Abstract
The coronavirus 2019 disease (COVID-19) pandemic emerged at a time of substantial investment in the United States substance use service infrastructure. A key component of this fiscal investment was funding for training and technical assistance (TA) from the Substance Abuse and Mental Health Services Administration (SAMHSA) to newly configured Technology Transfer Centers (TTCs), including the Addiction TTCs (ATTC Network), Prevention TTCs (PTTC Network), and the Mental Health TTCs (MHTTC Network). SAMHSA charges TTCs with building the capacity of the behavioral health workforce to provide evidence-based interventions via locally and culturally responsive training and TA. This commentary describes how, in the wake of the COVID-19 pandemic, TTCs rapidly adapted to ensure that the behavioral health workforce had continuous access to remote training and technical assistance. TTCs use a conceptual framework that differentiates among three types of technical assistance: basic, targeted, and intensive. We define each of these types of TA and provide case examples to describe novel strategies that the TTCs used to shift an entire continuum of capacity building activities to remote platforms. Examples of innovations include online listening sessions, virtual process walkthroughs, and remote “live” supervision. Ongoing evaluation is needed to determine whether virtual TA delivery is as effective as face-to-face delivery or whether a mix of virtual and face-to-face delivery is optimal. The TTCs will need to carefully balance the benefits and challenges associated with rapid virtualization of TA services to design the ideal hybrid delivery model following the pandemic.
Keywords: COVID-19, Workforce development, Behavioral health, Technology Transfer Centers
1. Introduction
The coronavirus 2019 disease (COVID-19) pandemic emerged at a time of substantial investment in the United States substance use service infrastructure. Between 2017 and 2019, Congress released $3.3 billion dollars in grants to scale up substance use prevention, treatment, and recovery efforts in an attempt to curtail the overdose epidemic (Goodnough, 2019). A key component of this fiscal investment was funding for training and technical assistance (TA) from the Substance Abuse and Mental Health Services Administration (SAMHSA) to newly configured Technology Transfer Centers (TTCs), including the Addiction TTCs (ATTC Network), Prevention TTCs (PTTC Network), and Mental Health TTCs (MHTTC Network). To ensure the modernization of the behavioral health service system, SAMHSA charges TTCs with building the capacity of the behavioral health workforce to provide evidence-based interventions via locally and culturally responsive training and TA (McCance-Katz, 2018).
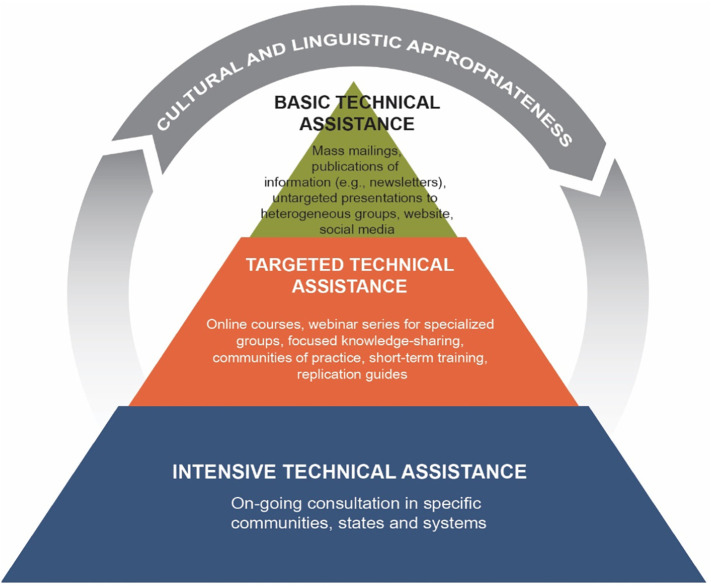
In March 2020, the COVID-19 pandemic upended the United States healthcare system, and challenged the behavioral health workforce in unprecedented ways. To meet the needs of the workforce, TTCs had to rapidly innovate to provide training and TA without service disruption. Fig. 1 presents a conceptual framework of the types of TA that the TTCs provided, which builds upon definitions of TA from the National Implementation Research Network (Fixsen et al., 2009) and U.S. Department of Education (2020). Each TA type is depicted as a layer in a pyramid, with the size reflecting the intensity and resource investment required. The arch over the pyramid indicates that TA provision should be grounded in culturally and linguistically appropriate practices. This commentary describes strategies that the TTCs used to shift an entire continuum of capacity building activities, spanning all three layers of the TA pyramid, to remote service delivery. Additionally, we consider how innovations in remote service delivery present new opportunities for TA provision.
Fig. 1.
Three tiers of technical assistance that the Technology Transfer Centers provide.
2. TA types and innovations during COVID-19
TTCs apply different TA strategies based on circumstances, need, and appropriateness (Powell et al., 2015) and consider training (i.e., conducting educational meetings) as a discrete activity that can be provided as part of any TA effort. TTCs are guided by extensive evidence that strategies beyond training are required for practice implementation and organizational change (Edmunds et al., 2013), underscoring the critical need for virtual TA in the wake of the COVID-19 pandemic. In May 2020, we surveyed all 39 U.S.-based TTCs to identify example innovations in each layer of the TA pyramid that the COVID-19 necessitated. Thirty-five TTCs (90%) across three networks (PTTC N = 13; ATTC N = 13; MHTTC N = 9) responded, representing both regional and national TTCs.
2.1. Basic TA
Basic TA is information dissemination or the provision of brief consultations. TCCs typically deliver basic TA to large audiences and focus on building awareness and knowledge. Common basic TA activities for untargeted audiences include conferences, brief consultation, and web-based lectures (i.e., webinars). TTCs reported a surge in requests for basic TA during the COVID-19 pandemic and responded with a significant increase in dissemination of information (i.e., best practice guidelines), as well as brief consultations to support interpretation of such information. TTCs emphasized virtual content curation, organizing content to enhance usability. Additionally, TTCs employed novel delivery channels, such as live streaming, pre-recorded videos, podcasts, and webinars with live transcription, to reach wide audiences. Another practice innovation was online listening sessions in which health professionals convened around a priority topic. For instance, two national TTCs co-hosted a series of listening sessions titled “Emerging Issues around COVID-19 and Social Determinants of Health” that experimented with “flipping the typical script” by first having participants engage in conversation and then having expert presenters address emergent topics via brief didactics. This series, which was not sequential or interconnected, built knowledge and awareness around evolving workforce needs.
2.2. Targeted TA
Targeted TA is the provision of directed training or support to specific groups (e.g., clinical supervisors) or organizations (e.g., prevention coalitions) focused on building skill and promoting behavior change. Targeted TA encompasses activities customized for specific recipients such as didactic workshop trainings, learning communities, and communities-of-practice. Due to the focus on provider skill-building, targeted TA often relies on experiential learning activities such as role plays and behavioral rehearsal (Edmunds et al., 2013). To transition targeted TA online, TTCs reduced didactic material to the minimum necessary; spread content over several sessions; and leveraged technology to foster interaction among small groups. For example, one regional TTC transformed a face-to-face, multi-day motivational interviewing skills-building series by moving the delivery to a multi-week virtual learning series. This TTC kept participants engaged by limiting the time for each session to 1–2 h, utilizing the full capabilities of videoconferencing platforms (e.g., small breakout rooms and interactive polling), and extending learning through SMS text messages containing reminders of core skills.
2.3. Intensive TA
Intensive TA is defined as ongoing, customized consultation to specific sites, communities, or systems to support full incorporation of a new practice or innovation into real world settings. Intensive TA includes a range of implementation supports, including site visits, ongoing consultation, live supervision, performance feedback, and practice facilitation. Because the focus is on sustainable implementation of a novel practice, intensive TA providers must have a deep understanding of organizational workflow, staffing models, and barriers and facilitators to implementation (Chambers et al., 2013). TTCs accomplished this virtually by replacing in-person workflow mapping and live supervision. To illustrate, one regional TTC had an intensive TA initiative focused on helping opioid treatment programs implement contingency management: this initiative was transformed by having a staff member at each program conduct a “virtual walkthrough” to demonstrate their workflow, followed by use of video- and/or tele-conferencing to allow an expert in contingency management to observe live session delivery.
3. Challenges to transitioning to virtual TA models
COVID-19 necessitated a rapid shift to remote training and TA that has expanded the possibilities for engaging the behavioral health prevention, treatment, and recovery workforce. TTCs reported increased convenience and decreased costs as two major advantages of remote TA. Virtual TA allowed trainers and service providers to connect without extensive travel or disruption to their routine. Yet TTCs also described challenges with remote TA, including inequitable access to those with insufficient equipment and bandwidth and disparate levels of attendee comfort and familiarity with technology, particularly in rural areas (see UN News, 2020). TTCs also described “Zoom fatigue” (Sander & Bauman, 2020) and the need to incorporate multiple learning platforms (e.g., live video, phone, pre-recorded sessions). Benefits and challenges of virtual service provision also varied by TA type: requests for and attendance at basic TA events surged, while requests for intensive TA decreased, likely due to the level of sustained engagement required of TA recipients.
4. Future directions
TTCs are currently analyzing systematic differences in the types and content of TA that the three TTC networks provide, to identify areas of convergence and divergence across the addiction, prevention, and mental health networks. For TTCs, ongoing evaluation will help to determine whether virtual delivery is as effective as face-to-face delivery or whether a mix of virtual and face-to-face delivery is optimal. TTCs will need to carefully balance benefits and challenges associated with rapid virtualization of TA services to design the ideal hybrid delivery model post-pandemic.
Acknowledgments
The co-chairs of the Cross Technology Transfer Center (TTC) Workgroup receive funding via the following grants from the Substance Abuse and Mental Health Services (SAMHSA): TI080205 (PI: Krom) and TI080209 (PI: Becker). The views summarized in this commentary represent those of the workgroup members and do not necessarily represent the views of SAMHSA or the U.S. Department of Health and Human Services, and should not be construed as such.
Footnotes
Authors' note: This commentary was drafted by the Cross-Technology Transfer Center (TTC) Workgroup on Virtual Learning. The Cross-TTC Workgroup on Virtual Learning is comprised of multiple representatives from the TTCs funded by the Substance Abuse and Mental Health Services Administration (SAMHSA). Membership in the workgroup does not guarantee authorship on academic products. The following workgroup members directly contributed to the conceptualization, interpretation of data, and review of this commentary (in alphabetical order): Sara Becker PhD, Brown University School of Public Health, Michael Chaple PhD, New York State Psychiatric Institute, Tom Freese PhD, UCLA Integrated Substance Abuse Programs, Holly Hagle PhD, University of Missouri-Kansas City School of Nursing and Health Studies, Maxine Henry MSW, MBA, National Latino Behavioral Health Association, Igor Koutsenok MD, MS, University of California, San Diego, Laurie Krom MS, University of Missouri-Kansas City School of Nursing and Health Studies, Rosemarie Martin PhD, Brown University School of Public Health, Todd Molfenter PhD, University of Wisconsin-Madison, Kristen Powell MSW, PhD, Rutgers School of Social Work, Nancy Roget MS, MFT, LADC, University of Nevada, Reno, Laura Saunders MSW, University of Wisconsin-Madison, Isa Velez PsyD, CATP, Universidad Central del Caribe, Ruth Yanez MSW, National Latino Behavioral Health Association.
Correspondence regarding this article should be sent to Sara J. Becker, Ph.D., Associate Professor, Center for Alcohol and Addictions Studies, Brown University School of Public Health, sara_becker@brown.edu. The views and opinions contained within this document do not necessarily reflect those of SAMHSA or the U.S. Department of Health and Human Services and should not be construed as such.
References
- Chambers D.A., Glasgow R.E., Stange K.C. The dynamic sustainability framework: Addressing the paradox of sustainment amid ongoing change. Implementation Science. 2013;8(1):117. doi: 10.1186/1748-5908-8-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmunds J.M., Beidas R.S., Kendall P.C. Dissemination and implementation of evidence–based practices: Training and consultation as implementation strategies. Clinical Psychology: Science and Practice. 2013;20(2):152–165. doi: 10.1111/cpsp.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fixsen D.L., Blase K.A., Naoom S.F., Van Dyke M., Wallace F. Implementation: The missing link between research and practice. NIRN Implementation Brief. 2009;1:218–227. [Google Scholar]
- Goodnough A. New York Times; 2019. States are making progress on opioids. Now the money that is helping them may dry up. https://www.nytimes.com/2019/07/16/health/opioids-grants-treatment-addiction.html
- McCance-Katz E.F. The Substance Abuse and Mental Health Services Administration (SAMHSA): New directions. Psychiatric Services. 2018;69(10):1046–1048. doi: 10.1176/appi.ps.201800281. [DOI] [PubMed] [Google Scholar]
- Powell B.J., Waltz T.J., Chinman M.J., Damschroder L.J., Smith J.L., Matthieu M.M.…Kirchner J.E. A refined compilation of implementation strategies: Results from the Expert Recommendations for Implementing Change (ERIC) project. Implementation Science. 2015;10(1):21. doi: 10.1186/s13012-015-0209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sander L., Bauman O. Zoom fatigue is real – Here is why video calls are so draining. 2020. https://ideas.ted.com/zoom-fatigue-is-real-heres-why-video-calls-are-so-draining/ Website.
- U.S. Department of Education Office of Special Education and Rehabilitative Services: Technical assistance centers and demonstration projects. 2020. https://www2.ed.gov/about/offices/list/osers/rsa/ta-centers.html Website.
- UN News Startling disparities in digital learning emerge as COVID-19 spreads: UN education agency. 2020. https://news.un.org/en/story/2020/04/1062232 Website.