Abstract
The recent COVID pandemic has had a major effect on anatomic pathology specimen volumes across the country. The effect of this pandemic on a subspecialty academic practice is presented. We used a data-driven approach to monitor the changing workloads in a granular fashion and dynamically adjust the scheduling of faculty and histology staff accordingly to minimize the number of people present on-site. At the peak of the pandemic locally, the main hospital in our health system had 450 COVID-positive inpatients. The surgical pathology specimen volume dropped to 13% of the pre-pandemic levels, and this occurred about 2 weeks before the peak of the inpatient census; cytology specimens (the majority of which are outreach gynecological) dropped to approximately 5% of the pre-pandemic volume, 4 weeks before the peak inpatient census. All of the surgical subspecialty services showed a significant decrease in volume, with hematopathology being the least affected (dropped to 30% of the pre-pandemic level). The genitourinary surgical subspecialty service (predominantly prostate and bladder biopsies) was the most affected (dropped to 1% of the pre-pandemic level) but was fastest to return as clinical operations began to return to normal. The only specimen type which showed a significant increase in turnaround time during the pandemic was our gynecologic cytology specimens and that occurred as the specimen volume returned. This was due to stay-at-home directives for the cytotechnologists and the fact that some of them were retasked to participate in our SARS-CoV-2 testing.
Keywords: anatomic pathology, COVID, SARS-CoV-2, specimen volumes, subspecialty, workload
Introduction
The recent COVID pandemic and the accompanying redirection of health care resources has had a major effect on anatomic pathology specimen volumes across the country. The closure of operating rooms, clinics, and physician offices; the need to commit multiple inpatient units to treating COVID patients; and the “stay-at-home” mandates to the population in general substantially compromised the acquisition and thus submission of specimens for pathologic evaluation. Although the impact of COVID on biosafety in anatomic pathology has been reported,1,2 as well as the response of an autopsy and mortuary service to the pandemic,3 the effect of COVID on a subspecialty surgical pathology and cytopathology operation has not been examined. Herein, we report a single-institution experience in a region of the United States that was heavily impacted by COVID at the outset of the national pandemic.
The Anatomic Pathology Division in our department receives specimens both from within the health system and from physician offices (outreach). We operate as a subspecialty system, although the majority of the faculty sign out on 2 or more subspecialty services. To address faculty manpower needs during the pandemic, we monitored daily specimen volumes and histology volumes, as well as weekly volumes by subspecialty (daily monitoring by subspecialty produced noisy data because of day-to-day variations in when particular surgical teams operated, and which days clinics were held or canceled). Average values for January and February were used as a baseline for comparison.
Materials and Methods
Daily inpatient census for the hospitals in our health system was obtained initially from daily emails sent to all members of the medical staff each morning and later was obtained from a web-based dashboard developed by the health system and drawing data from our electronic medical record system (Epic Hyperspace; Epic Systems Corporation). Census counts at approximately 8 am each morning were used. All other data presented were extracted from our anatomic pathology laboratory information system (CoPath Plus; Cerner Corporation) which had been customized locally4: (a) we have a custom morgue management module which tracks all hospital deaths and documents the cause of death for each patient as recorded on the death certificate; (b) we have a custom histology asset tracking module5 which records all histology events on each block and slide: for block counts, the day of the “embed” event was used; (c) we use CoPath’s “User Specimen” dictionary to record, for each specimen, the pathology subspecialty service which ultimately signs out each case. Data for analysis were extracted directly from the back-end database (Sybase Adaptive Server Enterprise 15.1; Sybase Inc; acquired by SAP America in 2010) using an SQL query tool (DB Solo 5.2.5; DB Solo LLC) running on a Macintosh Computer (Apple Computer). Extracted data were transferred to Microsoft Excel (Microsoft Corporation) for further analysis and to produce graphs of the data.
Results
Our region of the country (Connecticut) was significantly impacted by the SARS-CoV-2 pandemic; daily reported case incidence in the state peaked on April 13.6 In keeping with the reported several-day delay from the time of a positive test result for an ambulatory patient to hospitalization,7 on April 21, 2020, the main hospital in our health system peaked at 450 COVID-positive inpatients; the health system overall had just under 800 COVID-positive inpatients at this time (Figure 1A). So far, there is no indication of a resurgence or second wave of cases.6 As of the writing of this article, 216 deaths at our main hospital have been attributed to COVID-19 or SARS-CoV-2-related disease (Figure 1B), with the age and sex distribution shown (Figure 1C), consistent with what has been reported by the United States Centers for Disease Control.8
Figure 1.

Impact of the COVID-19 pandemic on the local health system. A, Daily counts of admitted patients with a diagnosis of COVID-19-related disease. Blue bars are the counts at the main hospital, and others represent affiliated hospitals. The peak census occurred on April 21, 2020. B, Daily counts of patient deaths at the main hospital (fetal deaths are excluded). Red bars indicate patients whose death certificate indicated a COVID-19- or SARS-CoV-2-related death. C, Breakdown of COVID-19-related deaths by patient age and sex.
Because of how we capture and store information in our anatomic pathology laboratory information system, and in particular the tracking of specimens by subspecialty sign-out service, we were able to monitor the changing workloads in a granular fashion and dynamically adjust the scheduling of faculty accordingly to minimize the number of people present on-site and the duration of their time on-site. Our laboratory information system also included custom morgue and histology tracking modules, allowing monitoring of daily deaths and histology information in addition to specimen information.
Surgical specimen volume, both from within the health system and from our outreach, dropped rapidly beginning in the third week of March 2020, bottoming out by the end of the first week in April (Figure 2A) at approximately 13% of our normal volume. This was a full 2 weeks before the peak COVID-positive census within the health system. Interestingly, histology volume, measured as the number of blocks embedded each day, showed a somewhat delayed and biphasic drop in volume (Figure 2B). The initial drop was to approximately half the typical volume during the fourth and fifth weeks in March. Using blocks per case as a metric of case complexity, during this period, the average number of blocks per case rose from 5 to 9 (Figure 2C). The most common specimens received during this period were major cancer resections and margins, as well as prostate core needle biopsies and bone marrow biopsies. Then, beginning in early April, a second drop in the histology volume occurred, and the average number of blocks per case dropped to just above 3 per case; this persisted through the first week of May. The most common specimens received during this period were placentas (volume did not change with the pandemic) and bone marrow biopsies (hematopathology was the least affected by the pandemic; see below). As specimen volume began to return in mid-May, the case-mix largely returned to normal, as suggested by the return to an average of 5 blocks per case. Throughout this entire period, the average number of blocks per case for the outreach specimens remained constant at about 2 (Figure 2C). Turnaround time remained essentially constant throughout this period.
Figure 2.

Impact of the COVID-19 pandemic on surgical pathology volumes. Light bars represent hospital-based specimens, and dark bars represent outreach specimens. Average daily data from January and February of 2020 are shown at the left for comparison. A, Daily counts of total specimens (cases) accessioned during the pandemic. B, Daily counts of blocks embedded in the main and outreach histology labs. C, Weekly counts of the average number of tissue blocks submitted per case (all parts) based on the date the specimen/case was accessioned.
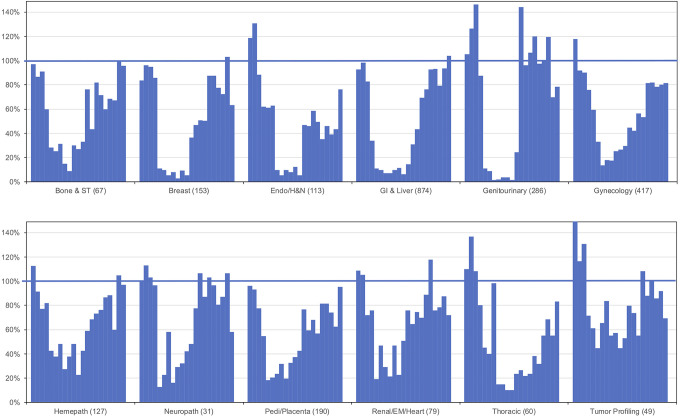
With respect to the surgical subspecialty services, a number of clinical services moved aggressively to see patients in the first few weeks of March, anticipating the closures of the operating rooms and clinics. This resulted in a temporary increase in specimen volume from endocrine/head/neck, the genitourinary service (comprised mostly of prostate biopsies), and thoracic surgery (Figure 3). Tumor profiling also saw an initial push in March. Then, most of the biopsy heavy services saw a precipitous drop with the closure of the clinics, with the genitourinary service falling to less than 1% of their typical volumes (benchmarked to average weekly part volumes for January and February 2020; Figure 3). This service was also the fastest to recover when clinics began to reopen in the second week of May. The services least affected by the pandemic were hematopathology and the tumor profiling service, which only dropped to 30% and 50%, respectively, of their typical volume. The pediatric service also did not drop below 20% of normal due to the continued receipt of placentas throughout the pandemic. The pattern of volume recovery differed across the services, some recovering very quickly and others far more gradually. The surgical services that have been the slowest to recover are endocrine/head/neck (much of this surgery was moved to an affiliated hospital during the pandemic) and thoracic. The majority of the pathology subspecialty services have returned to approximately 80% or more of their pre-pandemic levels.
Figure 3.
Weekly loss and return of surgical pathology specimen volume by subspecialty area. Data represent weekly counts of total specimen parts accessioned from the week of February 24, 2020, to the week of July 13, 2020. Because volumes varied greatly from subspecialty to subspecialty, data are shown as a percentage of the benchmark for each subspecialty, determined from averages from January and early February 2020. Benchmark values (part counts) are shown in parentheses after the name of each surgical pathology subspecialty area.
The majority of our gynecological cervical cytology specimens come from our outreach clients. Volume on that service took a major but more gradual drop beginning in early March and reaching its nadir in the second week of April at 3% of the typical pre-pandemic volume (Figure 4A). This reflected the closing of outside physician offices. In contrast, the majority (approximately two-thirds) of the nongynecologic cytology material is from within the health care system; these volumes fell to only 20% of the normal levels, and at the lowest point, health care specimens represented 80% of the nongynecologic volume (Figure 4B).
Figure 4.

Impact of the COVID-19 pandemic on cytology volumes. Light bars represent hospital-based specimens, and dark bars represent outreach specimens. Average daily data from January and February of 2020 are shown at the left for comparison. A, Daily counts of total gynecologic cytology specimens accessioned during the pandemic. B, Daily counts of total nongynecologic cytology specimens accessioned during the pandemic.
Discussion
As patient units within the hospital were converted to house COVID-19 patients, similar to what was occurring in New York City immediately to the west of Connecticut,9 many surgical floors were temporarily eliminated, and as such, the number of surgeries being performed dropped significantly. The rise in the average number of blocks examined per surgical specimen received (Figure 2C) indicates that initially it was the less complex elective surgeries which were canceled, with continuing of the major cancer resections (as well as prostate biopsies, as this was one of the last clinics to close). The average number of blocks per case did not change for our outreach material, consistent with these being almost exclusively biopsy specimens.
The subspecialty services least affected by the pandemic were hematopathology and tumor profiling. For hematopathology, most of the specimens received were bone marrow biopsies, a procedure that does not require the operating rooms and performed on patients who were often already in the hospital. The medical renal service was also less affected than some of the other services, presumably for the same reason. The relative persistence of tumor profiling work reflected initially the fact that there is often a lag between initial diagnosis and request for molecular testing and subsequently the fact that oncology was often looking for nonsurgical therapies to offer patients at a time when minimal surgeries were taking place. Of course, the pediatric and placenta service continued to receive placentas in normal numbers throughout the pandemic. This is a relevant point, since placental examination of deliveries from SARS-CoV-2-infected mothers10 or infants born during the COVID-19 pandemic11 might have reflected an altered demographic of our maternal population but did not appear to do so.
The departmental chair, vice chairs, and business manager met (remotely) each morning to monitor changing policies and workloads during the pandemic, and a “daily briefing” email was sent to all members of the department. As the workload began to return, additional individuals representing various groups within the workforce were added to the meeting, and the meeting frequency gradually decreased until the meetings were held only weekly. Manpower present on site was adjusted dynamically throughout the pandemic, using the specimen and histology volume data. For the faculty, most of the busier subspecialty services which had more than 1 pathologist on at a time were collapsed to a single attending present, noting that all case sign-out was done on-site and not remotely. Although consideration was given to combining some of the smaller volume subspecialty services, not all of our faculty were comfortable signing out all services, and it was decided to allow each subspecialty team to still function independently, with pathologists working only partial days as needed for the reduced specimen volume. Departmental medical leadership continued to work full days throughout the pandemic, partially to continue to monitor and adjust to the changing workflow, but also to recognize those individuals who did come to work. Residents were divided into teams so that, should one get sick, the entire group would not be exposed. Approximately one-third of the residents remained at home on “jeopardy.” Those coming to work covered their normally assigned services. For the other services, the attending signed out with just the fellow or without any trainee. In the histology laboratory, histotechnologists were split into 2 teams working on an every-other-day schedule. On a daily basis, the number of technologists actually called in on any given day was determined at 5 pm the day before, based on the total count of submitted blocks which was available from the dashboard of our in-house custom histology asset tracking system. As the work volume slowly returned through May and June, staff were increasingly called back to work. A tracing system was implemented to keep track of which employees were present at work each day, in the event that an employee subsequently tested positive.
Although all of the abovementioned measures were put into place to minimize the impact of a potential outbreak among the staff, their effectiveness was never actually tested. During this pandemic, only a handful of departmental employees ever tested positive for the SARS-CoV-2 virus, all of which occurred in individuals who were working exclusively from home; none of these acquisitions or transmissions occurred while at work. This is potentially important information, since the source of SARS-CoV-2 infection in health care workers is a topic of intense discussion.12,13
The only service which suffered a prolongation of the turnaround time during the pandemic was gynecologic cytology (Pap smears). This occurred not during the peak of the crisis but rather as the specimen volume started to return. This was due to a number of factors: stay-at-home directives from the university (cytotechnologists are university employees at our institution), reluctance of staff to work overtime, and the fact that a number of the cytotechnologists were retasked to work in our SARS-CoV-2 testing lab, decreasing their availability to screen Pap smears. There was no significant change in the turnaround time for nongynecologic cytology specimens, which were given priority, or for the surgical specimens.
One area which, in retrospect, could have been handled better is communication between operating room planning and pathology. During the reopening phase, the institution decided to move some of the surgical subspecialty teams (and their patients) to affiliated hospital campuses within the health care network. This was largely done without notification of pathology. Although this did not have a major impact on the attending staff (because slides routinely move about within our network and were transferred to the main campus for sign out), it did have implications for frozen sections and for the histology workload. Pathologists at an affiliated campus began seeing a larger volume of frozen sections in subspecialties in which they had more limited experience. In addition, while the histology volume at the main campus lab recovered slowly and in conjunction with the increasing specimen volume, the histology volume in the lab at an affiliated campus saw a rapid increase in the number of blocks to a level nearly 50% higher than normal, and this persisted for approximately 2 months before returning to normal levels as the surgical teams relocated to the main campus (data not shown). Clearly, in the future, better communication between surgery planning and pathology will be needed, and it is likely that pathology will need to initiate and drive that communication.
The use of modeling to predict pathology workload based on operative schedules has been reported14 and may in the future provide a supplemental approach to planning histology and pathologist staffing levels when there are significant changes in the operative volumes.
Undoubtedly, many of the details of the changes in workload presented here are specific to our institution and to the shutdown and reopening policies both of the institution(s) and of the state. However, it is hoped that other pathology practices will find these data and analysis helpful in benchmarking their own experiences. Other states which are not as far along in the recovery process may still benefit from this information, and it may also be helpful in planning for a possible second wave of cases in the fall.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: John H. Sinard  https://orcid.org/0000-0001-8739-517X
https://orcid.org/0000-0001-8739-517X
References
- 1. Lamas NJ, Esteves S, Alves JR, et al. The anatomic pathology laboratory adjustments in the era of COVID-19 pandemic: the experience of a laboratory in a Portuguese central hospital. Ann Diagn Pathol. 2020;48:151560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dietzel S, May EF, Fried H, et al. A joint action in times of pandemic: the German bioimaging recommendations for operating imaging core facilities during the SARS-CoV-2 emergency. Cytometry. 2020. doi:10.1002/cytoa.24178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McGuone D, Gill JR, Masters A, et al. Autopsy services and emergency preparedness of a tertiary academic hospital mortuary for the COVID-10 public health emergency: the Yale plan. Adv Anat Pathol. 2020. [DOI] [PubMed] [Google Scholar]
- 4. Sinard JH, Gershkovich P. Custom software development for use in a clinical laboratory. J Pathol Inform. 2012;3:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pantanowitz L, Mackinnon AC, Sinard JH. Tracking in anatomic pathology. Arch Pathol Lab Med. 2013;137:1798–1810. [DOI] [PubMed] [Google Scholar]
- 6. Connecticut COVID-19 Data Tracker. Daily data report for Connecticut. Published 2020 Accessed August 19, 2020 https://portal.ct.gov/-/media/Coronavirus/CTDPHCOVID19summary8182020.pdf
- 7. Reichberg S, Mitra PP, Haghamad A, et al. Rapid emergence of SARS-CoV-2 in the greater New York metropolitan area: geolocation, demographics, positivity rates, and hospitalization for 46, 793 persons tested by Northwell Health. Clin Infect Dis. 2020:ciaa922 doi:10.1093/cid/ciaa922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. CDC COVID—Response Team. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:382–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Richardson S, Hirsch J, Narasimhan M. Presenting characteristics, comorbidities and outcomes for 5700 patients hospitalized with COVID-19 in the New York City area. J Am Med Assoc. 2020. doi:10.1001/jama.2020.6775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yoon SH, Kang JM, Ahn JG. Clinical outcomes of 201 neonates born to mothers with COVID-19: a systematic review. Eur Rev Med Pharmacol Sci. 2020;24:7804–7815. [DOI] [PubMed] [Google Scholar]
- 11. Hedermann G, Hedley PL, Hansen MB, et al. Danish premature birth rates during the COVID-19 lockdown. Arch Dis Child Fetal Neonatal Ed. 2020. doi:10.1136/archdischild-2020-319990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Moscola J, Sembajwe G, Jarrett M, et al. Prevalence of SARS-CoV-2 antibodies in health care personnel in the New York city area. J Am Med Assoc. 2020. doi:10.1001/jama.2020.14765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Barrett ES, Horton DB, Roy J, et al. Prevalence of SARS-CoV-2 infection in previously undiagnosed health care workers at the onset of the U.S. COVID-19 epidemic. 2020. medRxiv. doi:10.1101/2020.04.20.20072470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Vanlandingham DM, Hampton W, Thompson KM, Badizadegan K. Modeling pathology workload and complexity to manage risks and improve patient quality and safety. Risk Anal. 2020;40:421–434. [DOI] [PubMed] [Google Scholar]