were supported by Hara [9] who found that primary trauma to nose causes epistaxis in 32.5% cases, Petruson [4] (1974) reported in 28.5% cases, Razdan U, Zada R [10] also found finger nail trauma as commonest cause (75.9%) of epistaxis.
Out of total 304 patients, maximum patients i.e. 287 (94.41%) got relieved by observation with medical management or spontaneously stopped, while in 6 patients anterior nasal packing done, in 3 patients nasal bone fracture reduction done and in 2 patients cautery with chemical done, in 2 patients septoplasty/FESS done, in 2 patients surgical excision of mass done while in only 1 patient posterior nasal packing done and in 1 patient more than 1 procedure used. Findings of our study supported by study of Urvashi et al [11] and Phillip et al [12] which shows most of the cases treated by medical or conservative treatment.
Conclusion
Epistaxis is a common clinical condition encountered by the otorhinolaryngologist. It is prevalent in the 1st to 3rd decade. It is found to be more common in males than females. It occurs frequently in cold and dry climate. Anterior epistaxis is more common than posterior. Common causes of epistaxis are trauma & hypertension. Trauma and infection being more common in children and young adults, whereas hypertension in the elderly. Although the treatment of epistaxis hasn’t change much, we found cauterization to be a very efficient and effective method to control epistaxis and these patients required less hospitalization.
Funding
This study was not funded by anyone.
Compliance with Ethical Standards
Conflict of interest
Sandeep Sharma declares that he has no conflict of interest. Sadat Qureshi declares that he has no conflict of interest. Shalini Jadia declares that she has no conflict of interest. Lavi Ukawat declares that she has no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.The American Heritage (2002) Stedman’s medical dictionary. Houghton Miffin Company, Boston
- 2.Mcgarry GW. Epistaxis. In: Gleeson M, editor. Scott-Brown’s otorhinolaryngology, head and neck surgery. 7. London: CRC Press; 2008. pp. 1603–1608. [Google Scholar]
- 3.Simmen DB, Jones NS, Cummings CW, Flint PW, Harker LA. Epistaxis. Otolaryngol Head Neck Surg. 2005;5:682–693. [Google Scholar]
- 4.Petruson B. Epistaxis in childhood. Rhinology. 1979;17:83–90. [PubMed] [Google Scholar]
- 5.Hussain G, Iqbal M, Shah SA, Said M, Sanaulla KSA, et al. Evaluation of aetiology and efficacy of management protocol of epistaxis. J Ayyub Med College Abbottabad. 2006;18(4):62–65. [PubMed] [Google Scholar]
- 6.Juselius H. Epistaxis: a clinical study of 1724 patients. J Laryngol Otol. 1974;88:317–327. doi: 10.1017/S0022215100078749. [DOI] [PubMed] [Google Scholar]
- 7.Jain L, Qureshi S, Maurya A, Jadia S, Mrityunjay S. Hand dominance and blood group: association in Epistaxis. Indian J Otolaryngol Head Neck Surg. 2017;69(1):121–124. doi: 10.1007/s12070-015-0934-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Emanuel JM. Epistaxis. Otolaryngol Head Neck Surg. 1998;2:852–865. [Google Scholar]
- 9.Hara J. Severe Epistaxis. Arch Otolaryngol. 1962;7S:258. doi: 10.1001/archotol.1962.00740040266016. [DOI] [PubMed] [Google Scholar]
- 10.Razdan U, Zada R, Chaturvedi VN. Epistaxis: study of aetiology, site and side of bleeding. Indian J Med Sci. 1999;53(12):1545–1552. [PubMed] [Google Scholar]
- 11.Razdan U, Raizada RM. Efficacy of conservative treatment modalities used in epistaxis. Indian J Otolaryngol Head Neck Surg. 2004;56(1):20–23. doi: 10.1007/BF02968765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pollice PA, Yude MG. A retrospective review of 249 hospitalised patients with epistaxis. AJO Head Neck Surg. 1997;1997:49–53. doi: 10.1016/S0194-5998(97)70205-5. [DOI] [PubMed] [Google Scholar]


