Abstract
Elderly patients awaiting lung resection surgery often have poor physical function, which puts them at a high risk of postoperative pulmonary complications. The aim of this study was to investigate the impact of preoperative physical performance on postoperative pulmonary complications in patients awaiting lung resection surgery. In this prospective multicenter cohort study, the characteristics of patients and postoperative pulmonary complications were compared between subjects with low (<10) and high (≥10) Short Physical Performance Battery (SPPB) scores. Postoperative pulmonary complications were defined as over grade II in Clavien-Dindo classification system. We estimated the effects of physical performance on postoperative pulmonary complications using multivariable hierarchical logistic regression. The postoperative pulmonary complications were compared between 331 patients in the high and 33 patients in the low SPPB group. Patients in the low SPPB score group had a significantly higher rate of postoperative pulmonary complications (p < 0.001). Low SPPB score was associated with a higher risk of postoperative pulmonary complications (odds ratio, 8.80; p < 0.001). The SPPB is a clinically useful evaluation tool to assess surgical patients’ physical performance. The low physical performance indicated by the SPPB may be predictive of postoperative pulmonary complications after lung resection surgery.
Trial registration: Clinical Trials. University hospital Medical Information Network Center (UMIN-CTR) UMIN000021875.
Keywords: The Short Physical Performance Battery, physical performance, thoracic surgery, postoperative complication, physiotherapy
Introduction
Lung resection surgery offers patients with lung cancer a chance of complete cure; however, it is associated with an increased risk of postoperative pulmonary complications.1 Previous studies have reported incident rates of postoperative pneumonia ranging from 3–10% after lung resection surgery.2,3 Postoperative pulmonary complications have an important clinical and economic impact associated with increased morbidity and mortality.4 Thus, preventing postoperative pulmonary complications of lung resection surgery is important.
Preoperative functional capacity is predictive of postoperative pulmonary complications of lung resection surgery. The elderly patients, especially those with poor functional capacity, are at an increased risk of postoperative pulmonary complications.5 Previous studies reported preoperative functional capacity to influence postoperative pulmonary complications in patients who underwent lung resection surgery.6,7 Functional capacity on the 6-minute walking test (6MWT) in patients who underwent lung resection was significantly associated with postoperative pulmonary complications.
Bui et al. reported that exercise capacity and physical performance are components of functional capacity based on the International Classification of Functioning, Disability and Health framework presents.8 The 6MWT evaluate exercise tolerance among functional capacity.9 The elderly have various problems related to physical performance in addition to exercise intolerance. Hence, an appropriate assessment tool is required to evaluate physical performance in the elderly awaiting lung resection surgery.
The Short Physical Performance Battery (SPPB), a simple tool to evaluate physical performance, has recently attracted considerable attention.10 It is a useful and well-established tool for evaluating physical performance of the elderly.10,11 The SPPB is used widely as a performance-based, three-part assessment to measure functional status. The SBBP has many advantages; it takes only takes a few minutes to complete, requires little training to administer and can be conducted in a small space. In addition, the results can be quantified, are reproducible and sensitive to changes in functionality through time.12 Preoperative evaluation of physical performance using SPPB has been associated with postoperative course in cardiac surgery, pancreaticoduodenectomy as well as lung and kidney transplantation surgeries.13–17 However, the relationship between poor preoperative physical performance as evaluated using SPPB and postoperative pulmonary complications in patients who underwent lung resection surgery has not been investigated. We hypothesized that poor preoperative physical performance evaluated by the SPPB in these patients may have an impact on postoperative pulmonary complications and the progress of postoperative course. Therefore, the aim of the present study was to evaluate the impact of preoperative physical performance evaluated by SPPB on postoperative pulmonary complications and course in patients undergoing lung resection surgery.
Methods
Study design
In this prospective multicenter cohort study, we enrolled patients who underwent lung resection surgery at five hospitals from November 2015 to December 2017. The inclusion criteria were patients older than 65 years, undergoing planned surgery, and able to provide written informed consent. Patients were excluded if their exercise performance could not be evaluated due to the comorbid conditions (e.g., musculoskeletal or neurological impairment) or if they had undergone re-operation. The Human Ethics Review Committees of Nagasaki University Hospital (approval number: 15100506), Steel Memorial Yawata Hospital (approval number: 15-58), KKR Takamatsu Hospital (approval number: E93), Japan Community Health care Organization Hokkaido Hospital (approval number: 2016-3) and Seirei Mikatahara General Hospital (approval number: 16-14) approved this study, which was registered at UMIN-CTR (http://www.umin.ac.jp/ctr/) by UMIN000021875.
Outcomes
All patients received standard perioperative management, nursing care and physical therapy according to the management protocols. Physical therapy focused on early mobilization, resistance training, and walking starting postoperative day (POD) 1.
The Short Physical Performance Battery (SPPB) was used to measure physical performance.10 The SPPB consists of three measures including walking speed, chair stands, and standing balance. Each performance measurement was assigned a score from 0 (inability to complete) to 4 (best performance possible). The total of the scores (0–12) was used to obtain an overall measurement of physical performance. In accordance with previous studies,14–16 patients were classified into low physical performance-related risk (SPPB < 10) or no physical performance-related risk (SPPB ≥ 10).
Preoperative nutritional status was evaluated using the Geriatric Nutritional Risk Index (GNRI). This is an established nutritional assessment tool and a predictor of morbidity and mortality in the elderly.18 The GNRI is based on three parameters: height, body weight, and serum albumin level. The GNRI was calculated as follows: 14.89 × serum albumin (g/dl) + 41.7 × body mass index (BMI)/22.
Modified Frailty Index (mFI) has been used in various surgical settings.19,20 The simplified mFI is a predictive tool, consisting of 11 variables, that provides a practical platform to gauge frailty during preoperative assessment. The variables used in mFI help predict clinical outcomes and quantify risk of complications independent of age.21
Postoperative pulmonary complications were evaluated using the Clavien-Dindo classification system that includes 5 grades, where grade I indicates any deviation from the normal postoperative course, but without the need for pharmacologic, surgical, endoscopic, and radiologic interventions while grade 5 indicates patient’s death.22 Patients with severity over grade II were classified as having postoperative pulmonary complications.23
We measured handgrip force (HF) and quadriceps force (QF) as indices of peripheral muscle strength. The HF of the dominant hand was evaluated in the standing position with the elbow extended and the arms fixed to the body using a dynamometer (T.K.K.5401; Takei-Kiki-Kogyou Corporation, Niigata, Japan). The QF was assessed as the peak force achieved during a maximal isometric knee extension maneuver using a hand-held dynamometer with a fixing belt (μ-Tas F-1; Anima Corporation, Tokyo, Japan).24 The QF of the dominant side was measured in a sitting position with the hip and knee joint flexed at approximately 90°. The average value of at least three attempts was recorded and notated in kilograms force (kgf) for HF and newtons (N) for QF.
The 6MWT was performed twice according to the published guidelines.25 The higher 6-min walk distance (6MWD) from the two attempts was recorded. Percutaneous oxygen saturation (SpO2) was recorded at baseline. Moreover, the lowest SpO2 value was recorded during and immediately after the test.
The Barthel Index was used to assess functional independence in activities of daily living (ADL).26 The scale evaluates 10 domains of activities (feeding, bathing, grooming, dressing, bowels, bladder, toilet use, transfer, walking, and climbing stairs). For each of the 10 items a score was assigned in increments of 5 (0, 5, 10, and 15). Subjects were given points even if they utilized aids to be independent. Total score from this assessment was used in the analysis.
The primary outcome of this study was the risk of SPPB score as an assessment of preoperative physical performance on the proportion of postoperative pulmonary complications. The secondary outcome was to extract independent factors related to preoperative physical performance using SPPB and postoperative pulmonary complications in lung resection surgery patients.
Statistical analysis
The categorical variables were described using numbers and percentages, while the quantitative variables using median and interquartile range (IQR). Data were compared using a Wilcoxon’s rank sum test and Fisher’s exact test between the high and low SPPB groups. We estimated the risk of preoperative physical performance on postoperative pulmonary complications using multivariable hierarchical logistic regression models. We selected SPPB and 6MWD as exposure variables to represent preoperative physical performance. The SPPB was treated as a binary and 6MWD as a continuous variable. For clinical relevance, age, gender, modified frailty index score, blood loss, GNRI and QF were selected as confounding factors. Hierarchical regression model was employed to take into account the possibility of interhospital variation. Due to the small number of events in the outcome, 29, it may not be reasonable to include these confounders in models. Therefore, we used model 1 as our model, in which age and gender were confounders that were likely to cause strong confounding. The model, including all confounders, was used as model 2 for sensitivity analysis. The effect measures of each exposure variable was assessed with odds ratios, confidence intervals [95% CI], and P-values. P-values < 0.05 were considered statistically significant. Statistical analyses were performed using JMP 14.0 software (SAS Institute Japan, Tokyo, Japan).
Results
A total of 470 patients awaiting lung resection surgery were screened. One hundred six patients were excluded from the analysis as they were under the age of 65 years, missing data and re-operation. Data from 364 patients who underwent lung resection surgery were analyzed. Patients’ baseline characteristics are described in Table 1. All patients had lung cancer and most had a severity stage of 1. Forty-one patients of unknown were recurrent of lung cancer and could not apply severity classification. Postoperative pulmonary complications of the respiratory system were found in 29 patients (8.0%): pneumonia in 13 patients (44.8%), pulmonary fistula in 9 patients (31.0%), atelectasis in 3 patients (10.3%), pleural effusion in 4 patients (13.8%).
Table 1.
Patients’ demographics and postoperative progress between groups.
| All patients (n = 364) | SPPB < 10 (n = 33) | SPPB ≥ 10 (n = 331) | p Value | ||||
|---|---|---|---|---|---|---|---|
| Age, years | 73 | (69–78) | 79 | (76–81) | 72 | (68–77) | <0.001 |
| Male, n (%) | 205 | (56.3) | 14 | (42.4) | 191 | (57.7) | 0.100 |
| BMI, kg/m2 | 22 | (20–25) | 22.1 | (19.6–23.8) | 22.3 | (20.5–25.0) | 0.425 |
| GNRI | 103 | (95–109) | 98.6 | (89.3–108.7) | 102.8 | (95.5–109.1) | 0.158 |
| Preoperative chemotherapy, n (%) | 33 | (9.1) | 1 | (3.0) | 32 | (9.7) | 0.338 |
| Preoperative comorbidities (respiratory), n (%) | 87 | (23.9) | 12 | (36.4) | 75 | (22.7) | 0.090 |
| Stage, n (%) | 0.935 | ||||||
| 1 | 247 | (67.9) | 23 | (71.9) | 224 | (69.6) | |
| 2 | 49 | (13.5) | 4 | (12.5) | 45 | (14.0) | |
| 3 | 21 | (5.8) | 2 | (6.3) | 19 | (5.9) | |
| 4 | 6 | (1.6) | 0 | 6 | (1.9) | ||
| Unknown | 41 | (11.3) | 4 | (12.5) | 37 | (11.2) | |
| Pulmonary function test | |||||||
| FVC, % | 104.6 | (91.8–117.4) | 98.5 | (87.1–109.9) | 105.2 | (92.6–117.5) | 0.087 |
| FEV1, %pred | 101.2 | (89.8–116.2) | 94.0 | (82.3–115.3) | 102.2 | (91.1–131.0) | 0.063 |
| FEV1/FVC, % | 73.4 | (68.0–79.2) | 73.8 | (64.6–80.1) | 73.4 | (68.1–79.2) | 0.903 |
| Side of resection (%) | 0.044 | ||||||
| Right | 203 | (55.8) | 24 | (72.7) | 179 | (54.1) | |
| Left | 161 | (44.2) | 9 | (27.3) | 152 | (45.9) | |
| Surgical procedure (%) | 0.652 | ||||||
| Pneumonectomy | 1 | (0.3) | 0 | 1 | (0.3) | ||
| Lobectomy | 300 | (82.4) | 27 | (81.8) | 273 | (82.5) | |
| Upper or middle lobectomy | 234 | (64.3) | 17 | (51.5) | 213 | (64.4) | |
| Lower lobectomy | 130 | (35.7) | 16 | (48.5) | 114 | (34.4) | |
| Others | 63 | (17.3) | 6 | (18.2) | 57 | (17.2) | |
| mFIS, n (%) | 0.896 | ||||||
| 0 | 124 | (34.1) | 10 | (30.3) | 114 | (34.4) | |
| 1 | 149 | (40.9) | 13 | (39.4) | 136 | (41.1) | |
| 2 | 74 | (20.3) | 8 | (24.2) | 66 | (19.9) | |
| ≥3 | 17 | (4.7) | 2 | (6.1) | 15 | (4.5) | |
| Handgrip force (dominant), kgf | 26 | (19–33) | 17.4 | (14.0–21.8) | 27 | (19.9–33.0) | <0.001 |
| Quadriceps muscle force (dominant), N | 264 | (194–343) | 192.6 | (144.8–265.6) | 272.7 | (204.5–347.3) | <0.001 |
| 6MWD, m | 490 | (420–545) | 317 | (240–390) | 500 | (433–550) | <0.001 |
| SPPB | 33 | (9.1) | |||||
| Balance, point | 4 | (4–4) | 2 | (1–2) | 4 | (4–4) | <0.001 |
| 4 m Gait speed, point | 4 | (4–4) | 3 | (2–4) | 4 | (4–4) | <0.001 |
| Sit to Stand, point | 4 | (4–4) | 3 | (2–4) | 4 | (4–4) | <0.001 |
| Gait speed, m/sec | 3.6 | (3.1–4.1) | 5.0 | (4.0–6.1) | 3.6 | (3.1–4.0) | <0.001 |
| Sit to Stand, sec | 8.0 | (6.6–10.0) | 11.9 | (10.1–15.4) | 7.8 | (6.5–9.5) | <0.001 |
| ASA-PS, n (%) | 0.537 | ||||||
| 1 | 42 | (11.5) | 2 | (6.1) | 40 | (12.1) | |
| 2 | 295 | (81.0) | 29 | (87.9) | 266 | (80.4) | |
| 3 | 27 | (7.4) | 2 | (6.1) | 25 | (7.6) | |
| Operative time, sec | 190 | (151–237) | 191 | (135–248) | 190 | (151–234) | 0.859 |
| Blood loss, g | 55 | (20–130) | 50 | (20–132) | 55 | (20–130) | 0.858 |
| Clavien-Dindo classification ≥ 2 on POD 7, n (%) | 29 | (8.0) | 9 | (27.3) | 20 | (6.0) | <0.001 |
| Initial walking, days | 1 | (1–1) | 1 | (1–2) | 1 | (1–1) | <0.001 |
| ADL (Barthel Index) on POD 7, days | 95 | (85–100) | 85 | (70–100) | 95 | (85–100) | 0.050 |
| Length of hospital stay, days | 10 | (7–14) | 11 | (8–14) | 10 | (7–14) | 0.324 |
Notes: Values are reported as the median (interquartile range) or number of patients (percentage).
Abbreviations: ASA-PS: The American Society of Anesthesiologists–Physical Status classification system; BMI: body mass index; GNRI: geriatric nutritional risk index; N: newton; mFIS: modified frailty index score; POD: postoperative day; SPPB: short physical performance battery; TNM classification: tumor-node-metastasis classification; 6MWD: 6-minutes walking distance.
Footnote: The simplified mFIS is a predictive tool to gauge frailty pre-operation, help predict clinical outcomes and quantify risk of complications. Minimum permissible value, 0; maximum permissible value, 11.
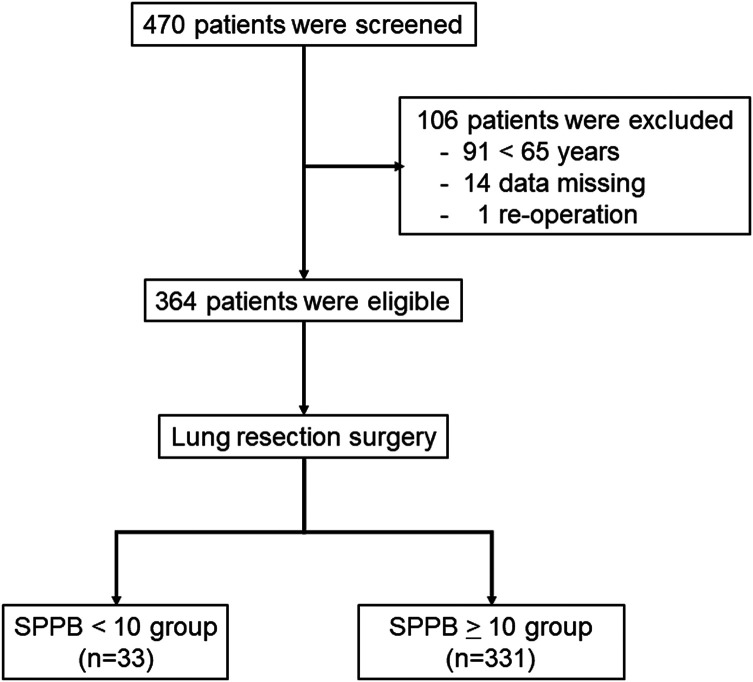
The patients were categorized based on physical performance-related risk: 331 in the high SPPB group (SPPB ≥ 10) (median age = 72; IQR = 68–77 years) and 33 in the low SPPB group (SPPB < 10) (median age = 79; IQR = 76–81 years) (Figure 1). Age of low SPPB group was significantly higher than the high SPPB group (p < 0.001). There were no significant differences in surgical procedure (p < 0.652). Based on the preoperative HF, QF and 6MWD, the high SPPB group had significantly higher performance than the low SPPB group (Table 1). The Clavien-Dindo grading (>2) on POD 7 indicated that post-operative complications are significantly greater in low SPPB group than the high SPPB group [9 patients (27.3%) vs. 20 patients (6.0%), respectively; p < 0.001]. There were no significant differences in the length of hospitalization. There was significant association of GNRI (OR: 0.99, 95% CI, 0.99 to 0.99; p < 0.001), 6MWD per 10 meters (OR: 0.98, 95% CI, 0.97 to 0.99; p < 0.001) and SPPB (OR: 7.02, 95% CI, 4.66 to 10.6; p < 0.001) on postoperative pulmonary complications (Table 2). The SPPB was significantly correlated with HF and QF (r = 0.31 p < 0.01, r = 0.15 p < 0.01, respectively), but not mFI and GNRI.
Figure 1.
Flow of patients through the study. Abbreviations: SPPB: short physical performance battery.
Table 2.
Results for determining factors associated with postoperative complications on POD 7.
| Variable | Unadjusted | ||
|---|---|---|---|
| OR | (95% CI) | p Value | |
| Age | 1.03 | (0.99 to 1.06) | 0.184 |
| Gender | 0.70 | (0.40 to 1.23) | 0.218 |
| Modified frailty index score | 1.25 | (0.95 to 1.65) | 0.108 |
| Blood loss | 1.00 | (1.00 to 1.00) | 0.085 |
| GNRI | 0.99 | (0.99 to 0.99) | <0.001 |
| Quadriceps force | 1.00 | (1.00 to 1.00) | 0.834 |
| 6MWD per 10 m | 0.98 | (0.97 to 0.99) | <0.001 |
| SPPB (≥10 = 0, <10 = 1) | 7.02 | (4.66 to 10.6) | <0.001 |
Abbreviations: 95% CI: 95-percent confidence interval; GNRI: geriatric nutritional risk index; OR: odds ratio, SPPB: short physical performance battery; 6MWD: 6-minutes walking distance.
Multivariable hierarchical logistic regression analyses showed that low SPPB score <10 was associated with a higher risk of postoperative pulmonary complications (odds ratio [OR] 9.74, 95% CI, 5.80 to 16.3; p < 0.001) (Table 3). There was a significant association of 6MWD per 10 meters on postoperative pulmonary complications (OR: 0.97, 95% CI, 0.97 to 0.99; p < 0.001). A Low SPPB score was found to be more strongly associated with the postoperative pulmonary complications than 6MWD. A similar result was obtained in the sensitivity analysis, model 2.
Table 3.
Factors associated with postoperative complications on POD 7.
| Exposure variable | Model 1* | Model 2** | ||||
|---|---|---|---|---|---|---|
| OR | (95% CI) | p Value | OR | (95% CI) | p Value | |
| 6MWD per 10 m | 0.97 | (0.97 to 0.99) | <0.001 | 0.98 | (0.97 to 0.99) | 0.001 |
| SPPB (≥10 = 0, <10 = 1) | 9.74 | (5.80 to 16.3) | <0.001 | 8.80 | (5.64 to 13.7) | <0.001 |
Abbreviations: ADL: activities of daily living; 95% CI: 95-percent confidence interval; GNRI: geriatric nutritional risk index; OR: odds ratio; SPPB: short physical performance battery; 6MWD: 6-minutes walking distance; POD: postoperative day.
* Adjusted for age and gender.
** Adjusted for age, gender, modified frailty index score, blood loss, GNRI, and quadriceps force.
Discussion
To our knowledge, this is the first multicenter trial to evaluate the influence of preoperative physical performance using SPPB on postoperative pulmonary complications and recovery course in patients undergoing lung resection surgery. The main findings include (1) low SPPB group (lower preoperative physical performance) had greater postoperative pulmonary complications than the high SPPB group; and (2) preoperative low SPPB score was associated with postoperative pulmonary complications.
We demonstrated that postoperative pulmonary complications in the low SPPB group were significantly higher than the high SPPB group. Dale et al.14 showed that SPPB is a clinically useful measurement tool to predict postoperative complications in pancreaticoduodenectomy patients. Although a different clinical population, our results were consistent confirming the relationship between preoperative physical performance and postoperative complications. The importance of preoperative interventions including physiotherapy for maintaining physical performance has been reported to facilitate physiological optimization of the cardiorespiratory and musculoskeletal systems, and mitigating the effects of general anesthesia.27 Maintaining preoperative physical function and/or improving exercise capacity could facilitate postoperative early mobilization, mitigate the effects of general anesthesia and important to the prevention of postoperative pulmonary complications by promoting increased ventilation and improved clearance of secretions in the lungs.
In our results, poor physical performance evaluated by SPPB was identified to affect postoperative pulmonary complications. Verweij et al.28 documented that physical performance tests including SPPB appear to show a significant correlation with survival and could be used as a prognostic tool, particularly for elderly patients. In this study, 29 of 364 (8.0%) patients were found to have postoperative pulmonary complications on POD 7. Among them, 13 (3.6%) patients had postoperative pneumonia, and incident rates of postoperative pneumonia were approximately 3–4%. These results are consistent with those found in this study.2,3 Ellenberger et al.29 showed that a direct relationship between poor pre-operative physical performance and postoperative pulmonary complications. It has been shown that patients with lung cancer, who are at risk of poor physical function preoperatively may benefit from physiotherapy to improve physical function before surgery to prevent postoperative pulmonary complications, shorten hospital length of stay and lower in-hospital cost.17,30 Overall, physical performance in perioperative patients is one of the most important factors when considering postoperative outcomes. Further larger scale studies that include longitudinal assessment of physical performance to investigate whether preoperative physical performance affects postoperative pulmonary complications are necessary.
Moreover, the relationships between SPPB and other measures were explored by correlation analysis. The SPPB was significantly correlated to HF and QF, measure of peripheral muscle force, but not mFI (measure as preoperative comorbidity) and GNRI (measure of preoperative nutrition status). These results indicate that skeletal muscle strength may affect SPPB rather than preoperative comorbidities and nutritional status.
Several previous studies6,7 evaluated preoperative exercise capacity using 6MWD. However, as previously stated, 6MWD is a test of exercise tolerance and is only one aspect of functional capacity. The SPPB assesses three measures including walking speed, chair stands, and standing balance; it is an excellent, multifaceted tool to evaluate different aspects of physical performance and lower limb function to identify frail adults.31 Our results of multivariable hierarchical logistic regression indicated low SPPB score to be a better predictor of postoperative pulmonary complications than 6MWD. Especially, elderly patients may have difficulty walking long distances, and SPPB may be able to identify the risk of postoperative pulmonary complications. Although 6MWT and SPPB assess different aspects of functional capacity and cannot be compared generally, our results recommend SPPB as a simple assessment tool in elderly patients who are awaiting lung resection surgery.
This study has several limitations. Firstly, this study was limited by the short postoperative period. Functional assessments over longer periods are required to further evaluate the predictive and prognostic significance of the SPPB in postoperative patients undergoing lung resection surgery. Secondly, although, a hierarchical regression model was executed considering the possibility of inter-hospital variation, perioperative management is variable across institutes, which may have influenced the postoperative complications. However, multicenter trial is also a strength of this study that captured that variability in management protocols. Thirdly, SPPB can have a ceiling effect affecting highly functioning patients.9 In this study, 25.6% of the subjects had a full score on SPPB, and the effect of the ceiling effect of SPPB can’t be denied. Therefore, SPPB may not be suitable for highly functional patients awaiting lung resection surgery.
Conclusion
The present study indicated that preoperative physical performance assessed with SPPB in patients who underwent lung resection surgery could affect postoperative pulmonary complications. Assessing patients undergoing lung resection surgery using SPPB could help stratify patients at risk of postoperative pulmonary complications. Thus, consideration of pre-operative countermeasures against physical performance is necessary.
Acknowledgments
The authors are grateful to the surgeons, physical therapists and all the staff who acquired data for study. We acknowledge Mr. S. Ahmed Hassan from Rehabilitation Sciences Institute, University of Toronto, Toronto, Canada, for his support in English review.
Footnotes
Author contributions: MH, KY and RK planned the study. MH, KY, SM, YO, YY collected the data. MH, KY, TM, TN, RK performed the statistical analysis and drafted the manuscript. MH, KY, SM, YO, YY, TM, TN, RK participated in its design and coordination. All authors read and approved the final manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Masatoshi Hanada  https://orcid.org/0000-0002-6201-4921
https://orcid.org/0000-0002-6201-4921
Yohei Oyama  https://orcid.org/0000-0001-5406-0242
https://orcid.org/0000-0001-5406-0242
References
- 1. Cavalheri V, Granger C. Preoperative exercise training for patients with non-small cell lung cancer. Cochrane Database Syst Rev 2017; 6: CD012020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Andalib A, Ramana-Kumar AV, Bartlett G, et al. Influence of postoperative infectious complications on long-term survival of lung cancer patients: a population-based cohort study. J Thorac Oncol 2013; 8(5): 554–561. [DOI] [PubMed] [Google Scholar]
- 3. Shiono S, Yoshida J, Nishimura M, et al. Risk factors of postoperative respiratory infections in lung cancer surgery. J Thorac Oncol 2007; 2(1): 34–38. [DOI] [PubMed] [Google Scholar]
- 4. Agostini P, Cieslik H, Rathinam S, et al. Postoperative pulmonary complications following thoracic surgery: Are there any modifiable risk factors? Thorax 2010; 65(9): 815–818. [DOI] [PubMed] [Google Scholar]
- 5. Mistry PK, Gaunay GS, Hoenig DM. Prediction of surgical complications in the elderly: Can we improve outcomes? Asian J Urol 2017; 4(1): 44–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Irie M, Nakanishi R, Yasuda M, et al. Risk factors for short-term outcomes after thoracoscopic lobectomy for lung cancer. Eur Respir J 2016; 48(2): 495–503. [DOI] [PubMed] [Google Scholar]
- 7. Hattori K, Matsuda T, Takagi Y, et al. Preoperative six-minute walk distance is associated with pneumonia after lung resection. Interact Cardiovasc Thorac Surg 2018; 26(2): 277–283. [DOI] [PubMed] [Google Scholar]
- 8. Bui KL, Nyberg A, Maltais F, et al. Functional tests in chronic obstructive pulmonary disease, part 1: clinical relevance and links to the International Classification of Functioning, Disability, and Health. Ann Am Thorac Soc 2017; 14(5): 778–784. [DOI] [PubMed] [Google Scholar]
- 9. Larsson P, Borge CR, Nygren-Bonnier M, et al. An evaluation of the short physical performance battery following pulmonary rehabilitation in patients with chronic obstructive pulmonary disease. BMC Res Notes 2018; 11(1): 348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994; 49(2): M85–M94. [DOI] [PubMed] [Google Scholar]
- 11. Pavasini R, Guralnik J, Brown JC, et al. Short physical performance battery and all-cause mortality: systematic review and meta-analysis. BMC Med 2016; 14(1): 215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bergland A, Strand BH. Norwegian reference values for the short physical performance battery (SPPB): the Tromsø study. BMC Geriatr 2019; 19(1): 216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kato M, Saitoh M, Kawamura T, et al. Postoperative atrial fibrillation is associated with delayed early rehabilitation after heart valve surgery: a multicenter study. Phys Ther Res 2019; 22(1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dale W, Hemmerich J, Kamm A, et al. Geriatric assessment improves prediction of surgical outcomes in older adults undergoing pancreaticoduodenectomy: a prospective cohort study. Ann Surg 2014; 259(5): 960–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nastasi AJ, Bryant TS, Le JT, et al. Pre-kidney transplant lower extremity impairment and transplant length of stay: a time-to-discharge analysis of a prospective cohort study. BMC Geriatr 2018; 18(1): 246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yuguchi S, Saitoh M, Oura K, et al. Impact of preoperative frailty on regaining walking ability in patients after cardiac surgery: multicenter cohort study in Japan. Arch Gerontol Geriatr 2019; 83: 204–210. [DOI] [PubMed] [Google Scholar]
- 17. Singer JP, Diamond JM, Anderson MR, et al. Frailty phenotypes and mortality after lung transplantation: a prospective cohort study. Am J Transplant 2018; 18(8): 1995–2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bouillanne O, Morineau G, Dupont C, et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr 2005; 82(4): 777–783. [DOI] [PubMed] [Google Scholar]
- 19. Dunne MJ, Abah U, Scarci M. Frailty assessment in thoracic surgery. Interact Cardiovasc Thorac Surg 2014; 18(5): 667–670. [DOI] [PubMed] [Google Scholar]
- 20. Wachal B, Johnson M, Burchell A, et al. Association of modified frailty index score with perioperative risk for patients undergoing total laryngectomy. JAMA Otolaryngol Head Neck Surg 2017; 143(8): 818–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Velanovich V, Antoine H, Swartz A, et al. Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. J Surg Res 2013; 183(1): 104–110. [DOI] [PubMed] [Google Scholar]
- 22. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240(2): 205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Shinohara S, Kobayashi K, Kasahara C, et al. Long-term impact of complications after lung resections in non-small cell lung cancer. J Thorac Dis 2019; 11(5): 2024–2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Katoh M, Yamasaki H. Test-retest reliability of isometric leg muscle strength measurements made using a hand-held dynamometer restrained by a belt: comparisons during and between sessions. J Phys Ther Sci 2009; 21: 239–243. [Google Scholar]
- 25. Holland AE, Spruit MA, Troosters T, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J 2014; 44(6): 1428–1446. [DOI] [PubMed] [Google Scholar]
- 26. Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J 1965; 14: 61–65. [PubMed] [Google Scholar]
- 27. Snowdon D, Haines TP, Skinner EH. Preoperative intervention reduces postoperative pulmonary complications but not length of stay in cardiac surgical patients: a systematic review. J Physiother 2014; 60(2): 66–77. [DOI] [PubMed] [Google Scholar]
- 28. Verweij NM, Schiphorst AH, Pronk A, et al. Physical performance measures for predicting outcome in cancer patients: a systematic review. Acta Oncol 2016; 55(12): 1386–1391. [DOI] [PubMed] [Google Scholar]
- 29. Ellenberger C, Garofano N, Reynaud T, et al. Patient and procedural features predicting early and mid-term outcome after radical surgery for non-small cell lung cancer. J Thorac Dis 2018; 10(11): 6020–6029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lai Y, Wang X, Zhou K, et al. Impact of one-week preoperative physical training on clinical outcomes of surgical lung cancer patients with limited lung function: a randomized trial. Ann Transl Med 2019; 7(20): 544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Abizanda P, Romero L, Sánchez-Jurado PM, et al. Association between functional assessment instruments and frailty in older adults: the FRADEA study. J Frailty Aging 2012; 1(4): 162–168. [DOI] [PubMed] [Google Scholar]