Abstract
Background
Total elbow arthroplasty (TEA) is the established treatment for end-stage rheumatoid arthritis but improved surgical techniques have resulted in expanded indications. The aim of this study is to review the literature to evaluate the evolution of surgical indications for TEA.
Methods
A systematic review of PubMed and EMBASE databases was conducted. Case series and comparative studies reporting results after three types of primary TEA were eligible for inclusion.
Results
Forty-nine eligible studies were identified (n = 1995). The number of TEA cases published annually increased from 6 cases in 1980 to 135 cases in 2008. The commonest indication for TEA throughout the review period was rheumatoid arthritis but its annual proportion reduced from 77% to 50%. The mean Mayo Elbow Performance Score significantly improved for all indications. Three comparative studies reported statistically improved functional outcomes in rheumatoid arthritis over the trauma sequelae group. Complication and revision rates varied; rheumatoid arthritis 5.2–30.9% and 11–13%, acute fracture 0–50% and 10–11%, trauma sequelae 14.2–50% and 0–30%, osteoarthritis 50% and 11%, respectively.
Discussion
TEA can provide functional improvements in inflammatory arthritis, acute fractures, trauma sequelae and miscellaneous indications. Long-term TEA survivorship appears satisfactory in rheumatoid arthritis and fracture cases; however, further research into alternative surgical indications is still required.
Keywords: total elbow arthroplasty, total elbow replacement, elbow, indications
Introduction
The primary purpose of total elbow arthroplasty (TEA) is to provide a stable, pain-free elbow and restore range of motion.1 TEA designs can simply be classified into ‘linked’ and ‘un-linked’ prostheses. Unlinked implants are not mechanically coupled and have been associated with higher rates of instability.2 Modern linked designs utilise a ‘sloppy’ hinge and are associated with a reduced rate of aseptic loosening and instability of the articulation.1 Reported outcomes of TEA are not as successful as after hip or knee replacements.3 Complication rates vary between 14% and 80% with aseptic loosening, infection, dislocation and post-operative wound problems being the most common complications.4,5
TEA is the established treatment choice for patients with end-stage rheumatoid elbow disease.1,6,7 Improved surgical techniques have resulted in an expansion in the indications to include osteoarthritis (OA), post-traumatic arthritis (PTA) and more recently acute distal humeral fractures.8 However, these additional indications place additional demands on the implants and may lead to higher failure rates.9–11 Currently the indications for TEA remain controversial and the aim of this study is to review the literature to evaluate the evolution of surgical indications for TEA.
Materials and methods
A systematic review of the literature using the online databases PubMed and EMBASE was conducted in accordance with the PRISMA guidelines (Supplementary File 1). The search terms used for the PubMed search are provided in Supplementary Appendix 1. The searches were performed independently by two authors on 27 May 2019 and repeated on 5 June 2019 to ensure accuracy. Any discrepancies were resolved through discussion between these two authors, with the senior author resolving any residual differences.
Clinical studies published in English were considered for eligibility. Studies could be either case series or comparative studies reporting results after primary TEA. Three TEA designs were included: Coonrad–Morrey (Zimmer, Warsaw, IN), Discovery Elbow System (DES; Biomet Orthopedics, Warsaw, IN) and Latitude (Tornier, Bloomington, IN). The decision to include only these three designs was made to reflect the UK National Joint Registry12 which reports that only these three implants are currently used in the UK. Studies reporting on multiple implants were only included if the independent results from only the included implants could be identified. Only primary research was considered for review with any abstracts, comments, review articles, case reports and technique articles excluded.
Due to heterogeneity of study populations only a narrative review was conducted and reported according to indication group; inflammatory arthritis, acute fracture, trauma sequelae, miscellaneous, general studies and OA. In order to illustrate the evolution in indications for TEA over the review period, the number of patients undergoing TEA for each indication was averaged over each study period. Data from all studies was then collated to produce an annual percentage for each indication from 1982 to 2011.
Results
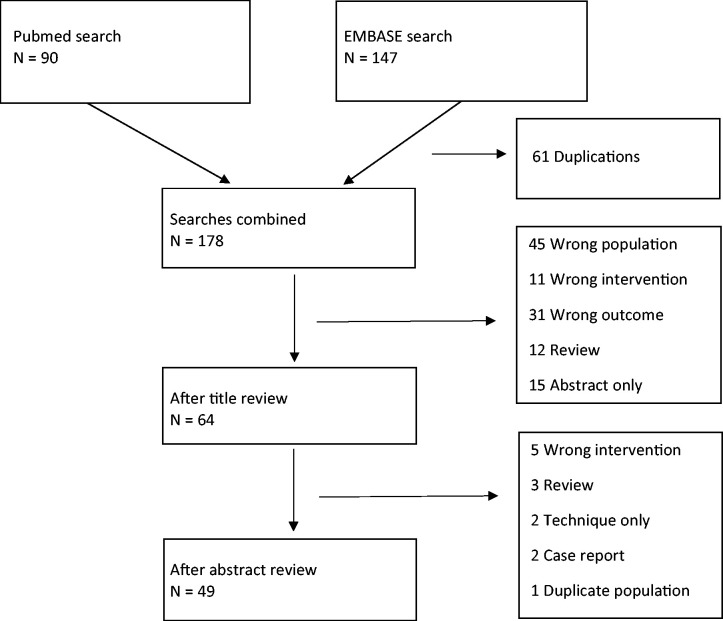
The search strategy identified 49 studies eligible for inclusion (n = 1995); 10 on inflammatory arthritis (n = 773),13–22 8 following acute fractures (n = 179),23–30 10 on post-trauma sequelae (n = 216)26,31–39 4 for miscellaneous indications (n = 82),40–43 17 reporting on multiple indications (n = 724)44–60 and 1 on OA (n = 18).61 This included one study that reported on separate subgroups of acute fractures and in post-trauma sequelae.26 A flow chart of the search strategy is shown in Figure 1. Concise details of the studies according to the indication for surgery are provided in Supplementary Appendices 2 to 7.
Figure 1.
Flow diagram of review process.
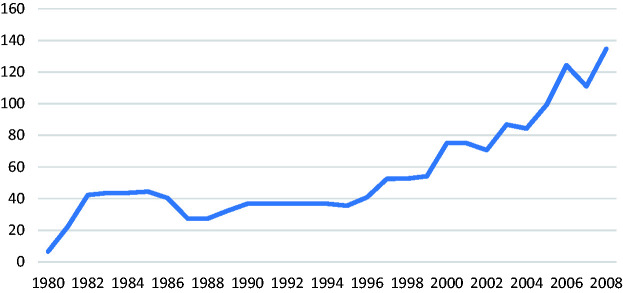
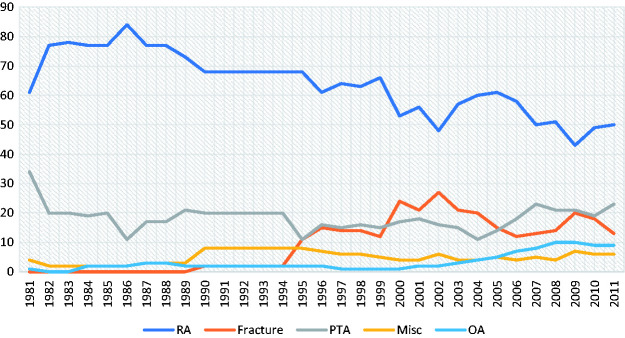
As illustrated in Figure 2, the number of TEA for any indication increased from 6 cases in 1980 to 135 cases in 2008. The commonest indication for TEA throughout the review period was rheumatoid arthritis (RA); however, the annual percentage of TEA performed for RA reduced from 77% in 1982 to 50% in 2011. Figure 3 illustrates the (published) annual percentage for each indication between 1982 and 2011.
Figure 2.
Total number of TEAs reported annually in the literature for any indication.
Figure 3.
Annual proportion of TEA according to indication.
Inflammatory arthritis
Ten studies reported on the results after TEA in inflammatory arthritis13–22 and concise details are provided in Supplementary Appendix 2. Six studies analysed the Coonrad–Morrey implant in RA reporting mean Mayo Elbow Performance Score (MEPS) ranging from 81 to 94, complications from 5.2% to 30.9% and revision rates from 11% to 13%. Survivorship analysis was performed in three studies and at 10 years ranged from 85% to 92.4%. Sanchez-Sotelo et al. reported the largest case series (n = 435) in their prospective cohort study that was conducted between 1982 and 2006 with a mean 10-year follow-up.16 The authors report excellent functional scores (mean MEPS 90) with a complication rate of 5.2% and revision rate of 11% including an overall infection rate of 2.2%. The reported survivorship was 92% at 10 years, 83% at 15 years and 68% at 20 years. Two studies analysed the DES in RA reporting mean MEPS of 93, complications from 8% to 15.4%, revision rates from 7.3% to 12% but no survivorship analysis was performed.15–17
Two studies reported results of TEA in solely juvenile inflammatory arthritis; both used the Coonrad–Morrey implant.14–19 Baghdadi et al.19 reported on 29 patients with a mean age of 37 years and mean MEPS of 78 at 126 months follow-up, survivorship of the implant was 79.9% at 10 years. Ibrahim et al.14 reported on seven patients with mean age 44 years at mean 113 months follow-up and showed a 71.4% complication rate, 28.6% revision rate and 10-year survivorship of 69%.
The literature reviewed has demonstrated that TEA is capable of providing significant improvements in pain and function for patients with RA. The 10-year survival rate of 85–92% suggests these implants have a reasonable longevity in this population. Although function is improved for patients with juvenile inflammatory arthritis, the survivorship figures at 10 years are lower (69–79%) and this should be factored into decision making and counselling of these patients prior to surgery.
Acute fractures
Eight studies reported on TEA in acute fractures23–30 with the majority being in elderly patients and female gender; mean age 66.5 to 80 years and 63% to 90% female. Concise study details are provided in Supplementary Appendix 3. The Coonrad–Morrey implant was used in six studies with the Latitude and Discovery in each of the other studies. These studies demonstrated a good functional outcome with mean MEPS 83 to 99.5 and the mean ASES 87. The complication rate varied from 0% to 50%, revision rate 10% to 11% and the 10-year survivorship when reported in one study was 89%.23
Mansat et al.27 reported the largest series (n = 87) in their multicentred retrospective study conducted between 2000 and 2010 with a mean 37.5 months follow-up. The authors report good post-operative function with mean MEPS 86 and Quick-DASH 24, whilst the complication rate was 23% with neuropathy 8% and haematoma 5.7% being the most commonly reported. Ellwein et al.25 compared open reduction and internal fixation (ORIF) to TEA and reported similar ROM and function in the groups but found that ORIF was associated with a 4.4 higher risk of complication.
The studies reviewed have shown that TEA is a viable option in the management of distal humeral fractures with the ability to provide comparable functional outcomes to other surgical indications. The 89% 10-year survivorship reported by Prasad et al.23 suggests that TEA has acceptable longevity for acute fractures, but this data has yet to be validated in additional studies. The one comparative study included has shown comparable function of TEA to ORIF with a lower rate of complication.25
Trauma sequelae
Ten studies reported the results of TEA following the sequelae of trauma with either PTA or non-unions accounting for the majority of cases.26,31–39 Concise study details are provided in Supplementary Appendix 4. Eight studies utilised the Coonrad–Morrey implant, one study the DES and the final study a combination of the Coonrad–Morrey and the Latitude implant. The mean age of patients ranged from 56 to 72 years. Overall, the studies reported a mean range of MEPS from 80 to 94.3 and ASES of 82. Complication and revision rates varied from 14.2% to 50% and 0% to 30%, respectively.
The two largest series from Schneeberger et al.38 (n = 41) and Morrey et al.39 (n = 53) were both published over 20 years ago and report a high complication rate (18.9% to 34%) with the commonest complications being fractures, infection and triceps rupture. Morrey et al. report a high 30% revision rate at mean 75 months follow-up with aseptic loosening accounting for the majority of cases (88%). Barthel et al.36 compared results from those undergoing TEA after non-union and PTA; the authors report comparable functional outcomes but a trend to higher complications (58% vs. 28%) and revision rates (25% vs. 14%) in the PTA group. Three studies in the general indication subgroup compared the outcomes after inflammatory arthritis and trauma sequelae; all three reported that the mean MEPS was significantly higher in RA group.53,55,59
The evidence reviewed has demonstrated that TEA can provide improved functional scores in this complex patient group. However, comparative studies suggest that outcomes are less predictable than when performed for inflammatory arthritis. In addition, the relatively high and variable complication and revision rates should be noted and used when counselling these patients prior to surgery.
Miscellaneous indications
Four studies reported on miscellaneous indications for TEA40–43 and concise study details are given in Supplementary Appendix 5. Ernstbrunner et al. and Vochteloo et al. reported outcomes of TEA after haematological conditions. Ernstbrunner conducted the largest study and used the Coonrad–Morrey implant in 13 patients with haemophilia.40 The authors report improvement in function mean MEPS 64 to 89 but a high complication rate 62% and revision rate of 38% at just under 10 years mean follow-up. The infection rate requiring revision was high at 15.4% and the survivorship was 92% and 42% at 5 and 10 years, respectively.
Two studies reported the use of Coonrad–Morrey in patients with a mixture of primary and metastatic tumours with the age of patients varying from 9 to 86 years in a wide variety of tumours. Mean follow-up in both studies was under three years. An improvement in mean MEPS was observed but complications rate (29% to 35%) and revision rate (4.2% to 20%) at short-term follow-up were relatively high.
TEA has been shown to improve function for haematological and oncological patients. The limited number of studies reviewed for these miscellaneous indications restrict the strength of conclusions that can be drawn. However, the high complication and revision rates even at short-term follow-up suggest these patients are at risk of implant failure.
General Indication Papers
Seventeen studies were identified that reported TEA after multiple indications44–60 and concise details of these studies are given in Supplementary Appendix 6. Overall, the commonest indications were RA and post-trauma sequelae. Eleven studies reported outcomes after the Coonrad–Morrey prosthesis, four after the DES (including one cementless series) and two after the Latitude prosthesis. In the studies using the Coonrad–Morrey implant, the mean MEPS ranged from 84 to 91, complication rate 14% to 54% and revision rate 5.6% to 33%. When using the Latitude implant the mean ASES was 37.9, complication rate ranged from 7.9% to 27% and revision rate 9.5%. In the studies using the DES, the mean MEPS ranged from 77.2 to 86.5, complication rate 5% to 43.5% and revision rate 13.3% to 13.7%. Frostick et al. reported the only cementless arthroplasty using the DES and at a mean five years follow-up reported mean MEPS 77.25, mean Liverpool Elbow Score 6.76 and only a 5% complication rate. Survivorship analysis was performed in only three studies; two using the Coonrad–Morrey with 5-year survivorship 72% to 97.7% and 10-year survivorship 91% and in one study reporting the DES where the 5-year survivorship was 90.2%.
Three studies compared the outcomes after inflammatory arthritis and trauma sequelae. Mansat et al. conducted the largest series with 78 elbows and reported that the mean MEPS was significantly higher in RA group (mean 89) than after trauma (mean 90), p < 0.01.53 Similarly, Hildebrand et al.59 reported that mean MEPS was higher in RA (mean 90) than in PTA group (mean 78), p < 0.05. Celli and Morrey55 demonstrated significantly improved results in RA over the trauma sequelae group in MEPS 93 versus 84 (p = 0.03), complications 23% versus 100% (p = 0.02) and revision rates 37% versus 11% (p < 0.05).
Osteoarthritis
One study published results of TEA in solely OA patients61 and concise details of this study are provided in Supplementary Appendix 7. In addition, 12 of the 17 articles reviewed under the ‘General Indication Papers’ subheading reported patients who had undergone TEA for OA.44–52,54,56,58 However, the cumulative number of OA patients reported within these 12 studies was only 70, which represented 9.6% of all patients in these 17 studies. In addition, the majority of studies did not present the data according to surgical indication separately which further restricted analysis of the outcome of TEA in OA patients.
Schoch et al. reported on 18 OA patients with a mean age of 68 years. At a mean follow-up of nine years 53% were reported to have an excellent or good outcome according to MEPS. However, the complication and revision rates were 50% and 11%, respectively, and the authors reported a 10-year implant survival of 89.4%. Within the ‘General Indication Papers’, three studies did report outcomes in OA patients and demonstrated no significant difference between OA and other pathologies in terms of function, pain and range of motion, although the mean outcome values for the different groups were not provided.47–49 Corradi et al. reported outcomes for individual patients, demonstrating improvement in mean MEPS from 60 to 89 in RA patients and 40 to 75 in OA patients; however, only two patients underwent TEA for OA in this study.54 Na et al. did not compare the functional results between different surgical indications but reported a higher complication rate in RA (33%) compared to OA (0%) patients with all complications being intra-operative fractures.44
The studies reviewed suggest that OA is responsible for a significant number of TEA and by 2008 10% of published cases were performed for OA. However, the literature on this specific indication is restricted as the majority of cases reported are only included in General Indication Papers. The limited studies comparing the results of OA against other pathologies suggest outcomes are comparable but the numbers in these studies are low restricting any conclusions that can be drawn.
Discussion
During the review period the number of TEAs reported annually in the literature has increased as illustrated in Figure 2. This rise in publication number has enhanced the understanding of TEA and should be used to facilitate the practice of evidence-based medicine. This increase may reflect the improvement in surgical techniques, expansion in surgical indications and subsequent interest in the outcomes of the procedure in these newer indications.8 However, the increased publication number does not necessarily reflect an increase in the number of actual surgical procedures performed. During the same time period, the Norwegian registry has reported a reduction in the number of TEA performed between 1994 and 1999 (n = 317) and 2011 and 2016 (n = 145).62 In contrast, the Danish registry has reported an increase in incidence of TEA from 41 between 1981 and 1990 to 146 between 2001 and 2008.63 However, the UK National Joint Registry only commenced recording TEA in 2012, since 2013 the UK registry has seen only a small increase in the annual number performed from 421 to 484.12
TEA is the established treatment choice for end-stage rheumatoid elbow disease1,6,7 and the results of TEA after RA have previously been shown to be superior to any other indication in terms of functional outcome, lower complication and revision rate.64.65 Three studies included in this review compared RA to post-trauma sequelae and all reported statistically significant improvements in functional scores in RA patients over post-trauma patients.53,55,59 RA remained the commonest indication for TEA over the review period but the percentage of TEAs being performed for RA reduced from 77% in 1982 to 50% in 2010. This reduction may reflect a decrease in end-stage rheumatoid disease as a result of advances in non-operative management which include disease modifying anti-rheumatoid drugs.66.67 Alternatively, this decrease may reflect the advancement of surgical techniques and increase in alternative surgical indications.8 The Norwegian registry has demonstrated a comparable reduction in TEA for inflammatory arthritis; between 1994 and 2006 surgical indications were 93% RA, 5% OA and 2% fractures68 and between 2006 and 2017 indications were 68% RA, 7% OA and 10% fracture.62 The Danish registry similarly reports that the RA is the most common indication, but its frequency is reducing with fracture sequelae and OA the next most common indications.63
Survivorship analysis was performed in only a small number of studies; the 10-year survivorship for general indications was 91%, RA 85% to 92.4%, acute fracture 89%, OA 89%, juvenile inflammatory arthritis 69% to 79.9% and haemophilia 42%. Scandinavian registry data for all indications showed 10-year survivorship ranging from 81% to 83%.62,63,69 These discrepancies in survivorship across registry data and surgical indications can be partly explained by the numerous factors that have been shown to influence the risk of revision after TEA. Sanchez-Sotelo et al.16 demonstrated that male sex (p = 0.006), concurrent traumatic pathology (p = 0.026) and type of ulna component (p = 0.017) increased the risk of revision. Mansat et al.53 reported the risk of revision was increased with young age (p < 0.01), previous surgery (p < 0.05) and duration of surgery (p < 0.01). Schoch et al.70 have previously suggested caution when using TEA in patients under 50 years reporting an 82% complication rate and high rates of early mechanical failure in this subgroup. Plaschke et al. demonstrated higher revision rate after trauma sequelae (37%) than after RA (11%), p < 0.05, a factor that is supported by the Danish registry which showed fracture sequelae had a relative risk of revision of 1.9 (95% CI 1.05–3.45).63 Previous literature has linked obesity with poor outcome after TEA;71–73 Baghdadi et al.74 reported a lower implant survivorship in the obese patients (72% vs. 86%) and Griffin et al.75 reported higher infection rates, dislocation rates, peri-prosthetic fractures and two-year revision rate in obese patients. Therefore, the lower survivorship rates reported for juvenile idiopathic arthritis, haemophilia and tumours are likely to be multifactorial with patient age at surgery one potentially important factor.
The role of TEA in acute distal humeral fractures is controversial and this is reflected in the increase in published cases undergoing TEA for fractures from 0% in 1982 to 18% in 2010. The management of distal humeral fractures is challenging but particularly relevant given their incidence is predicted to triple by 2030.76 An international questionnaire reported that surgeons considered important factors in decision making for these patients to be age, RA, bone quality and presence of degenerative elbow disease.71 Few studies have compared the outcomes of ORIF with TEA; the study from Ellwein et al. was included in this review and reported similar function after TEA but found that ORIF was associated with a 4.4 higher risk of complication. McKee et al. in a randomised controlled trial in 40 patients older than 65 years demonstrated significantly improved functional outcomes after TEA at two years.72 However, this potential advantage of TEA over ORIF has not been reproduced in all comparative studies. Egol et al. and Charissoux et al. compared these treatment modalities and showed no significant improvement of TEA over ORIF.73.77
Limitations of this systematic review are acknowledged. The included studies provide only level III and IV evidence with common weaknesses being the low study numbers and lack of comparative groups. The number of available studies for certain indications and surgical implants was low, which restricted the conclusions that can be drawn from these. Heterogeneity of surgical indications, surgical techniques and reporting of outcome measures significantly restricted direct comparison of results between studies. An example of this is the varied reporting of complications after TEA which may result from differing definitions, thresholds to report and length of follow-up. Comparison of the results from the review to registry data is important but also has limitations given most registries rely on self-reporting from surgeons to gather their data.
Conclusion
TEA can provide functional improvements in inflammatory arthritis, acute fractures, trauma sequelae and miscellaneous indications. Although RA remains the commonest indication, the proportion undergoing the procedure for alternative indications has increased. Long-term TEA survivorship appears satisfactory in RA and fracture cases; however, further research into the influence of alternative surgical indications and patient factors on implant failure is required.
Supplemental Material
Supplemental material, Supplemental Material1 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Supplemental material, Supplemental Material2 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Supplemental material, Supplemental Material3 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Supplemental material, Supplemental Material4 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Supplemental material, Supplemental Material5 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Supplemental material, Supplemental Material6 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Supplemental material, Supplemental Material7 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Supplemental material, Supplemental Material8 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Authors’ Contribution
VS, GM, and RJ performed the literature searches and constructed the manuscript. AW, PJ, RK, MT, AR, SMH conceived the topic of the review, oversaw the literature searches and provided guidance in article production. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor
SMH.
Supplemental Material
Supplemental material for this article is available online.
References
- 1.Sanchez-Sotelo J. Total elbow arthroplasty. Open Orthop J 2011; 5: 115–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banagan KE, Murthi AM. Current concepts in total elbow arthroplasty. Curr Opin Orthop 2006; 17: 335–339. [Google Scholar]
- 3.Rahme H, Jacobsen MB, Salomonsson B. The Swedish Elbow Arthroplasty Register and the Swedish Shoulder Arthroplasty Register: two new Swedish arthroplasty registers. Acta Orthop Scand 2001; 72: 107–112. [DOI] [PubMed] [Google Scholar]
- 4.Little CP, Graham AJ, Carr AJ. Total elbow arthroplasty: a systematic review of the literature in the English language until the end of 2003. J Bone Joint Surg Br 2005; 87: 437–444. [DOI] [PubMed] [Google Scholar]
- 5.van der Lugt JC, Rozing PM. Systematic review of primary total elbow prostheses used for the rheumatoid elbow. Clin Rheumatol 2004; 23: 291–298. [DOI] [PubMed] [Google Scholar]
- 6.Sanchez-Sotelo J, Ramsey ML, King GJ, et al. Elbow arthroplasty: lessons learned from the past and directions for the future. Instr Course Lect 2011; 60: 157–169. [PubMed] [Google Scholar]
- 7.Gill DR, Morrey BF. The Coonrad–Morrey total elbow arthroplasty in patients who have rheumatoid arthritis. A ten to fifteen-year follow-up study. J Bone Joint Surg Am 1998; 80: 1327–1335. [DOI] [PubMed] [Google Scholar]
- 8.Voloshin I, Schippert DW, Kakar S, et al. Complications of total elbow replacement: a systematic review. J Shoulder Elbow Surg 2011; 20: 158–168. [DOI] [PubMed] [Google Scholar]
- 9.Dee R. Reconstructive surgery following total elbow endoprosthesis. Clin Orthop Relat Res 1982; 170: 196–203. [PubMed] [Google Scholar]
- 10.Fevang B-TS, Lie SA, Havelin LI, et al. Results after 562 total elbow replacements: a report from the Norwegian Arthroplasty Register. J Shoulder Elbow Surg 2009; 18: 449–456. [DOI] [PubMed] [Google Scholar]
- 11.Mansat P, Bonnevialle N, Rongieres M, et al. Experience with Coonrad–Morrey total elbow arthroplasty: 78 consecutive total elbow arthroplasties reviewed with an average 5 years of follow-up. J Shoulder Elbow Surg 2013; 22: 1461–1468. [DOI] [PubMed] [Google Scholar]
- 12.National Joint Registry. Details for primary elbow procedures, http://www.njrreports.org.uk/elbows-primary-procedures-activity (accessed May 2019).
- 13.Pham TT, Delclaux S, Huguet S, et al. Coonrad–Morrey total elbow arthroplasty for patients with rheumatoid arthritis: 54 prostheses reviewed at 7 years' average follow-up (maximum 16 years). J Shoulder Elbow Surg 2018; 27: 398–403. [DOI] [PubMed] [Google Scholar]
- 14.Ibrahim EF, Rashid A, Thomas M. Linked semi constrained and unlinked total elbow replacement in juvenile idiopathic arthritis: a case comparison series with mean 11.7-year follow-up. J Shoulder Elbow Surg 2017; 26: 305–313. [DOI] [PubMed] [Google Scholar]
- 15.Hanninen P, Niinimaki T, Flinkkila T, et al. Discovery Elbow System: clinical and radiological results after 2- to 10-year follow up. Eur J Orthop Surg Traumatol 2017; 27: 901–907. [DOI] [PubMed] [Google Scholar]
- 16.Sanchez-Sotelo J, Baghdadi YM, Morrey BF. Primary linked semi constrained total elbow arthroplasty for rheumatoid arthritis: a single-institution experience with 461 elbows over three decades. J Bone Joint Surg Am 2016; 98: 1741–1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mukka S, Berg G, Hassany HR, et al. Semi constrained total elbow arthroplasty for rheumatoid arthritis patients: clinical and radiological results of 1-8 years follow-up. Arch Orthop Trauma Surg 2015; 135: 595–600. [DOI] [PubMed] [Google Scholar]
- 18.Ogino H, Ito H, Furu M, et al. Outcome of shortened extra-small ulnar component in linked total elbow arthroplasty for patients with rheumatoid arthritis. Mod Rheumatol 2015; 25: 849–853. [DOI] [PubMed] [Google Scholar]
- 19.Baghdadi YMK, Jacobson JA, Duquin TR, et al. The outcome of total elbow arthroplasty in juvenile idiopathic arthritis (juvenile rheumatoid arthritis) patients. J Shoulder Elbow Surg 2014; 23: 1374–1380. [DOI] [PubMed] [Google Scholar]
- 20.Prasad N, Dent C. Outcome of total elbow replacement for rheumatoid arthritis: single surgeon's series with Souter–Strathclyde and Coonrad–Morrey Prosthesis. J Shoulder Elbow Surg 2010; 19: 376–383. [DOI] [PubMed] [Google Scholar]
- 21.Lee KT, Singh S, Lai CH. Semi-constrained total elbow arthroplasty for the treatment of rheumatoid arthritis of the elbow. Singapore Med J 2005; 46: 718–722. [PubMed] [Google Scholar]
- 22.Gill DR, Morrey BF The Coonrad–Morrey total elbow arthroplasty in patients who have rheumatoid arthritis. J Bone Joint Surg 1998; 80: 1327–1335. [DOI] [PubMed] [Google Scholar]
- 23.Prasad N, Ali A, Stanley D. Total elbow arthroplasty for non-rheumatoid patients with a fracture of the distal humerus – a minimum ten-year follow-up. Bone Joint J 2016; 98: 381–386. [DOI] [PubMed] [Google Scholar]
- 24.Tian W, He C, Jia J. Total elbow joint replacement for the treatment of distal humerus fracture of type C in eight elderly patients. Int J Clin Exp Med 2015; 8: 10066–10073. [PMC free article] [PubMed] [Google Scholar]
- 25.Ellwein A, Lill H, Voigt C, et al. Arthroplasty compared to internal fixation by locking plate osteosynthesis in comminuted fractures of the distal humerus. Int Orthop 2015; 39: 747–754. [DOI] [PubMed] [Google Scholar]
- 26.Giannicola G, Scacchi M, Polimanti D, et al. Discovery elbow system: 2- to 5-year results in distal humerus fractures and posttraumatic conditions: a prospective study on 24 patients. J Hand Surg Am 2014; 39: 1746–1756. [DOI] [PubMed] [Google Scholar]
- 27.Mansat P, Degorce NH, Bonnevialle N, et al. SOFCOT. Total elbow arthroplasty for acute distal humeral fractures in patients over 65 years old – results of a multicenter study in 87 patients. Orthop Traumatol Surg Res 2013; 99: 779–784. [DOI] [PubMed] [Google Scholar]
- 28.Ducrot G, Ehlinger M, Adam P, et al. Complex fractures of the distal humerus in the elderly: is primary total elbow arthroplasty a valid treatment alternative? A series of 20 cases. Orthop Traumatol Surg Res 2013; 99: 10–20. [DOI] [PubMed] [Google Scholar]
- 29.Lee KT, Lai CH, Singh S. Results of total elbow arthroplasty in the treatment of distal humerus fractures in elderly Asian patients. J Trauma 2006; 61: 889–892. [DOI] [PubMed] [Google Scholar]
- 30.Garcia JA, Mykula R, Stanley D. Complex fractures of the distal humerus in the elderly. The role of total elbow replacement as primary treatment. J Bone Joint Surg Br 2002; 84: 812–816. [DOI] [PubMed] [Google Scholar]
- 31.Celli A. A new posterior triceps approach for total elbow arthroplasty in patients with osteoarthritis secondary to fracture: preliminary clinical experience. J Shoulder Elbow Surg 2016; 25: e223–e231. [DOI] [PubMed] [Google Scholar]
- 32.Kodde IF, Van Riet RP, Eygendaal D. Semi constrained total elbow arthroplasty for posttraumatic arthritis or deformities of the elbow: a prospective study. J Hand Surg 2013; 38A: 1377–1382. [DOI] [PubMed] [Google Scholar]
- 33.Kho JY, Adams BD, O'Rourke H. Outcome of semi-constrained total elbow arthroplasty in posttraumatic conditions with analysis of bushing wear on stress radiographs. Iowa Orthop J 2015; 35: 125–129. [PMC free article] [PubMed] [Google Scholar]
- 34.Pogliacomi F, Aliani D, Cavaciocchi M, et al. Total elbow arthroplasty in distal humeral nonunion: clinical and radiographic evaluation after a minimum follow-up of three years. J Shoulder Elbow Surg 2015; 24: 1998–2007. [DOI] [PubMed] [Google Scholar]
- 35.Ersen A, Demirhan M, Atalar AC, et al. Is Coonrad–Morrey total elbow arthroplasty a viable option for treatment of distal humeral nonunions in the elderly?. Acta Orthop Traumatol Turc 2015; 49: 354–360. [DOI] [PubMed] [Google Scholar]
- 36.Barthel PY, Mansat P, Sirveaux F, et al. Is total elbow arthroplasty indicated in the treatment of traumatic sequelae? 19 cases of Coonrad–Morrey reviewed at a mean follow-up of 5.2 years. Orthop Traumatol Surg Res 2014; 100: 113–118. [DOI] [PubMed] [Google Scholar]
- 37.Prasad N, Dent C. Outcome of total elbow replacement for distal humeral fractures in the elderly: a comparison of primary surgery and surgery after failed internal fixation or conservative treatment. J Bone Joint Surg Br 2008; 90: 343–348. [DOI] [PubMed] [Google Scholar]
- 38.Schneeberger AG, Adams R, Morrey BF. Semi constrained total elbow replacement for the treatment of post-traumatic osteoarthrosis. J Bone Joint Surg 1977; 79: 1211–1222. [DOI] [PubMed] [Google Scholar]
- 39.Morrey BF, Adams RA, Bryan RS. Total replacement for post-traumatic arthritis of the elbow. J Bone Joint Surg Br 1991; 73: 607–612. [DOI] [PubMed] [Google Scholar]
- 40.Ernstbrunner L, Hingsammer A, Imam MA, et al. Long-term results of total elbow arthroplasty in patients with haemophilia. J Shoulder Elbow Surg 2018; 27: 126–132. [DOI] [PubMed] [Google Scholar]
- 41.Casadei R, De PaolisM, Drago G, et al. Total elbow arthroplasty for primary and metastatic tumor. Orthop Traumatol Surg Res 2016; 102: 459–465. [DOI] [PubMed] [Google Scholar]
- 42.Vochteloo AJ, Roche SJ, Dachs RP, et al. Total elbow arthroplasty in bleeding disorders: an additional series of 8 cases. J Shoulder Elbow Surg 2015; 24: 773–778. [DOI] [PubMed] [Google Scholar]
- 43.Athwal GS, Chin PY, Adams RA, et al. Coonrad–Morrey total elbow arthroplasty for tumours of the distal humerus and elbow. J Bone Joint Surg Br 2005; 87: 1369–1374. [DOI] [PubMed] [Google Scholar]
- 44.Na KT, Song SW, Lee YM, et al. Modified triceps fascial tongue approach for primary total elbow arthroplasty. J Shoulder Elbow Surg 2018; 27: 887–893. [DOI] [PubMed] [Google Scholar]
- 45.Frostick SP, Elsheikh AA, Mohammed AA, et al. Results of cementless total elbow arthroplasty using the Discovery elbow system at a mean follow-up of 61.8 months. J Shoulder Elbow Surg 2017; 26: 1348–1354. [DOI] [PubMed] [Google Scholar]
- 46.Metha SS, Watts AC, Talwalkar SC, et al. Early results of Latitude primary total elbow replacement with a minimum follow-up of 2 years. J Shoulder Elbow Surg 2017; 26: 1867–1872. [DOI] [PubMed] [Google Scholar]
- 47.Alizadehkhaiyat O, Mandhari AA, Sinopidis C, et al. Total elbow arthroplasty: a prospective clinical outcome study of Discovery elbow system with a 4-year mean follow up. J Shoulder Elbow Surg 2015; 24: 52–59. [DOI] [PubMed] [Google Scholar]
- 48.Kiran M, Jariwala A, Wigderowitz C. Medium term outcomes of primary and revision Coonrad–Morrey total elbow replacement. Indian J Orthop 2015; 49: 233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Waegner ML, de Vos MJ, Hannink G, et al. Mid-term clinical results of a modern convertible total elbow arthroplasty. J Bone Joint Surg 2015; 97: 691–699. [DOI] [PubMed] [Google Scholar]
- 50.Large R, Tambe A, Cresswell T, et al. Medium-term clinical results of a linked total elbow replacement system. J Bone Joint Surg 2014; 96: 1359–1365. [DOI] [PubMed] [Google Scholar]
- 51.Maheswari R, Vaziri S, Helm RH. Total elbow replacement with Coonrad–Morrey prosthesis: our medium to long-term results. Ann R Coll Surg Engl 2012; 94: 189–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hastings H, Lee DH, Pietrzak WS. A prospective multicentre clinical study of the Discovery elbow. J Shoulder Elbow Surg 2014; 23: e95–e107. [DOI] [PubMed] [Google Scholar]
- 53.Mansat P, Bonnevialle N, Rongieres M, et al. Experience with the Coonrad–Morrey total elbow arthroplasty: 78 consecutive total elbow arthroplasties reviewed with an average 5 years of follow-up. J Shoulder Elbow Surg 2013; 22: 1461–1468. [DOI] [PubMed] [Google Scholar]
- 54.Corradi M, Frattini M, Panno B, et al. Linked semi-constrained total elbow prosthesis in chronic arthritis: results of 18 cases. Musculoskelet Surg 2010; 94: S11–S23. [DOI] [PubMed] [Google Scholar]
- 55.Celli A, Morrey BF. Total elbow arthroplasty in patients forty years of age or less. J Bone Joint Surg Am 2009; 91: 1414–1418. [DOI] [PubMed] [Google Scholar]
- 56.Shi LL, Zurakowski D, Jones DG, et al. Semi constrained primary and revision total elbow arthroplasty with use of the Coonrad–Morrey prosthesis. J Bone Joint Surg Am 2007; 89: 1467–1475. [DOI] [PubMed] [Google Scholar]
- 57.Schneeberger AG, Meyer DC, Yian EH. Coonrad–Morrey total elbow replacement for primary and revision surgery: a 2- to 7.5-year follow-up study. J Shoulder Elbow Surg 2007; 16: 47–54. [DOI] [PubMed] [Google Scholar]
- 58.Aldridge JM, Lightdale NR, Mallon WJ, et al. Total elbow arthroplasty with the Coonrad/Coonrad–Morrey prosthesis. J Bone Joint Surg Br 2006; 88: 509–514. [DOI] [PubMed] [Google Scholar]
- 59.Hildebrand KA, Patterson SD, Regan WD, et al. Functional outcome of semi constrained total elbow arthroplasty. J Bone Joint Surg Am 2000; 82: 1379–1386. [DOI] [PubMed] [Google Scholar]
- 60.Wright TW, Wong AM, Jaffe R. Functional outcome comparison of semi constrained and unconstrained total elbow arthroplasties. J Shoulder Elbow Surg 2000; 9: 524–531. [DOI] [PubMed] [Google Scholar]
- 61.Schoch BS, Werthel JD, Sanchez-Sotelo J, et al. Total elbow arthroplasty for primary osteoarthritis. J Shoulder Elbow Surg 2017; 26: 1355–1359. [DOI] [PubMed] [Google Scholar]
- 62.Krukhaug Y, Hallan G, Dybvik E, et al. A survivorship study of 838 total elbow replacements: a report from the Norwegian Arthroplasty Register 1994-2016. J Shoulder Elbow Surg 2018; 27: 260–269. [DOI] [PubMed] [Google Scholar]
- 63.Plaschke HC, Thillemann TM, Brorson S, et al. Implant survival after total elbow arthroplasty: a retrospective study of 324 procedures performed from 1980 to 2008. J Shoulder Elbow Surg 2014; 23: 829–836. [DOI] [PubMed] [Google Scholar]
- 64.Kim JM, Mudgal CS, Konopka JF, et al. Complications of total elbow arthroplasty. J Am Acad Orthop Surg 2011; 19: 328–339. [DOI] [PubMed] [Google Scholar]
- 65.Lubiatowski P, Olczak I, Lisiewicz E, et al. Clinical and functional evaluation of patients after total elbow arthroplasty. Pol Orthop Traumatol 2013; 78: 53–58. [PubMed] [Google Scholar]
- 66.Inagaki K. Current concepts of elbow-joint disorders and their treatment. J Orthop Sci 2013; 18: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Vollans S, Limb D. Elbow replacement for elective elbow conditions. Orthop Trauma 2016; 30: 322–328. [Google Scholar]
- 68.Fevang BT, Lie SA, Havelin LI, et al. Results after 562 total elbow replacements: a report from the Norwegian Arthroplasty Register. J Shoulder Elbow Surg 2009; 18: 449–456. [DOI] [PubMed] [Google Scholar]
- 69.Skytta ET, Eskelinen A, Paavolainen P, et al. Total elbow arthroplasty in rheumatoid arthritis. A population-based study from the Finnish Arthroplasty Register. Acta Orthop 2009; 80: 472–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schoch BS, Wong J, Abboud J, et al. Results of total elbow arthroplasty in patients less than 50 years old. J Hand Surg 2017; 42: 797–802. [DOI] [PubMed] [Google Scholar]
- 71.Ali A, Shahane S, Stanley D. Total elbow arthroplasty for distal humeral fractures: Indications, surgical approach, technical tips, and outcome. J Shoulder Elbow Surg 2010; 19: 53–58. [DOI] [PubMed] [Google Scholar]
- 72.McKee MD, Veillette CJ, Hall JA, et al. A multicenter, prospective, randomized, controlled trial of open reduction–internal fixation versus total elbow arthroplasty for displaced intra-articular distal humeral fractures in elderly patients. J Shoulder Elbow Surg 2009; 18: 3–12. [DOI] [PubMed] [Google Scholar]
- 73.Egol KA, Tsai P, Vazquez O, et al. Comparison of functional outcomes of total elbow arthroplasty vs plate fixation for distal humerus fractures in osteoporotic elbows. Am J Orthop 2011; 40: 67–71. [PubMed] [Google Scholar]
- 74.Baghdadi YMK, Veillette CJH, Malone AA, et al. Total elbow arthroplasty in obese patients. J Bone Joint Surg Am 2014; 96: e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Griffin JW, Werner BC, Gwathmey FW, et al. Obesity is associated with increased postoperative complications after total elbow arthroplasty. J Shoulder Elbow Surg 2015; 24: 1594–1601. [DOI] [PubMed] [Google Scholar]
- 76.Palvanen M, Kannus P, Niemi S, et al. Secular trends in distal humeral fractures of elderly women: nationwide statistics in Finland between 1970 and 2007. Bone 2010; 46: 1355–1358. [DOI] [PubMed] [Google Scholar]
- 77.Charissoux JL, Mabit C, Fourastier J, et al. Comminuted intra-articular fractures of the distal humerus in elderly patients. Rev Chir Orthop Reparatrice Appar Mot 2008; 94: S36–S62. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplemental Material1 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Supplemental material, Supplemental Material2 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Supplemental material, Supplemental Material3 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Supplemental material, Supplemental Material4 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Supplemental material, Supplemental Material5 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Supplemental material, Supplemental Material6 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Supplemental material, Supplemental Material7 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow
Supplemental material, Supplemental Material8 for Indications and outcome in total elbow arthroplasty: A systematic review by Vasileios Samdanis, Gopikanthan Manoharan, Robert W Jordan, Adam C Watts, Paul Jenkins, Rohit Kulkarni, Michael Thomas, Amar Rangan and Stuart M Hay in Shoulder & Elbow