Abstract
During the last years probiotics gained the attention of clinicians for their use in the prevention and treatment of multiple diseases. Probiotics main mechanisms of action include enhanced mucosal barrier function, direct antagonism with pathogens, inhibition of bacterial adherence and invasion capacity in the intestinal epithelium, boosting of the immune system and regulation of the central nervous system. It is accepted that there is a mutual communication between the gut microbiota and the liver, the so-called “microbiota-gut-liver axis” as well as a reciprocal communication between the intestinal microbiota and the central nervous system through the “microbiota-gut-brain axis.” Moreover, recently the “gut-lung axis” in bacterial and viral infections is considerably discussed for bacterial and viral infections, as the intestinal microbiota amplifies the alveolar macrophage activity having a protective role in the host defense against pneumonia. The importance of the normal human intestinal microbiota is recognized in the preservation of health. Disease states such as, infections, autoimmune conditions, allergy and other may occur when the intestinal balance is disturbed. Probiotics seem to be a promising approach to prevent and even reduce the symptoms of such clinical states as an adjuvant therapy by preserving the balance of the normal intestinal microbiota and improving the immune system. The present review states globally all different disorders in which probiotics can be given. To date, Stronger data in favor of their clinical use are provided in the prevention of gastrointestinal disorders, antibiotic-associated diarrhea, allergy and respiratory infections. We hereby discuss the role of probiotics in the reduction of the respiratory infection symptoms and we focus on the possibility to use them as an adjuvant to the therapeutic approach of the pandemic COVID-19. Nevertheless, it is accepted by the scientific community that more clinical studies should be undertaken in large samples of diseased populations so that the assessment of their therapeutic potential provide us with strong evidence for their efficacy and safety in clinical use.
Keywords: probiotics, medicine, intestine, COVID-19, lung, allergy, Lactobacillus, Bifidobacterium
Probiotics are living non-pathogenic microorganisms, which when given in sufficient amounts (at least 106 viable CFU/g) should be beneficial to host by improving its microbial balance in gut and participate in the metabolism (1).
Moreover, probiotics are known to have particular properties such as; resistance to acid pH, bile tolerance, tolerance to pancreatic fluid, adhesion and invasion capacity in the intestinal epithelial cells (2). The above properties permit their survival in the gastrointestinal tract and the improvement of the intestinal balance (2).
During the past years, the use of probiotic microorganisms has been applied to modulate the microbiome in a beneficial way and thus fighting against infections threatening human and animal health (3). Their use might sometimes be an alternative to antibiotics permitting to reduce antimicrobial resistance due to the overuse or misuse of antibiotics against infections (4, 5). Spreading of antibiotic resistance is a major public health problem among human pathogens (4). The development of antibiotic resistance through different mechanisms may result in unsuccessful treatment of infectious diseases.
Nevertheless, neither the FDA, more the EFSA have approved the use of probiotics for preventing or treating health issues, despite their classification as safe food supplements (6, 7). Both authorities have punctuated the faulty characterization and health claims, the scarcity of an efficient explanation of their mechanism of action as well as the failing of considerable studies in humans to really show a benefit of the probiotics' administration.
The Japanese Ministry of Health and Welfare seems to have a different policy. FOSHU label (Food for Specified Health Use) is given to a specific probiotic product allowing health claims (8).
Lactobacillus and Bifidobacterium genera are principally reported as probiotics. These bacterial genera are isolated in the human intestine in considerable populations. Lactobacillus includes different species with the most semantic as probiotics; L. acidophilus, L. rhamnosus, L. bulgaricus, L. reuteri, L. casei, L. johnsonii, L. pantarum. These strains are acid-tolerant in the stomach acidity and have a good adherence capacity to the intestinal cells. Bifidobacterium belong to the phylum of Actinobacteria as they have a characteristic ramified morphology. The most common Bifidobacterium probiotic species are B. animalis, B. bifidum, B. breve, B. infantis, B. lactis, B. longum.
Streptococcus thermophilus, Enterococcus faecalis, Enterococcus faecium, Pediococcus, and several Bacilli, as well as the yeasts Saccharomyces boulardii and Saccharomyces cerevisiae also show some probiotic properties.
Probiotic microorganisms are part of our intestinal flora, yet they can also be found in other ecological environments. However, it must be clear that probiotic properties are strain-related and even tissue-dependent. Thus, the probiotic effect neither universal to all bacterial species nor to all human tissues.
Early intestinal colonization seems to provide protection against certain diseases by strengthening our immune system (1). Until now, it is not known which bacterial species are necessary to induce an appropriate and effective “barrier effect” against pathogens, but it seems that this “barrier effect” can be strongly supported by providing beneficial food supplements called probiotics (3). Specifically, through this type of diet a beneficial microbiota dominated by Lactobacilli (phylum of Firmicutes) and Bifidobacteria (phylum of Actinobacteria) is registered (9).
International Scientific Association for Probiotics and Prebiotics (2014) (8) declared that metabolic by-products, bacterial molecular components and dead microorganisms might have some beneficial effect; despite the real conviction that a probiotic must have a high ability to survive under intestinal conditions (acidic pH, enzymes, bile salts, etc.) and that their activity and effectiveness are linked to viability (10). Currently, the term “postbiotic” is developed for soluble bacterial components with biological activities which are believed to be safer than the use of whole bacteria (11).
Multiple studies on the probiotic strains' characteristics have been done, including biochemical profile, adherence and invasion capacities to intestinal cells (12). Moreover, pharmacokinetic studies (half - life time, intestinal permeability, correlation of the obtained dose and persistence in stools) have been reported (13) as well as studies on the tolerance of the probiotic strain by the host and its input on the bacterial microflora (14). All the above tests and studies have permitted to characterize by the Food and Drug Administration (FDA) (USA) a probiotic given strain under the acronym of “GRAS” (Generally Recognized As Safe), meaning a food supplement which is considered safe by experts (6).
The bacterial colonization of newborns by vaginal delivery or cesarean section has been thoroughly studied in relation to the immune system, the diet, the environment as well as many other involved factors (1). Hospital staff, personal habits, infections, stress, hormonal status, vaccination and agedness seem to be crucial factors for the establishment of the bacterial microflora which is actually called “microbiome” (1).
New technological applications have been brought into light. Next generation sequencing (NGS) methodologies include sequencing of the 16S ribosomal RNA gene (r RNA) as well as metagenomic sequencing. Without any doubt technological developments have empowered scientists with advanced knowledge and stand for an in depth perception of the human ecological communities of commensal, symbiotic and pathogenic microorganisms. Microbes are able to participate in multiple metabolic processes in our intestine, synthetizing and producing key nutrients as well as repulsing pathogenic bacteria. To this end, the “Human Microbiome Project” in the United States (US National Institutes of Health, NIH, http://commonfund.nih.gov/hmp/) (15) and the metaHIT Consortium (https://www.gutmicrobiotaforhealth.com/metahit/) in Europe (16) have been able to shed light on the composition of bacterial populations in detail at the various human sites.
Without any doubt, diet is the major player of the microbiota composition. Diet consists of introducing chemical substances following consumption preferences in our intestinal ecosystem in different timing (17, 18). On another hand, host physiology, immunological status and metabolism capacity regulate the response to the bacterial colonization and the presence of specific microbial species (1).
The Gut-associated lymphoid tissue (GALT) system sits in the intestinal wall furnished by immunological elements able to protect the intestinal wall from invasion. Malfunction of the GALT following treatment by antibiotics, inappropriate alimentation or stress leads to dysbiosis and increasing of the intestinal permeability (1, 19). GALT malfunction results in an impaired immunity, either inefficient or exacerbated. Therefore, infectious diseases as well as immune-mediated diseases (20, 21) such as allergy (22) and auto-immune (inflammatory) disorders (23–25) may occurred following disruption of the equilibrium between microbiota and host, the so-called dysbiosis. Along these lines, probiotics seem to be beneficial in these issues as they stimulate the host immune system and preserve the microbial intestinal balance via the barrier effect (1).
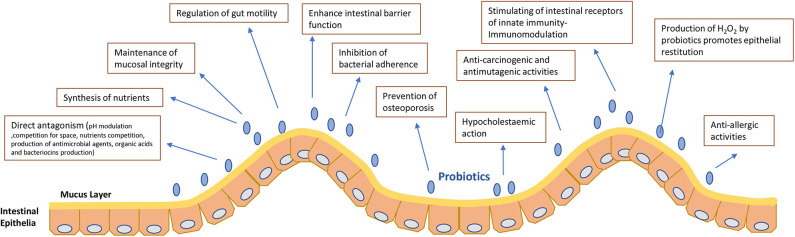
Probiotics seem to exert their effect through different mechanisms (1, 20) (Figure 1);
Figure 1.
Mechanisms of action and properties of probiotics.
- Competition for space (Spatial arrangement theory) in the intestinal lumen and wall (26, 27).
- Antagonism between pathogenic bacteria and probiotics which is produced by competition for nutrients found in limited quantities in the intestine (26) or by pH modulation. Maintenance of an acid pH on the epithelium by probiotics (27, 28).
- Synthesis of nutrients reported as sources for energy for epithelial cells or bacteria (26).
- Maintenance of mucosal integrity. The intestinal epithelium is part of the intestinal mucosa layer. This epithelium is monolayer and the locus in between the epithelial cells is tightly unified by transmembranar proteins. The intestinal mucosa has 2 more layers, the lamina propria and the muscularis mucosae, which bracket the epithelial monolayer. Probiotics show a cytoprotective action upon the gastric mucosa integrity by strengthening the epithelial junctions and preserving the mucosal barrier function (29).
-Enhance intestinal barrier function. Preservation of the microbial intestinal balance via the barrier effect (1).
- Regulation of gut motility (30). Intestinal motility as well as reflexes and secretory functions of the gastrointestinal tract are regulated by the Enteric Nervous System (ENS) found in the intestinal wall. ENS is considered as a second brain as it is composed of a complex neural network of sensory, motor, inter neurons and glial cells. In this vein, there is a reciprocal communication between Central Nervous System (CNS) and bacterial flora in the intestine. The CNS affects the microbiota by altering the motility and permeability of the gut or even via mediators secreted by neuro-endocrine cells (30).
- Prevention of osteoporosis. Studies showed that probiotic supplementation can both increase bone density and protect against primary (estrogen-deficiency) and secondary osteoporosis (31).
- Hypocholestaemic action (32). Hypocholestaemic effect is bacterial species related. Different mechanisms have been proposed. Deconjugation of bile acids (30), assimilation of endogenous or exogenous cholesterol (33), binding of cholesterol and free bile acids to the microbial cell (34) or co-precipitation of the free bile acids (34).
- Anti-carcinogenic, antimutagenic and anti-allergic activities (35–37). Studies in animals as well as cohort studies in humans have demonstrated a correlation between consumption of dairy products and the risk of colorectal cancer. Anticancer activity of some strains is associated to the capacity of the probiotic strain to inhibit or reduce DNA destruction in the very first stages of carcinogenesis.
- Production of H2O2 by probiotics promotes epithelial restitution (38).
- Production of antimicrobial agents, organic acids and bacteriocins (39–41) stimulates the production of intestinal mucins which will prevent the implantation of pathogens.
- Their action on the intestinal immune system (1, 42) by stimulating the receptors of innate immunity, TLRs which will cause the production of pro-inflammatory cytokines and lead to the initiation of phagocytosis by macrophages.
Specifically, some probiotics induce activation of CD4 + and CD8 + T lymphocytes and secretion of IgA by lamina propria plasma cells to neutralize pathogens, while other probiotics suppress the Th1 inflammatory response and the production of inflammatory cytokines IL-12, TNF-a, and stimulate Treg lymphocytes (39). Therefore, they appear to have a multifaceted role as an adjuvant to immunity or as a stifle of inflammatory responses.
Undoubtedly antibiotics play a crucial role in the treatment of infections, however their uncontrollable use has led to serious ecological consequences but also for human health, as for example the increase of multi-resistant strains and the alteration of human floras and specifically of the intestinal microbiota and its functions (5). In this vein, probiotics have been proposed as a “non-invasive” alternative therapy or co-therapy to antibiotics. As already stated, probiotics help to preserve the normal human microbiota in a beneficial status.
According to WHO, probiotics are “living microorganisms, which, when consumed in adequate amounts, have a health benefit for the host.” Historically, Metchnikoff was the first scientist to propose the use of probiotics. They may be used as food supplements to consume or as medicines in the form of pills or powder containing a single or a combination of several strains. It is generally accepted that the dose of probiotic microorganisms must be 100 million to 10 billion microorganisms for it to be effective.
Gastrointestinal Diseases
Without any doubt, the strongest evidence supporting the use of probiotics is related to the treatment of gastrointestinal diseases and specifically the acute diarrhea.
Gastroenteritis
Probiotics are of scientific interest for intestinal pathology. Their effects are reported in multiple clinical studies (Table 1).
Table 1.
Use of probiotics in gastrointestinal disorders.
| Disease state | Probiotic | References |
|---|---|---|
| Gastroenteritis | -Lactobacillus | (43) |
| -Lactobacillus F19 and L. reuteri | (44, 45) | |
| -L. casei (431strain) | (45, 46) | |
| -S. thermophilus and B. bifidum (TH-4+ BB12 strain) | (46, 47) | |
| -L. acidophilus (NCFM strain) + B. lactis (Bi-07 strain) | (48) | |
| Antibiotic associated diarrhea and traveler's diarrhea | -Lactobacillus GG, E. faecium (SF68 strain) and S. boulardii | (49, 50) |
| - Saccharomyces cerevisiae variant boulardii CNCM I-1079 | (51, 52) | |
| -Lactobacillus Rosell-52, Bifidobacterium Rosell-175 and Lactobacillus Rosell-11 | (51, 52) | |
| -L. reuteri DSM 17938 and L acidophilus LB (low efficacy) | (53) | |
| Clostridioides difficile infection | -S. boulardii, Lactobacillus spp. | (54–58) |
| Inflammatory bowel disease | -Escherichia coli Nissle 1917 or Lactobacillus GG | (59–63) |
| -Bifidobacterium spp. and L. acidophilus | (59–63) | |
| -S. boulardii | (64) | |
| -Lactobacillus GG and L. johnsonii | (65) | |
| Celiac disease | -Bifidobacterium spp. and L. acidophilus, various | (59–63, 66) |
| Helicobacter pylori infection | -Bifidobacterium BB-12 | (67) |
| -L. acidophilus La-5 | (13) | |
| Lactose Intolerance | -Lactobacillus delbrueckii subspecies bulgaricus and S. thermophilus | (68) |
Some strains of E. coli, as well as Salmonella spp., Shigella spp., Campylobacter spp. and viruses like Rotavirus, Norovirus etc are among the most frequent causes of gastroenteritis leading to inflammation of the intestine. Lactobacillus strains are the main players of the commercially available probiotics. Lactobacillus strains have been shown to be effective against the pathogens E. coli and C. difficile (43).
Specifically, Lactobacillus F19 and L. reuteri have a positive impact on the gastrointestinal microbiota by boosting the immunological status (44, 45). Similarly, Lactobacillus casei (431strain) is boosting the immune response and contributes on the faster convalescence of the diarrheal disease in children (45, 46). Streptococcus thermophilus and Bifidobacterium bifidum (TH-4+ BB12 strain) drop the risk of the Rotavirus diarrhea and colic's in children (46, 47). Lactobacillus acidophilus (NCFM strain) + Bifidobacterium lactis (Bi-07 strain) have a beneficial effect on the gastrointestinal ecosystem by reducing abdominal floating (48).
Antibiotic Associated Diarrhea and Traveler's Diarrhea
Lactobacillus GG, Enterococcus faecium (SF68 strain), and Saccharomyces boulardii have a strong recommendation for the prevention of antibiotic-associated diarrhea, the treatment of C. difficile colitis, as well as treatment of gastroenteritis in addition to oral rehydration therapy (49, 50) (Table 1). Saccharomyces cerevisiae variant boulardii CNCM I-1079 has been given successfully to treat and prevent acute cases of antibiotic-associated diarrhea and traveler's diarrhea as described (51, 52). The same authors (51, 52) observed that Lactobacillus Rosell-52, Bifidobacterium Rosell-175 and Lactobacillus Rosell-11 strains were able to prevent pathogen invasion and treat traveler's diarrhea.
Nevertheless, studies have shown that a Lactobacillus acidophilus commercial strain acquired vancomycin resistance of vanA genes from enterococci in the gastrointestinal tract of germ-free mice in vitro and in vivo (69).
Similarly, we should note that the SF68 strain of Enterococcus faecium is a possible recipient of the van A gene cluster (70). Thus, Enterococcus faecium SF68 strain profile has led to concerns about the safety of probiotics containing this strain (70).
Those studies underpin the issue of the potential health risk when consuming probiotic foods containing enterococci which could be potential recipient of glycopeptide resistance genes (70).
Following EFSA and the Panel on Additives and Products or Substances used in Animal Feed (FEEDAP) (2008), Microbial Inhibition Concentration(MIC) antimicrobials standards have been designated for most common probiotics; Lactobacillus, Streptococcus thermophilus, Pediococcus, Lactococcus, Leuconostoc, Enterococcus, Bifidobacterium, Propionibacterium, and Bacillus.
More studies bring into light that the glycopeptide resistance of Lactobacillus strains is different from Enterococci and underline the safety of Lactobacillus strains used as probiotics with regard to their vancomycin resistance (71).
L. reuteri DSM 17938 and L. acidophilus LB have a lower recommendation (53). In a Cochrane's study (72), the efficacy of probiotics on acute infectious diarrhea in subjects of all ages was studied and a reduction in the duration of diarrhea by 1 day was demonstrated. There is no doubt that the evidence is weak and the methodological limits are questionable.
Clostridioides difficile (Formerly Clostridium) Infection Pseudomembranous Colitis
As aforementioned, probiotics can be given as part of the treatment of Clostridium difficile colitis (Table 1). We focus our interest in this part during the last years; we notice an increase of C. difficile cases worldwide, associated to the misuse of antibiotics (54). The effect of administering probiotics on a Clostridium difficile has been evaluated in several studies with questionable results (73). A Swiss study finds that the action of probiotics depends on the basic risk of patients (>5%) of developing post-antibiotic pseudomembranous colitis (55, 74, 75).
C. difficile infection is a cause of post-antibiotic nosocomial diarrhea, the so called pseudomembranous colitis. The infection is due to gut microbiota alterations as a result of antibiotic treatment or other causes of microbiome alterations such as travel (76).
Clostridioides difficile and its spores are ubiquitous in the environment and thus are able to colonize the human intestine (74). The intestinal mucus appeared to be an important chemotactic factor for colon colonization by Clostridium difficile (55). Recently, the epidemics observed of Clostridium difficile seem to be linked to extremely virulent clones of this anaerobic bacterium in several countries; the genotypes 027 and 078 (77, 78). The infection could induce a toxic megacolon and lead to intestinal perforation and septic shock (73). In Switzerland, the disease is not obligatory reportable and only the clone 078 has been isolated (74, 75).
In a European global study on hospital strains, the ribotype 078 was the 11th most frequent ribotype in Europe. Of all 14 European countries enrolled in this study, Greece represented >10% of the strains with the virulent ribotype 078 (54). Moreover, in Greece, the hypervirulent genotype 027 has not been found, whereas genotypes 017 and 126 predominate (79). In Spain, the genotypes 078 and 126 predominate in patients (80). Globally in Southern Europe (Greece, Italy, Portugal and Spain), the genotypes 078 and 126 and 017 are the most common dominating genotypes (77). The genotype 017 is also found in Bulgaria and Poland (79).
It is of note that most patients having Clostridium difficile infection have been exposed to longterm antibiotics suffer from comorbidities and are elderly. It seems that the prevalence of the disease is closely associated to the abuse of antibiotics, specifically fluoroquinolones, cephalosporins as well as penicillins (78). Yet, most of the cases are hospital acquired (64%) compared to the community acquired cases (79).
The European Society of Clinical Microbiology and Infection (ESCMID) (2009) issued treatment guidance for Clostridium difficile infection (73), reviewing different treatment protocols such as antibiotics, immunotherapy, toxin-binding resins and polymers, probiotics, and fecal or bacterial intestinal transplantation. Guidelines are specified following disease state. Recommended antibiotics, are mostly vancomycin and fidaxomicin and less metronidazole than it used to be. In cases of recurrences fecal transplantation is recommended in combination with oral antibiotic treatment. Probiotics (Saccharomyces boulardii, Lactobacillus spp.) are also given in combination with oral antibiotic treatment (54, 56–58).
Probiotics (Saccharomyces boulardii, Lactobacillus spp.) can also be given in combination with oral antibiotic treatment (55).
Although several studies showed a moderate evidence on the beneficial effect of probiotic prophylaxis in C. difficile diarrhea (56, 57), a Cochrane study analysis suggests to adjunct them to the antibiotic therapy in the treatment of CDI (58). However, a study on the use of Saccharomyces boulardii in immunocompromised patients showed occurrence of invasive disease (81, 82). Another study on probiotic use as prophylaxis agent showed increased mortality due to non-occlusive mesenteric ischemia (83).
Therefore, the ESCMID guidelines do not recommend probiotics as an adjunctive treatment for CDI.
In consent with the European guidelines, the Infectious Diseases Society of America (IDSA) together with the Society for Healthcare Epidemiology of America (SHEA) issued similar guidelines summarizing that due to lack of evidence probiotics are not recommended (84).
Inflammatory Bowel Disease
Probiotics seem to have an effect on inflammatory bowel disease (85, 86) (Table 1). Studies on colitis animal models show a decrease in inflammatory status and the expression of inflammatory mediators.
Administration studies of the various probiotics remain differentiated in terms of treatment effectiveness. While some authors report that there is no difference in the relapse rate but simply a longer interval without relapse for the treatment of ulcerative colitis with probiotics such as Escherichia coli Nissle 1917 or Lactobacillus GG, others accept that supplementation of medical treatment with Bifidobacterium spp. and L. acidophilus improves clinical response (59–63). In addition, remission seems to be observed in pediatric subjects after long-term probiotic treatment as a supplement to medical treatment with mesalazine (87). Administration of S. boulardii in combination with mesalazine shows a considerable positive effect. Probiotics have also been applied in the treatment of Crohn's disease (64). Fewer recurrences were observed after administration of Lactobacillus GG and Lactobacillus johnsonii (65).
Pouchitis is the inflammation in the lining of a pouch as a result of colorectal surgery. In this context, some researchers have used probiotics for the treatment of active pouchitis inducing remission in 69% of subjects (65, 88), while other authors doubt the efficacy of probiotics on the treatment of pouchitis (66).
Celiac Disease
To date, it is well known that gluten is the trigger in celiac disease. Nevertheless, it is suggested that intestinal microbiota might play a certain role in the pathogenesis and progression of the disease (66). Dysbiosis in the microbiota of patients with celiac disease has been reported in some studies with an intestinal microflora characterized by an abundance of Bacteroides spp. and a decrease in Bifidobacterium spp. (66). This could suggest that probiotics might have a beneficial effect on this condition (Table 1).
Other Intestinal Associated Pathology
Intake of Bifidobacterium BB-12 has an impact on Helicobacter pylori infection in humans (67). Likewise, L. acidophilus La-5 also impacts Helicobacter pylori, boosts the immune effect and alleviate diarrheal symptoms (13) (Table 1).
Treatment of Lactose Intolerance
Lactose intolerance is due to the inability to digest lactose in dairy products. It is believed to affect 60% of the world's population (89). However, lactose malabsorption varies considerably in the different countries from 5 to 15% in Northern Europe and America to 50–100% in South America, Asia and Africa. Lactobacillus delbrueckii subspecies bulgaricus and S. thermophilus in yogurts improve the intolerance to lactose as they possess the enzyme beta- galactosidase (68) (Table 1). Recently, randomized double-blind studies showed the efficiency of probiotic bacteria in fermented and unfermented milk preparations given to alleviate the clinical symptoms of lactose malabsorption (89).
Allergy
Allergy results from an exacerbated hypersensitivity response of the immune system to usually harmless triggering substances in the environment. These substances are called allergens and they usually include drugs, foods, grass and tree pollen, insects, insect's bites and stings, dust mites, pet dander, chemicals and latex.
This hypersensitivity in immune system tolerance mechanisms seems to be modulated by the gut microbiota (90). Dysbiosis has been incriminated for the development of allergies (91). Probiotics have been successfully used in the treatment of allergic diseases such as allergic rhinitis, asthma, atopic dermatitis and food allergy (90). However, there is still controversy over their use.
Two meta-analyses reported improvement in the prevention of atopic dermatitis by the use of probiotics (92, 93). Lactobacillus alone and Lactobacillus along with Bifidobacterium seem to be protective against the development of atopic dermatitis, specifically when given early in pre- and postnatal high allergy risk populations as well as in the general population (93) (Table 2).
Table 2.
Use of probiotics in allergy.
| Disease state | Probiotic | References |
|---|---|---|
| Atopic dermatitis | -Lactobacillus | (93) |
| -Lactobacillus + Bifidobacterium | (93) | |
| -L. paracasei | (94, 95) | |
| -L. salivarius (LS01) | (94, 95) | |
| -L. fermentum | (94, 95) | |
| Allergic rhinitis | -L. casei, L. rhamnosus, L. johnsonii EM1, L. acidophilus, L. gasseri, L. paracasei | (96–99) |
| - B. lactis NCC2818 (Nestle) | (100) | |
| -L. paracasei (LP-33 strain) | (101) | |
| -Lactobacillus GG (LGG) + L. gasseri, L. acidophilus+ Bifidobacterium lactis | (102–104) | |
| - VSL#3 (4 Lactobacillus+3 Bifidobacterium+ 1 Streptococcus thermophiles) | (102–104) | |
| -Lactobacillus+Bifidobacterium | (105) | |
| -L. casei | (106) | |
| Atopic eczema | -Bifidobacterium BB-12 | (90, 107, 108) |
| -B. longum, B. clausii,E. coli Nissle (EcN) 1917 | (90, 107, 108) |
Lactobacillus paracasei, Lactobacillus salivarius (LS01 strain), and Lactobacillus fermentum are also used for the treatment of atopic dermatitis as antiallergic in children (94, 95). The use of probiotics in allergic conditions such as atopic dermatitis is promising (109).
Initially treatment was succeeded with a single probiotic strain. Among Lactobacillus species the most common in the therapy of allergic rhinitis are; Lactobacillus casei, Lactobacillus rhamnosus, Lactobacillus johnsonii EM1, Lactobacillus acidophilus, Lactobacillus gasseri, Lactobacillus paracasei (96–99).
As stated previously, Bifidobacterium BB-12 alleviate symptomatology of the atopic eczema.
Bifidobacterium longum, Bacillus clausii, and Escherichia coli Nissle (EcN) 1917 are also used as pharmatherapeutics (107, 108).
The use of Bifidobacterium lactis NCC2818 (Nestle) as well as Lactobacillus paracasei (LP-33 strain) seems to reduce the severity of the symptoms of allergic rhinitis (100, 101).
Recently, combination treatment was made possible with more than one probiotic strains. Lactobacillus GG (LGG) + L. gasseri, L. acidophilus + Bifidobacterium lactis and also the commercial mixture VSL#3 consisting of 4 lactobacilli+3 bifidobacteria+ 1 Streptococcus thermophilus were used combined (102–104).
The combination of Lactobacillus + Bifidobacterium in treatment seems to be the most popular and successful for the allergic rhinitis (105).
Lactobacillus casei administered in children with mite allergies decreased the frequency and severity of symptoms (106).
Studies on the role of probiotics in prevention or treatment of food allergies were conducted but with contradictory results (90, 110). Heterogeneity of strains, duration and dosage of treatment should probably explain some of the differences.
Respiratory Diseases
Asthma
A raise in asthma and respiratory diseases has been observed during the last years in most industrialized countries (111).
As formerly discussed, the gut microbiota plays a capital role in the development of allergic diseases.
The modulation of the normal gut microbiota in an experimental model of asthma in animals has been registered (112). Children at risk of asthma showed microbial dysbiosis in their intestine with complete absence of certain bacterial genera (112). Hence, the administration of these “missing bacteria” in models of mice showed a decline in respiratory tract inflammation indicating their potential role as a causal agent in asthma (112). Recently, there appeared evidence that Enterococcus faecalis FK-23 suppresses the asthmatic hypersensibility which seems to be associated with attenuation of Th17 cell development (113) (Table 3).
Table 3.
Use of probiotics in respiratory diseases.
However, meta-analyses and double-blind randomized controlled studies did not perceive any substantial benefit from probiotic treatments (122–124).
Cystic Fibrosis
Cystic fibrosis is an autosomal recessive disorder caused by a mutation in the CF transmembrane conductance regulator (CFTR) gene encoding the CFTR protein which regulates the movement of chloride and sodium ions across epithelial cell membranes. The result is a defective ion transport with a buildup of thick mucus throughout the body, leading to respiratory insufficiency, along with many other systemic disorders, mostly digestive. Moreover, the decreased mucociliary clearance in the respiratory tract, combined to the defective ion transport allows the proliferation of Pseudomonas aeruginosa as well as other pathogens in the respiratory tract which become more and more resistant due to iterative treatments and result in a repetitive inflammatory response (114).
Other than chronic respiratory disease, cystic fibrosis is associated, as aforementioned with digestive disorders (pancreatic, biliary and intestinal) also resulting in chronic inflammation as well as malabsorption of nutritious substances.
Probiotics seem to be promising for certain respiratory tract diseases including cystic fibrosis (115) (Table 3). In the case of cystic fibrosis there is a dysbiosis and frequent antibiotic therapy is able to unbalance the microbiota (116). In this context, the use of probiotics has been studied as it appears that they may reduce the rate of pulmonary exacerbations in the disease (117, 118).
Respiratory Infections and COVID-19
L. rhamnosus GG reduces the risk of respiratory and gastrointestinal infections in infants (119).
Viral respiratory infections affect morbidity and mortality of a population. Pattern recognition receptors (PRRs) are the main sensor players of the innate immune response. Expression of many Pattern Recognition Receptors (RRs) is exacerbated in the lung cells during inflammation. In this vein, macrophages, monocytes, neutrophils are responding by increasing levels of PAMPs (Pathogen-Associated Molecular patterns) and DAMPs (Danger-Associated Molecular Patterns) (125).
It is known that intruder's pathogens have a specific unique profile of PAMPs resulting in a specific immune response (126). PAMPs are necessary molecules for the pathogens survival; hence they are not produced by the host. In viruses, the major PAMPs are nucleic acids or glycoproteins. PAMPs should be recognized by PRRs conducting to the expression of cytokines, chemokines, and other co-stimulatory molecules in order to eliminate the pathogenic virus and activating then antigen presenting cells and specific adaptive immunity (127, 128). The most studied PRRs for pathogens recognition are TLRs (Toll Like Receptors) which are membrane glycoproteins (129).
Without any doubt, there is a clear diversity in the patterns for pathogen recognition and host protection upon viral infections.
On the other side, PRRs recognize DAMPs (Danger-Associated Molecular Patterns) as danger signals released by damaged or necrotic host cells which reinforce the pro-inflammatory response (130). As a result, stimulation of TLRs is crucial for the protection from the development of diseases.
Probiotics' regulatory effect on the expression of Toll-like receptors (TLRs) was observed in several disease cases (131). Specifically, probiotics impede or reduce inflammation by minimizing the expression of TLR4 (132). In this vein, a large randomized controlled trial was conducted (PROSPECT Investigators and the Canadian Critical Care Trials Group) for the use of probiotics in critically ill patients of intensive care units (ICU) with ventilator-associated pneumonia (VAP) showing beneficial and salutary effects of probiotics in this seriously ill patients (133).
Although, it has long been known that Coronaviruses cause respiratory and sometimes gastrointestinal diseases with mostly like clinical presentations, the SARS-CoV-2 has recently monopolized our interest due to the COVID-19 pandemic as a result of its contagiousness as well as unexpected mortality rates.
Coronaviruses are recognizably different than most enveloped viruses in nature as they are localized in the lumen of the ERGIC (ER-Golgi intermediate compartment). The ERGIC mediates between the endoplasmic reticulum and the Golgi on the secretory pathway for releasing of the infectious virions from the infected cell (134). This is where the majority of the E protein is localized, participating in the assembly and budding of the infectious virion.
It is known that virus replication in the host for establishment of an infection occurs through host-viral PPIs (Protein-protein interactions) (135, 136). In SARS-CoV-1, The E protein has only been mentioned to connect to five host proteins (Bcl-xL, PALS1, syntenin, sodium/potassium (Na+/K+) ATPase α-1 subunit, and stomatin) (135).
Latest information states that Coronaviruses encode PBM-containing proteins that bind to cellular PDZ proteins. Those proteins keep an important role in the anchoring receptor proteins (135). Alongside, E protein interaction partners are identified as p38 mitogen-activated protein kinase (MAPK) inhibitors. Clearly, this is an important therapeutic tool as studies have shown that inhibitors of p38 mitogen-activated protein kinase (MAPK) prolonged survival in mice (137, 138).
Lactobacillus contains a HSP27-inducible polyphosphate (poly P) fraction. Probiotic-deriving polyphosphates have the ability to strengthen the epithelial barrier function and keep intestinal homeostasis through the integrin-p38 MAPK pathway (139).
As most treatments targeting Coronaviruses are currently ineffective, bringing into light more interaction partners for Coronavirus protein E could enhance a therapeutic approach.
L. reuteri DSM 17938 showed beneficial effects against upper respiratory tract and gastrointestinal symptomatology (120).
Similarly, L. reuteri ATCC 55730 has been shown to alleviate respiratory tract and gastrointestinal symptomatology in workers in Sweden (121).
During the last years, the gut–lung axis in bacterial and viral infections is considerably discussed (140). It seems that intestinal microbiota amplifies the alveolar macrophage function (140) and as a result, gut microbiota acts as a protective mediator during pneumonia (141).
We state here the importance to clarify the involved mechanisms of the probiotic efficiency in respiratory diseases which could potentialize their use as prophylactic or field therapy.
In conclusion, more knowledge is necessary to define the role of probiotics as therapeutics in viral and other respiratory diseases, as we have as yet only scratched the tip of this complicated issue.
Neurological and Psychiatric Diseases
During the last years, there is increasing interest in the use of probiotics for prevention and treatment of neurologic diseases (Table 4). Recent studies stated the potential role for microbiota in the pathogenesis of neurological and brain disorders (150–152).
Table 4.
Use of probiotics in neurological and psychiatric diseases.
It is believed that there is reciprocal communication between the central nervous system and the intestine, the so-called “microbiota-gut-brain axis” (150, 152). which is a model of interaction between the intestinal microflora and the brain.
Physical and psychological stress may interfere in the control of the intestinal and the vaginal microflora. Higher numbers of the putrefactive bacteria Clostridium sp are found under stress (153, 154).
Early-life events such as stress, environmental factors or other may impact the intestinal microbiota (155).
Studies report that the ingestion of Lactobacillus rhamnosus regulated the transcription of γ-aminobutyric acid (GABA) receptors and therefore emotional behavior (154). The intestinal microbiota affect GABA which transmit signals to the brain trough enteric nerve s (142).
Normal microbiota preserves the intestinal balance by improving epithelial tight junctions reducing gut permeability (150). Otherwise, in case of cellular damage, multiple immune and inflammatory responses are produced as well as activation of the spinal neurons and the vagus nerve (156). As a result, inflammatory cytokines are produced affecting the central nervous system (156).
Autism spectrum disorder (ASD) is a developmental disability that can cause problematic behavior in social, emotional, and communication skills. It seems that there is a connection between gut bacteria and autism (145, 146).
Taking the above into account, we understand the pivotal role of the gut microbiota in the neural and brain development and regulation and general and mental health affection in case of imbalance. Maternal feeding plays an important role in gut microbiota of the newborn (1), as it contains probiotics.
Studies showed potential effects of probiotics in the treatment of neurologic diseases (143) (Table 4).
Positive effect of probiotics have been observed in the progression of the autoimmune myasthenia gravis (148), the autoimmune encephalomyelitis (149), as well as on motor behaviors (144). Moreover, probiotics seem to have neuroprotective properties (157) and a positive impact on cognition (158).
Improvement of the antisocial behavior, communication and concentration problems was observed in a cohort study of children with ASD treated with the probiotic strain L. acidophilus Rosell-11 during a period of 2 months (147).
Probiotics have been studied in the treatment of the above neurological diseases. However, the current evidence on their efficacy is poor. As already discussed, their efficiency is strain, tissue, and dose dependent.
Studies undertaken are not uniform in terms of the chosen characteristics of the population, the population size, the undertaken therapies and procedures and the suitable strain or strains' mixture.
Rare cases of adverse effects of probiotics have been observed (159). It is also notable to state that immaturity of the neurological system, mental retardation and other severe neurodevelopmental problems predispose those patients at potentially higher risk of adverse effects.
Without any doubt, when the mechanisms of action of the probiotics are completely understood, we would then be able to evaluate their safety and efficiency issues on neurological diseases (140).
Liver Diseases and Hepatic Encephalopathy
There is mutual communication between the central nervous system and the liver, the so-called “microbiota-gut-liver axis.” Thereby, there is a reciprocal interaction between hepatic receptors (Toll-like receptors) and bacterial lipopolysaccharides. When intestinal imbalance occurs prompting the alteration of the intestinal permeability, immune and inflammatory responses are produced and can result in hepatic disorders. Moreover, nutrients absorbed by the gut reach the liver.
Cirrhosis seems to be associated with changes in the presence of Bifidobacterium species in the intestinal microbiota (160).
Moreover, modifications of the intestinal microbiota have been observed among patients with chronic hepatitis B (161), primary sclerosing cholangitis (160) and proliferation of hepatocellular carcinoma (161). There was diversity observed in intestinal microbiota amongst subjects with hepatitis B virus-related cirrhosis and subjects with chronic hepatitis B (160, 161).
Hepatic encephalopathy is closely related to the intestinal microbiota (162). The metabolic activity of the intestinal microbiota on amino-acids results in the production of toxic substances (NH3, phenols, amines, phenolic acids) that are inactivated in the liver. However, when liver failure occurs these substances are not inactivated, they enter the circulation, cross the hematoencephalic barrier and cause hepatic encephalopathy resulting in coma.
The mainstay of treatment of hepatic encephalopathy is lactulose and lactitol, laxative agents that can be considered as prebiotics as they lower blood ammonia concentrations, possibly by favoring colonization with acid-resistant, non-urease producing bacteria. Moreover, they also act by altering the colonic pH, improving gastrointestinal transit and increasing fecal nitrogen excretion (163).
In this same spirit, probiotics have also been proposed as an adjunctive treatment for hepatic encephalopathy.
Lactic acid bacilli, more specifically Lactobacilli and Bifidobacteria seem to be the most effective species for hepatic encephalopathy but Clostridium butyricum, Escherichia coli Nissle 1917, Streptococcus salivarius, and Saccharomyces boulardii are also used (164) (Table 5).
Table 5.
Use of probiotics in Liver diseases.
Treatment with the probiotics Clostridium butyricum and Bifidobacterium infantis seems to be promising as an adjuvant therapy for the management of the mild hepatic encephalopathy (162, 165).
According to a meta-analysis of 21 trials, when compared to placebo/no treatment, probiotics seem to be beneficial in treatment of hepatic encephalopathy but do not seem superior compared to lactulose (165).
Other than the treatment of hepatic encephalopathy, probiotics have also been studied as prophylaxis to prevent recurrence with beneficial effects (166).
Based on the fact that changes in gut microbiota are inducing liver diseases, an increasing interest in regulating the gut microbiota by probiotics for the treatment of liver disorders is reported (167). However, the current evidence on this efficacy is unclear. As stated previously, the efficiency of a probiotic is strictly strain, tissue, and dose dependent.
It is necessary to proceed to high-quality randomized clinical trials with standardized procedures on the undertaken probiotic therapy with appropriate strains and diligent choice of the population size and characteristics in order to get knowledge on the efficacy and safety of probiotics. In these terms, probiotics cannot be recommended for the treatment of most hepatic disorders, aside from some implication on hepatic encephalopathy.
Genito-Urinary Infections
Bacterial vaginosis is a vaginal inflammation caused by an imbalance of the vaginal flora with overgrowth of several bacterial species and decrease in Lactobacilli. It seems that women at reproductive age develop more frequently vaginosis.
Historically, Albert and Döderlein in 1892 stated the importance of the vaginal flora in women's overall health (168).
Lactobacillus spp. and specifically the species L. crispatus are predominant in the bacterial flora of healthy women (169). As known, Lactobacillus spp produce lactic acid protecting the vagina from colonization by pathogens. However, when the balance is disturbed and Lactobacillus are decreasing or missing vaginosis occurs.
In this vein, scientists have tried to restore this imbalance of the vaginal flora by oral or vaginal administration of lactobacilli (170, 171) (Table 6).
Table 6.
Use of probiotics in Genito-Urinary tract infections.
| Disease state | Probiotic | References |
|---|---|---|
| Bacterial vaginosis | -Lactobacillus spp. | (169) |
| -L. crispatus | (169) | |
| -L. acidophilus | (170, 171) | |
| -L. rhamnosus GR-1 | (170, 171) | |
| -L. fermentum RC-14 | (170, 171) | |
| Gardnerella vaginalis | -Lactobacillus spp. | (172) |
| -L. acidophilus | (172) | |
| Urinary tract infections (UTIs) | -Lactobacillus rhamnosus GR-1 | (173) |
| -L. reuteri RC-14 | (173) | |
| -L. casei Shirota | (173) | |
| -L. crispatus CTV-05 | (173–175) | |
| -L. rhamnosus GG | (173) |
L. acidophilus seems to have a positive effect in prevention and treatment of bacterial vaginosis (171, 176).
However, the mechanism of action of Lactobacillus remains unclear. While some scientists claim that the production of lactic acid inhibits the establishment of pathogens by creating an acid environment (1), in vitro studies have stated that the production of H2O2 or bacteriocins by certain Lactobacillus protects against pathogens involved in bacterial vaginosis (176, 177). Thus, the adherence of Gardnerella vaginalis to the vaginal epithelium is inhibited by Lactobacillus strains (172). Studies have shown that the bacteriostatic effect of L. acidophilus on G. vaginalis NCTC 11292 dropped by 60% when culture pH turned to alkaline by the addition of NaOH or by catalase denaturation of the H2O2 (172) (Table 6).
Moreover, it seems that administration of L. acidophilus or Lactobacillus rhamnosus GR-1 and Lactobacillus fermentum RC-14 for an extended period of 2 months is beneficial in the vaginosis treatment (170, 171).
In conclusion, probiotics can be effective in preventing and treating vaginal imbalance in bacterial vaginosis. Studies undertaken are encouraging. More research and clinical studies are necessary in order to define whether or not probiotics are efficient for the prevention and treatment of vaginosis and which strains should be involved.
Urinary tract infections (UTIs) are among the most common infections. Shortness of the women urethra is associated with more frequent urinary tract infections in women. They are divided in uncomplicated and complicated and include cystitis, pyelonephritis, febrile UTIs, prostatitis and urinary-source bacteriemia. UTIs mostly result when uropathogens, mostly from the fecal flora, ascend the urinary tract or from seeding of the kidneys via bacteremia or following medical interventions (urinary catheters, urological surgery). Clinical presentations vary from asymptomatic bacteriuria to urethritis, cystitis, prostatitis, pyelonephritis and bacteriemia.
UTIs are associated with an important economic impact due to many hospitalisations as well as morbidity, mortality and most importantly development of microbial resistance (178–180).
Development of multi-drug resistance has led doctors to look for milder prophylactic therapies in order to minimize the high cost of therapies (181).
Probiotic effects on urinary tract infections remain controversial (181–183) (Table 6). While a team states that there is no benefit from probiotics administration (182), other scientists observe a shortening of the average duration of illness, as well as a considerable reduction of the infection rate (181, 184).
An extended review based on a search of PubMed for relevant articles showed the efficacy and safety of probiotics as prophylaxis against potential pathogenic bacteria of the urinary tract (185). Lactobacillus rhamnosus GR-1 and L. reuteri RC-14 seemed to be the most effective probiotic strains followed by L. casei Shirota and L. crispatus CTV-05 (185). The effectivity of L. crispatus in UTIs has been observed by many authors (186, 187).
On the contrary, L. rhamnosus GG is not shown to be sufficiently effective (185). It seems that probiotics' activity and efficiency is closely related to the specific administered strain. Hence, all authors agree on the safety issue of their use (185).
Metabolic Syndrome and Cardiovascular Diseases
Diabetes
The gut microbiome seems to play a role in the development of diabetes. Studies in animals have shown that some species of Lactobacillus and Bifidobacterium could prevent or reduce the severity of type 2 diabetes (188) (Table 7).
Table 7.
Use of probiotics in metabolic syndrome and cardiovascular diseases.
Studies in humans have attempted to assess the factors that justify metabolic changes, oxidative stress and inflammation (188).
Lactic acid bacteria show antioxidant activity. Diabetic subjects are characterized by constant systematic inflammation with high levels of proinflammatory cytokines [TNF-a, IL-6, b kinase inhibitor (IKKb), and Jun N-terminal kinase (JNK)] which exert a negative effect on insulin. Lactic acid bacteria have positive clinical effects on the treatment of specific populations with type 2 diabetes by modulating the inflammatory status.
A meta-analysis of 12 randomized controlled trials showed that probiotics considerably improved the fasting plasma glucose (FPG) and the glycosylated hemoglobin (HbA1c) in type 2 diabetes (189). Similarly, the role of probiotic supplementation in persons developing type 2 Diabetes Mellitus (T2DM) in improving glycemic control showed an overall beneficial effect (190).
Our body is exposed to different physico-chemical or pathological conditions having as outcomes the production of free radicals (ROS) which causes the oxidation in the human cell. Hence, it has developed endogenous antioxidant mechanisms to keep the homeostasis. Oxidative stress is occurring when imbalance between free radicals (ROS) and antioxidant mechanisms are taking place (193). In the case of diabetes, disorders in lipid peroxidation, enzymatic systems as well as impaired glutathione metabolism are observed.
Pathogenesis of diabetes is then characterized by a potent oxidative stress, as increased levels of reactive oxygen species (ROS) are present (194).
The consumption of yogurt with live probiotics seems to touch up the antioxidant status and fasting plasma glucose (FPG) levels in type 2 diabetic patients (191).
Obesity
The significance of the human gastrointestinal microbiota is stated in the case of obesity as well.
Obesity is linked to structural and functional changes in the gastrointestinal ecosystem. The intestinal microbiota of obese patients is characterized by increased numbers of bacteria of the phylum of Bacteroidetes. Low numbers of bacteria of the phylum of Firmicutes are observed.
Diversity and abundance of certain bacterial populations can trigger metabolic pathways leading to obesity (173).
Obesity is an important risk factor for type 2 Diabetes mellitus and cardiovascular diseases due to the high levels of inflammation mediators which (39) are recorded in obese persons. Administration of probiotics and antibiotics - has been used to stimulate weight gain in farm animals (3, 40). However, there is controversy in their efficacy by authors (174).
In humans, probiotics supplementation seems to decrease values of metabolic parameters and leads to the reducing of the weight gain in obese adults (175) (Table 7).
Lactobacillus spp. are associated with weight gain in children treated for diarrhea (195). Without any doubt more research is needed for estimating the role of probiotics in obesity.
Cardiovascular Disease and Cholesterol
Cardiovascular diseases are a pivotal cause of death in the western world.
Multiple studies in animal and humans have demonstrated an important correlation between cholesterol levels and the risk of coronary heart disease. Dietary interventions suggest lowering of fat (low-saturated-fat diets) for the prevention of cardiovascular disease.
Supplementation of diet with fermented dairy products containing lactic acid bacteria seems to be in lowering blood cholesterol alleviating the cardiovascular disease (Table 7).
In this context, Bifidobacterium spp. and Lactobacillus spp. have been studied as food supplements with very promising effects.
However, the mechanisms of action of the antihypercholesterolemic potential of probiotics are yet under study. Several scientists propose a cellular pattern, which includes the binding of cholesterol to cellular surfaces and/or cholesterol assimilation by growing cells and cholesterol incorporation into the cellular membrane (196). Others rather accept a chemical pattern which comprises the deconjugation of bile via bile salt hydrolase, the coprecipitation of cholesterol with deconjugated bile (192) or the production of short-chain fatty acids by oligosaccharides (41).
Cancer
Gastrointestinal (GI) cancers are a major health problem, accounting for 20% of all cancers and 9% of all causes of cancer death in the world (197).
The role of the human intestinal microflora has been extensively discussed in cancer disorders. Microbiota imbalance seems to be linked to cancer. One of the most representative examples is the correlation between S. bovis/S. equinus complex infection and intestinal cancer, principally colorectal (198).
Functional foods and probiotics seem to have a protective role against cancer development (Table 8) and also reduce the incidence of the post-operative inflammations (206).
Table 8.
Use of probiotics in cancer and cancer cellular lines.
| Disease state | Probiotic | References |
|---|---|---|
| Tumor cell apoptosis | -L. casei | (199) |
| -B. longum | (199) | |
| -L. acidophilus | (199) | |
| Inhibition of human colon cancer cell lines including HT-29, SW 480, Caco-2 | B. adolescentis SPM0212 | (200) |
| Anti-proliferative and pro-apoptotic effects in human gastric cancer cells and colonic cancer cells | -L. paracasei IMPC2.1 | (201) |
| - L. rhamnosus GG | (201) | |
| -L. acidophilus 606 | (202) | |
| - LGG/Bifidobacteriumanimalis subsp. lactis | (203) | |
| Antitumor activities | -Bacillus polyfermenticus | (204) |
| -L. acidophilus NCFB 1748 | (205) |
As shown by some investigators, probiotics possess anti-proliferative and pro-apoptotic properties against gastrointestinal cancers (207, 208) (Table 8).
Similarly, milk fermented with Lactobacillus casei, Bifidobacterium longum, and L. acidophilus showed beneficial effects on tumor cell apoptosis (199).
Moreover, in cellular lines it has been observed that Bifidobacterium adolescentis SPM0212 inhibited the proliferation of three human colon cancer cell lines including HT-29, SW 480, and Caco-2 (200) (Table 8).
Anti-proliferative and pro-apoptotic effects of Lactobacillus paracasei IMPC2.1 and L. rhamnosus GG strain have been observed in both human gastric cancer cells and colonic cancer cells (201) (Table 8).
Furthermore, antitumor activities have been shown by Bacillus polyfermenticus (204).
In addition, L. acidophilus 606 (202), and LGG/Bifidobacterium animalis subsp. lactis (203) have also shown activity against human colon cancer cells.
L. casei Shirota is reported to prevent intestinal dysbiosis and having an effect on bladder cancer by lowering fecal enzyme activity (205). Lowering of fecal enzyme activity has also been observed by L. acidophilus NCFB 1748 which decreases cancer risk and radiotherapy-related diarrhea (205).
Nevertheless, most of the above studies were performed in vitro, in cellular lines or in animal models displaying the efficiency of probiotics in gastrointestinal cancers. As stated previously, those studies ascribe in probiotics properties such as, anti-carcinogenic effect, anti-mutagenic effect, derangement in differentiation process in tumor cells, modifications of tumor gene-expressions, inhibition of pro-carcinogenic bacteria and improvement of the immune system and intestinal balance (206).
However, the mechanisms inducing these effects are not completely understood. It is of paramount interest to expand these studies in humans with specific clinical trials which could strengthen our knowledge of the potential probiotic strain related efficiency and safety, as well as of the administration procedure and dosage for the different types and stages of cancer (206).
Osteoporosis
Human and animal studies indicated that probiotic supplementation may be a therapeutic tool to the prevention and treatment of bone loss as they strengthen bones and skeleton (31). Moreover, probiotics protect against primary estrogen-deficiency and secondary osteoporosis (31) (Table 9).
Table 9.
Use of probiotics in osteoporosis.
| Disease state | Probiotic | References |
|---|---|---|
| Osteoporosis | -Various | (31) |
Oral Diseases
Gingivitis is an inflammation confined to the gingiva, while in periodontitis the inflammation process affects all peridental tissues and the alveolar bone.
P. gingivalis, A. actinomycetemcomitans, T. forsythia, Staphylococcus intermedius, Candida albicans, and T. denticola are the main pathogens associated to periodontitis.
Lactobacillus salivarius WB21 modulates the oral microbiota and reduces risk of gingivitis and periodontitis (209) (Table 10). Chewing gums or lozenges with probiotics can improve periodontal disease (214).
Table 10.
Use of probiotics in oral diseases.
Dental caries is tooth decay due to acids made by bacteria. Following excess of sucrose, Streptococcus mutans found in the oral cavity are able to adhere to the teeth enamel causing demineralization of the tooth enamel. Probiotics can reduce levels of Streptococcus mutans. It is reported that systematic yogurt and fermented by Lactobacillus reuteri bovine milk consumption for 2 weeks reduces Streptococcus mutans population in the oral cavity by up to 80%(210) (Table 10). Moreover, fluid or lozenges containing probiotics reduce Streptococcus mutans levels (211).
Halitosis (Chronic bad breathing) is the unpleasant breath odor attributed to the production of volatile sulfur compounds especially during the mornings due to poor oral hygiene or dental caries, periodontitis and other oral conditions. Reduction of the volatile sulfur compounds is observed by H2O2 produced by probiotics. Additionally, probiotics compete for colonization in the oral cavity (212) (Table 10).
Lastly, oral candidiasis (oral trush) is an opportunistic mycosis, due to colonization of the mucous membranes of the oral cavity mostly by C. albicans on the mucous membranes of the oral cavity. Candidiasis occurs when the normal oral microbiota balance is disturbed in immunocomprised patients, elderly or patients receiving long antibiotic regimens. L. rhamnosus GG seems to reduce the prevalence of C. albicans which is a normal component of our oral microbiota (213) (Table 10).
Autoimmune Diseases
Dysbiosis is linked to the pathogenesis of Sjogren's autoimmune syndrome (215) as a possible interaction between the human microbiome and the clinical manifestations of the disease seems to exist. All the same, if the human microbiome is revealed to play a key role in the pathogenesis of Sjogren's disease (215), the next step could be new and promising therapeutic approaches such as the administration of probiotics as an adjunctive treatment to immunosuppressive therapy (Table 11).
Table 11.
Use of probiotics in autoimmune diseases.
Randomized controlled trials have shown promising results in modulating beneficially human microbiota in autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus and multiple sclerosis (23, 216) (Table 11).
Vaccine Adjuvant
Lactobacillus casei 431 was used for boosting the immune response and Lactobacillus fermentum strain VRI 003 (PCC) as an adjuvant to flu vaccine and athletic endurance (217, 218) (Table 12).
Table 12.
Use of probiotics as vaccine adjuvant.
Probiotics were shown effective in increasing immunogenicity levels by auctioning upon seroconversion and seroprotection rates in adults inoculated with Influenza vaccines (219) (Table 12).
Discussion
The normal microbiota of the intestine plays a very important role in the body's defenses (1) and in the occurrence of multiple diseases such as, infections, autoimmune and allergic diseases and other (218–222). Probiotics seem to be a modern approach to prevent and reduce the symptoms of these diseases or as an adjuvant therapy by maintaining the proper balance of our intestinal microbiota (114).
A plethora of commercial products with differences in strain(s) composition and potentiality have been developed as probiotics and functional foods; Align B. infantis (4 mg/capsule 1 billion CFU), Activia yogurt (B. lactis; 100 million bacteria per gr), Culturelle (L. rhamnosus GG (L. rhamnosus:10 billion bacteria plus insulin 200 mg per capsule), Culturelle for kids (L. rhamnosus:1.5 billion bacteria per packet), Florajen (L. acidophilus: 20 billion bacteria per capsule), Florastor S. boulardii lyo: 250 mg per capsule), Howaru (L. acidophilus/B. lactis: 10 billion bacteria per capsule), Kefir (L. lactis. L. rhamnosus, L. plantarum, L. casei, L. acidophilus, L. reuteri, Leuconostoc cremoris, Streptococcus diacetylactis, S. florentinus, B. longum, B. breve, B. lactis: 7–10 billion CFU per cup), Lactinex (L. acidophilus, L. bulgaricus: 106 CFU/tablet and 109 CFU/packet), RepHresh Pro-B (L. rhamnosus, L. reuteri: 5 billion CFU per capsule; vaginal use),VSL#3 (L. acidophilus, L. plantarum, L. paracasei, L. bulgaricus, B. breve, B. infantis, B. longum, S. thermophilus: 225 billion bacteria per 2 capsules), Yakult (L. casei: 8 billion bacteria per 80 mL bottle), Ultralevure (Saccharomyces boulardii CNCM I-745: 250,00 mg, 50 mg/cap) (223).
Adverse effects (224) of probiotics have been reported such as abdominal cramps, loose stools, bloating, gas and flatulence.
Moreover, as probiotics are “living organisms,” their use is not recommended in immunocompromised patients, such as those receiving corticosteroid therapy and other immunosuppressive treatment, transplanted and oncological patients especially those undergoing chemotherapy. Besides, probiotic treatment is not recommended in patients with prosthetic valves as there have been reports of infective endocarditis due to probiotics (225).
It is also important to have a deep understanding of the role of CYP enzymes (226). CYP enzymes represent a superfamily of enzymes that play an important role in the process of activating or inactivating a plethora of therapeutic agents. The high metabolic rate of the gut microbiome is due to the many enzymes that catalyze reactions in the metabolism of drugs. This high enzymatic activity of the intestinal microflora is linked to the presence of P450 in the main bacterial strains from the human fecal microbiota. The fact that many intestinal bacterial strains have CYP enzymes (P450), arises the question that if living probiotics express P450 activity it could possibly influence the metabolism of drugs and their bioavailability? (226).
In addition, if the intestinal barrier is disrupted (226–228), this metabolism is affected. Undoubtedly, the role of probiotics is to restore deficiencies and imbalance in the intestinal microbiome and to establish a protective effect. Albeit that, the high enzymatic activity of the intestinal microbiota as well as the action of probiotics on the intestinal microbiome remain to be clarified. It is obvious that future trials should focus on clarifying the multifactorial association of the role of the cytochromes CYP (P450) in the various disease states, environmental toxic effects or chemical exposures and nutritional status. It also worth to mention once more that the effectiveness of a probiotics is strictly dependent on the strain and the dose received.
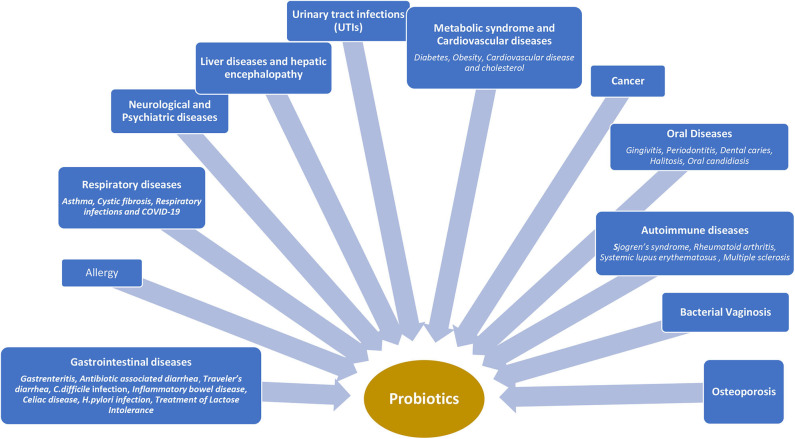
Probiotics have a beneficial impact on the immune system by stimulating non-specific immune response, improving several disease states and alleviating allergies (Figure 2).
Figure 2.
Clinical use of probiotics in different disease states.
As it is well known, pathogens induce a pro-inflammatory response in epithelial cells by activating transcription factor activating transcription Nuclear Factor-κB (NF-kB) which keeps a crucial role in immunity, inflammation, and cell proliferation. There is evidence that probiotic strains have an effect on epithelial immune activation by blocking this factor (229).
Administration of probiotics improves the immune system in multiple ways; stimulated production of natural antibodies IgM and IgG levels systemically, increased IgA antibodies locally and systemically as well as interferon (230) and increased phagocytosis ability which modulate cytokines presence (231). In this spirit, probiotics have shown immunostimulatory effects that may be associated to the initial inflammation following human macrophages response (231).
It is emphasized that early intestinal colonization with probiotic microorganisms such as Lactobacilli and Bifidobacteria offers subsequent protection from many different types of diseases. In addition, the beneficial probiotic microflora dominated by Bifidobacteria and Lactobacilli could modify the gut microbiota by reducing the risk of cancer following their capacity to decrease β-glucoronidase and carcinogen levels (37).
Moreover, probiotics are able to produce antimicrobial substances,bacteriocins and lower the pH in order to inhibit pathogens (232), compete for nutrients with pathogens and finally enhance the intestinal barrier function (1, 224).
The integrity of the intestinal barrier is a hallmark of a healthy intestinal ecosystem (233). As discussed many factors are contributing to this issue.
A variety of in vitro and animal studies implied the significance of the human microbiota and the improvement of the mucosal barrier function by probiotic treatment (3, 234).
In spite of the aforementioned, there are difficulties to extrapolate results of these studies to human populations.
Multiple clinical trials have been conducted so as to evaluate the prophylactic and therapeutic effect of probiotics in different diseases and states, especially in infections after the failure of multiple courses of antibiotics.
At this point, we underpin that it is catalytic that more clinical studies should be undertaken in a large sample of diseased populations in order to evaluate the probiotics therapeutic potential. Selection criteria, efficacy and safety issues of probiotics should be considered as well as the fact that the probiotic ability seems to be strain-dependent.
In this review, we tried to summarize current knowledge on probiotics' application and therapeutic potential in different disease states and despite their possible benefits, the lack of sufficient evidence for their efficacy and safety profile makes the probiotic use a long-lasting debate.
Author Contributions
ES focuses on all clinical aspects. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Bezirtzoglou E, Stavropoulou E. Immunology and probiotic impact of the newborn and young children intestinal microflora. Anaerobe. (2011) 17:369–74. 10.1016/j.anaerobe.2011.03.010 [DOI] [PubMed] [Google Scholar]
- 2.Vassos D, Bezirtzoglou E, Voidarou C, Alexopoulos A, Maipa V. Biochemical and antimicrobial profile of Enterococcusfaecium and E. faecalis isolated from traditional dairy products and infant intestinal microbiota. Microbial Ecol Health Dis. (2009) 21:241–50. 10.3109/08910600903495095 [DOI] [Google Scholar]
- 3.Fuller R. Probiotics in man and animals. J Appl Bacteriol. (1989) 66:365–78. 10.1111/j.1365-2672.1989.tb05105.x [DOI] [PubMed] [Google Scholar]
- 4.Bezirtzoglou E, Alexopoulos A, Voidarou C. Apparent antibiotic misuse in environmental ecosystems and food. Microb Ecol Health Dis. (2008) 20:197–8. 10.1080/08910600802408103 [DOI] [Google Scholar]
- 5.Stavropoulou E, Tsigalou C, Bezirtzoglou E. Spreading of antimicrobial resistance across clinical borders. Erciyes Med J. (2019) 41:238–43. 10.14744/etd.2019.99075 [DOI] [Google Scholar]
- 6.FDA Dietary Supplements New Dietary Ingredient Notifications and Related Issues: Guidance for Industry. (2016). Available online at: http://www.fda.gov/downloads/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/UCM515733.pdf (accessed October 10, 2017).
- 7.EFSA Guidance on the scientific requirements for health claims related to the immune system the gastrointestinal tract and defence against pathogenic microorganisms EFSA J. (2016) 14:4369 10.2903/j.efsa.2016.4369 [DOI] [Google Scholar]
- 8.Mercenier A, Pavan S, Pot B. Probiotics as biotherapeutic agents: present knowledge and future prospects. Curr Pharm Des. (2002) 9:175–91. 10.2174/1381612033392224 [DOI] [PubMed] [Google Scholar]
- 9.Bezirtzoglou E, Tsiotsias A, Welling GW. Microbiota profile in feces of breast- and formula-fed newborns by using fluorescence in situ hybridization (FISH). Anaerobe. (2011) 17:478–82. 10.1016/j.anaerobe.2011.03.009 [DOI] [PubMed] [Google Scholar]
- 10.Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, et al. Expert consensus document; The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. (2014) 11:506–14. 10.1038/nrgastro.2014.66 [DOI] [PubMed] [Google Scholar]
- 11.Tsilingiri K, Barbosa T, Penna G, Caprioli F, Sonzogni A, Viale G, et al. Probiotic and postbiotic activity in health and disease: comparison on a novel polarised ex-vivo organ culture model. Gut. (2012) 61:1007–15. 10.1136/gutjnl-2011-300971 [DOI] [PubMed] [Google Scholar]
- 12.Monteagudo-Mera A, Rastall RA, Gibson GR, Charalampopoulos D, Chatzifragkou A. Adhesion mechanisms mediated by probiotics and prebiotics and their potential impact on human health. Appl Microbiol Biotechnol. (2019) 103:6463–72. 10.1007/s00253-019-09978-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marteau P, Vesa T. Pharmacokinetics of probiotics and biotherapeutic agents in humans. Bioscience Microflora. (1998) 17:1–6. 10.12938/bifidus1996.17.1 [DOI] [Google Scholar]
- 14.Marteau P, Shanahan F. Basic aspects and pharmacology of probiotics: an overview of pharmacokinetics, mechanisms of action and side-effects. Best Pract Res Clin Gastroenterol. (2003) 17:725–40. 10.1016/S1521-6918(03)00055-6 [DOI] [PubMed] [Google Scholar]
- 15.Human Microbiome Project Consortium . A framework for human microbiome research. Nature. (2012) 486:215–21. 10.1038/nature11209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The MetaHIT Consortium Available online at: https://www.sanger.ac.uk/resources/downloads/bacteria/metahit/ (accessed March 15, 2020).
- 17.Yoshikata R, Myint KZ, Ohta H, Ishigaki Y. Inter-relationship between diet, lifestyle habits, gut microflora, and the equol-producer phenotype: baseline findings from a placebo-controlled intervention trial. Menopause. (2019) 26:273–85. 10.1097/GME.0000000000001202 [DOI] [PubMed] [Google Scholar]
- 18.Magklis E, Howe LD, Johnson L. Eating style and the frequency, size and timing of eating occasions: a cross-sectional analysis using 7-day weighed dietary records. Sci Rep. (2019) 9:15133. 10.1038/s41598-019-51534-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barbara G, Stanghellini V, Brandi G, Cremon C, Di Nardo G, De Giorgio R, et al. Interactions between commensal bacteria and gut sensorimotor function in health and disease. Am J Gastroenterol. (2005) 100:2560–68. 10.1111/j.1572-0241.2005.00230.x [DOI] [PubMed] [Google Scholar]
- 20.Lardeur D. L'intérêt de l'Utilisation des Probiotiques dans Certaines Affections de la Petite Enfance. Thèse de Doctorat d'État de Docteur de Pharmacie. Université de Lille; (2018). [Google Scholar]
- 21.Alvarez-Olmos MI, Oberhelman RA. Probiotic agents and infectious diseases: a modern perspective on a traditional therapy. Clin Infect Dis. (2001) 32:1567–15. 10.1086/320518 [DOI] [PubMed] [Google Scholar]
- 22.Wang HT, Anvari S, Anagnostou K. The role of probiotics in rreventing allergic disease. Children. (2019) 6:24. 10.3390/children6020024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu Y, Alookaran JJ, Rhoads JM. Probiotics in autoimmune and inflammatory disorders. Nutrients. (2018) 10:1537. 10.3390/nu10101537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mikov MM, Stojančević MP, Bojić GM. Probiotics as a promising treatment for inflammatory bowel disease. Hosp Pharmacol. (2014) 1:52–60. 10.5937/hpimj1401052M [DOI] [Google Scholar]
- 25.Mack DR. Probiotics in inflammatory bowel diseases and associated conditions. Nutrients. (2011) 3:245–64. 10.3390/nu3020245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.He S, Ran C, Qin C, Li S, Zhang H, de Vos WM, et al. Anti-Infective effect of adhesive probiotic Lactobacillus in fish is correlated with their spatial distribution in the intestinal tissue. Sci Rep. (2017) 7:13195. 10.1038/s41598-017-13466-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hart SP, Marshall DJ. Spatial arrangement affects population dynamics and competition independent of community composition. Ecology. (2009) 90:1485–91. 10.1890/08-1813.1 [DOI] [PubMed] [Google Scholar]
- 28.Conway PL, Gorbach SL, Goldin BR. Survival of lactic acid bacteria in the human stomach and adhesion to intestinal cells. J Dairy Sci. (1987) 70:1–12. 10.3168/jds.S0022-0302(87)79974-3 [DOI] [PubMed] [Google Scholar]
- 29.Rao RK, Samak G. Protection and restitution of gut barrier by probiotics: nutritional and clinical implications. Curr Nutr Food Sci. (2013) 9:99–107. 10.2174/1573401311309020004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dimidi E, Christodoulides S, Scott SM, Whelan K. Mechanisms of action of probiotics and the gastrointestinal microbiota on gut motility and constipation. Adv Nutr. (2017) 8:484–94. 10.3945/an.116.014407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Collins FL, Rios-Arce ND, Schepper JD, Parameswaran N, McCabe LR. The potential of probiotics as a therapy for osteoporosis. Microbiol Spectr. (2017) 5:1–16. 10.1128/microbiolspec.BAD-0015-2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Plaza-Diaz J, Ruiz-Ojeda FJ, Gil-Campos M, Gil A. Mechanisms of action of probiotics. Adv Nutr. (2019) 10(Suppl_1):S49–66. 10.1093/advances/nmy063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gilliland SE. Health and nutritional benefits from lactic acid bacteria. FEMS Microbiol Rev. (1990) 7:175–88. 10.1111/j.1574-6968.1990.tb04887.x [DOI] [PubMed] [Google Scholar]
- 34.Guo C, Zhang L. [Cholesterol-lowering effects of probiotics–a review]. Wei Sheng Wu Xue Bao. (2010) 50:1590–9. [PubMed] [Google Scholar]
- 35.Drago L. Probiotics and colon cancer. Microorganisms. (2019) 7:66. 10.3390/microorganisms7030066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Commane D, Hughes R, Shortt C, Rowland I. The potential mechanisms involved in the anti-carcinogenic action of probiotics. Mutat Res. (2005) 591:276–89. 10.1016/j.mrfmmm.2005.02.027 [DOI] [PubMed] [Google Scholar]
- 37.Górska A, Przystupski D, Niemczura MJ, Kulbacka J. Probiotic bacteria: a promising tool in cancer prevention and therapy. Curr Microbiol. (2019) 76:939–49. 10.1007/s00284-019-01679-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Singh AK, Hertzberger RY, Knaus UG. Hydrogen peroxide production by lactobacilli promotes epithelial restitution during colitis. Redox Biol. (2018) 16:11–20. 10.1016/j.redox.2018.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Matur E, Eraslan E. The impact of probiotics on the gastrointestinal physiology. In: Brzozowski T. editor. Book: New Advances in the Basic and Clinical Gastroenterology. Rijeka: InTech; (2012). [Google Scholar]
- 40.Ocaña VS, Elena Nader-Macías M. Production of antimicrobial substances by lactic acid bacteria II: screening bacteriocin-producing strains with probiotic purposes and characterization of a Lactobacillus bacteriocin. Methods Mol Biol. (2004) 268:347–53. 10.1385/1-59259-766-1:347 [DOI] [PubMed] [Google Scholar]
- 41.LeBlanc JG, Chain F, Martín R, Bermúdez-Humarán LG, Courau S, Langella P. Beneficial effects on host energy metabolism of short-chain fatty acids and vitamins produced by commensal and probiotic bacteria. Microb Cell Fact. (2017) 16:79. 10.1186/s12934-017-0691-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heyman M, Heuvelin E. Micro-organismes Probiotiques et Régulation Immunologique: Le Paradoxe. Available online at: http://www.em-premium.com.doc-distant.univlille2.fr/article/47796/resultatrecherche/26 (accessed January 29, 2018).
- 43.Bauer MP, Notermans DW, Van Benthem BH, Brazier JS, Wilcox MH, Rupnik M, et al. Clostridium difficile infection in Europe: a hospital-based survey. Lancet. (2011) 377:63–73. 10.1016/S0140-6736(10)61266-4 [DOI] [PubMed] [Google Scholar]
- 44.Salminen S. Human studies on probiotics: aspects of scientific documentation–review. Scand J Nutr. (2001) 45:8–12. 10.3402/fnr.v45i0.1783 [DOI] [Google Scholar]
- 45.Sullivan A, Bennet R, Viitanen M, Palmgren AC, Nord CE. Influence of Lactobacillus F19 on intestinal microflora in children and elderly persons and impact on Helicobacter pylori infections. Microbial Ecol Health Dis. (2002) S 3:17–21. 10.1080/089106002760003305 [DOI] [Google Scholar]
- 46.Saavedra JM, Abi-Hanna A, Moore N, Yolken RH. Longterm consumption of infant formulas containing live probiotic bacteria: tolerance and safety. Am J Clin Nutr. (2004) 79:261–7. 10.1093/ajcn/79.2.261 [DOI] [PubMed] [Google Scholar]
- 47.Saavedra JM, Bauman NA, Oung I, Perman JA, Yolken RH. Feeding of Bifidobacterium bifidum and Streptococcus thermophilus to infants in hospital for prevention of diarrhea and shedding of rotavirus. Lancet. (1994) 344:1046–9. 10.1016/S0140-6736(94)91708-6 [DOI] [PubMed] [Google Scholar]
- 48.Ringel-Kulka T, Palsson OS, Maier D, Carroll I, Galanko JA, Leyer G, et al. Probiotic bacteria Lactobacillus acidophilus NCFM and Bifidobacterium lactis Bi-07 versus placebo for the symptoms of bloating in patients with functional bowel disorders: a double-blind study. J Clin Gastroenterol. (2011) 45:518–25. 10.1097/MCG.0b013e31820ca4d6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pothoulakis C, Becker SD, LaMant JT. Mechanism of action of Clostridium difficile toxins. ln: Rambaud JC, Ducluzeau R. editors. Clostridium difficile et Pathologie Intestinale. Pans: Springer-Verlag; (1990). p. 55-61. [Google Scholar]
- 50.Lawley TD, Clare S, Walker AW, Douga G. Targeted restoration of the intestinal microbiota with a simple, defined bacteriotherapy resolves relapsing Clostridium difficile disease in mice. PLoS Pathogens. (2012) 8:e1002995. 10.1371/journal.ppat.1002995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Doron SI, Hibberd PL, Gorbach SL. Probiotics for prevention of antibiotic-associated diarrhea. J Clin Gastroenterol. (2008) 42:S58–63 80. 10.1097/MCG.0b013e3181618ab7 [DOI] [PubMed] [Google Scholar]
- 52.Choi CH, Jo SY, Park HJ, Chang SK, Byeon JS, Myung SJ. A randomized, double-blind, placebo-controlled multicenter trial of Saccharomyces boulardii in irritable bowel syndrome: effect on quality of life. J Clin Gastroenterol. (2011) 45:679–83. 10.1097/MCG.0b013e318204593e [DOI] [PubMed] [Google Scholar]
- 53.Szajewska H, Guarino A, Hojsak I, Indrio F, Kolacek S, Shamir R, et al. On behalf of the ESPGHAN working group for probiotics and prebiotics. Use of probiotics for management of acute gastroenteritis: A Position Paper by the ESPGHAN Working Group for Probiotics and Prebiotics. JPGN. (2014) 58:531–9. 10.1097/MPG.0000000000000320 [DOI] [PubMed] [Google Scholar]
- 54.Barbut FP, Mastrantonio P, Delmée M, Brazie JS, Kuijper EJ, Poxton IR, on behalf of the European Study Group on Clostridium difficile (ESGCD) . Prospective study of Clostridium difficile infections in Europe with phenotypic and genotypic characterisation of the isolates. Clin Microbiol Infect. (2007) 13:1048−57. [DOI] [PubMed] [Google Scholar]
- 55.Barbut F, Corthier G, Petit JC. Mécanismes physiopathologiques des infections digestives à Clostridium difficile. Médecine/Sciences. (1992) 8:214–22. 10.4267/10608/3107 [DOI] [Google Scholar]
- 56.McFarland LV. Evidence-based review of probiotics for antibiotic-associated diarrhea and Clostridium difficile infections. Anaerobe. (2009) 15:274–80. 10.1016/j.anaerobe.2009.09.002 [DOI] [PubMed] [Google Scholar]
- 57.Johnston BC, Ma SSY, Goldenberg JZ, Thorlund K, Vandvik PO, Loeb M, et al. Probiotics for the prevention of Clostridium difficile associated diarrhea. Ann Intern Med. (2012) 157:878–88. 10.7326/0003-4819-157-12-201212180-00563 [DOI] [PubMed] [Google Scholar]
- 58.Pillai A, Nelson R. Probiotics for treatment of Clostridium difficile-associated colitis in adults. Cochrane Database Syst Rev. (2008) 23:CD004611. 10.1002/14651858.CD004611.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dinleyici EC, Kara A, Dalgic N, Kurugol Z, Arica V, Metin O, et al. Saccharomyces boulardii CNCM I-745 reduces the duration of diarrhoea, length of emergency care and hospital stay in children with acute diarrhoea. Benef Microbes. (2015) 6:415–21. 10.3920/BM2014.0086 [DOI] [PubMed] [Google Scholar]
- 60.Fitzpatrick LR, Hertzog KL, Quatse AL, Koltun WA, Small JS, Vrana K, et al. Effects of the probiotic formulation VSL#3 on colitis in weanling rats. J Pediatr Gastroenterol Nutr. (2007) 44:561–70. 10.1097/MPG.0b013e31803bda51 [DOI] [PubMed] [Google Scholar]
- 61.Kruis W, Fric P, Pokrotnieks J, Lukás M, Fixa B, Kascák M, et al. Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as with standard mesalazine. Gut. (2004) 53:1617–23. 10.1136/gut.2003.037747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zocco MA, dal Verme LZ, Cremonini F, Piscaglia AC, Nista EC, Candelli M, et al. Efficacy of Lactobacillus GG in maintaining remission of ulcerative colitis. Aliment Pharmacol Ther. (2006) 23:1567–74. 10.1111/j.1365-2036.2006.02927.x [DOI] [PubMed] [Google Scholar]
- 63.Kato K, Mizuno S, Umesaki Y, Ishii Y, Sugitani M, Imaoka A, et al. Randomized placebo-controlled trial assessing the effect of bifidobacteria-fermented milk on active ulcerative colitis. Aliment Pharmacol Ther. (2004) 20:1133–41. 10.1111/j.1365-2036.2004.02268.x [DOI] [PubMed] [Google Scholar]
- 64.Marteau P, Lémann M, Seksik P, Laharie D, Colombel JF, Bouhnik Y, et al. Ineffectiveness of Lactobacillus johnsonii LA1 for prophylaxis of postoperative recurrence in Crohn's disease: A randomised, double blind, placebo controlled GETAID trial. Gut. (2006) 55:842–7. 10.1136/gut.2005.076604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Van Gossum A, Dewit O, Louis E, de Hertogh G, Baert F, Fontaine F, et al. Multicenter randomized-controlled clinical trial of probiotics (Lactobacillus johnsonii, LA1) on early endoscopic recurrence of Crohn's disease after ileo-caecal resection. Inflamm Bowel Dis. (2007) 13:135–42. 10.1002/ibd.20063 [DOI] [PubMed] [Google Scholar]
- 66.Cristofori F, Indrio F, Miniello VL, De Angelis M, Francavilla R. Probiotics in celiac disease. Nutrients. (2018) 10:1824. 10.3390/nu10121824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang KY, Li SN, Liu CS, Perng DS, Su YC, Wu DC, et al. Effects of ingesting Lactobacillus- and Bifidobacterium-containing yogurt in subjects with colonized Helicobacter pylori. Am J Clin Nutr. (2004) 80:737−41. 10.1093/ajcn/80.3.737 [DOI] [PubMed] [Google Scholar]
- 68.Kolars JC, Levitt MD, Aouji M, Savaiano DA. Yogurt—an autodigesting source of lactose. N Engl J Med. (1984) 310:1–3. 10.1056/NEJM198401053100101 [DOI] [PubMed] [Google Scholar]
- 69.Mater DDG, Langella P, Corthier G, Flores MJ. Probiotic Lactobacillus strain can acquire vancomycin resistance during digestive transit in mice. J Mol Microbiol Biotechnol. (2008) 14:123–7. 10.1159/000106091 [DOI] [PubMed] [Google Scholar]
- 70.Lund B, Edlund C. Probiotic Enterococcus faecium strain is a possible recipient of the vanA gene cluster. Clin Inf Dis. (2001) 32:1384–5. 10.1086/319994 [DOI] [PubMed] [Google Scholar]
- 71.Klein G, Hallmann C, Casas IA, Abad J, Louwers J, Reuter G. Exclusion of vanA, vanB and vanC type glycopeptide resistance in strains of Lactobacillus reuteri and Lactobacillus rhamnosus used as probiotics by polymerase chain reaction and hybridization methods. J Appl Microbiol. (2000) 89:815–24. 10.1046/j.1365-2672.2000.01187.x [DOI] [PubMed] [Google Scholar]
- 72.Goldenberg JZ, Yap C, Lytvyn L, Lo C, Beardsley J, Mertz D, et al. Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Cochrane Database Syst Rev. (2017) 12:CD006095. 10.1002/14651858.CD006095.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Debast SB, Bauer MP, Kuijper EJ. European Society of Clinical Microbiology and Infectious Diseases: update of the treatment guidance document for Clostridium difficile infection. Clin Microbiol Infect. (2014) 20:1–26. 10.1111/1469-0691.12418 [DOI] [PubMed] [Google Scholar]
- 74.Romano V, Pasquale V, Krovacek K, Mauri F, Demarta A, Dumontet S. Toxigenic Clostridium difficile PCR ribotypes from wastewater treatment plants in Southern Switzerland. Appl Environ Microbiol. (2012) 78:6643–6. 10.1128/AEM.01379-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cantero C, Schrenzel J, Darbellay Farhoumand P. Place des probiotiques dans la prévention d'un épisode inaugural d'infection à Clostridium difficile. Rev Med Suisse. (2018) 14 :1834−7. [PubMed] [Google Scholar]
- 76.Michal Stevens A, Esposito DH, Stoney RJ. Clostridium difficile infection in returning travelers. J Travel Med. (2017) 24, 1–14. 10.1093/jtm/taw099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Davies KA, Ashwin H, Longshaw CM, Burns DA, Davis GL, et al. Diversity of Clostridium difficile PCR ribotypes in Europe: results from the European, multicentre, prospective, biannual, point prevalence study of Clostridium difficile infection in hospitalised patients with diarrhoea (EUCLID), 2012 and 2013. Euro Surveill. (2016) 21, 1–11. 10.2807/1560-7917.ES.2016.21.29.30294 [DOI] [PubMed] [Google Scholar]
- 78.Deshpande A, Pasupuleti V, Thota P, Pant C, Rolston DD, Sferra TJ, et al. Community-associated Clostridium difficile infection and antibiotics: a meta-analysis. J Antimicrob Chemother. (2013) 68:1951–61. 10.1093/jac/dkt129 [DOI] [PubMed] [Google Scholar]
- 79.Kachrimanidou M, Tsachouridou O, Ziogas IA, Christaki E, Protonotariou E, Metallidis S, et al. Clostridium difficile infections in a university hospital in Greece are mainly associated with PCR ribotypes 017 and 126. J Med Microbiol. (2017) 66:1774–81. 10.1099/jmm.0.000623 [DOI] [PubMed] [Google Scholar]
- 80.Alcala L, Reigadas E, Marín M, Fernandez-Chico A, Catalan P, Bouza E, et al. Comparison of genomera C. difficile and Xpert C. difficile as confirmatory tests in a multistep algorithm for diagnosis of Clostridium difficile infection. J Clin Microbiol. (2015) 53:332–5. 10.1128/JCM.03093-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Enache-Angoulvant A, Hennequin C. Invasive Saccharomyces infection: a comprehensive review. Clin Infect Dis. (2005) 41:1559–68. 10.1086/497832 [DOI] [PubMed] [Google Scholar]
- 82.Munoz P, Bouza E, Cuenca-Estrella M, Eiros JM, Pérez MJ, Sánchez-Somolinos M, et al. Saccharomyces cerevisiae fungemia: an emerging infectious disease. Clin Infect Dis. (2005) 40:1625–34 10.1086/429916 [DOI] [PubMed] [Google Scholar]
- 83.Besselink MGH, van Santvoort HC, Buskens E, Boermeester MA, van Goor H, Timmerman HM, et al. Probiotic prophylaxis in predicted severe acute pancreatitis: a randomised, double-blind, placebo-controlled trial. Lancet. (2008) 371:651–9. 10.1016/S0140-6736(08)60207-X [DOI] [PubMed] [Google Scholar]
- 84.Clifford McDonald L, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Inf Dis. (2018) 66:e1–48. 10.1093/cid/cix1085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Marteau P, de Vrese M, Cellier C, Schrezenmeir J. Protection from gastrointestinal diseases with the use of probiotics. Am J Clin Nutr. (2001) 73:430S−6S. 10.1093/ajcn/73.2.430s [DOI] [PubMed] [Google Scholar]
- 86.Girardin M, Frossard JL. Place des probiotiques dans le traitement des maladies inflammatoires intestinales. Rev Med Suisse. (2012) 8:1674–8. [PubMed] [Google Scholar]
- 87.Miele E, Pascarella F, Giannetti E, Quaglietta L, Baldassano RN, Staiano A, et al. Effect of a probiotic preparation (VSL#3) on induction and maintenance of remission in children with ulcerative colitis. Am J Gastroenterol. (2009) 104:437–43. 10.1038/ajg.2008.118 [DOI] [PubMed] [Google Scholar]
- 88.Gionchetti P, Rizzello F, Morselli C, Poggioli G, Tambasco R, Calabrese C, et al. Highdose probiotics for the treatment of active pouchitis. Dis Colon Rectum. (2007) 50:2075–82. 10.1007/s10350-007-9068-4 [DOI] [PubMed] [Google Scholar]
- 89.Oak SJ, Jha R. The effects of probiotics in lactose intolerance: a systematic review. Crit Rev Food Sci Nutr. (2019) 59:1675–83. 10.1080/10408398.2018.1425977 [DOI] [PubMed] [Google Scholar]
- 90.Crovesya l, Gonçalvesa DC, Trigoa EL. Probiotics in allergy treatment: a literature review. Rev Esp Nutr Hum Diet. (2017) 21:293–9. 10.14306/renhyd.21.3.361 [DOI] [Google Scholar]
- 91.Berni Canani R, Paparo L, Nocerino R, Di Costanzo M, Bruno C, Buono A. Targeting food allergy with probiotics. In: Adv Exp Med Biol-Advances in Microbiology, Infectious Diseases and Public Health. Springer Nature Switzerland AG; (2018). p. 1125. [DOI] [PubMed] [Google Scholar]
- 92.Cao L, Wang L, Yang L, Tao S, Xia R, Fan W. Long-term effect of early-life supplementation with probiotics on preventing atopic dermatitis: A meta-analysis. J Dermatolog Treat. (2015) 26:537–40. 10.3109/09546634.2015.1027168 [DOI] [PubMed] [Google Scholar]
- 93.Panduru M, Panduru NM, Sălăvăstru CM, Tiplica GS. Probiotics and primary prevention of atopic dermatitis: a meta-analysis of randomized controlled studies. J Eur Acad Dermatol Venereol. (2015) 29:232–42. 10.1111/jdv.12496 [DOI] [PubMed] [Google Scholar]
- 94.Kalliomaki M, Salminen S, Arvilommi H, Kero P, Koskinen P, Isolauri E. Probiotics in primary prevention of atopic disease: a randomised placebo-controlled trial. Lancet. (2001) 357:1076–87. 10.1016/S0140-6736(00)04259-8 [DOI] [PubMed] [Google Scholar]
- 95.Wang IJ, Wang JY. Children with atopic dermatitis show clinical improvement after Lactobacillus exposure. Clin Exp Allergy. (2015) 45:779–87. 10.1111/cea.12489 [DOI] [PubMed] [Google Scholar]
- 96.Ishida Y, Nakamura F, Kanzato H, Sawada D, Hirata H, Nishimura A, et al. Clinical effects of Lactobacillus acidophilus strain L-92 on perennial allergic rhinitis: a double-blind, placebo-controlled study. J Dairy Sci. (2005) 88:527–33. 10.3168/jds.S0022-0302(05)72714-4 [DOI] [PubMed] [Google Scholar]
- 97.Yonekura S, Okamoto Y, Okawa T, Hisamitsu M, Chazono H, Kobayashi K, et al. Effects of daily intake of Lactobacillus paracasei strain KW3110 on Japanese cedar pollinosis. Allergy Asthma Proc. (2009) 30:397–405. 10.2500/aap.2009.30.3256 [DOI] [PubMed] [Google Scholar]
- 98.Helin T, Haahtela S, Haahtela T. No effect of oral treatment with an intestinal bacterial strain, Lactobacillus rhamnosus (ATCC 53103), on birch-pollen allergy: a placebo-controlled double-blind study. Allergy. (2002) 57:243–6. 10.1034/j.1398-9995.2002.1s3299.x [DOI] [PubMed] [Google Scholar]
- 99.Morita H, He F, Kawase M, Kubota A, Hiramatsu M, Kurisaki J, et al. Preliminary human study for possible alteration of serum immunoglobulin E production in perennial allergic rhinitis with fermented milk prepared with Lactobacillus gasseri TMC0356. Microbiol Immunol. (2006) 50:701–6. 10.1111/j.1348-0421.2006.tb03842.x [DOI] [PubMed] [Google Scholar]
- 100.Singh A, Hacini-Rachinel F, Gosoniu ML, Bourdeau T, Holvoet S, Doucet-Ladeveze R, et al. Immune-modulatory effect of probiotic Bifidobacterium lactis NCC2818 in individuals suffering from seasonal allergic rhinitis to grass pollen: an exploratory, randomized, placebo-controlled clinical trial. Eur J Clin Nutr. (2013) 67:161–7. 10.1038/ejcn.2012.197 [DOI] [PubMed] [Google Scholar]
- 101.Costa DJ, Marteau P, Amouyal M, Poulsen LK, Hamelmann E, Cazaubiel M, et al. Efficacy and safety of the probiotic Lactobacillus paracasei LP-33 in allergic rhinitis: a double-blind, randomized, placebo-controlled trial (GA2LEN Study). Eur J Clin Nutr. (2014) 68:602–7. 10.1038/ejcn.2014.13 [DOI] [PubMed] [Google Scholar]
- 102.Ouwehand AC, Nermes M, Collado MC, Rautonen N, Salminen S, Isolauri E. Specific probiotics alleviate allergic rhinitis during the birch pollen season. World J Gastroenterol. (2009) 15:3261–8. 10.3748/wjg.15.3261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kawase M, He F, Kubota A, Hiramatsu M, Saito H, Ishii T, et al. Effect of fermented milk prepared with two probiotic strains on Japanese cedar pollinosis in a double-blind placebo-controlled clinical study. Int J Food Microbiol. (2009) 128:429–34. 10.1016/j.ijfoodmicro.2008.09.017 [DOI] [PubMed] [Google Scholar]
- 104.Di Felice G, Barletta B, Butteroni C, Corinti S, Tinghino R, Colombo P, et al. Use of probiotic bacteria for prevention and therapy of allergic diseases: studies in mouse model of allergic sensitization. J Clin Gastroenterol. (2008) 42:S130–2. 10.1097/MCG.0b013e318169c463 [DOI] [PubMed] [Google Scholar]
- 105.Meijerink M, Wells JM, Taverne N, de Zeeuw Brouwer ML, Hilhorst B, Venema K, et al. Immunomodulatory effects of potential probiotics in a mouse peanut sensitization model. FEMS Immunol Med Microbiol. (2012) 65:488–96. 10.1111/j.1574-695X.2012.00981.x [DOI] [PubMed] [Google Scholar]
- 106.Peng GC, Hsu CH. The efficacy and safety of heat-killed Lactobacillus paracasei for treatment of perennial allergic rhinitis induced by house-dust mite. Pediatr Allergy Immunol. (2005) 16:433–8. 10.1111/j.1399-3038.2005.00284.x [DOI] [PubMed] [Google Scholar]
- 107.Xiao JZ, Kondo S, Yanagisawa N, Takahashi N, Odamaki T, Iwabuchi N, et al. Effect of probiotic Bifidobacterium longum BB536 in relieving clinical symptoms and modulating plasma cytokine levels of Japanese cedar pollinosis during the pollen season. A randomized double-blind, placebo-controlled trial. J Investig Allergol Clin Immunol. (2006) 16:86−93. [PubMed] [Google Scholar]
- 108.Bickert T, Trujillo-Vargas CM, Duechs M, Wohlleben G, Polte T, Hansen G, et al. Probiotic Escherichia coli Nissle 1917 suppresses allergen-induced Th2 responses in the airways. Int Arch Allergy Immunol. (2009) 149:219–30. 10.1159/000199717 [DOI] [PubMed] [Google Scholar]
- 109.Niccoli AA, Artesi AL, Candio F, Ceccarelli S, Cozzali R, Ferraro L, et al. Preliminary results on clinical effects of probiotic Lactobacillus salivarius LS01 in children affected by atopic dermatitis. J Clin Gastroenterol. (2014) 48:S34–6. 10.1097/MCG.0000000000000233 [DOI] [PubMed] [Google Scholar]
- 110.Castellazzi AM, Valsecchi C, Caimmi S, Licari A, Marseglia A, Leoni MC, et al. Probiotics and food allergy. Ital J Pediatr. (2013) 39:47. 10.1186/1824-7288-39-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. (2006) 368:733–43. 10.1016/S0140-6736(06)69283-0 [DOI] [PubMed] [Google Scholar]
- 112.Arrieta MC, Stiemsma LT, Dimitriu PA, Thorson L, Russell S, Yurist-Doutsch S, et al. Early infancy microbial and metabolic alterations affect risk of childhood asthma. Sci Translat Med. (2015) 7:307ra152. 10.1126/scitranslmed.aab2271 [DOI] [PubMed] [Google Scholar]
- 113.Zhang B, An J, Shimada T, Liu S, Maeyama K. Oral administration of Enterococcus faecalis FK-23 suppresses Th17 cell development and attenuates allergic airway responses in mice. Int J Mol Med. (2012) 30:248–54. 10.3892/ijmm.2012.1010 [DOI] [PubMed] [Google Scholar]
- 114.Elborn JS. Cystic fibrosis. Lancet. (2016) 388:2519–31. 10.1016/S0140-6736(16)00576-6 [DOI] [PubMed] [Google Scholar]
- 115.Dumas A, Bernard L, Poquet Y, Lugo-Villarino G, Neyrolles O. The role of the lung microbiota and the gut-lung axis in respiratory infectious diseases. Cell Microbial. (2018) 20:e12966. 10.1111/cmi.12966 [DOI] [PubMed] [Google Scholar]
- 116.Alexandre Y, Le Blay G, Boisrame-Gastrin S, Le Gall F, Héry-Arnaud G, Gouriou S, et al. Probiotics: a new way to fight pulmonary infections? Med Malad Inf. (2014) 44:9–17. 10.1016/j.medmal.2013.05.001 [DOI] [PubMed] [Google Scholar]
- 117.Weiss B, Bujanover Y, Yahav Y, Efrati O. Probiotic supplementation affects pulmonary exacerbations in patients with cystic fibrosis: a pilot study. Pediatric Pulmonol. (2010) 45:536–40. 10.1002/ppul.21138 [DOI] [PubMed] [Google Scholar]
- 118.Neri LCL, Taminato M, da Silva LV. Systematic Review of probiotics for cystic fibrosis patients: moving forward. J Pediatr Gastroenterol Nutr. (2019) 68:394–9. 10.1097/MPG.0000000000002185 [DOI] [PubMed] [Google Scholar]
- 119.Hojsak I, Snovak N, Abdovic S, Szajewska H, Misak Z, Kolacek S. Lactobacillus GG in the prevention of gastrointestinal and respiratory tract infections in children who attend day care centers: a randomized, double-blind, placebo-controlled trial. Clin Nutr. (2010) 29:312–6. 10.1016/j.clnu.2009.09.008 [DOI] [PubMed] [Google Scholar]
- 120.Gutierrez-Castrellon P, Lopez-Velazquez G, Diaz-Garcia L, Jimenez-Gutierrez C, Mancilla-Ramirez J, Estevez-Jimenez J, et al. Diarrhea in preschool children and Lactobacillus reuteri: a randomized controlled trial. Pediatrics. (2014) 133:e904–9. 10.1542/peds.2013-0652 [DOI] [PubMed] [Google Scholar]
- 121.Tubelius P, Stan V, Zachrisson A. Increasing work-place healthiness with the probiotic Lactobacillus reuteri: a randomised, double-blind placebo-controlled study. Environ Health. (2005) 4:25. 10.1186/1476-069X-4-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Das RR, Naik SS, Singh M. Probiotics as additives on therapy in allergic airway diseases: a systematic review of benefits and risks. Biomed Res Int. (2013) 2013:231979. 10.1155/2013/231979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Abrahamsson TR, Jakobsson T, Björkstén B, Oldaeus G, Jenmalm MC. No effect of probiotics on respiratory allergies: a seven-year follow-up of a randomized controlled trial in infancy. Pediatr Allergy Immunol. (2013) 24:556–61. 10.1111/pai.12104 [DOI] [PubMed] [Google Scholar]
- 124.Azad MB, Coneys JG, Kozyrskyj AL, Field CJ, Ramsey CD, Becker AB, et al. Probiotic supplementation during pregnancy or infancy for the prevention of asthma and wheeze: systematic review and meta-analysis. BMJ. (2013) 347:f6471 10.1136/bmj.f6471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Mortaz E, Adcock IM, Folkerts G, Barnes PJ, Vos AP, Garssen J. Probiotics in the management of lung diseases. Mediators Inflamm. (2013) 2013:751068. 10.1155/2013/751068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Baccala R, Gonzalez-Quintial R, Lawson BR, Theofilopoulos AN. Sensors of the innate immune system: their mode of action. Nat Rev Rheumatol. (2009) 5:448–56. 10.1038/nrrheum.2009.136 [DOI] [PubMed] [Google Scholar]
- 127.Mogensen TH. Pathogen recognition and inflammatory signaling in innate immune defenses. Clin Microbiol Rev. (2009) 22:240–73. 10.1128/CMR.00046-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Pedraza ST, Betancur JG. Viral Recognition by the Innate Immune System: The Role of Pattern Recognition Receptors. Available online at: http://colombiamedica.univalle.edu.co/index.php/comedica/article/view/731/1195
- 129.Steinhagen F, Schmidt SV, Schewe C, Bode C. Immunotherapy in sepsis - brake or accelerate? Pharmacol Therap. (2020) 208:107476 10.1016/j.pharmthera.2020.107476 [DOI] [PubMed] [Google Scholar]
- 130.Wiersinga WJ, Leopold SJ, Cranendonk DR, van der Poll T. Host innate immune responses to sepsis. Virulence. (2014) 5:36–44. 10.4161/viru.25436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Khor B, Gardet A, Xavier RJ. Genetics and pathogenesis of inflammatory bowel disease. Nature. (2011) 474:307–17. 10.1038/nature10209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Yao P, Tan F, Gao H, Wang L, Yang T, Cheng Y. Effects of probiotics on Toll-like receptor expression in ulcerative colitis rats induced by 2,4,6-trinitro-benzene sulfonic acid. Mol Med Rep. (2017) 15:1973–80. 10.3892/mmr.2017.6226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Cook DJ, Johnstone J, Marshall JC, Lauzier F, Thabane L, Mehta S, et al. Probiotics: prevention of severe pneumonia and endotracheal colonization trial—PROSPECT: a pilot trial. Trials. (2016) 17:377. 10.1186/s13063-016-1495-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Westerbeck JW, Machamer CE. A coronavirus E protein is present in two distinct pools with different effects on assembly and the secretory pathway. J Virol. (2015) 89:9313–23. 10.1128/JVI.01237-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Javier RT, Rice AP. Emerging theme: cellular PDZ proteins as common targets of pathogenic viruses. J Virol. (2011) 85:11544–56. 10.1128/JVI.05410-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Schoeman D, Fielding BC. Coronavirus envelope protein: current knowledge. Virol J. (2019) 16:69. 10.1186/s12985-019-1182-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Jimenez-Guardeño JM, Nieto-Torres JL, DeDiego ML, Regla-Nava JA, Fernandez-Delgado R, Castaño-Rodriguez C, et al. The PDZ-binding motif of severe acute respiratory syndrome coronavirus envelope protein is a determinant of viral pathogenesis. PLoS Pathog. (2014) 10:e1004320. 10.1371/journal.ppat.1004320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Börgeling Y, Schmolke M, Viemann D, Nordhoff C, Roth J, Ludwig S. Inhibition of p38 mitogen-activated protein kinase impairs influenza virus-induced primary and secondary host gene responses and protects mice from lethal H5N1 infection. J Biol Chem. (2014) 289:13–27. 10.1074/jbc.M113.469239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Segawa S, Fujiya M, Konishi H, Ueno N, Kobayashi N, Shigyo T, et al. Probiotic-derived polyphosphate enhances the epithelial barrier function and maintains intestinal homeostasis through integrin-p38 MAPK pathway. PLoS ONE. (2011) 6:e23278. 10.1371/journal.pone.0023278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Enaud R, Prevel R, Ciarlo E, Beaufils F, Wieërs G, Guery B, et al. The gut-lung axis in health and respiratory diseases: a place for inter-organ and inter-kingdom crosstalks. Front Cell Infect Microbiol. (2020) 10:9. 10.3389/fcimb.2020.00009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Schuijt TJ, Lankelma JM, Scicluna BP, de Sousa e Melo F, Roelofs JJTH, Daan de Boer J, et al. The gut microbiota plays a protective role in the host defence against pneumococcal pneumonia. Gut. (2016) 65:575–83. 10.1136/gutjnl-2015-309728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Bravo JA, Forsythe P, Chew MV, Escaravage E, Savignac HM, Dinan TG, et al. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc Natl Acad Sci USA. (2011) 108:16050–5. 10.1073/pnas.1102999108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Liu X, Cao S, Zhang X. Modulation of gut microbiota-brain axis by probiotics, prebiotics, and diet. J Agric Food Chem. (2015) 63:7885–95. 10.1021/acs.jafc.5b02404 [DOI] [PubMed] [Google Scholar]
- 144.Kwon HK, Kim GC, Kim Y, Hwang W, Jash A, Sahoo A, et al. Amelioration of experimental autoimmune encephalomyelitis by probiotic mixture is mediated by a shift in T helper cell immune response. Clin Immunol. (2013) 146:217–27. 10.1016/j.clim.2013.01.001 [DOI] [PubMed] [Google Scholar]
- 145.Finegold SM, Downes J, Summanen PH. Microbiology of regressive autism. Anaerobe. (2012) 18:260–2. 10.1016/j.anaerobe.2011.12.018 [DOI] [PubMed] [Google Scholar]
- 146.Finegold SM, Molitoris D, Song Y, Liu C, Vaisanen ML, Bolte E, et al. Gastrointestinal microflora studies in late-onset autism. Clin Inf Dis. (2002) 35:S6–16. 10.1086/341914 [DOI] [PubMed] [Google Scholar]
- 147.Kaluzna-Czaplinska J, Blaszczyk S. The level of arabinitol in autistic children after probiotic therapy. Nutrition. (2012) 28:124–6. 10.1016/j.nut.2011.08.002 [DOI] [PubMed] [Google Scholar]
- 148.Chae CS, Kwon HK, Hwang JS, Kim JE, Im SH. Prophylactic effect of probiotics on the development of experimental autoimmune myasthenia gravis. PLoS ONE. (2012) 7:e52119. 10.1371/journal.pone.0052119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Lavasani S, Dzhambazov B, Nouri M, Fak F, Buske S, Molin G, et al. A novel probiotic mixture exerts a therapeutic effect on experimental autoimmune encephalomyelitis mediated by IL-10 producing regulatory T cells. PLoS ONE. (2010) 5:e9009. 10.1371/journal.pone.0009009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Umbrello G, Esposito S. Microbiota and neurologic diseases: potential effects of probiotics. J Transl Med. (2016) 14:298. 10.1186/s12967-016-1058-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Wang Y, Kasper LH. The role of microbiome in central nervous system disorders. Brain Behav Immun. (2014) 38:1–12. 10.1016/j.bbi.2013.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ghaisas S, Maher J, Kanthasamy A. Gut microbiome in health and disease: linking the microbiome-gut-brain axis and environmental factors in the pathogenesis of systemic and neurodegenerative diseases. Pharmacol Ther. (2016) 158:52–62. 10.1016/j.pharmthera.2015.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Tsiotsias A, Voidarou C, Skoufos J, Simopoulos C, Konstadi M, Kostakis D, et al. Repeated-stress alterations in the intestinal microflora. Microb Ecol Health Dis. (2004) 16:28–31. 10.1080/08910600410028632 [DOI] [Google Scholar]
- 154.Konstandi M, Voidarou C, Papadaki E, Tsiotsias A, Kotsovolou O, Evangelou E, et al. Stress modifies the vaginal flora in cyclic female rats. Microb Ecol Health Dis. (2006) 18:161–9. 10.1080/08910600601072464 [DOI] [Google Scholar]
- 155.O'Mahony SM, Clarke G, Dinan TG, Cryan JF. Early-life adversity and brain development: is the microbiome a missing piece of the puzzle? Neurosci. (2017) 342:37–54. 10.1016/j.neuroscience.2015.09.068 [DOI] [PubMed] [Google Scholar]
- 156.Yarandi SS, Peterson DA, Treisman GJ, Moran TH, Pasricha PJ. Modulatory effects of gut microbiota on the central nervous system: how gut could play a role in neuropsychiatric health and diseases. J Neurogastroenterol Motil. (2016) 22:201–12. 10.5056/jnm15146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Sun J, Ling Z, Wang F, Chen W, Li H, Jin J, et al. Clostridium butyricum pretreatment attenuates cerebral ischemia/reperfusion injury in mice via anti-oxidation and anti-apoptosis. Neurosci Lett. (2016) 613:30–5. 10.1016/j.neulet.2015.12.047 [DOI] [PubMed] [Google Scholar]
- 158.Savignac HM, Tramullas M, Kiely B, Dinan TG, Cryan JF. Bifidobacteria modulate cognitive processes in an anxious mouse strain. Behav Brain Res. (2015) 287:59–72. 10.1016/j.bbr.2015.02.044 [DOI] [PubMed] [Google Scholar]
- 159.Shanahan F. A commentary on the safety of probiotics. Gastroenterol Clin North Am. (2012) 41:869–76. 10.1016/j.gtc.2012.08.006 [DOI] [PubMed] [Google Scholar]
- 160.Xu M, Wang B, Fu Y, Chen Y, Yang F, Lu H, et al. Changes of fecal Bifidobacterium species in adult patients with hepatitis B virus-induced chronic liver disease. Microb Ecol. (2012) 63:304–13. 10.1007/s00248-011-9925-5 [DOI] [PubMed] [Google Scholar]
- 161.Dapito DH, Mencin A, Gwak GY, Pradere JP, Jang MK, Mederacke I, et al. Promotion of hepatocellular carcinoma by the intestinal microbiota and TLR4. Cancer Cell. (2012) 21:504–16. 10.1016/j.ccr.2012.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Xia X, Chen J, Xia J, Wang B, Liu H, Yang L, et al. Role of probiotics in the treatment of minimal hepatic encephalopathy in patients with HBV-induced liver cirrhosis. J Int Med Res. (2018) 46:3596–604. 10.1177/0300060518776064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Liu Q, Duan ZP, Ha DK, Bengmark S, Kurtovic J, Riordan SM, et al. Synbiotic modulation of gut flora: effect on minimal hepatic encephalopathy in patients with cirrhosis. Hepatology. (2004) 39:1441–52. 10.1002/hep.20194 [DOI] [PubMed] [Google Scholar]
- 164.Khungar V, Poordad F. Hepatic encephalopathy. Clin Liver Dis. (2012) 16:301–10. 10.1016/j.cld.2012.03.009 [DOI] [PubMed] [Google Scholar]
- 165.Dalal R, McGee RG, Riordan SM, Webster AC. Probiotics for people with hepatic encephalopathy. Cochrane Database Syst Rev. (2017) 2:CD008716. 10.1002/14651858.CD008716.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Agrawal A, Sharma BC, Sharma P, Sarin SK. Secondary prophylaxis of hepatic encephalopathy in cirrhosis: an open-label, randomized controlled trial of lactulose, probiotics, and no therapy. Am J Gastroenterol. (2012) 107:1043–50. 10.1038/ajg.2012.113 [DOI] [PubMed] [Google Scholar]
- 167.Sharma V, Garg S, Aggarwal S. Probiotics and liver disease. Perm J. (2013) 17:62–7. 10.7812/TPP/12-144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Albert DM, Döderlein G–. ein kritischer Blick auf zwei besondere Lebensläufe deutscher Ordinarien. Zentralblatt Gynäkol. (2006) 128: 56–9. 10.1055/s-2006-921412 [DOI] [PubMed] [Google Scholar]
- 169.Vasquez A, Jakobsson T, Ahrne S, Forsum U, Molin G. Vaginal Lactobacillus flora of healthy Swedish women. J Clin Microbiol. (2002) 40:2746–9. 10.1128/JCM.40.8.2746-2749.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Homayouni A, Bastani P, Ziyadi S, Mohammad-Alizadeh-Charandabi S, Ghalibaf M, Mortazavian AM, et al. Effects of probiotics on the recurrence of bacterial vaginosis: a review. J Low Genit Tract Dis. (2014) 18:79–86. 10.1097/LGT.0b013e31829156ec [DOI] [PubMed] [Google Scholar]
- 171.Falagas M, Betsi GI, Athanasiou S. Probiotics for the treatment of women with bacterial vaginosis. Clin Microbiol Infect. (2007) 13:657–64. 10.1111/j.1469-0691.2007.01688.x [DOI] [PubMed] [Google Scholar]
- 172.McLean NW, McGroarty JA. Growth inhibition of metronidazole-susceptible and metronidazole-resistant strains of Gardnerella vaginalis by lactobacilli in vitro. Appl Environ Microbiol. (1996) 62:1089–92. 10.1128/AEM.62.3.1089-1092.1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Mazloom k, Siddiqi I, Covasa M. Probiotics: how effective are they in the fight against pbesity? Nutrients. (2019) 11:258. 10.3390/nu11020258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Brusaferro A, Cozzali R, Orabona C, Biscarini A, Farinelli E, Cavalli E, et al. Is it time to use probiotics to prevent or treat obesity? Nutrients. (2018) 10:1613 10.3390/nu10111613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Wang Z-B, Xin S-S, Ding L-N, Ding W-Y, Hou Y-L, Liu C-Q, et al. The potential role of probiotics in controlling overweight/obesity and associated metabolic parameters in adults: a systematic review and metanalysis. Evid Based Comp Altern Med. (2019) 1–15. 10.1155/2019/3862971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Rosenstein IJ, Fontaine EA, Morgan DJ, Sheehan M, Lamont RF, Taylor-Robinson D. Relationship between hydrogen peroxide-producing strains of lactobacilli and vaginosis-associated bacterial species in pregnant women. Eur J Clin Microbiol Infect Dis. (1997) 16:517–22. 10.1007/BF01708235 [DOI] [PubMed] [Google Scholar]
- 177.Alvarez-Olmos MI, Barousse MM, Rajan L, Van Der Pol BJ, Fortenberry D, Orr D, et al. Vaginal lactobacilli in adolescents: presence and relationship to local and systemic immunity, and to bacterial vaginosis. Am Sex Trans Dis Assoc. (2004) 31:393–400. 10.1097/01.OLQ.0000130454.83883.E9 [DOI] [PubMed] [Google Scholar]
- 178.Johnson JR, Russo TA. Acute pyelonephritis in adults. New Engl J Med. (2018) 378:48–59. 10.1056/NEJMcp1702758 [DOI] [PubMed] [Google Scholar]
- 179.Walsh C, Collyns T. The pathophysiology of urinary tract infections. Surgery. (2017) 35:293–8. 10.1016/j.mpsur.2017.03.007 [DOI] [Google Scholar]
- 180.Wagenlehner FME, Cloutier DJ, Komirenko AS, Cebrik DS, Krause KM, Keepers TR, et al. Once-daily plazomicin for complicated urinary tract infections. N Engl J Med. (2019) 380:729–40. 10.1056/NEJMoa1801467 [DOI] [PubMed] [Google Scholar]
- 181.Akgül T, Karakan T. The role of probiotics in women with recurrent urinary tract infections. Turk J Urol. (2018) 44:377–83. 10.5152/tud.2018.48742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Schwenger EM, Tejani AM, Loewen PS. Probiotics for preventing urinary tract infections in adults and children. Cochrane Database Syst Rev. (2015) CD008772. 10.1002/14651858.CD008772.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Grin PM, Kowalewska PM, Alhazzan W, Fox-Robichaud AE. Lactobacillus for preventing recurrent urinary tract infections in women: meta-analysis. Can J Urol. (2013) 20:6607–14. [PubMed] [Google Scholar]
- 184.Borchert D, Sheridan L, Papatsoris A, Faruquz Z, Barua JM, Junaid I, et al. Prevention and treatment of urinary tract infection with probiotics: review and research perspective. Indian J Urol. (2008) 24:139–44. 10.4103/0970-1591.40604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Falagas ME, Betsi GI, Tokas T, Athanasiou S. Probiotics for prevention of recurrent urinary tract infections in women: a review of the evidence from microbiological and clinical studies. Drugs. (2006) 66:1253–61. 10.2165/00003495-200666090-00007 [DOI] [PubMed] [Google Scholar]
- 186.Stapleton AE, Au-Yeung M, Hooton TM, Fredricks DN, Roberts PL, Czaja CA, et al. Randomized, placebo controlled Phase 2 trial of a Lactobacillus crispatus probiotic given intravaginally for the prevention of recurrent urinary tract infection. Clin Infect Dis. (2011) 52:1212–7. 10.1093/cid/cir183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Ghartey JP, Smith BC, Chen Z, Buckley N, Lo Y, Ratner AJ, et al. Lactobacillus crispatus dominant vaginal microbiome is associated with inhibitory activity of female genital tract secretions against Escherichia coli. PLoS ONE. (2014) 9:e96659. 10.1371/journal.pone.0096659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Bordalo Tonucci L, Olbrich Dos Santos KM, De Luces Fortes Ferreira CL, Machado Rocha Ribeiro S, Licursi De Oliveira L, Stampini Duarte Martino H. Gut microbiota and probiotics: focus on diabetes mellitus. Crit Rev Food Sci Nutr. (2017) 57:2296–309. 10.1080/10408398.2014.934438 [DOI] [PubMed] [Google Scholar]
- 189.Yao K, Zeng L, He Q, Wang W, Lei J, Zou X. Effect of probiotics on glucose and lipid metabolism in type 2 diabetes mellitus: a meta-analysis of 12 randomized controlled trials. Med Sci Monit. (2017) 23:3044–53. 10.12659/MSM.902600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Rittiphairoj T, Pongpirul K, Mueller NT, Li T. Probiotics for glycemic control in patients with type 2 diabetes mellitus: protocol for a systematic review. Syst Rev. (2019) 8:227. 10.1186/s13643-019-1145-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Ejtahed HS, Mohtadi-Nia J, Homayouni-Rad A, Niafar M, Asghari-Jafarabadi M, Mofid V. Probiotic yogurt improves antioxidant status in type 2 diabetic patients. Nutrition. (2012) 28:539–43. 10.1016/j.nut.2011.08.013 [DOI] [PubMed] [Google Scholar]
- 192.De Smet I, De Boever P, Verstraete W. Cholesterol lowering in pigs through enhanced bacterial bile salt hydrolase activity. Br J Nutr. (1998) 79:185–94. 10.1079/BJN19980030 [DOI] [PubMed] [Google Scholar]
- 193.Ullah A, Khan A, Khan I. Diabetes mellitus and oxidative stress—A concise review. Saudi Pharm J. (2016) 24:547–53. 10.1016/j.jsps.2015.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Yi-Cheng Chang Y-C, Chuang L-M. The role of oxidative stress in the pathogenesis of type 2 diabetes: from molecular mechanism to clinical implication. Am J Transl Res. (2010) 2:316−31. [PMC free article] [PubMed] [Google Scholar]
- 195.Ley RE. Human gut microbes associated with obesity. Nature. (2006) 444:1022–3. 10.1038/4441022a [DOI] [PubMed] [Google Scholar]
- 196.Kumar M, Nagpal R, Kumar R, Hemalatha R, Verma V, Kumar A, et al. Cholesterol-;owering probiotics as potential biotherapeutics for metabolic diseases. Exp Diabetes Res. (2012) 2012:902917 10.1155/2012/902917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Siegel RL, Miller KD, Jemal A. Cancer statistics. CA Cancer J Clin. (2020) 70:7–30. 10.3322/caac.21590 [DOI] [PubMed] [Google Scholar]
- 198.Pasquereau-Kotula E, Martins M, Aymeric L, Dramsi S. Significance of Streptococcus gallolyticus subsp. gallolyticus association with colorectal cancer. Front Microbiol. (2018) 9:614. 10.3389/fmicb.2018.00614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Lee JW, Shin JG, Kim EH, Kang HE, Yim IB, Kim JY, et al. Immunomodulatory and antitumor effects in vivo by the cytoplasmic fraction of Lactobacillus casei and Bifidobacterium longum. J Vet Sci. (2004) 5:41–8. 10.4142/jvs.2004.5.1.41 [DOI] [PubMed] [Google Scholar]
- 200.Kim Y, Lee D, Kim D, Cho J, Yang J, Chung M, et al. Inhibition of proliferation in colon cancer cell lines and harmful enzyme activity of colon bacteria by Bifidobacterium adolescentis SPM0212. Arch Pharm Res. (2008) 31:468–73. 10.1007/s12272-001-1180-y [DOI] [PubMed] [Google Scholar]
- 201.Orlando A, Refolo MG, Messa C, Amati L, Lavermicocca P, Guerra V, et al. Antiproliferative and proapoptotic effects of viable or heat-killed Lactobacillus paracasei IMPC2.1 and Lactobacillus rhamnosus GG in HGC-27 gastric and DLD-1 colon cell lines. Nutr Cancer. (2012) 64:1103–11. 10.1080/01635581.2012.717676 [DOI] [PubMed] [Google Scholar]
- 202.Stein K, Borowicki A, Scharlau D, Schettler A, Scheu K, Obst U, Glei M. Effects of synbiotic fermentation products on primary chemoprevention in human colon cells. J Nutr Biochem. (2012) 23:777–84. 10.1016/j.jnutbio.2011.03.022 [DOI] [PubMed] [Google Scholar]
- 203.Kim Y, Oh S, Yun HS, Oh S, Kim SH. Cell-bound exopolysaccharide from probiotic bacteria induces autophagic cell death of tumour cells. Lett Appl Microbiol. (2010) 51:123–30. 10.1111/j.1472-765X.2010.02859.x [DOI] [PubMed] [Google Scholar]
- 204.Ma EL, Choi YJ, Choi J, Pothoulakis C, Rhee SH, Im E. The anticancer effect of probiotic Bacillus polyfermenticus on human colon cancer cells is mediated through ErbB2 and ErbB3 inhibition. Int J Cancer. (2010) 127:780–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Salminen S, Ouwehand AC, Isolauri E. Clinical applications of probiotic bacteria. Int Dairy J. (1998) 8:563–72. 10.1016/S0958-6946(98)00077-6 [DOI] [Google Scholar]
- 206.Javanmard A, Ashtari S, Sabet B, Davoodi SH, Rostami-Nejad M, Akbari ME, et al. Probiotics and their role in gastrointestinal cancers prevention and treatment; an overview. Gastroenterol Hepatol Bed Bench. (2018) 11:284–95. [PMC free article] [PubMed] [Google Scholar]
- 207.Liong MT. Roles of probiotics and prebiotics in colon cancer prevention: postulated mechanisms and in-vivo evidence. Int J Mol Sci. (2008) 9:854–63. 10.3390/ijms9050854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Rafter J. The effects of probiotics on colon cancer development. Nutr Res Rev. (2004) 17:277–84. 10.1079/NRR200484 [DOI] [PubMed] [Google Scholar]
- 209.Shimauchi H, Mayanagi G, Nakaya S, Minamibuchi M, Ito Y, Yamaki K, et al. Improvement of periodontal condition by probiotics with Lactobacillus salivarius WB21: a randomized, double-blind, placebo-controlled study. J Clin Periodontol. (2008) 35:897–905. 10.1111/j.1600-051X.2008.01306.x [DOI] [PubMed] [Google Scholar]
- 210.Nikawa H, Makihira S, Fukushima H, Aimi R. Lactobacillus reuteri in bovine milk fermented decreases the oral carriage of mutans streptococci. Int J Food Microbiol. (2004) 95:219–23. 10.1016/j.ijfoodmicro.2004.03.006 [DOI] [PubMed] [Google Scholar]
- 211.Flichy-Fernández AJ, Alegre-Domingo T, Peñarrocha-Oltra D, Peñarrocha Diago M. Probiotic treatment in the oral cavity: an update. J Med Oral Patol Oral Cir Bucal. (2010) 15:677–80. 10.4317/medoral.15.e677 [DOI] [PubMed] [Google Scholar]
- 212.Haukioja A. Probiotics and oral health. Eur J Dentistry. (2010) 4:348–55. 10.1055/s-0039-1697851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Hatakka K, Ahola AJ, Yli-Knuuttila H, Richardson M, Poussa T, Meurman JK, et al. Probiotics reduce the prevalence of oral Candida in the elderly – a randomized controlled trial. J Dent Res. (2007) 86:125–30. 10.1177/154405910708600204 [DOI] [PubMed] [Google Scholar]
- 214.Singh VP, Sharma J, Babu S, Rizwanulla, Singla A. Role of probiotics in health and diseases: a review. J Pak Med Assoc. (2013) 63:253–7. [PubMed] [Google Scholar]
- 215.Tsigalou C, Stavropoulou E, Bezirtzoglou E. Current insights in microbiome shifts in Sjogren's syndrome and possible therapeutic interventions. Front. Immunol. (2018) 9:1106. 10.3389/fimmu.2018.01106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Sales-Campos H, Soares SC, Oliveira CJF. An introduction of the role of probiotics in human infections and autoimmune diseases. Crit Rev Microbiol. (2019) 45:413–32. 10.1080/1040841X.2019.1621261 [DOI] [PubMed] [Google Scholar]
- 217.Cox AJ, Pyne DB, Saunders PU, Fricker PA. Oral administration of the probiotic Lactobacillus fermentum VRI-003 and mucosal immunity in endurance athletes. Br J Sports Med. (2010) 44:222–6. 10.1136/bjsm.2007.044628 [DOI] [PubMed] [Google Scholar]
- 218.French PW, Penny R. Use of probiotic bacteria as an adjuvant for an influenza vaccine. Int J Probiotics Prebiotics. (2009) 4:175−80. [Google Scholar]
- 219.Lei WT, Shih PC, Liu SJ, Lin CY, Yeh TL. Effect of probiotics and prebiotics on immune response to influenza vaccination in adults: a systematic review and meta-analysis of randomized controlled trials. Nutrients. (2017) 9:E1175. 10.3390/nu9111175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Isolauri E, Arvola T, Sutas Y, Moilanen E, Salminen S. Probiotics in the management of atopic eczema. Clin Exp Allergy. (2000) 30:1604–10 23. 10.1046/j.1365-2222.2000.00943.x [DOI] [PubMed] [Google Scholar]
- 221.Yan F, Li N, Shi J, Li H, Yue Y, Jiao W, et al. Lactobacillus acidophilus alleviates type 2 diabetes by regulating hepatic glucose, lipid metabolism and gut microbiota in mice. Food Funct. (2019) 10:5804–15. 10.1039/C9FO01062A [DOI] [PubMed] [Google Scholar]
- 222.Raoult D. Probiotics and obesity: a link? Nat Rev Microbiol. (2009) 7:616. 10.1038/nrmicro2209 [DOI] [PubMed] [Google Scholar]
- 223.Lawrence T. The nuclear factor NF-κB pathway in inflammation. Cold Spring Harb Perspect Biol. (2009) 1:a001651. 10.1101/cshperspect.a001651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Bron PA, Kleerebezem M, Brummer RJ, Cani PD, Mercenier A, MacDonald TT, et al. Can probiotics modulate human disease by impacting intestinal barrier function? Br J Nutr. (2017) 117:93–107. 10.1017/S0007114516004037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Pharmacist's Lett. (2012) 28:280707. [Google Scholar]
- 226.Graf C, Sarasin FP. Probiotiques: efficacité et dangerosité. Rev Med Suisse. (2007) 3:32635. [PubMed] [Google Scholar]
- 227.Boumis E, Capone A, Galati V, Venditti C, Petrosillo N. Probiotics and infective endocarditis in patients with hereditary hemorrhagic telangiectasia: a clinical case and a review of the literature. BMC Infect Dis. (2018) 18:65. 10.1186/s12879-018-2956-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Bezirtzoglou E. Intestinal cytochromes P450 regulating the intestinal microbiota and its probiotic profile. Microb Ecol Health Dis. (2012) 23:1–10. 10.3402/mehd.v23i0.18370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Stavropoulou E, Bezirtzoglou E. Human microbiota in aging and infection: a review. Crit Rev Food Sci Nutr. (2019) 59:537–45. 10.1080/10408398.2017.1379469 [DOI] [PubMed] [Google Scholar]
- 230.Rogers GB, Narkewicz MR, Hoffman LR. The CF gastrointestinal microbiome: structure and clinical impact. Pediatric Pulmonol. (2016) 51:S35–44. 10.1002/ppul.23544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Karlsson M, Scherbak N, Reid G, Jass J. Lactobacillus rhamnosus GR-1 enhances NF-kappaB activation in Escherichia coli-stimulated urinary bladder cells through TLR4. BMC Microbiol. (2012) 12:15. 10.1186/1471-2180-12-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Haghighi HR, Gong J, Gyles CL, Hayes MA, Zhou H, Sanei B, et al. Probiotics stimulate production of natural antibodies in chickens. Clin Vaccine Immunol. (2006) 13:975–80. 10.1128/CVI.00161-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Rocha-Ramírez LM, Pérez-Solano RA, Castañón-Alonso SL, Moreno Guerrero SS, Ramírez Pacheco A, García Garibay M, et al. Probiotic Lactobacillus strains stimulate the inflammatory response and activate human macrophages. J Immunol Res. (2017) 2017:4607491. 10.1155/2017/4607491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Mathipa MG, Thantsha MS. Probiotic engineering: towards development of robust probiotic strains with enhanced functional properties and for targeted control of enteric pathogens. Gut Pathog. (2017) 9:28. 10.1186/s13099-017-0178-9 [DOI] [PMC free article] [PubMed] [Google Scholar]