Abstract
Background
The present study was designed to verify the accuracy of the noninvasive biomarkers enolase/Cr, CA125, and CA19-9 as a clinical diagnostic tool for the detection of endometriosis.
Methods
A cross-sectional study was performed at Rasool-e-Akram Hospital affiliated to Iran University of Medical Sciences, Tehran, Iran, from April 2015 to April 2018. Eighty-six women were scheduled to undergo laparoscopy due to chronic pelvic pain, infertility, pelvic mass, and abnormal uterine bleeding. Serum and urine samples of all patients were collected preoperatively. Serum levels of CA125 and CA19-9, and urine levels of enolase-1 were measured. Serum levels of CA125 and CA19-9 were determined by the electrochemiluminescence method (ECL). Urinary enolase-1 was measured by the ELISA method.
Result
Serum levels of CA125 and CA19-9 were significantly higher in the endometriosis group than in controls (p < 0.001, p = 0.004, respectively). Levels of enolase I and enolase/Cr were higher in patients with endometriosis, but the differences were not statistically significant. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of combined enolase/Cr, CA125, and CA19-9 were 65%, 66.6%, 71%, and 60.1%, respectively. The positive likelihood ratio (PLR) and negative likelihood ratio (NLR) of combined enolase/Cr, CA125, and CA19-9 was 1.94 and 0.52, respectively. The area under the ROC curve for enolase/Cr + CA125 + CA19 − 9 was 0.675 (95% confidence interval 0.573-0.710).
Conclusion
The present study revealed that concurrent measurement of enolase-1, CA125, and CA19-9 might be a valuable noninvasive test for the identification of endometriosis.
1. Introduction
Endometriosis is an estrogen-dependent disorder that severely affects the health and quality of life of 10% of women of reproductive age [1, 2]. Endometriosis causes infertility and debilitating symptoms such as dysmenorrhea, dyspareunia, dyschezia, and dysuria [3–5]. The gold standard for the diagnosis of endometriosis is direct visualization of a lesion in laparoscopy and histological confirmation of suspicious lesions in biopsy specimens [6]. The invasive nature of laparoscopy and the ambiguous symptoms tend to delay the diagnosis [7]. Due to the progressive nature of endometriosis, any delay in its diagnosis or treatment is liable to have severe consequences for the patient [8], including impairment of the patient's quality of life [9]. The greater burden of symptoms signifies much higher healthcare costs [10] and also reduces the patient's reproductive potential and fertility [11].
The discovery of a sufficiently sensitive and specific biomarker for nonsurgical detection of endometriosis would permit early diagnosis as well as prevent harmful sequelae of the disease [12]. As endometriosis is linked with a number of potentially confounding factors, the development of a noninvasive biomarker has been a challenging issue [13]. Despite various studies, no single biomarker or panel of biomarkers in peripheral blood or urine has been confirmed as a diagnostic test for endometriosis [14–16]. A review of the published literature suggests that an extremely high CA125 level combined with a high CA19-9 level is a possible indicator of endometriosis [17]. These tests may well be useful for the diagnosis of endometriosis, particularly deep infiltrating endometriosis (DIE) [18]. However, the power of the tests is considered low because they are unspecific. Besides, the tests are used to detect ovarian tumors as well [17, 19, 20]. In view of the fact that surgery is expensive and ridden with risks, and the validity of blood biomarkers has not been confirmed yet, some authors have investigated biomarkers in other body fluids such as saliva, peritoneal fluid [21, 22], and urine for their ability to detect endometriosis noninvasively [16].
A reliable urine examination could lead to the diagnosis of endometriosis without surgery or could eliminate the need for diagnostic surgery [16]. Elevated urinary enolase I levels have been claimed to be a determinant of endometriosis [12, 23], but other studies have shown that there is too little evidence to recommend any urinary biomarker alone for use in clinical practice [12, 16]. Some authors have employed a combination of biomarkers for the diagnosis of endometriosis [23]. Yun et al. reported that elevated urinary enolase, in conjunction with serum CA-125, may be used as a potential biomarker for endometriosis [23]. In view of the poor diagnostic accuracy of some biomarkers in the diagnosis of endometriosis [16], the present study was designed to verify the accuracy of the noninvasive biomarkers enolase/Cr, CA125, and CA19-9 as a clinical diagnostic tool for endometriosis.
2. Materials and Methods
This cross-sectional study was performed in Rasool-e-Akram Hospital, a tertiary care center, from April 2015 to April 2018. The investigation was approved by the committee of science and research ethics at the Iran University of Medical Science (IR.IUMS.REC 1395.95-01-204-27483).
Women who were candidates for diagnostic or operative laparoscopy due to an ovarian cyst, pelvic pain, infertility, suspicious endometriosis, or abnormal uterine bleeding were eligible for the study. The following inclusion criteria were used: (1) age 15-45 years; (2) no use of hormones or gonadotropin-releasing hormone agonists (GnRHa) during the preceding 3 months; (3) no underlying diseases such as infection, autoimmune disease, or cardiovascular conditions. Women who were diagnosed with gynecological diseases other than endometriosis (adenomyosis, malignancy, uterine polyp, acute or chronic inflammatory condition, endometrial hyperplasia) during surgery were excluded from the study.
General demographic data including age, weight, height, body mass index (BMI, kg/m2), marital status, gravidity, parity, abortion, smoking status, menstrual phase, menstrual pattern, and infertility history were either obtained directly from the patients or extracted from their medical records. The menstrual phase (proliferative and luteal phase) was determined on the basis of the published literature [24]. Urine and blood samples were taken from all patients preoperatively. For measurement of enolase-1, a urine sample (20 mL) was taken in a sterile plastic container after the induction of anesthesia and bladder catheterization. The urine sample was centrifuged at 1000 × g for 10 minutes in order to obtain sediment-free urine samples. The latter were stored at −70° Celsius until analysis [12]. The concentration of enolase-1 in urine was measured in ng/cc, using an ELISA kit according to the manufacturer's protocols (USCN Life Science & Technology Company, Missouri, TX), with a minimum detectable concentration of 0.312 ng/cc. Urine creatinine (Cr) levels were measured with commercial ELISA assays, and enolase-Cr levels were determined by the following formula: enolase-1/urinary Cr.
For measurement of CA19-9 and CA125 levels, blood samples were taken and centrifuged for 5 minutes with the serum withdrawn, and frozen at −80°C until analysis. Serum levels of CA19-9 and CA125 (U/mL) were measured using the electrochemiluminescence immunoassay on the Roche Cobas 6000 analyzer (Roche Diagnostics, Mannheim, Germany). All experiments were performed in a single laboratory.
All patients underwent laparoscopic surgery. Suspicious endometriotic lesions were excised during the operation and the patients were assigned to the endometriosis group or the control group after histological confirmation (Figure 1). The stage of endometriosis was determined according to the revised classification of the American Society of Reproductive of Medicine [25].
Figure 1.
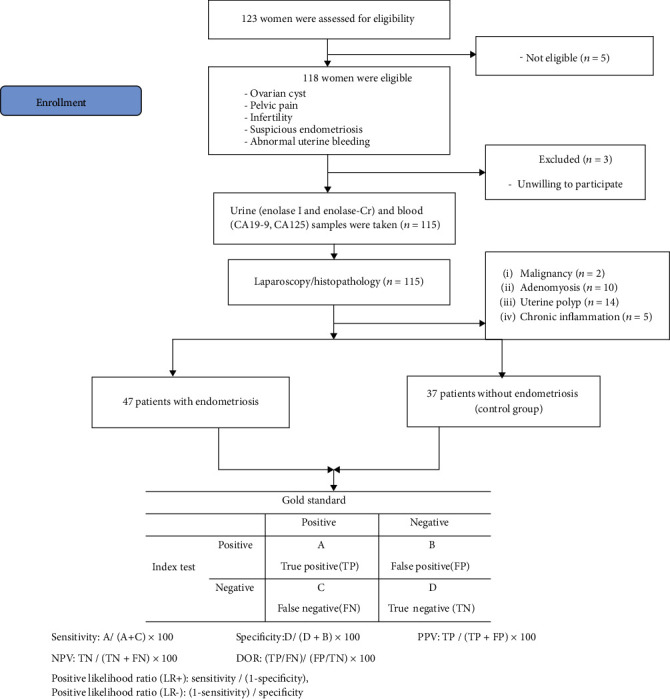
Diagram of the study.
The primary outcome of the study was the diagnostic accuracy of the individual tests enolase/Cr, CA125, and CA19-9, and their combined application, as a clinical diagnostic tool for the determination of endometriosis. Associations between the patients' clinical characteristics and their biomarker levels were regarded as secondary outcomes.
2.1. Statistical Analysis
Commercially available software (IBM SPSS Statistics version 22; IBM, Chicago, IL, USA) was used for data analysis. Descriptive statistics (mean ± standard deviation) were used to present the data. The Shapiro-Wilk test showed that the data were not normally distributed. Data were also tested for geographical normality using the Q-Q plot and were found to be not normally distributed because of their nonlinear pattern. Therefore, nonparametric tests were used for analysis. The Mann-Whitney U test and the AVONA test were used to assess differences between the study groups. The chi-square test or the Fisher exact test was used to assess categorical variables. Diagnostic test analysis was applied to determine the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (PLR), and negative likelihood ratio (NLR) of the test. The usefulness of the test was established by the area under the ROC curve (AUC). Receiver-operator characteristics (ROC) of the combined marker (urinary enolase/Cr, and serum CA125, and CA19-9) were computed by plotting sensitivity vs. 1-specificity. All comparisons were based on a significance level of p < 0.05.
3. Results
Of 115 patients who underwent laparoscopy, 31 had a pathology of malignancy, adenomyosis, a uterine polyp, or chronic inflammation and were therefore excluded from the study. Endometriosis was confirmed in 47 patients and not confirmed in 37 patients. Women without endometriosis were regarded as controls. Ultimately, the data of 84 patients were eligible for analysis (Figure 1). No significant differences were observed between groups in regard to age, BMI, marital status, gravities, parity, abortion, smoking status, menstrual phase, menstrual pattern, infertility history, and urine creatinine levels. 61.7% (n = 29) of patients with endometriosis were operated in the follicular phase. Of 37 patients in the control group, 7 had a functional cyst, 6 had a dermoid cyst, 4 a hydrosalpinx, 7 a para ovarian cyst, 10 were infertile, and 3 patients had a serous cystadenoma. The patients' clinical characteristics are summarized in Table 1.
Table 1.
Clinical characteristics of the patients.
(a).
| Variable | Endometriosis group (n = 47) | Controls (n = 37) | p value | ||
|---|---|---|---|---|---|
| Min.-max. | Means ± SD | Min.-max. | Means ± SD | ||
| Age (years) | 18-44 | 32.4 ± 6.2 | 17-40 | 32.1 ± 7.3 | 0.942∗ |
| BMI (kg/m2) | 18-34 | 25.2 ± 3.8 | 18-40 | 26.7 ± 4.8 | 0.194∗ |
| Cr | 25-557 | 173† (113) †† | 35-601 | 147† (133) †† | 0.885∗ |
(b).
| Frequency (percent) | Frequency(percent) | |||
|---|---|---|---|---|
| Marital status | Single | 7 (14.9) | 4 (10.8) | 0.415∗∗ |
| Married | 40 (85.1) | 33 (89.2) | ||
| Gravidity | 0 | 23 (48.9) | 11 (29.7) | 0.199∗∗ |
| 1 | 11 (23.4) | 11 (29.7) | ||
| 2-5 | 13 (27.7) | 15 (40.5) | ||
| Parity | 0 | 24 (51.1) | 13 (35.1) | 0.201∗∗ |
| 1 | 14 (29.8) | 11 (29.7) | ||
| 2-5 | 9 (19.1) | 13 (35.1) | ||
| Abortion | 0 | 41 (87.2) | 32 (86.5) | 0.585∗∗ |
| 1-2 | 6 (12.8) | 5 (13.5) | ||
| Smoking | Yes | 0 (0) | 1 (2.8) | 0.440∗∗ |
| No | 47 (100) | 36 (97.2) | ||
| Stage of endometriosis | 1 | 1 (2.1) | — | — |
| 2 | 7 (14.9) | — | ||
| 3 | 12 (25.5) | — | ||
| 4 | 27 (57.5) | — | ||
| Menstrual phase | Follicular phase | 29 (61.7) | 20 (54) | 0.511∗∗ |
| Luteal phase | 18 (38.3) | 17 (46) | ||
| Menstrual pattern | Regular | 29 (61.7) | 21 (56.7) | 0.806∗∗ |
| Irregular | 17 (36.2) | 16 (43.3) | ||
| Amenorrhea | 1 (2.1) | 0 | ||
| Infertility | Yes | 19 (40.4) | 12 (32.4) | 0.501∗∗ |
| No | 28 (59.6) | 25 (67.6) | ||
∗Results of the Mann-Whitney U test; ∗∗results of the chi-square test or the Fisher exact test, † median, †† IQR.
Urinary enolase-Cr was higher in patients with endometriosis than in controls, but the difference was not statistically significant (p = 0.106). Mean serum levels of CA125 were significantly higher in the endometriosis group than in controls (62.0 IU/mL versus 11.0 IU/mL) (p < 0.001). Likewise, mean serum levels of CA19-9 were higher in the endometriosis group than in controls (10.4 IU/ml versus 3.0 IU/mL). This difference was statistically significant (p = 0.004).
Urine and blood markers in patients with endometriosis and controls are shown in Table 2.
Table 2.
Urine and blood markers in patients with endometriosis and controls.
| Group | N | Urinary enolase 1 ng/cc | Enolase-Cr ng/mg of Cr |
CA125 (IU/mL) | CA19-9 (IU/mL) | |
|---|---|---|---|---|---|---|
| Endometriosis | 47 | Median (1st, 3rd quartiles) | 1300.9 (757.5,2434.2) | 8.2 (4.8,18.6) | 62.0 (33.3,162.0) | 10.4 (1.5,45.0) |
| Min-max | 68.5-8250 | 026-105 | 5-655 | 0.1-138 | ||
| Controls | 37 | Median (1st, 3rd quartiles) | 1132.5 (434.2,1754.4) | 6.98 (3.0,11.4) | 11.0 (6.59,19.0) | 3.0 (1.25,9.93) |
| Min.-max. | 23.2-7350 | 0.34-51 | 4-407 | 0.3-31.9 | ||
| ∗ p value | 0.080 | 0.106 | <0.001 | 0.004 |
∗The Mann–Whitney U test was used.
Sensitivity, specificity, PPV, NPV, PLR, and NLR were determined for the individual and combined biomarkers of endometriosis; the results are summarized in Table 3. The sensitivity of combined enolase/Cr + CA125 + CA19 − 9 (65%) was higher than that of enolase/Cr alone (44.3%). However, the NPV of enolase/Cr alone was higher than that of combined enolase/Cr + CA125 + CA19 − 9 (83.5% vs. 60.1%). The PLR and NLR of combined enolase/Cr + CA125 + CA19 − 9 were 1.94 and 0.52, respectively (Table 3).
Table 3.
AUC, sensitivity, specificity, PPV, NPV, +LR, and -LR of individual and combined markers for endometriosis.
| Marker | ROC-AUC | Sensitivity | Specificity | Positive predictive value | Negative predictive value | Positive likelihood ratio | Negative likelihood ratio |
|---|---|---|---|---|---|---|---|
| (95% CI) | |||||||
| Enolase-Cr | 0.443 (0.317-0.569) | 97.8 (88.7-99.9) | 13.5 (4.5-28.8) | 58.9 (55.94-62.27) | 83.3 (36.91-99.26) | 1.13 (0.8-52.0) | 0.16 (0.1-1.0) |
| CA125 | 0.220 (0.117-0.322) | 69.5 (54.2-82.3) | 86.5 (71.2-95.5) | 86.4 (73.37-93.6) | 69.5 (59.14-78.23) | 5.11 (1.8-5.5) | 0.35 (0.08-0.4) |
| CA19-9 | 0.359 (0.241-0.476) | 27.6 (15.6-42.6) | 100 (90.5-100.0) | 100 (90.1-100.0) | 52.1 (47.74-56.52) | — | 0.72 (0.2-1.6) |
| Enolase/Cr + CA125 + CA19 − 9 | 0.675 (0.573-0.710) | 65 (56.5-72.9) | 66.6 (57.1-75.3) | 71 (64.69-76.57) | 60.1 (53.82-66.28) | 1.94 (1.5-5.5) | 0.52 (0.4-0.7) |
The cut-off values for urinary enolase 1, enolase-Cr, CA125, and CA19-9 were 1181 ng/mL, 0.96 ng/mg Cr, 35 IU/mL, and 37 IU/mL, respectively. Abbreviations: ROC-AUC: areas under the receiver operating characteristic curves.
An ROC analysis was performed to distinguish endometriosis from other conditions. The ROC analysis was also used to evaluate the diagnostic performance of combined enolase/Cr + CA125 + CA19 − 9.
Table 3 shows the areas under the ROC (ROC-AUC) curves for the individual markers and combinations of biomarkers for all stages of endometriosis. Of the individual markers, enolase/Cr had an ROC-AUC of 0.443, and the combination of enolase/Cr + CA125 + CA19 − 9 had ROC-AUCs of 0.675 for all stages of endometriosis (Table 3 and Figure 2).
Figure 2.
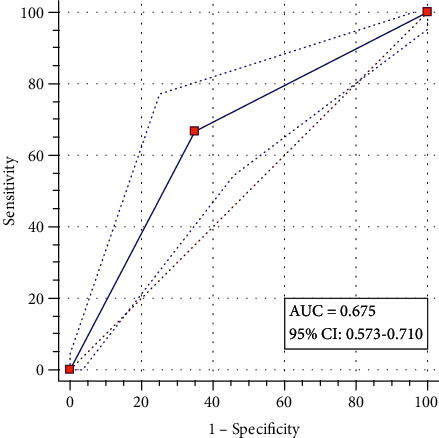
ROC-AUC curve for combined enolase/Cr + CA125 + CA19 − 9 as a test for the detection of endometriosis.
The ROC analysis was also used to determine the severity of endometriosis and evaluate the diagnostic performance of combined enolase/Cr + CA125 + CA19 − 9.
The ROC-AUC (0.763) for combined enolase/Cr + CA125 + CA19 − 9 showed that it was possible to distinguish between severe (stage III and IV) and mild (stage I and II) endometriosis (Table 4).
Table 4.
Individual and combined markers of endometriosis: ROC-AUCs for the severity of endometriosis (n = 47).
| Variable | N (%) | ROC-AUC | ||||
|---|---|---|---|---|---|---|
| Enolase-Cr | CA125 | CA19-9 | Enolase/Cr + CA125 + CA19 − 9 | |||
| Stage of endometriosis | Stage I + II | 8 (17) | 0.480 (0.283-0.678) | 0.516 (0.345-0.716) | 0.470 (0.206-0.683) | 0.690 (0.492-0.839) |
| Stage III + IV | 39 (83) | 0.601 (0.468-0.756) | 0.653 (0.461-0.700) | 0.589 (0.500-0.739) | 0.763 (0.578-0.878) | |
Abbreviations: ROC-AUC: area under the receiver operating characteristic curves.
Associations between the clinical characteristics of patients with endometriosis and marker levels are shown in Table 5. Women with endometriosis had higher enolase/Cr levels in the luteal phase than in the follicular phase (21.8 ± 5.8 ng/mg Cr versus 11.3 ± 2.5 ng/mg Cr) (p = 0.039). The mean difference was -10.5 (95% CI -21.7-0.6).
Table 5.
Marker levels and clinical characteristics of patients with endometriosis (n = 47).
| Variable | N (%) | Urinary enolase 1 ng/mL | Enolase-Cr (ng/mg Cr) | CA125 (IU/mL) | CA19-9 (IU/mL) | |
|---|---|---|---|---|---|---|
| Mean ± SD | ||||||
| Age (years) | <30 | 17 (36.2) | 1672 ± 467 | 19 ± 6.5 | 129.3 ± 33.3 | 34.2 ± 10 |
| 30–39 | 20 (42.6) | 1668 ± 288 | 12.8 ± 3.2 | 129.8 ± 35.4 | 27.4 ± 8.4 | |
| ≥40 | 10 (21.3) | 2585 ± 626 | 14 ± 2.6 | 62.7 ± 20.9 | 18.8 ± 6.5 | |
| p value | — | 0.610∗ | 0.567∗ | 0.378∗ | 0.509∗ | |
| BMI (kg/m2) | <24.9 | 20 (42.6) | 2125 ± 454 | 15.69 ± 5.5 | 114 ± 27.9 | 39.8 ± 9.9 |
| ≥24.9 | 27 (57.4) | 1672 ± 272 | 15.11 ± 2.6 | 116 ± 28.1 | 19.3 ± 5 | |
| p value | — | 0.493∗∗ | 0.345∗∗ | 0.420∗∗ | 0.176∗∗ | |
| Stage of endometriosis | Stage I + II | 8 (17) | 1727 ± 943 | 11.47 ± 6.2 | 104.8 ± 42.4 | 15.9 ± 9 |
| Stage III + IV | 39 (83) | 1933 ± 254 | 16.16 ± 3.1 | 117.5 ± 22.5 | 30.5 ± 6 | |
| p value | — | 0.819∗∗ | 0.575∗∗ | 0.795∗∗ | 0.274∗∗ | |
| CA125 (35 U/mL) | ≤35 | 14 (29.8) | 1948 ± 553 | 16 ± 4.4 | — | 5.46 ± 0.98 |
| >35 | 33 (70.2) | 1814 ± 269 | 15 ± 3.5 | — | 34.27 ± 11.3 | |
| p value | — | 0.567∗∗ | 0.378∗∗ | — | <0.001∗∗ | |
| Menstrual phase | Follicular phase | 29 (61.7) | 1430 ± 207 | 11.3 ± 2.5 | 135.7 ± 29.2 | 28.1 ± 5.9 |
| Luteal phase | 18 (38.3) | 2565 ± 523 | 21.8 ± 5.8 | 82.6 ± 20.3 | 28 ± 10.1 | |
| p value | — | 0.017∗∗ | 0.039∗∗ | 0.091∗∗ | 0.712∗∗ | |
| Infertility | Yes | 19 (40.4) | 2101 ± 420 | 16.9 ± 3.8 | 93.2 ± 19.1 | 26.2 ± 7.6 |
| No | 28 (59.6) | 1704 ± 305 | 14.3 ± 3.9 | 130 ± 30.7 | 29.3 ± 7.3 | |
| p value | — | 0.480∗∗ | 0.503∗∗ | 0.422∗∗ | 0.885∗∗ | |
∗Results of the ANOVA test; ∗∗results of the Mann-Whitney U test.
There was no association between urinary enolase-Cr, CA 125, and CA19-9 levels on the one hand, and the patients' age, BMI, endometriosis stage, and infertility on the other hand (Table 5).
4. Discussion
Endometriosis has debilitating effects, including infertility and pain [3], which disrupts the patients' quality of life [23]. A sufficiently sensitive and specific biomarker for nonsurgical detection of endometriosis will enable clinicians to diagnose the condition early. The present study was designed to verify the accuracy of combined enolase/Cr + CA125 + CA19 − 9 as a diagnostic tool for endometriosis. A number of authors have reported on non-invasive biomarkers for endometriosis, determined from blood, urine, the eutopic endometrium, the peritoneum, as well as epigenetic markers of the endometrium [13, 14, 21, 23, 26–29]. The diagnostic accuracy of the tests has been shown in some studies but has not been conclusively proven yet [14, 21, 29].
The present investigation revealed higher levels of urinary enolase-Cr, CA-125, and CA19-9 levels in patients with endometriosis than in controls. In line with our findings, some studies have reported elevated serum levels of CA125, CA19-9 [17, 30, 31], and enolase-1 in women with endometriosis [12, 16, 23]. In Yun and coworkers' study, enolase-Cr levels were significantly higher in patients with endometriosis (1.25 ng/mg Cr vs. 0.75 ng/mg Cr) than in those without endometriosis. The underlying reason for increased levels of urinary enolase-1 is obscure [23]. Some authors state that the inflammatory process and hypoxia occurring in endometriotic lesions lead to hyper-expression of enolase-1 in renal tubules, causing secretion to urine [23, 27]. As for blood biomarkers, some studies have shown that inflammatory reactions in endometriosis lead to an alternation of endothelial permeability, and biomarkers enter the bloodstream. Thus, there will be a higher concentration of biomarkers in the ectopic endometrium than in the entopic endometrium [32].
Although in some studies have been reported that endometriosis is significantly associated with elevated serum CA19-9 and CA125 concentrations [15, 17, 33, 34], the diagnostic value of serum CA125 and CA19-9 concentration in endometriosis therefore remains unclear [30]. It has been reported that CA19-9 is elevated further in the more advanced stages of endometriosis [15]. The CA 19-9 is a pentasaccharide with carbohydrate ingredients including fructose components, and it belongs to a group of oncofetal antigens. In the fetal period, it is synthesized in the epithelial structures of the stomach, and its production is significantly decreased by adulthood. As well as recent studies report that CA 19-9 may be produced by glandular structures of the pancreas, gall bladder, bronchus, and some gynecological tumors [15]. Some studies show that CA-19-9 may be demonstrably elevated in endometriosis and show the same or decreased sensitivity as CA-125 [15, 17, 33].
In the present study, the sensitivity of enolase/Cr for identifying women with endometriosis was 97.8%, which was higher than the sensitivity of CA125 (69.5%), and much higher than the sensitivity of CA19-9 (27.5%). In Yun and coworkers' study, the sensitivity of normalized urine enolase-1 (enolase/Cr) was 76.9% for the diagnosis of endometriosis [23].
A wide range of data have been published about the sensitivity of enolase/Cr, CA125, and CA19-9 for the detection of endometriosis [18, 23, 30]. In the present study, the sensitivity of CA125 in the detection of endometriosis was 69.5%. CA 125 was reported to possess a higher sensitivity of 63% (95% CI, 42% to 77%) in the presence of severe disease. In the present study, the majority of women with endometriosis had stage III or IV disease. In line with previously reported data, we found that CA19-9 had the lowest sensitivity for the detection of endometriosis [24, 35].
Although urinary enolase 1, enolase/Cr, CA 125, and CA19-9 levels are increased in women with endometriosis, these parameters alone are reported to possess no diagnostic power [12, 14, 15, 23]. Therefore, in the present study, we used a combination of enolase-Cr, CA-125, and CA19-9 for the diagnosis of endometriosis. The sensitivity and specificity of the combined biomarkers in the detection of endometriosis were 65% and 66.6%, respectively. In line with our data, Yun and coworkers reported a sensitivity and specificity of 76.9% and 85.0%, respectively, for combined enolase I and CA-125 [23]. In the present study, the PPV and NPV of combined enolase-Cr, CA-125, and CA19-9 in women with endometriosis were 71% and 60.1%, respectively. The majority of researchers believe that the main parameters of a screening test are PPV and NPV. However, it should be noted that PPV and NPV depend on the population being tested and the technical characteristics of the screening test [25].
In the present study, although the diagnostic power of urinary enolase-Cr was lower than that of serum CA-125 for the detection of endometriosis, when combined with serum CA-125 and CA19-9, the AUC was increased to 0.675 (95% CI 0.573-0.710). Consistent with these data, in Yun and coworkers' study, the AUC of urinary enolase-Cr for the detection of endometriosis was 0.621 (95% CI 0.476–0.765), while the AUC of combined enolase I and CA-125 increased to 0.821 (95% CI 0.713–0.928) [23]. Any value between 0 and 1 is reported to be a good indicator of the accuracy of a test. The AUC value of 0.6-0.7 proved the sufficient diagnostic accuracy of the test [36]. Based on our data, we conclude that the combination of enolase/Cr, CA125, and CA19-9 is a sufficiently accurate and valid test for the detection of endometriosis.
The present study revealed that combined biomarkers possess greater sensitivity and specificity, and greater diagnostic power for the detection of endometriosis [23, 37, 38]. Urinary enolase-Cr may serve as one of several combined biomarkers for the detection of endometriosis in the future [16, 23].
As a secondary outcome, we noted that patients with endometriosis had significantly higher enolase-1 and enolase/Cr levels in the luteal phase than in the follicular phase. Analogously, Yun and coworkers reported significantly higher urinary enolase-1 and enolase/Cr levels in the secretory phase than in the follicular phase [23]. Further larger studies are needed to confirm the role of NNE in detecting endometriosis [16].
An ideal noninvasive test should have a high sensitivity and good specificity in patients with endometriosis. Easy and noninvasive detection of endometriosis would be a noteworthy achievement in preventing the progression of endometriosis, provide more options for planning the patient's treatment (medical or surgical), and help to determine the best time for administering the treatment. Although the present study yielded important data, it was limited by the small sample size. The data will have to be confirmed and proven in larger controlled studies.
5. Conclusion
The diagnosis and treatment of endometriosis are demanding because the symptoms vary. To date, laparoscopy is the gold standard for the diagnosis of endometriosis. Given the current ambiguity about various aspects of the condition, a period of 12 years may elapse between the onset of symptoms and the definitive diagnosis of endometriosis. It would be useful to consider the biomarkers addressed in the present study for early detection and better treatment of endometriosis. Despite the limited sample size, the present study showed that the combination of enolase-Cr, CA125, and CA19-9 levels enhances the individual diagnostic power of these tests for the detection of endometriosis. However, larger studies will be needed to evaluate the diagnostic potential of this combination.
Acknowledgments
The authors wish to thank the women who kindly agreed to participate in the study. We extend our special thanks to the Iran University of Medical Science for their technical support of this research project. This study was funded by Iran University of Medical Science, Tehran, Iran (Grant number 95-01-204-27483).
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Consent
Informed consent was obtained from all participants of the study.
Conflicts of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- 1.Tamaresis J. S., Irwin J. C., Goldfien G. A., et al. Molecular classification of endometriosis and disease stage using high-dimensional genomic data. Endocrinology. 2014;155(12):4986–4999. doi: 10.1210/en.2014-1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehdizadeh Kashi A., Moradi Y., Chaichian S., et al. Application of the world health organization quality of life instrument, short form (WHOQOL-BREF) to patients with endometriosis. Obstetrics & Gynecology Science. 2018;61(5):598–604. doi: 10.5468/ogs.2018.61.5.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.D'Hooghe T., Hummelshoj L. Multi-disciplinary centres/networks of excellence for endometriosis management and research: a proposal. Human Reproduction. 2006;21(11):2743–2748. doi: 10.1093/humrep/del123. [DOI] [PubMed] [Google Scholar]
- 4.AlKudmani B., Gat I., Buell D., et al. In vitro fertilization success rates after surgically treated endometriosis and effect of time interval between surgery and in vitro fertilization. Journal of Minimally Invasive Gynecology. 2018;25(1):99–104. doi: 10.1016/j.jmig.2017.08.641. [DOI] [PubMed] [Google Scholar]
- 5.Mettler L., Ruprai R., Alkatout I. Impact of medical and surgical treatment of endometriosis on the cure of endometriosis and pain. BioMed Research International. 2014;2014:9. doi: 10.1155/2014/264653.264653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nisenblat V., Bossuyt P. M., Farquhar C., Johnson N., Hull M. L. Imaging modalities for the non-invasive diagnosis of endometriosis. The Cochrane Database of Systematic Reviews. 2016;2, article CD009591 doi: 10.1002/14651858.CD009591.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taylor H. S., Adamson G. D., Diamond M. P., et al. An evidence-based approach to assessing surgical versus clinical diagnosis of symptomatic endometriosis. International Journal of Gynecology & Obstetrics. 2018;142(2):131–142. doi: 10.1002/ijgo.12521. [DOI] [PubMed] [Google Scholar]
- 8.D'Hooghe T. M., Debrock S. Endometriosis, retrograde menstruation and peritoneal inflammation in women and in baboons. Human Reproduction Update. 2002;8(1):84–88. doi: 10.1093/humupd/8.1.84. [DOI] [PubMed] [Google Scholar]
- 9.Nnoaham K. E., Hummelshoj L., Webster P., et al. Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertility and Sterility. 2011;96(2):366–73.e8. doi: 10.1016/j.fertnstert.2011.05.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Surrey E., Soliman A. M., Trenz H., Blauer-Peterson C., Sluis A. Impact of Endometriosis Diagnostic Delays on Healthcare Resource Utilization and Costs. Advances in Therapy. 2020;37(3):1087–1099. doi: 10.1007/s12325-019-01215-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parasar P., Ozcan P., Terry K. L. Endometriosis: epidemiology, diagnosis and clinical management. Current Obstetrics and Gynecology Reports. 2017;6(1):34–41. doi: 10.1007/s13669-017-0187-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fassbender A., Vodolazkaia A., Saunders P., et al. Biomarkers of endometriosis. Fertility and Sterility. 2013;99(4):1135–1145. doi: 10.1016/j.fertnstert.2013.01.097. [DOI] [PubMed] [Google Scholar]
- 13.Ahn S. H., Singh V., Tayade C. Biomarkers in endometriosis: challenges and opportunities. Fertility and Sterility. 2017;107(3):523–532. doi: 10.1016/j.fertnstert.2017.01.009. [DOI] [PubMed] [Google Scholar]
- 14.Fassbender A., Dorien O., de Moor B., et al. Endometriosis. Springer; 2014. Biomarkers of Endometriosis; pp. 321–339. [DOI] [Google Scholar]
- 15.Fassbender A., Burney R. O., Dorien F. O., D’Hooghe T., Giudice L. Update on biomarkers for the detection of endometriosis. BioMed Research International. 2015;2015:14. doi: 10.1155/2015/130854.130854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu E., Nisenblat V., Farquhar C., Fraser I., Bossuyt P. M., Johnson N., et al. Urinary biomarkers for the non-invasive diagnosis of endometriosis. The Cochrane Database of Systematic Reviews. 2015;23(12, article CD012019) doi: 10.1002/14651858.CD012019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harada T., Kubota T., Aso T. Usefulness of CA19-9 versus CA125 for the diagnosis of endometriosis. Fertility and Sterility. 2002;78(4):733–739. doi: 10.1016/S0015-0282(02)03328-9. [DOI] [PubMed] [Google Scholar]
- 18.Oliveira M. A. P., Raymundo T. S., Soares L. C., Pereira T. R. D., Demoro A. V. E. How to use CA-125 more effectively in the diagnosis of deep endometriosis. BioMed Research International. 2017;2017, article 9857196:6. doi: 10.1155/2017/9857196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hirsch M., Duffy J., Davis C. J., Nieves Plana M., Khan K. S. Diagnostic accuracy of cancer antigen 125 for endometriosis: a systematic review and meta-analysis. BJOG. 2016;123(11):1761–1768. doi: 10.1111/1471-0528.14055. [DOI] [PubMed] [Google Scholar]
- 20.Kennedy S., Bergqvist A., Chapron C., et al. ESHRE guideline for the diagnosis and treatment of endometriosis. Human Reproduction. 2005;20(10):2698–2704. doi: 10.1093/humrep/dei135. [DOI] [PubMed] [Google Scholar]
- 21.El-Kasti M. M., Wright C., Fye H. K., Roseman F., Kessler B. M., Becker C. M. Urinary peptide profiling identifies a panel of putative biomarkers for diagnosing and staging endometriosis. Fertility and Sterility. 2011;95(4):1261–1266.e6. doi: 10.1016/j.fertnstert.2010.11.066. [DOI] [PubMed] [Google Scholar]
- 22.Gueye N.-A., Stanhiser J., Valentine L., Kotlyar A., Goodman L., Falcone T. Biomarkers for Endometriosis. Springer; 2017. Biomarkers for Endometriosis in Saliva, Urine, and Peritoneal Fluid; pp. 141–163. [DOI] [Google Scholar]
- 23.Yun B. H., Lee Y. S., Chon S. J., et al. Evaluation of elevated urinary enolase I levels in patients with endometriosis. Biomarkers. 2013;19(1):16–21. doi: 10.3109/1354750X.2013.863973. [DOI] [PubMed] [Google Scholar]
- 24.AL-Tai T. H., AL-Hadithi H. S., Abdulsalam H. S. CA19-9 versus CA-125 in Endometriosis. Journal of Dental and Medical Sciences. 2014;13(4):27–30. doi: 10.9790/0853-13432730. [DOI] [Google Scholar]
- 25.Goetzinger K. R., Odibo A. O. Statistical analysis and interpretation of prenatal diagnostic imaging studies, part 1: evaluating the efficiency of screening and diagnostic tests. Journal of Ultrasound in Medicine. 2011;30(8):1121–1127. doi: 10.7863/jum.2011.30.8.1121. [DOI] [PubMed] [Google Scholar]
- 26.He P., Naka T., Serada S., et al. Proteomics-based identification of α-enolase as a tumor antigen in non-small lung cancer. Cancer Science. 2007;98(8):1234–1240. doi: 10.1111/j.1349-7006.2007.00509.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gitlits V. M., Toh B.-H., Sentry J. W. Disease association, origin, and clinical relevance of autoantibodies to the glycolytic enzyme enolase. Journal of Investigative Medicine. 2001;49(2):138–145. doi: 10.2310/6650.2001.34040. [DOI] [PubMed] [Google Scholar]
- 28.Gajbhiye R., Bendigeri T., Ghuge A., et al. Panel of Autoimmune Markers for Noninvasive Diagnosis of Minimal-Mild Endometriosis. Reproductive Sciences. 2017;24(3):413–420. doi: 10.1177/1933719116657190. [DOI] [PubMed] [Google Scholar]
- 29.Cho S., Choi Y. S., Yim S. Y., et al. Urinary vitamin D-binding protein is elevated in patients with endometriosis. Human Reproduction. 2012;27(2):515–522. doi: 10.1093/humrep/der345. [DOI] [PubMed] [Google Scholar]
- 30.Shen A., Xu S., Ma Y., et al. Diagnostic value of serum CA125, CA19-9 and CA15-3 in endometriosis: a meta-analysis. Journal of International Medical Research. 2015;43(5):599–609. doi: 10.1177/0300060515583076. [DOI] [PubMed] [Google Scholar]
- 31.Somigliana E., Viganò P., Tirelli A. S., et al. Use of the concomitant serum dosage of CA 125, CA 19-9 and interleukin-6 to detect the presence of endometriosis. Results from a series of reproductive age women undergoing laparoscopic surgery for benign gynaecological conditions. Human Reproduction. 2004;19(8):1871–1876. doi: 10.1093/humrep/deh312. [DOI] [PubMed] [Google Scholar]
- 32.Seeber B., Sammel M. D., Fan X., et al. Panel of markers can accurately predict endometriosis in a subset of patients. Fertility and Sterility. 2008;89(5):1073–1081. doi: 10.1016/j.fertnstert.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 33.Fiala L., Bob P., Raboch J. Oncological markers CA-125, CA 19-9 and endometriosis. Medicine. 2018;97(51, article e13759) doi: 10.1097/MD.0000000000013759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hirsch M., Duffy J. M. N., Deguara C. S., Davis C. J., Khan K. S. Diagnostic accuracy of Cancer antigen 125 (CA125) for endometriosis in symptomatic women: a multi-center study. European Journal of Obstetrics, Gynecology, and Reproductive Biology. 2017;210:102–107. doi: 10.1016/j.ejogrb.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 35.Speer L. CA 125 Relatively Specific for Diagnosing Endometriosis. American Family Physician. 2017;95(2) [Google Scholar]
- 36.Šimundić A.-M. Measures of diagnostic accuracy: basic definitions. Ejifcc. 2009;19(4):203–211. [PMC free article] [PubMed] [Google Scholar]
- 37.Vodolazkaia A., El-Aalamat Y., Popovic D., et al. Evaluation of a panel of 28 biomarkers for the non-invasive diagnosis of endometriosis. Human Reproduction. 2012;27(9):2698–2711. doi: 10.1093/humrep/des234. [DOI] [PubMed] [Google Scholar]
- 38.Mihalyi A., Gevaert O., Kyama C. M., et al. Non-invasive diagnosis of endometriosis based on a combined analysis of six plasma biomarkers. Human Reproduction. 2010;25(3):654–664. doi: 10.1093/humrep/dep425. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.


