Abstract
Introduction
Both regional analgesia and intravenous analgesia are frequently used perioperatively for patients with critical limb ischaemia (CLI). Nevertheless, the comparison of perioperative effect of regional and intravenous analgesia has not yet been thoroughly illustrated. This study will comprehensively compare patient-controlled regional analgesia (PCRA) and patient-controlled intravenous analgesia (PCIA) as two different perioperative analgesia approaches for patients with CLI. It investigates their effects on analgesia, reperfusion and the quality of recovery perioperatively, also aims to provide clinical evidence to those non-surgical patients with non-reconstructable arteries.
Methods and analysis
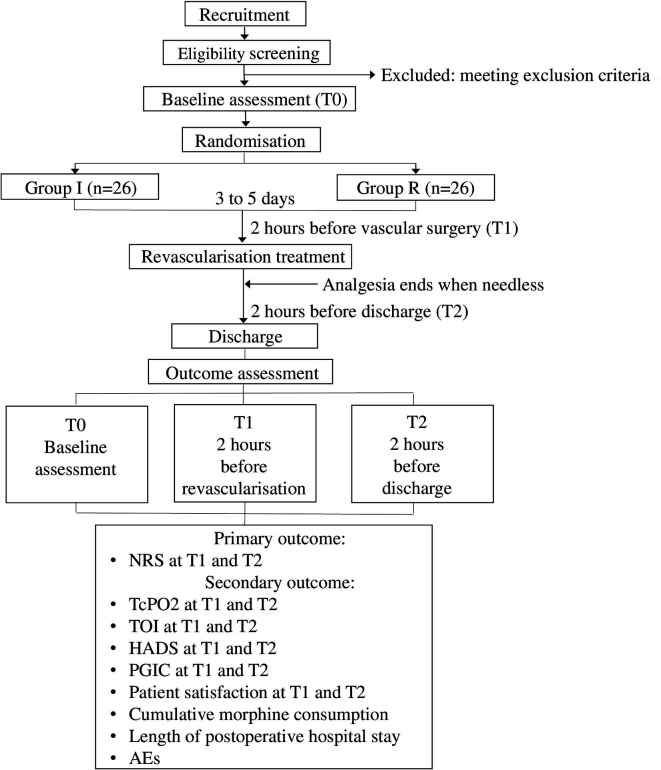
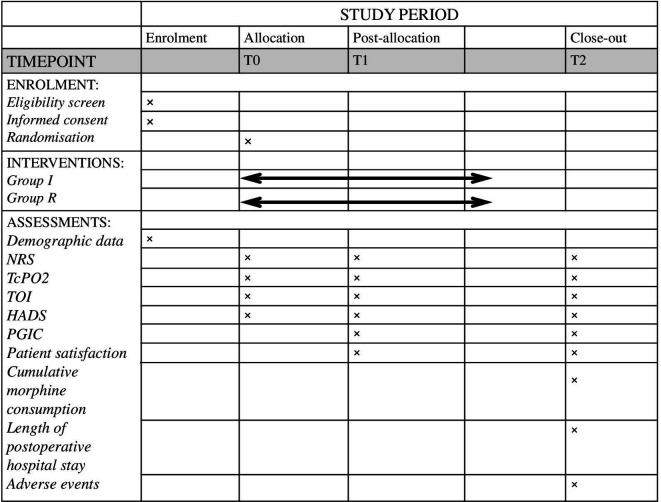
This trial is a randomised, single-centre, open-label, parallel trial with target sample size of 52 in total. Eligible participants will be randomly allocated to the PCRA group (group R) or the PCIA group (group I) after admission. Participants in group R will receive ultrasound-guided subgluteal sciatic catheterisation, followed by continuous PCRA infusion (0.2% ropivacaine 15 mL as loading dose, 8 mL/hour as background with a patient-controlled bolus of 6 mL). Participants in group I will receive PCIA (morphine is given in boluses of 1 mg as needed, background infusion at 1 mg/hour). Data will be collected at baseline (T0), 2 hours before revascularisation treatment (T1) and 2 hours before discharge (T2). The primary outcomes include the Numerical Rating Scale pain score at T1 and T2. The secondary outcomes include the perioperative transcutaneous oxygen pressure, the Tissue Haemoglobin Index, Hospital Anxiety and Depression Scale at T1 and T2; the Patient Global Impression of Change and patient satisfaction at T1 and T2; the perioperative cumulative morphine consumption, the length of postoperative hospital stay and adverse events.
Ethics and dissemination
This study received authorisation from the Institutional Review Board of Peking Union Medical College Hospital on 21 March 2017 (approval no. ZS-1289X). Study findings will be disseminated through presentations at scientific conferences or publications in peer-reviewed journals.
Trial registration number
Chinese Clinical Trial Registry (ChiCTR2000029298).
Protocol version
V.4CP.B2 (15 June 2020).
Keywords: vascular surgery, pain management
Strengths and limitations of this study.
Aiming to compare the perioperative efficacy of two different analgesia approaches, this study will assess their effects on analgesia, reperfusion, as well as the quality of recovery, rather than their effects on analgesia alone.
Patient-controlled analgesia is used in this study so that the perioperative pain management for patients with critical limb ischaemia could be individual and continuous. The analgesia approaches cover the perioperative period thoroughly.
Two different principle-based measuring parameters are used to evaluate the reperfusion effect. Transcutaneous oxygen pressure is by heating skin to a stable hyperaemia equilibrium condition, Tissue Haemoglobin Index is by detecting the absorption and reflection of near-infrared light.
As an open-labelled trial, all participants and some of the investigators are aware of group assignment, their expectation may introduce bias.
Introduction
Critical limb ischaemia (CLI) presents the end stage of peripheral arterial disease (PAD).1 CLI is clinically defined as ischaemic rest pain, ulcers and gangrene in the presence of haemodynamic evidence of arterial insufficiency.2 The mean annual incidence of CLI was 0.35% reported in a national investigation from the USA.3 The prevalence is approximately 1% of the adult population, and up to 10% of patients with PAD may have CLI. In recent years, a consensus from Peripheral Academic Research Consortium has provided an objective haemodynamic definition for CLI.4 In this study, this consensus definition will also be used to diagnose CLI.
The major goal of CLI treatment is to relieve ischaemic pain, improve limb perfusion, heal wounds and prevent further tissue loss.5 The Inter-Society Consensus for the Management of Peripheral Arterial Disease emphasised the importance of the pain management for patients with CLI and recommended a multidisciplinary approach to control pain.1 Pain control is important not only to improve quality of life, but also reduce the possibility of phantom limb pain.6 7 For patients with PAD, the general principles of perioperative pain management should be individual, continuous and cover the whole perioperative period thoroughly.8 Over the past years, the patient-controlled analgesia has become the mainstay for providing postoperative pain relief.9 Accordingly, we considered to establish patient-controlled analgesia preoperatively in our study. Existing studies suggested that intravenous morphine10 and ultrasound-guided peripheral nerve block provided satisfactory analgesia effect on patients with CLI.11–14 However, the analgesia effect of intravenous morphine and ultrasound-guided regional block has not been compared before. Therefore, in this study, we plan to compare the perioperative analgesia effect of patient-controlled regional analgesia (PCRA) and patient-controlled intravenous analgesia (PCIA) for patients diagnosed with CLI.
Additionally, few of the previous studies have studied the effects on reperfusion besides analgesia. A previous prospective study showed that continuous peridural ropivacaine infusion provided satisfactory analgesia, dilated vessels, reconstructed collateral circulation and improved reperfusion remarkably in patients with diabetes.15 Regional analgesia can cause changes in vascular blood flow, but data with regard to perioperative experiences of patients with CLI are limited. Therefore, in this study, the reperfusion effect of the PCRA and PCIA methods will be further evaluated within participants with CLI. To compare the effect on reperfusion between the two analgesia approaches, we plan to use two different principle-based measuring parameters, namely, the perioperative transcutaneous oxygen pressure (TcPO2) and the Tissue Haemoglobin Index (TOI). TcPO2 is a transcutaneous, conventional clinical parameter measured heating a skin tissue in the range of 37℃–45℃ to reach a stable hyperaemia equilibrium condition.16 Near-infrared spectroscopy (NIRS) detects the absorption and reflection of near-infrared light and has the potential to provide continuous, real-time measurement of both blood volume and cellular respiration in skin tissue. Other perioperative data regarding the quality of recovery, such as the patients’ emotional state, global impression of change, patient satisfaction, perioperative morphine consumption, length of postoperative hospital stay and adverse events (AEs) will be investigated as well.
Objective
The objectives of this randomised controlled trial are to compare the perioperative analgesia efficacy between PCRA and PCIA for patients with CLI. The perioperative effect on peripheral inflow perfusion, emotion, patient global impression of change (PGIC), patient satisfaction, morphine consumption, length of postoperative hospital stay, and AEs of PCRA and PCIA will also be evaluated and compared.
Methods and analysis
Overall design
This trial is a randomised, single-centre, open-label, parallel trial, and will be carried out in Peking Union Medical College Hospital (PUMCH). Institutional research ethics board approval was obtained from PUMCH Institutional Review Board (IRB) (No. ZS-1289X, 21 March 2017). An overall flow diagram is provided in figure 1. The timing of interventions and data collection is detailed in figure 2. This protocol was designed in accordance with the Standard Protocol Items: Recommendations for Interventional Trials guidelines,17 the checklist can be found in online supplemental appendix 1. The trial will be conducted at PUMCH in accordance with the Good Clinical Practice-International Conference on Harmonisation (GCP-ICH) guidelines.
Figure 1.
Study process diagram. AEs, adverse events; HADS, Hospital Anxiety and Depression Scale; NRS, Numerical Rating Scale; PGIC, patient global impression of change; TcPO2, transcutaneous oxygen pressure; TOI, Tissue Haemoglobin Index.
Figure 2.
Schedule of the enrolment, interventions and assessments. HADS, Hospital Anxiety and Depression Scale; NRS, Numerical Rating Scale; PGIC, patient global impression of change; TcPO2, transcutaneous oxygen pressure; TOI, Tissue Haemoglobin Index.
bmjopen-2020-037879supp001.pdf (76.5KB, pdf)
Recruitment
Recruitment for this study will begin on 27 July 2020. Full written informed consents will be obtained from each participant by a qualified member of the research team prior to any trial-related procedures.
Inclusion criteria
Participants who meet the following criteria will be enrolled in this trial:
18–80 years of age.
Diagnosed with critical limb ischaemia,2 4 admitted in hospital for elective surgery treatment, either open surgical or endovascular revascularisation.
The lesions are mainly unilateral and in the supplied area of sciatic nerve.
Stage 6 in Rutherford symptom classification system.18
American Society of Anesthesiology physical status II–III.
Exclusion criteria
Participants who meet the following criteria will be excluded:
Are taking opioids before admission.
Have known allergy to the drugs that will be used in the study.
Have severe liver or kidney dysfunction.
Have contraindication for the catheterisation (eg, infection at injection site, coagulation disorders, refuse or be unable to cooperate with the procedure).
The dorsum of the affected foot is not intact.
Are unable to understand the scales or to describe to the investigators.
Dropout criteria
Participants who meet the following criteria will be withdrawn from the study:
Not willing to continue their participation or cannot follow the initial treatment plan.
From whom none of the primary outcome data can be obtained due to any reason.
Randomisation, sequence concealment and blinding
All eligible participants will be randomly allocated to either group R or the group I in a ratio of 1:1 using the R software (R Foundation for Statistical Computing). The random allocation sequence will be computer-generated by an independent researcher who has no contact with any participant and will not be involved in the following research. The participants’ respective treatment group (group R or group I) will be sealed in an opaque envelope and will only be opened after the enrolment of the participants in the study. An investigator will be responsible for enrolling patients, obtaining consent form and requesting randomisation.
This study is an open-label study whereby the participants, the personnel who carry out the intervention and the outcome assessor cannot be blinded because of the nature of the intervention. However, the researchers who are responsible for the statistical analysis will be blinded to the allocation.
Interventions
Analgesia approaches will be established after the baseline assessment (T0) and randomisation, normally 3–5 days before the revascularisation treatment. The FORNIA CPE-101 electronic infusion pump will be used as the continuous patient-controlled analgesia device. Relevant concomitant intervention is not involved in this study. Analgesics outside the intervention plan are prohibited during the trial. Remedial analgesia therapy will be carried out according to clinical needs for participants who are dropped out from the trial.
The PCRA group (group R)
Ultrasound-guided continuous subgluteal sciatic block will be applied on the participants enrolled in the group R. Patient will be placed partly lateral and partly prone, with the legs flexed in the hip and knee. Scanning begins in the depression between the greater trochanter of femur and the ischial tuberosity using the 8-3 MHz curved probe of the ultrasound equipment (X-porte, SONOSITE, USA). The sciatic nerve can be identified in the cross-sectional view in between of the two bones, below the gluteus muscle. Then rotate the transducer 90° so that the sciatic nerve is imaged in the longitudinal view. Insert needle in-plane from the cranial to caudal direction and underneath the fascia to enter the subgluteal space, then advance the needle until the tip is adjacent to the nerve. After confirming the needle placement by obtaining a motor response of the calf and foot using the peripheral nerve stimulator, inject 0.2% ropivacaine 15 mL for loading dose, then insert the catheter 5 cm beyond the needle tip in vicinity of the sciatic nerve. Finally, secure the catheter by tunnelling and taping. The infusion strategy includes 0.2% ropivacaine at 8 mL/hour as background with a patient-controlled bolus of 6 mL, lockout time 30 min, 1 hour limit 20 mL.
The PCIA group (group I)
For the participants enrolled in the group I, PCIA will be connected after intravenous access is established. The infusion strategy is as follows: intravenous morphine is given in boluses of 1 mg as needed, background infusion 1 mg/hour, with a lockout time of 20 min. The 1-hour limit is 4 mg morphine.
The intraoperative and postoperative patient management
The continuous patient-controlled analgesia will not be suspended during the revascularisation treatment despite the type of anaesthesia method. After the revascularisation, the device will be paused when patients report it is no longer needed, which usually takes several days. The device will be on standby for an additional 48 hours before removal. In case of inadequate analgesia is provided perioperatively, the infusion strategy dosage may be increased for patients in group I, extra doses of intravenous morphine may be used and recorded for patients in group R. Ancillary and post-care will not be involved in this study.
Outcomes
Primary outcomes
The primary outcome of this trial is the Numerical Rating Scale (NRS). NRS allows patients to describe the intensity of pain, which is 11-point scale ranging from 0 to 10, with 0 defined as no pain and 10 defined as the worst pain imaginable.19 The measurement timepoint of the primary outcome will be 2 hours before revascularisation treatment (T1) and 2 hours before discharge (T2).
Secondary outcomes
The secondary outcomes are as follows:
The TcPO2 at T1 and T2. TcPO2 will be obtained with PeriFlux System 5000 (PERIMED, Sweden) transcutaneously using the TcPO2 unit-PF 5040. Calibration will be completed before use. When measuring, patients will be in sitting position. The electrode of the PF 5040 will be placed on the dorsum of the affected foot, away from any skin lesion. Wait 10–15 min for a stable reading.
The TOI at T1 and T2. TOI will be obtained with the EGOS-600A NIRS (ENGINMED, China). The transducer of NIRS will be placed at the same spot as PF5040 on a sitting position, after the completion of TcPO2 measurement. Wait 30 s for each interval to gain five readings. The values at each timepoint will be calculated as the mean of five consecutive values over 2 min.
Hospital Anxiety and Depression Scale (HADS) at T1 and T2. HADS is a self-rating patient-reported outcome measure developed to assess depression and anxiety of patients with illness. The 24-item questionnaire is divided into two subscales: anxiety (HADS-A) and depression (HADS-D). The ratings are summed to yield a total score (0–42), or for each subscale (0–21) with special attention.20
PGIC at T1 and T2. PGIC is a 7-point verbal scale commonly used to assess patient’s perception of pain relief following treatment, which has proven its significant relevance and correlations for peripheral neuropathic pain in daily practice.21
Patient satisfaction at T1 and T2. This item allows patients to describe their satisfaction in medical procedures according to the experience in hospital using a 11-point scale from 0 to 10, with 0 defined as extremely dissatisfied and 10 defined as vastly satisfied.
Cumulative morphine consumption perioperatively, the sum will be calculated before discharge.
Length of postoperative hospital stay.
AEs, such as haematoma, catheter displacement, nausea, vomiting, drowsiness, dizziness, urinary retention, pruritus, local anaesthesia intoxication, fall and others. The occurrence time, nature, duration and severity of AEs will all be collected in detail.
Trial safety
The establishment, configuration and dispensing of the patient-controlled analgesia devices will be completed by a dependable anaesthesiologist. The continuous ultrasound-guided subgluteal sciatic block will be performed in an operating room, only after intravenous access and standard monitoring is established for the patient. Investigators will follow up the patient at least two times per day during the research. Motor block will be assessed every day using Bromage Motor Blockade Score22 in group R to prevent falling. All the reported AEs and other unintended effects of trial conduct will be collected, assessed, reported and managed according to the GCP-ICH guidelines. Any severe AE happens perioperatively will be reported to the adverse event registration system of the hospital.
Patient and public involvement
Patients and public were not involved in the development of the research question or in the design of the study. Patients will receive oral and written information about this trial. However, they will not be involved in the recruitment and conduct of the study. The burden of the intervention will be assessed by patients themselves. On completion of the study, dissemination of the general study results or the anonymised individual patient data will be made on demand.
Sample size
The primary outcome of this trial is the NRS score after analgesia. Sample size was calculated based on our pilot study which had included ten patients in total (five for each group). The result of the pilot study showed that the NRS scores in group R and group I were 1.63 and 3.31, and the SD was 1.85 and 2.12, respectively. We used the statistical power of 80% and two-sided α of 0.05. The target sample size for each group is at least 22 participants. Taking into account a dropout rate of 20%, a sample size of 52 (26 for each group) was finally determined.
Data collection, monitoring and confidentiality
Each patient’s ID and demographic information (including age, gender, height, weight) will be collected. We will document all the AEs related to PCRA or PCIA, including haematoma, catheter displacement, local anaesthesia intoxication, nausea, dizziness, urinary retention, pruritus, fall and others. All the calibration and measurements of TcPO2 and TOI will be performed and recorded by one special technician using the same apparatuses. Participant retention and follow-up engagement is enhanced by communicating verbally and via a common instant message app. In the case where primary outcome data are missing at T2, investigators will call the participants within 2 days of discharge to collect the missing data. Collected data will be recorded on paper case report forms (CRFs), then entered into electronic case report forms (eCRFs) and uploaded to a central server. The CRFs and eCRFs will be kept for at least 5 years after publication in case of any inquiry. A qualified clinical trial expert will be invited in the middle and at the end of the investigation to ensure that the protocol and GCP-ICH are being followed. No interim analysis will be performed during the study. There is no planned auditing for the study. Personal information about the enrolled participants will be safely and confidentially kept. After completion of the study, the eCRFs and all the data collected will be stored anonymously in the password-protected central server and restricted to relevant members of the research team. Paper copies of the CRFs will be stored in a locked cabinet in the relevant research office.
Statistical analyses
Continuous variables will first be checked for normality using the visual inspection of the histogram. Normally distributed continuous variables will be expressed as the mean±SD, and non-normally distributed continuous variables will be expressed as the median and IQR. The categorical variables will be summarised as frequencies and percentages. Variables such as anaesthesia method and surgery type will be checked in the description of baseline characteristics, unbalanced variables will be adjusted using a multivariable method. The primary outcome, difference of NRS between groups, which is generally normally distributed from experience, will be analysed using Student’s t-test, and the mean difference with corresponding one-sided 95% CI will be calculated. For the secondary outcomes including TcPO2, TOI, HADs and PGIC, Student’s t-test will be used to compare the group difference. Data with a skewed distribution, such as cumulative morphine consumption and length of postoperative hospital stay, will be analysed using the Mann-Whitney U test. As categorical variables, AEs will be compared using Χ2 test. A post-hoc subgroup analysis by the type of revascularisation treatment (whether endovascular or open surgical) will be conducted. The main analysis will be performed after the study has been completed. Data analysis will be performed according to the intention-to-treat principle. The results of this study will be reported according to the Consolidated Standards of Reporting Trials statement.23 Statistical analyses will be conducted using SPSS 19.0. A two-sided p<0.05 is considered significant.
Ethics and dissemination
Ethics approval and consent to participate
This research project was approved by the PUMCH IRB (ZS-1289X) on 21 March 2017. Important protocol amendments will be communicated with relevant parties (eg, investigators, IRB, trial participants, trial registries, journals) by Dr Yuehong Zheng, trial principal investigator, as soon as changes are made. Written informed consent (details see online supplemental appendix 2) will be obtained from all participants.
bmjopen-2020-037879supp002.pdf (113.1KB, pdf)
Dissemination plan
The result of this study will be presented in national and international meetings and will be submitted for publication to relevant vascular surgery, analgesia or anaesthesia peer-reviewed journals. Authorship eligibility will follow the Good Publication Practice guideline 3.
Trial organisation
Steering Committee
The Steering Committee carries the ultimate responsibility for the trial and has access to the final dataset. Specific tasks of the Steering Committee are: final approval of the study protocol, approval of the amendments to the study protocol, approval of manuscripts and publications of the trial. The Steering Committee is chaired by Yuehong Zheng, vascular surgery surgeon. Other members include Si Chen, anaesthesiologist and Yuelun Zhang, statistician.
Data and Safety Monitoring Committee (DSMC)
The DSMC is established to assess the progress of the study, the safety of data and the critical efficacy end points independently from the sponsor and competing interests. Well-being of the participants will be monitored by the DSMC, who makes decision on the suspension or termination of the trial to protect the participants under circumstances of severe or unexpected AEs. The DSMC is chaired by Yuguang Huang, anaesthesiologist. Other members include Hongju Liu, anaesthesiologist and Yuexin Chen, vascular surgery surgeon.
Trial status and time scale
The study was funded and ethically approved in 2017. A pilot study was conducted subsequently. We had finished the pilot study by 8 July 2018, then the study was delayed because of the maternity leave of Si Chen until January 2020. The trial was registered on 22 January 2020 and will begin to recruit participants on 27 July 2020.
Discussion
The purpose of this study is to compare the analgesia effect of PCRA and PCIA. The effects on reperfusion and quality of recovery are meanwhile investigated in patients diagnosed with CLI.
In this study, a low concentration ropivacaine of 0.2% will be used for patients in group R, and a low to median dosage of intravenous morphine will be used for patients of group I. Morphine is a strong opioid which is well known for its supreme analgesia and adverse effects such as nausea, vomiting, drowsiness, itching and others. Ropivacaine is a long-acting regional anaesthetic that blocks nerve fibres involved in pain transmission to a greater degree than those controlling motor functions.24
Regional analgesia can cause changes in vascular blood flow, but data with regard to perioperative experiences of patients with CLI are limited. In this study, we plan to perform two different measuring methods to observe the effects on reperfusion of PCRA and PCIA. In previous researches, the parameter TOI was also known as the region tissue oxygenation saturation (rSO2). A recent study has revealed a significant correlation between TcPO2 and rSO2 measured by NIRS to evaluate limb ischaemia in patients with peripheral arterial disease.25 We expect the outcomes of this study provide clinical evidence for the efficacy of the two different analgesia approaches perioperatively.
We also hope this study offers a reference for the non-surgical patients. Although revascularisation has been the most effective treatment for patients with CLI, some patients’ arteries are impossible to revascularise and require other treatments such as drugs,26 transcutaneous electrical stimulation,27 peripheral blood mononuclear cells therapy28 or lumbar sympathectomy29 to relieve pain and/or increase peripheral perfusion to avoid amputation. For those patients with non-reconstructable arteries, long-term PCRA may be less invasive and adequate for both analgesia and perfusion. There are evidences showing that it is safe to discharge patient home with catheter.30 In addition, it has been previously reported that continuous sciatic nerve block could be used at home for long-term pain control.31 We expect this perioperative study can also be a future reference for those who lost their opportunity for revascularisation to improve their quality of life.
Supplementary Material
Acknowledgments
We acknowledge Chinese Anesthesiologist Association for funding this study. We would also like to thank Dujian Wang for her valuable effort on the investigation.
Footnotes
Contributors: SC and ZX are joint first authors. SC obtained funding and the ethical approval, registered and drafted the manuscript. ZX and YZ conceived the study and participated in the design of the study. YH, HL and YC participated in the study coordination. YZ contributed to the statistical analysis plan. JZ acquired and analysed the data of the work. YZ is the corresponding author. He critically edited the manuscript. All authors read and approved the final manuscript and agreed the submission.
Funding: This work was supported by Young Scholar Research Grant of Chinese Anesthesiologist Association (220160900007). Contact information: +86-0717-6345093, mail@ycrenfu.com.cn.
Disclaimer: The funders will not participate in the study design and management; data collection, analysis and interpretation; report writing; or publication.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Norgren L, Hiatt WR, Dormandy JA, et al. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg 2007;45 Suppl S:S5–67. 10.1016/j.jvs.2006.12.037 [DOI] [PubMed] [Google Scholar]
- 2.Fontaine R, Kim M, Kieny R. [Surgical treatment of peripheral circulation disorders]. Helv Chir Acta 1954;21:499–533. [PubMed] [Google Scholar]
- 3.Nehler MR, Duval S, Diao L, et al. Epidemiology of peripheral arterial disease and critical limb ischemia in an insured national population. J Vasc Surg 2014;60:686–95. 10.1016/j.jvs.2014.03.290 [DOI] [PubMed] [Google Scholar]
- 4.Patel MR, Conte MS, Cutlip DE, et al. Evaluation and treatment of patients with lower extremity peripheral artery disease: consensus definitions from peripheral academic research Consortium (PARC). J Am Coll Cardiol 2015;65:931–41. 10.1016/j.jacc.2014.12.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farber A, Eberhardt RT. The current state of critical limb ischemia: a systematic review. JAMA Surg 2016;151:1070–7. 10.1001/jamasurg.2016.2018 [DOI] [PubMed] [Google Scholar]
- 6.Collins TC, Beyth RJ, Nelson DB, et al. Process of care and outcomes in patients with peripheral arterial disease. J Gen Intern Med 2007;22:942–8. 10.1007/s11606-007-0203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu CL, Tella P, Staats PS, et al. Analgesic effects of intravenous lidocaine and morphine on postamputation pain: a randomized double-blind, active placebo-controlled, crossover trial. Anesthesiology 2002;96:841–8. 10.1097/00000542-200204000-00010 [DOI] [PubMed] [Google Scholar]
- 8.Bloomquist T. Amputation and phantom limb pain: a pain-prevention model. Aana J 2001;69:211–7. [PubMed] [Google Scholar]
- 9.Taylor A, Stanbury L. A review of postoperative pain management and the challenges. Current Anaesthesia & Critical Care 2009;20:188–94. 10.1016/j.cacc.2009.02.003 [DOI] [Google Scholar]
- 10.Vahidi E, Shakoor D, Aghaie Meybodi M, et al. Comparison of intravenous lidocaine versus morphine in alleviating pain in patients with critical limb ischaemia. Emerg Med J 2015;32:516–9. 10.1136/emermed-2014-203944 [DOI] [PubMed] [Google Scholar]
- 11.Azuma N, Kikuchi S, Okuda H, et al. Recent progress of bypass surgery to the Dialysis-Dependent patients with critical limb ischemia. Ann Vasc Dis 2017;10:178–84. 10.3400/avd.ra.17-00076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tureli D, Deniz S, Unlukaplan A, et al. Ultrasound-Guided popliteal sciatic block provides adequate analgesia during urgent endovascular treatment of critical limb ischemia with resting pain. Cardiovasc Intervent Radiol 2018;41:43–8. 10.1007/s00270-017-1802-2 [DOI] [PubMed] [Google Scholar]
- 13.Sgroi MD, McFarland G, Mell MW. Utilization of regional versus general anesthesia and its impact on lower extremity bypass outcomes. J Vasc Surg 2019;69:1874–9. 10.1016/j.jvs.2018.08.190 [DOI] [PubMed] [Google Scholar]
- 14.Kontopodis N, Papaioannou A, Tavlas E, et al. The use of local anesthesia to perform lower limb revascularization in the fragile patient with critical limb ischemia. G Chir 2018;39:77–81. [PubMed] [Google Scholar]
- 15.Di Minno MND, Milone M, Russolillo A, et al. Ropivacaine infusion in diabetics subject with peripheral arterial disease. A prospective study. Exp Clin Endocrinol Diabetes 2013;121:91–3. 10.1055/s-0032-1327757 [DOI] [PubMed] [Google Scholar]
- 16.Cobb J, Claremont D. Noninvasive measurement techniques for monitoring of microvascular function in the diabetic foot. Int J Low Extrem Wounds 2002;1:161–9. 10.1177/153473460200100303 [DOI] [PubMed] [Google Scholar]
- 17.Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. Spirit 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rutherford RB, Baker JD, Ernst C, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg 1997;26:517–38. 10.1016/S0741-5214(97)70045-4 [DOI] [PubMed] [Google Scholar]
- 19.Lee JJ, Lee MK, Kim JE, et al. Pain relief scale is more highly correlated with numerical rating scale than with visual analogue scale in chronic pain patients. Pain Physician 2015;18:E195–200. [PubMed] [Google Scholar]
- 20.Beekman E, Verhagen A. Clinimetrics: Hospital anxiety and depression scale. J Physiother 2018;64:198. 10.1016/j.jphys.2018.04.003 [DOI] [PubMed] [Google Scholar]
- 21.Perrot S, Lantéri-Minet M. Patients' global impression of change in the management of peripheral neuropathic pain: clinical relevance and correlations in daily practice. Eur J Pain 2019;23:1117–28. 10.1002/ejp.1378 [DOI] [PubMed] [Google Scholar]
- 22.Craig D, Carli F. Bromage motor blockade score - a score that has lasted more than a lifetime. Can J Anaesth 2018;65:837–8. 10.1007/s12630-018-1101-7 [DOI] [PubMed] [Google Scholar]
- 23.Moher D, Hopewell S, Schulz KF, et al. Consort 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 2010;63:e1–37. 10.1016/j.jclinepi.2010.03.004 [DOI] [PubMed] [Google Scholar]
- 24.McClellan KJ, Faulds D. Ropivacaine: an update of its use in regional anaesthesia. Drugs 2000;60:1065–93. 10.2165/00003495-200060050-00007 [DOI] [PubMed] [Google Scholar]
- 25.Yata T, Sano M, Kayama T, et al. Utility of a Finger-Mounted tissue oximeter with near-infrared spectroscopy to evaluate limb ischemia in patients with peripheral arterial disease. Ann Vasc Dis 2019;12:36–43. 10.3400/avd.oa.18-00117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Laoire Áine Ní, Murtagh FEM. Systematic review of pharmacological therapies for the management of ischaemic pain in patients with non-reconstructable critical limb ischaemia. BMJ Support Palliat Care 2018;8:400–10. 10.1136/bmjspcare-2017-001359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mifsud M, Cassar K. The use of transcutaneous electrical stimulation of the calf in patients undergoing infrainguinal bypass surgery. Ann Vasc Surg 2015;29:1524–32. 10.1016/j.avsg.2015.05.040 [DOI] [PubMed] [Google Scholar]
- 28.Persiani F, Paolini A, Camilli D, et al. Peripheral blood mononuclear cells therapy for treatment of lower limb ischemia in diabetic patients: a single-center experience. Ann Vasc Surg 2018;53:190–6. 10.1016/j.avsg.2018.05.036 [DOI] [PubMed] [Google Scholar]
- 29.Karanth VK, Karanth TK, Karanth L, et al. Lumbar sympathectomy techniques for critical lower limb ischaemia due to non-reconstructable peripheral arterial disease. Cochrane Database Syst Rev 2016;12:CD011519. 10.1002/14651858.CD011519.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.King R, Mariano ER, Yajnik M, et al. Outcomes of ambulatory upper extremity surgery patients discharged home with perineural catheters from a Veterans health administration medical center. Pain Med 2019;20:2256–62. 10.1093/pm/pnz023 [DOI] [PubMed] [Google Scholar]
- 31.Ilfeld BM, Morey TE, Wang RD, et al. Continuous popliteal sciatic nerve block for postoperative pain control at home: a randomized, double-blinded, placebo-controlled study. Anesthesiology 2002;97:959–65. 10.1097/00000542-200210000-00031 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-037879supp001.pdf (76.5KB, pdf)
bmjopen-2020-037879supp002.pdf (113.1KB, pdf)