Abstract
Digital whole slide images are Food and Drug Administration approved for clinical diagnostic use in pathology; however, integration is nascent. Trainees from 9 pathology training programs completed an online survey to ascertain attitudes toward and experiences with whole slide images for pathological interpretations. Respondents (n = 76) reported attending 63 unique medical schools (45 United States, 18 international). While 63% reported medical school exposure to whole slide images, most reported ≤ 5 hours. Those who began training more recently were more likely to report at least some exposure to digital whole slide image training in medical school compared to those who began training earlier: 75% of respondents beginning training in 2017 or 2018 reported exposure to whole slide images compared to 54% for trainees beginning earlier. Trainees exposed to whole slide images in medical school were more likely to agree they were comfortable using whole slide images for interpretation compared to those not exposed (29% vs 12%; P = .06). Most trainees agreed that accurate diagnoses can be made using whole slide images for primary diagnosis (92%; 95% CI: 86-98) and that whole slide images are useful for obtaining second opinions (93%; 95% CI: 88-99). Trainees reporting whole slide image experience during training, compared to those with no experience, were more likely to agree they would use whole slide images in 5 years for primary diagnosis (64% vs 50%; P = .3) and second opinions (86% vs 76%; P = .4). In conclusion, although exposure to whole slide images in medical school has increased, overall exposure is limited. Positive attitudes toward future whole slide image diagnostic use were associated with exposure to this technology during medical training. Curricular integration may promote adoption.
Keywords: digital whole slide imaging, virtual microscopy, pathology training, medical education, optical microscopy, digital pathology
Introduction
There is a nascent shift in the field of pathology and laboratory medicine toward integrating digital whole slide images (WSI) for surgical pathology and medical diagnosis following Food and Drug Administration (FDA) approval of the first whole slide imaging system for primary diagnosis in 2017.1,2 Further developments in scanning systems and viewing software are expected to arrive quickly.3,4 However, studies indicate there are lengthy delays in adopting new technologies into clinical practice.5-7 Education of future pathologists, as they transition from medical students to practicing pathologists during residency training, is a potential driver of future uptake and utilization of digital pathology.
Navigating a digital WSI is quite different from traditional microscopy.8 The pathologist is not confined to a physical microscope requiring manual manipulation of a glass slide viewed through a set of ocular lenses to provide varied magnification of the tissue biopsy. Rather, the digitized images of the histology tissue sections are viewed on a computer screen using a pointing device such as a mouse, trackpad, or dedicated console to manipulate location and magnification of the image (pan and zoom). The technology may be easily adapted to virtual reality glasses.9-11 Given these important differences between digital WSI and traditional microscopy, adoption and effective use of WSI in clinical practice requires exposure to and training using this new format.
The future integration and deployment of digital WSI may be influenced by whether trainees are exposed to WSI during medical school and subsequent pathology residency training. While both the Liaison Committee on Medical Education, the accrediting body for US medical schools granting an MD degree, and the AOA Commission on Osteopathic College Accreditation, the accrediting body for the DO degree have general requirements for pathology education, neither includes specific requirements for training that include digital WSI. A few institutions have examined the efficacy of digital slides as a teaching tool,12-14 whether students favor one method over the other,15,16 and whether students’ performance and competence were improved with adoption of whole slide imaging in the curriculum.16-18 The existing literature does not include the extent to which formal exposure to WSI is provided during medical school and subsequent pathology training. In addition, information on pathology trainees’ perspective on adoption of this new technology into clinical practice is missing.
To address this knowledge gap, we surveyed US pathology trainees with medical degrees from a wide variety of United States and international medical schools about the training they received using digital WSIs as well as their attitudes regarding the future use of WSI.
Methods
Study Context
This research is part of a large longitudinal NIH/NCI-funded study evaluating how pathology trainees in academic medical centers across the US approach the diagnostic process when interpreting digital WSI and how that approach may change over the course of their residency training. Nine pathology training programs from eight different states (CA, KY, MA, NH, UT, VA, VT, and WA) participated in the first year of the study. Each site was provided information about the study, introduced the study to their trainees, and provided names and contact information for candidate participants but were not otherwise involved in data collection or analyses. All procedures were HIPAA compliant, and approval was obtained from the appropriate institutional review boards (IRB), with UCLA acting as the IRB of record.
Baseline Survey and Data Collection
Data presented here were collected between January and October of 2019. Eligible participants were enrolled in an anatomic pathology (AP) or combined anatomic and clinical (AP/CP) pathology training program (including post sophomore fellowships or other specialized AP fellowships) and were available during a site visit to their institution. Invitations to participate were sent via email (maximum of 4 attempts).
Study procedures for the larger study included completing an online consent form, online baseline survey, interpreting 14 digital WSIs of breast biopsies, and completing a diagnostic histology form for each case (data not shown). Participants received a US $50 gift card following completion of study activities. Only data from the baseline survey are described in this paper. Briefly, the content of the baseline survey included demographic information, medical school training, attitudes and experiences interpreting pathology, and attitudes on digital whole slide imaging. The survey was programmed and administered using Qualtrics Software. See Table 1 for the key survey questions described in this paper. The full survey is available in Supplemental Appendix 1.
Table 1.
Key Survey Questions.
|
|
|
|
|
|
|
|
|
|
Abbreviation: H&E, hematoxylin and eosin; WSI, whole slide image.
* Categorical responses: 1 to 5 hours, 6 to 10 hours, 11 to 25 hours, 26 to 50 hours, 51 to 100 hours, >100 hours, I have never used a traditional microscope with glass slides.
† Likert scale (1 = strongly disagree, 6 = strongly agree).
Data Analyses
Descriptive statistics, including means, SD, and frequencies of trainees’ responses, were calculated and hypothesis testing was performed using the Fisher exact test. All tests were 2-tailed. A P value < .05 was considered statistically significant. SAS version 9.4 (SAS Institute) was used to perform all statistical analyses.
Results
We invited 159 trainees to participate in the study. Of those invited, 3 were ineligible and 29 were unavailable to participate on the day of the site visit (eg, due to competing clinical responsibilities, working off site at another hospital on the day of the site visit, vacation, etc). Of the 127 pathology trainees who were eligible and potentially available to participate, 76 (60%) were able to join the study and completed the baseline survey. Data collection for the trainees’ review of the WSI cases required an individual 1-hour appointment during the site visit day(s), and as only 1 trainee could participate at a time, only a small number of appointments were available during each site visit limiting our ability to accommodate all trainees at all sites.
Demographics
The mean age of trainees was 33 years (range: 27-46, SD: 4). Just over half of the trainees were female (53%). The following describes the distribution of pathology training year: post-sophomore medical student fellows in pathology or Program Year 1: n = 20; Program Year 2: n = 27; Program Year 3: n = 20; and Program Year 4 or higher including post-residency Pathology Fellows: n = 9.
Medical School and Trainees’ Digital Training
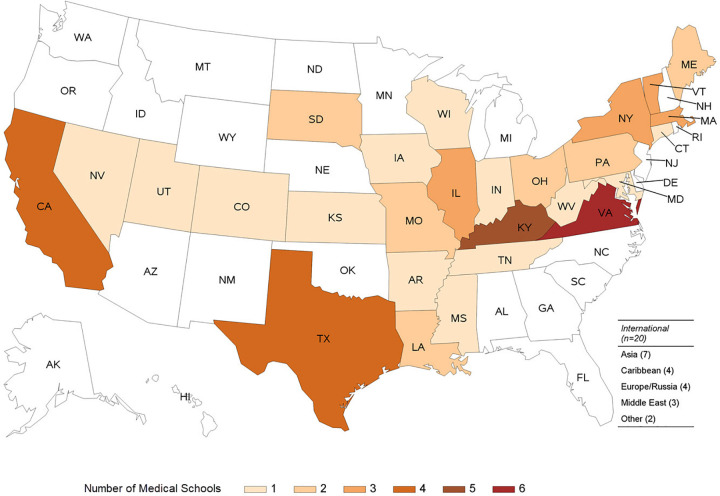
Trainees graduated from 63 different medical schools: 45 (71%) medical schools were in the United States (across 27 states), and 18 were located internationally (Figure 1). Most trainees (56 of 76 participants, 74%) graduated from US medical schools and the remaining 20 (26%) graduated from international medical schools.
Figure 1.
Geographic distribution of medical schools attended by pathology trainees participating in our study (3 participants indicated that they attended medical school in another country but did not specify which medical school. In the numbers reported, we assume that all 3 of these participants attended a different medical school from each other and other study participants. If this assumption is incorrect, then the number of different medical schools represented could be 60 rather than 63.).
The total number of hours reported by trainees spent using digital WSI during medical school training was: none by 25 (33%), 1 to 5 hours by 17 (22%), 6 to 10 hours by 10 (13%), and at least 11 hours by 21 (28%). Figure 2 illustrates the full distribution showing reported hours using digital WSI in the United States compared to international medical schools. While 33% reported no exposure at all, 67% reported having at least some experience in digital WSI during medical school. Those who began pathology training more recently were more likely to report at least some exposure to digital WSI training in medical school compared to those who began earlier (P value for trend = .10). Specifically, 75% of trainees who began in 2017 or 2018 reported WSI training compared to 54% for trainees who began pathology training in prior calendar years.
Figure 2.
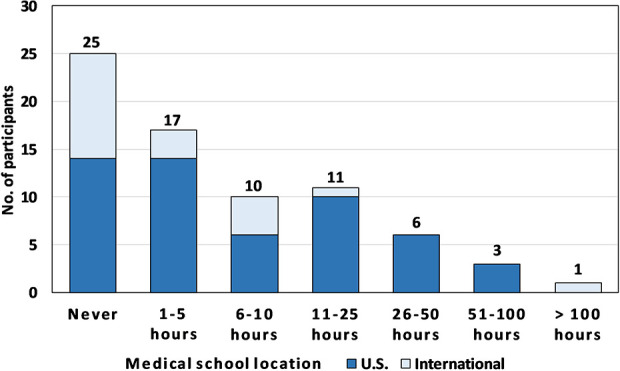
Number of hours spent using digital WSI during training by medical school location (3 trainees with missing data). WSI indicates whole slide image.
Trainees’ Attitudes Regarding Digital WSI
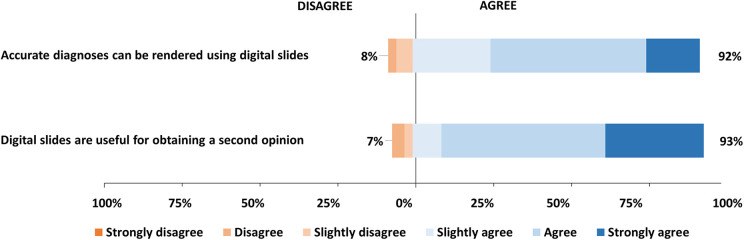
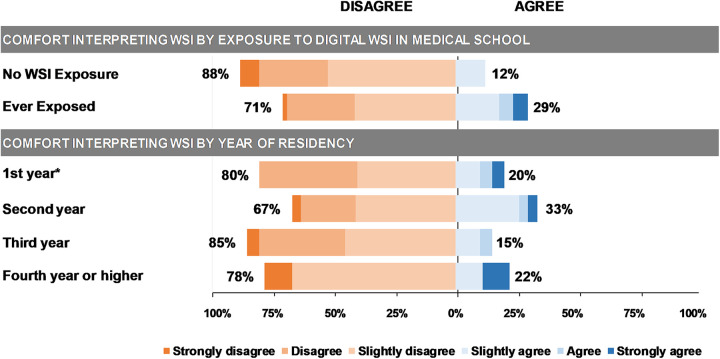
Most trainees agreed with the survey question that accurate diagnoses can be achieved using digital WSI for primary diagnostic purposes (92%; 95% CIs: 86-98) and that the digital format is useful for obtaining second opinions (93%; 95% CIs: 88-99; Figure 3). Only a quarter of trainees (24%, 95% CIs: 14-33) agreed that they are comfortable interpreting cases using digital slides. Trainees exposed to digital WSI in medical school, compared to those who were not exposed, tended to indicate that they are comfortable interpreting cases using digital slides (29% vs 12%; P = .06; Figure 4). There was no statistically significant association between trainees’ attitudes regarding digital WSI and their year of pathology training. The percentages of trainees who agreed that they are comfortable interpreting cases using digital WSI are 20% for post-sophomore/first year, 33% for second year, 15% for third year, and 22% for fourth year or higher (ie, fellow).
Figure 3.
Pathology trainees’ response to a Likert scale survey question on the use of digital WSI for primary diagnoses and second opinions. WSI indicates whole slide image.
Figure 4.
Pathology trainees’ response to survey question “I am comfortable interpreting cases using digital slides” by their exposure to digital WSI in medical school and year of training (*includes 1 post-sophomore fellow). WSI indicates whole slide image.
Trainees’ Perspectives About Future Use of Digital WSI
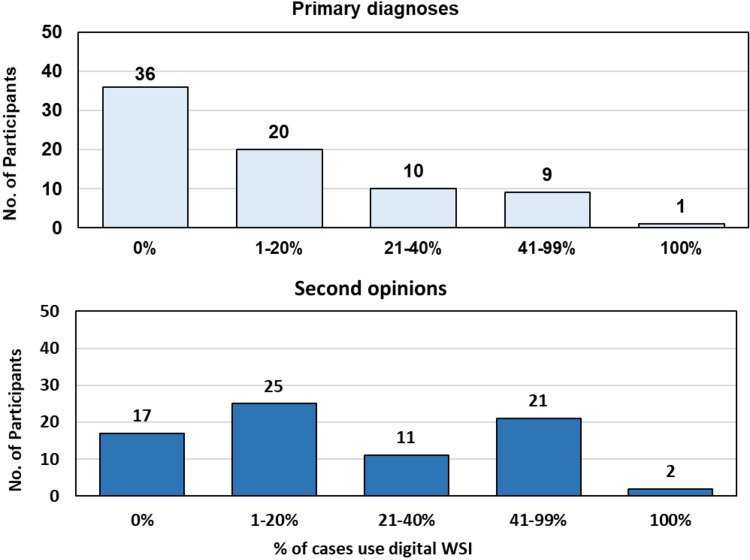
Most trainees predicted that in 5 years they would use digital WSI for either primary diagnosis or for providing a consultative second opinion for at least some of the cases in their professional practice as a pathologist (Figure 5). Trainees who had at least some experience interpreting cases using digital WSI during post-medical school pathology training were more likely to predict that in 5 years, they would use digital WSI for primary diagnosis (64% vs 50%; P = .3) and for providing a second opinion (86% vs 76%; P = .4). Trainees who thought digital slides are useful for obtaining a second opinion were more likely to predict that they would use digital WSI for either primary diagnosis (54% vs 40%, P = .6) or providing second opinions in their future practice (80% vs 40%; P = .03).
Figure 5.
Trainees’ predictions on the percentage of cases that will be interpreted using digital whole slide images in their future professional practice for primary diagnoses and second opinions.
Discussion
This study is unique in that it provides an overview of training across numerous medical schools, both in the United States and internationally and it queried pathology trainees shortly after FDA approval for WSI was granted. The data provides insight on exposure to training using digital WSI, including possible increased use in recent years, and it provides perspectives regarding future use among trainees who will begin independent clinical practice in a few years.
The findings indicate that though most respondents reported no or minimal WSI exposure during undergraduate medical education, trainees who entered pathology training in more recent years (2017/2018) reported slightly more exposure, suggesting that exposure to WSI may be increasing in graduate medical education. Further, trainees’ predictions regarding whether they will use WSI in their own future practice are especially positive.
Implementing curricular changes in medical education is time-intensive, and accreditation requirements are often primary drivers of curricular change.19,20 Internationally, the field of pathology and pathology education is shifting toward adoption of virtual microscopy using WSI.21-23 In addition, histology and microscopic anatomy courses are also transitioning towards incorporating virtual microscopy in their curricula.24 To understand how the clinical application of this technology will shape the future of clinical medicine, it will be increasingly important to assess incorporation of and proficiency with digital WSIs in undergraduate and graduate medical training programs.
Limitations of the study include that the sample included only 9 pathology residency sites, although more than 50 medical schools were represented. While the response rate of 60% was modest, this was a logistic consequence of the study, which required potential participants to be available during a specific site visit date and as only a limited number of appointments were available on each day, we stopped enrollment once full. A possible selection bias exists as trainees were incentivized by a gift certificate for participating. It is currently unknown whether exposure to WSI during medical education may be higher in those who pursue pathology training versus other career choices. Medical schools also vary in terms of when pathology courses are taught and the level of detail covered (eg, some programs have advanced courses in histology or pathology). We do not know which medical schools offered advanced courses in pathology or which trainees may have taken additional courses or elective rotations in pathology during undergraduate training.
Conclusions
Our findings indicate that although exposure to digital WSIs during training was higher among pathology trainees who began training in recent years (2017-2018), overall exposure to digital WSIs and virtual microscopy is limited to just a few hours for most trainees. The positive attitudes of current pathology trainees toward future use of digital whole slide imaging in their own practices for both primary diagnoses and second opinions highlight the importance of exposure to this technology in training programs if successful integration of WSI into clinical practice is expected.
Supplemental Material
Supplemental_Appendix_1 for Pathology Trainees’ Experience and Attitudes on Use of Digital Whole Slide Images by Joann G. Elmore, Hannah Shucard, Annie C. Lee, Pin-Chieh Wang, Kathleen F. Kerr, Patricia A. Carney, Trafton Drew, Tad T. Brunyé and Donald L. Weaver in Academic Pathology
Acknowledgments
The authors appreciate the support and involvement of staff and trainees at the various pathology training programs across the United States for their participation and help in this study.
Author’s Note: Tad T. Brunyé is also affiliated with Center for Applied Brain and Cognitive Sciences, Medford, MA, USA.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Dr. Elmore serves as Editor in Chief of Adult Primary Care topics at UpToDate.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in the article was supported by R01 CA225585, U01 CA231782, and R01 CA200690 from the National Cancer Institute of the National Institutes of Health. The funder had no role in the design and conduct of the study.
ORCID iD: Joann G. Elmore  https://orcid.org/0000-0002-7311-6835
https://orcid.org/0000-0002-7311-6835
Kathleen F. Kerr  https://orcid.org/0000-0002-6438-9583
https://orcid.org/0000-0002-6438-9583
Supplemental Material: Supplemental material for this article is available online.
References
- 1. FDA allows marketing of first whole slide imaging system for digital pathology. 2017. Accessed April 22, 2020 https://www.fda.gov/news-events/press-announcements/fda-allows-marketing-first-whole-slide-imaging-system-digital-pathology
- 2. Abels E, Pantanowitz L. Current state of the regulatory trajectory for whole slide imaging devices in the USA. J Pathol Inform. 2017;8:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Newitt VN. Digital pathology: a 1st anniversary report card. CAP today. 2018. Accessed April 22, 2020 https://www.captodayonline.com/digital-pathology-1st-anniversary-report-card/
- 4. Robertson S, Azizpour H, Smith K, Hartman J. Digital image analysis in breast pathology—from image processing techniques to artificial intelligence. Trans Res. 2018;194:19–35. [DOI] [PubMed] [Google Scholar]
- 5. Parwani AV, Hassell L, Glassy E, Pantanowitz L. Regulatory barriers surrounding the use of whole slide imaging in the United States of America. J Pathol Inform. 2014;5:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pantanowitz L, Valenstein PN, Evans AJ, et al. Review of the current state of whole slide imaging in pathology. J Pathol Inform. 2011;2:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Farahani NPA, Pantanowitz L. Whole slide imaging in pathology: advantages, limitations, and emerging perspectives. Pathol Lab Med Int. 2015;7:23–33. [Google Scholar]
- 8. Aeffner F, Zarella MD, Buchbinder N, et al. Introduction to digital image analysis in whole-slide imaging: a white paper from the digital pathology association. J Pathol Inform. 2019;10:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Farahani N, Post R, Duboy J, et al. Exploring virtual reality technology and the oculus rift for the examination of digital pathology slides. J Pathol Inform. 2016;7:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pantaoniwitz L. Telepathology heads up: wearable devices show promise for improving pathology workflow. 2016. Accessed April 22, 2020 https://thepathologist.com/diagnostics/telepathology-heads-up
- 11. Parini V, Christensen E, Yeldandi A. Utility of Google Glass® in Pathology Practice. Paper presented at: Pathology Visions; 2014. [Google Scholar]
- 12. Triola MM, Holloway WJ. Enhanced virtual microscopy for collaborative education. BMC Med Educ. 2011;11:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dee FR. Virtual microscopy in pathology education. Hum Pathol. 2009;40:1112–1121. [DOI] [PubMed] [Google Scholar]
- 14. Kumar RK, Freeman B, Velan GM, De Permentier PJ. Integrating histology and histopathology teaching in practical classes using virtual slides. Anat Rec B New Anat. 2006; 289:128–133. [DOI] [PubMed] [Google Scholar]
- 15. Koch LH, Lampros JN, Delong LK, Chen SC, Woosley JT, Hood AF. Randomized comparison of virtual microscopy and traditional glass microscopy in diagnostic accuracy among dermatology and pathology residents. Hum Pathol. 2009;40:662–667. [DOI] [PubMed] [Google Scholar]
- 16. Krippendorf BB, Lough J. Complete and rapid switch from light microscopy to virtual microscopy for teaching medical histology. Anat Rec (Part B: New Anat). 2005;285B:19–25. [DOI] [PubMed] [Google Scholar]
- 17. Wilson AB, Taylor MA, Klein BA, Sugrue MK, Whipple EC, Brokaw JJ. Meta-analysis and review of learner performance and preference: virtual versus optical microscopy. Med Educ. 2016;50:428–440. [DOI] [PubMed] [Google Scholar]
- 18. Diaz-Perez J, Raju S, Echeverri J. Evaluation of a teaching strategy based on integration of clinical subjects, virtual autopsy, pathology museum, and digital microscopy for medical students. J Pathol Inform. 2014;5:25–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kassebaum DG, Cutler ER, Eaglen RH. The influence of accreditation on educational change in U.S. medical schools. Acad Med. 1997;72:1127–1133. [DOI] [PubMed] [Google Scholar]
- 20. van Zanten M, Boulet JR, Greaves I. The importance of medical education accreditation standards. Med Teach. 2012;34:136–145. [DOI] [PubMed] [Google Scholar]
- 21. Kuo K-H, Leo JM. Optical versus virtual microscope for medical education: a systematic review. Anat Sci Educ. 2018;12:678–685. [DOI] [PubMed] [Google Scholar]
- 22. Williams BJ, Bottoms D, Treanor D. Future-proofing pathology: the case for clinical adoption of digital pathology. J Clin Pathol. 2017;70:1010–1018. [DOI] [PubMed] [Google Scholar]
- 23. Hamilton PW, Wang Y, McCullough SJ. Virtual microscopy and digital pathology in training and education. APMIS. 2012;120:305–315. [DOI] [PubMed] [Google Scholar]
- 24. Drake RL, McBride JM, Lachman N, Pawlina W. Medical education in the anatomical sciences: the winds of change continue to blow. Anat Sci Educ. 2009;2:253–259. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental_Appendix_1 for Pathology Trainees’ Experience and Attitudes on Use of Digital Whole Slide Images by Joann G. Elmore, Hannah Shucard, Annie C. Lee, Pin-Chieh Wang, Kathleen F. Kerr, Patricia A. Carney, Trafton Drew, Tad T. Brunyé and Donald L. Weaver in Academic Pathology