The introduction of state insurance mandates for ASD are associated with greater workforce supply of behavioral analysts and child psychiatrists but not pediatricians.
Abstract
BACKGROUND:
State mandates have required insurance companies to provide coverage for autism-related child health care services; however, it has not been determined if insurance mandates have improved the supply of child health care providers. We investigate the effect of state insurance mandates on the supply of child psychiatrists, pediatricians, and board-certified behavioral analysts (BCBAs).
METHODS:
We used data from the National Conference of State Legislatures and Health Resources and Services Administration’s Area Health Resource Files to examine child psychiatrists, pediatricians, and BCBAs in all 50 states from 2003 to 2017. Fixed-effects regression models compared change in workforce density before versus one year after mandate implementation and the effect of mandate generosity across 44 US states implementing mandates between 2003 and 2017.
RESULTS:
From 2003 to 2017, child psychiatrists increased from 7.40 to 10.03 per 100 000 children, pediatricians from 62.35 to 68.86, and BCBAs from 1.34 to 29.88. Mandate introduction was associated with an additional increase of 0.77 BCBAs per 100 000 children (95% confidence interval [CI]: 0.18 to 1.42) one year after mandate enactment. Mandate introduction was also associated with a more modest increase among child psychiatrists (95% CI: 0.10 to 0.91) and was not associated with the prevalence of pediatricians (95% CI: −0.76 to 1.13). We also found evidence that more generous mandate benefits were associated with larger effects on workforce supply.
CONCLUSIONS:
State insurance mandates were associated with an ∼16% increase in BCBAs from 2003 to 2017, but the association with child psychiatrists was smaller and nonsignificant among pediatricians. In these findings, it is suggested that policies are needed that specifically address workforce constraints in the provision of services for children with autism spectrum disorder.
What’s Known on this Subject:
State mandates requiring that insurance companies provide coverage for autism-related child health care services have resulted in modest effects on service use and spending.
What this Study Adds:
In this study, it is indicated that state insurance mandates have had a significant but modest effect on the size of the US workforce for autism-related child health care services, suggesting that other policies may be necessary to address a shortage of care for autism spectrum disorder.
Over the past 2 decades, all US states and the District of Columbia have enacted laws requiring health insurers provide coverage for autism-related child health care services, including physical and behavioral health care; speech, occupational, and physical therapy; and applied behavioral analysis (ABA).1 Although these laws, known as state insurance mandates, contain exemptions,2 they have aimed to respond to an increase in the identified prevalence of autism spectrum disorder (ASD).3 As a neurologic and developmental disorder beginning in early childhood,4 ASD often requires up to 40 hours per week of educational intervention5 and significant ongoing health care services throughout childhood and adolescence.6
These mandates appear to have had significant but modest impacts on autism-related health care use and spending among children with ASD. In one recent study, the authors found that the probability of using ASD-specific pediatric services in a month was 27.9% in states with mandates versus 25.0% in nonmandate states.7 Others have observed that monthly family spending on autism-related child health care services has increased by <$100 as a function of mandates.7–10 One potential explanation for these limited impacts is that mandates primarily remove financial barriers to accessing care but do not directly address a shortage in service availability: more than half of US counties have no board-certified behavioral analysts (BCBAs) who provide therapy to help children with ASD improve social and communication skills. More than 70% have no child psychiatrists.11 Additionally, a majority of mental health treatment facilities do not provide behavioral health care services for children with ASD.12 However, there is a paucity of information regarding whether insurance mandates have impacted workforce availability.13
We evaluated the effect of state insurance mandates on workforce supply of three types of health care providers that commonly provide services to children with ASD (BCBAs, child psychiatrists, and pediatricians) over a 15-year period (2003–2017) during which 44 states introduced mandates. We anticipated mandates would be associated with a modest increase in BCBAs14 but unrelated to supply of child psychiatrists and pediatricians because these latter roles are often overwhelmed by existing patient volume11,15 and children with ASD likely represent a small percentage of their patient population.
Methods
Study Design
In this retrospective time series analysis of all 50 US states and the District of Columbia, we used repeated cross-sectional data from 2003 to 2017 that were based on five data sources described below. Data were aggregated at the state level, as this represents the level at which insurance mandates went into effect. The research protocol was deemed exempt from review by the lead author’s institutional review board.
Measures
Exposures and Outcomes
Insurance Mandate
ASD-specific legislation at the state level in 2003–2017 was abstracted from the National Conference of State Legislatures’ autism and insurance coverage data set14 and the American Speech-Language-Hearing Association’s insurance data set.1 These data allowed for development of a binary exposure for insurance mandate, with states yet to implement scored as 0 through year of enactment; they are coded as 1 in the year after enactment. Following a coding scheme developed by Callaghan and Sylvester,16 we also introduced a generosity score for state mandates, ranging from 0 to 4 in 0.5-step increments. Briefly, states were awarded a higher score if they were less restrictive on benefit age limits and spending caps and were adjusted annually for inflation.16 For example, in states such as Alabama, the mandate does not apply to children older than age 12, leaving coverage to the discretion of the insurance plan. By contrast, in states such as Nevada, the mandate does not apply to children >17, and in states such as Massachusetts, it extends above age 17. The full specification is offered in Callaghan and Sylvester’s16 article.
Workforce
The Area Health Resource Files of the Department of Health and Human Services maintains an inventory of health professionals, including child psychiatrists and pediatricians. We did not include developmental pediatricians because this is a relatively novel specialty with small representation in the United States (N = 673 as of 2017). Data on BCBAs draw from the Behavior Analyst Certification Board,17 a nonprofit corporation from which BCBAs attain professional certification and register as actively practicing. Although other workforce groups were considered (eg, child psychologists, audiologists), data were either unavailable on an annual basis or data quality was inadequate to produce reliable estimates.
For each of the three workforce groups (BCBAs, child psychiatrists, and pediatricians), we calculated the state-level number of providers per 100 000 children. Counts of children and adolescents ages 0 to 19 at state level in 2003–2017 were obtained from the Census of Population and Housing, prepared by the US Census Bureau.18
Covariates
Income per Capita
We derived median income per capita from the Bureau of Economic Analysis within the US Department of Commerce.19 Personal income includes wages and salaries as well as sources of noncash income such as employer-provided insurance.
Race and Ethnicity
Race and ethnicity composition was also abstracted from the US Census Bureau. We specifically focused on two underserved populations: Black non-Hispanic and Hispanic.18 For each, we measured the percentage of the total state population represented by these categories.
Statistical Analysis
State Mandates and Workforce Supply
After inspecting measures of central tendency and dispersion,20 we made two adjustments to account for nonlinearities. First, we created variables for each year in the data set (2003–2017) to account for nonlinear growth trends in the number of providers over time. Second, we log transformed outcome measures (providers per 100 000 children) to normalize the right skew of this distribution at the state level.
After this, we estimated multivariable linear fixed-effects regression models consistent with a multiple interrupted time series analysis framework.21 Interrupted time series analysis allowed for examination of the localized change in workforce supply at the point of introducing a state insurance mandate, relative to the secular trajectory of workforce growth within a state. State fixed effects were included to address potential omitted variable bias, such as state-level policies that might influence workforce supply, by removing state-specific variance components.22 The exposure of interest (mandate) was included with a one-year lag to allow a sufficient time interval after law ratification for the mandate to have an effect on observed outcomes.7 We limited our analysis to this one-year interval to minimize the potential for other policies or factors to influence measured effects. We also included the time-varying covariates as described above. SEs were clustered at the state level.
To aid interpretation of results, we computed predicted counts using Stata’s (version 15.0; Stata Corp, College Station, TX) margins command.23 Predicted counts quantified the number of providers in a state on the basis of fitted models, calculated over the full distribution of all covariates values. All tests were two sided, used an α level of .05, and were conducted in Stata.
Sensitivity Analyses
To test potential premandate trends, we employed an event study design.24 The specification estimates the temporal effect of the mandate at varying points relative to their adoption.25 Specifically, we focus on the results from 6 years before enactment of the mandate through 6 years after enactment. Each of these models also included state and year fixed effects and the same covariates included in our primary analysis. The results after enactment explain how the effect of the mandate has varied over time, including in years subsequent to mandate introduction.26 In addition to examining the binary effect of introducing state mandates, we also examined a continuous measure for mandate generosity following a framework developed by Callaghan and Sylvester.16
Results
Descriptive Overview
Between 2003 and 2017, the number of BCBAs per 100 000 children in the United States increased from 1.34 to 29.88. Likewise, the number of child psychiatrists increased from 7.40 per 100 000 children to 10.03 per 100 00 children, and the number of pediatricians increased from 62.35 per 100 000 children to 68.86 per 100 000 children. Over this same period, 44 states introduced autism insurance mandates: an average of 3 states per year, which peaked in 2009 when 7 states introduced laws (CO, CT, MT, NV, NJ, NM, and WI). Details on the average number of BCBAs, child psychiatrists, and pediatricians providing care in states with versus without insurance mandates over this time period are shown in Table 1.
TABLE 1.
Health Providers per 100 000 Children by Year and Insurance Mandate Status
| Year | States With Mandates | States Without Mandates | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total States | Total Child Population | BCBAsa | Child Psychiatristsa | Pediatr-iciansa | Total States | Total Child Population | BCBAsa | Child Psychiatristsa | Pediatr-iciansa | |
| 2003 | 2 | 3 308 343 | 0.6 | 9.7 | 69.7 | 48 | 77 782 840 | 1.2 | 7.5 | 57.7 |
| 2004 | 2 | 3 325 590 | 1.0 | 10.0 | 69.6 | 48 | 78 101 528 | 1.9 | 7.5 | 58.1 |
| 2005 | 2 | 3 335 782 | 1.2 | 10.3 | 71.4 | 48 | 78 275 761 | 2.4 | 7.9 | 59.1 |
| 2006 | 3 | 4 865 016 | 2.6 | 8.6 | 69.8 | 47 | 77 075 244 | 2.8 | 8.0 | 58.9 |
| 2007 | 5 | 13 399 245 | 2.8 | 8.2 | 62.4 | 45 | 68 824 654 | 3.6 | 8.1 | 59.7 |
| 2008 | 11 | 29 450 360 | 6.8 | 8.5 | 66.4 | 39 | 53 052 618 | 3.8 | 8.1 | 58.3 |
| 2009 | 18 | 37 432 229 | 7.4 | 9.0 | 64.7 | 32 | 45 848 483 | 4.5 | 8.2 | 58.1 |
| 2010 | 24 | 41 725 605 | 9.1 | 9.1 | 64.7 | 26 | 41 414 495 | 4.4 | 7.4 | 55.2 |
| 2011 | 30 | 60 355 062 | 11.0 | 9.7 | 68.5 | 20 | 22 358 295 | 4.1 | 6.9 | 50.9 |
| 2012 | 35 | 67 346 300 | 12.4 | 9.8 | 68.3 | 15 | 15 022 570 | 4.9 | 7.2 | 49.0 |
| 2013 | 37 | 69 446 576 | 14.9 | 10.3 | 69.8 | 13 | 12 664 156 | 6.5 | 7.4 | 48.1 |
| 2014 | 40 | 71 624 210 | 18.7 | 10.1 | 68.8 | 10 | 10 370 446 | 8.4 | 7.4 | 48.7 |
| 2015 | 45 | 78 306 947 | 21.3 | 10.3 | 67.4 | 5 | 3 675 349 | 8.3 | 5.3 | 39.4 |
| 2016 | 46 | 79 322 582 | 25.0 | 10.5 | 67.2 | 4 | 2 636 922 | 12.1 | 5.9 | 38.9 |
| 2017 | 46 | 79 346 548 | 29.6 | 10.9 | 67.6 | 4 | 2 657 410 | 14.6 | 6.0 | 41.0 |
BCBAs, child psychiatrists, and pediatricians calculated as number per 100 000 children.
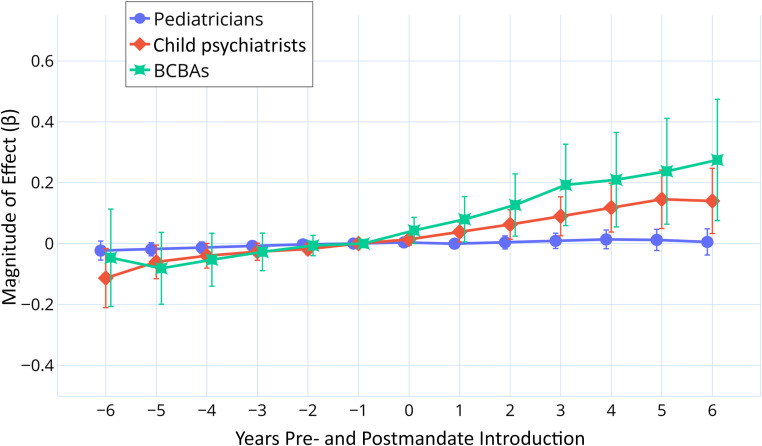
A descriptive comparison of change in BCBA levels each year for states that had passed a mandate versus those that had not passed a mandate is provided in Fig 1. Among states with insurance mandates, BCBAs increased by 0.35 BCBAs per 100 000 children from 2003 to 2004 compared to 4.63 BCBAs per 100 000 children from 2016 to 2017, approximately a 12-fold difference. Among states with no mandate, BCBAs increased by 0.62 BCBAs per 100 000 children from 2003 to 2004 compared to 2.51 BCBAs per 100 000 children from 2016 to 2017, approximately a threefold difference.
FIGURE 1.
Change in BCBAs per 100 000 children: states with versus without mandates. Annual increase in BCBAs represents the change in BCBAs per 100 000 children from one year to the next. “No Mandate” states represent those states, in a given year, that have yet to implement an insurance mandate for autism-related coverage or states in the year of implementation. “Mandate” states represent those states, in a given year, that have implemented an insurance mandate in the previous year or at an earlier time point. The year 2003 is absent from the figure because it represents the first reference year for year-to-year change (ie, change from 2003 to 2004).
Regression Analyses: Mandate Effect
Multivariable linear regression models indicated a significant relationship between mandate introduction and logged number of BCBAs per 100 000 children (β = .12; 95% confidence interval [CI]: 0.03 to 0.22; P = .01). The coefficient represents an expected increase of 0.25 BCBAs per 100 000 children in 2003 and 2.34 per 100 000 children in 2017 based on marginal estimates.
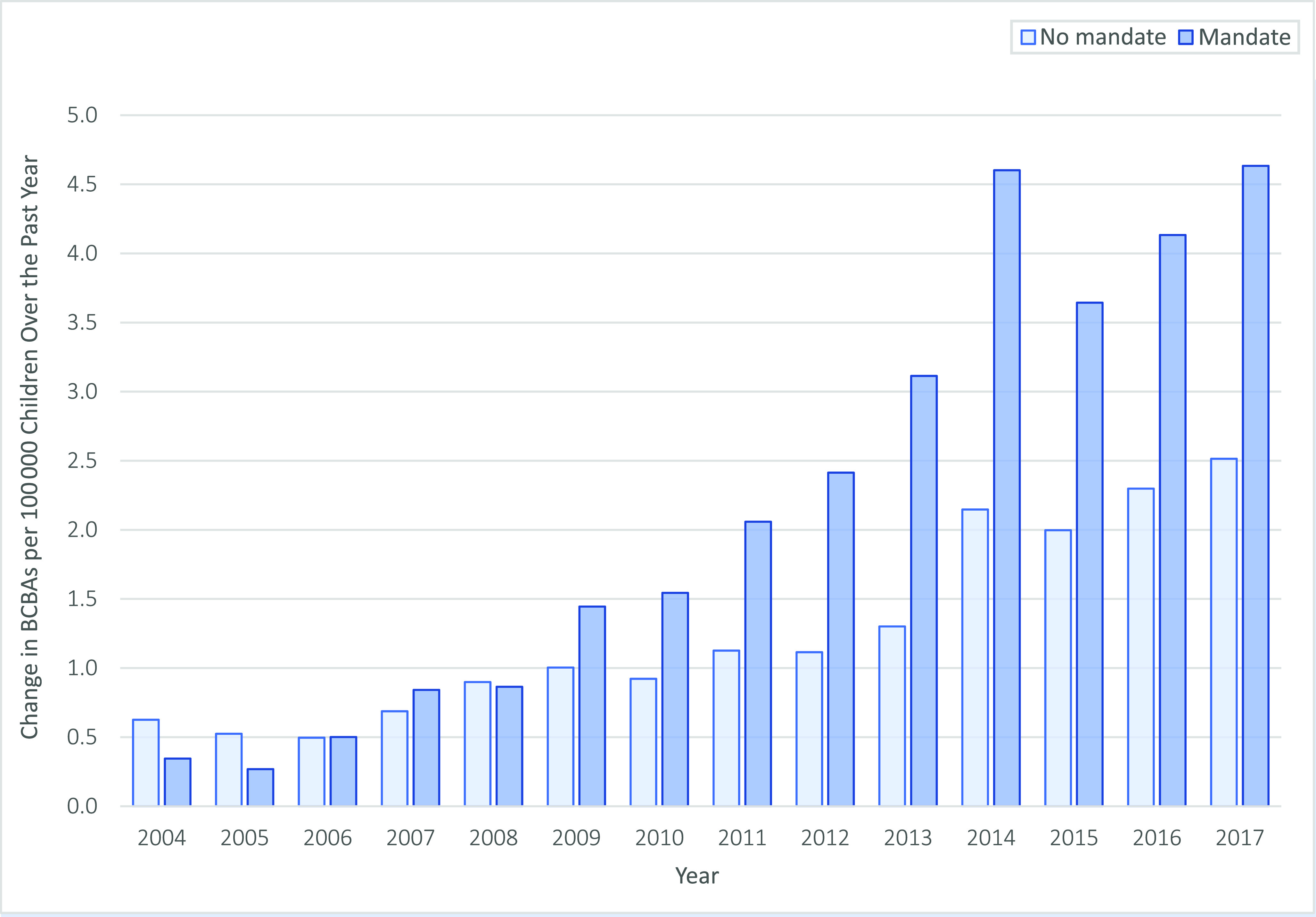
Models also indicated a modest relationship between state insurance mandate introduction and number of child psychiatrists per 100 000 children (β = .06; 95% CI: 0.01 to 0.10; P = .01), representing an additional increase of 0.45 child psychiatrists per 100 000 children in 2003 and 0.53 child psychiatrists per 100 000 children in 2017. The relationship between mandate introduction and pediatrician supply was nonsignificant (β = .003; 95% CI: −0.01 to 0.02; P = .72). Figure 2 reveals the expected number of providers in 2003 vs 2017, by profession type, for states with versus without insurance mandates based on predictive margins. In 2003, the expected difference in provider levels (via comparing states with versus without mandates) was 0.24 additional BCBAs and 0.45 additional child psychiatrists per 100 000 children. In 2017, this expected difference rose to 2.34 additional BCBAs per 100 000 children, whereas among child psychiatrists, this difference remained relatively static at 0.53 additional child psychiatrists per 100 000 children.
FIGURE 2.
A, Expected health providers (2003), by mandate status. B, Expected health providers (2017), by mandate status. Shown is the expected number of health providers per 100 000 child population based on predictive margins from multivariate regression models with the year set to 2003 vs 2017 and state insurance mandate status set to 0 (no mandate) or 1 (mandate). Models also included average income per capita, percent Black non-Hispanic, and percent Hispanic at the state level.
Sensitivity Analyses
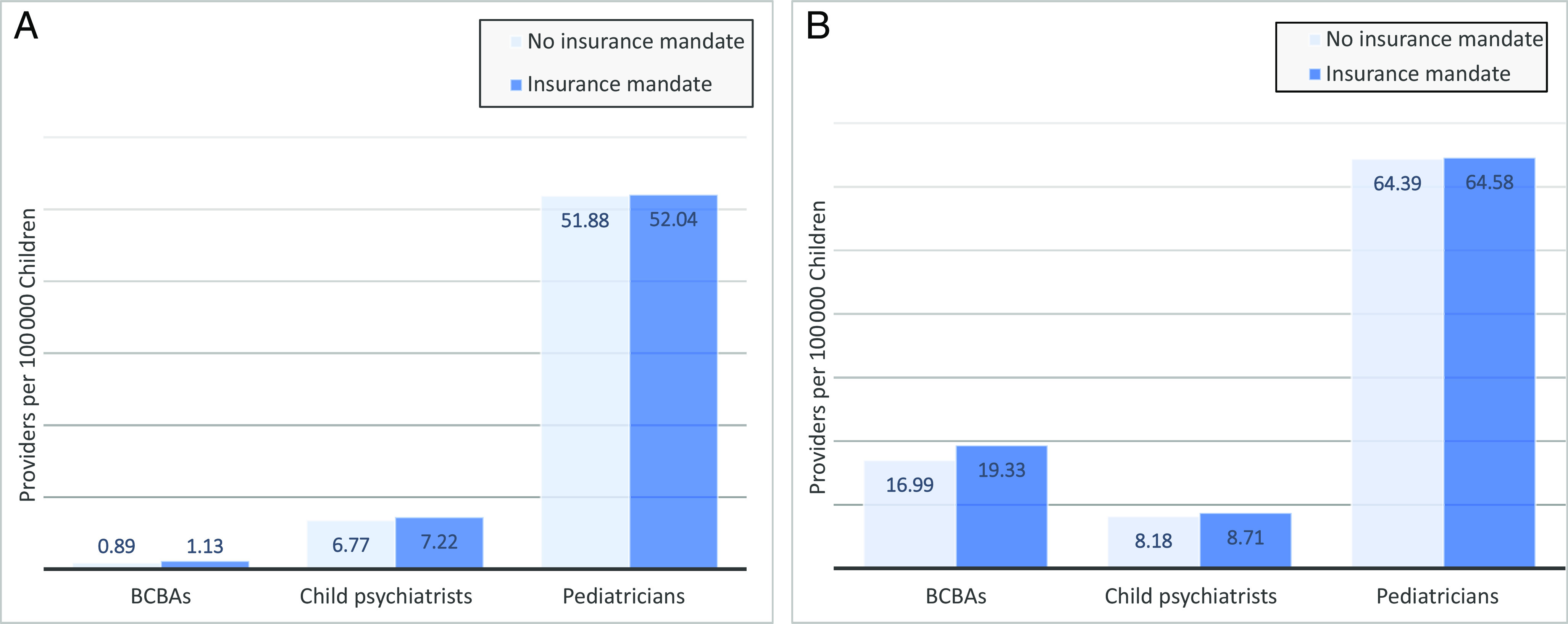
Results from the event study framework were substantively similar to primary results. We did not find evidence that the parallel trends assumption was violated, as connoted by all 95% CIs overlapping with the null value of 0 during the premandate period, with the one exception of child psychiatrists during the period of 6+ years before mandate implementation (Fig 3). This implies that previous trends in health care did not appear to influence the result of this study. Consistent with longitudinal regression results, one year after mandate introduction, there was a significant association with the supply of BCBAs (β = .080; 95% CI: 0.003 to 0.156; P = .04), more modest association with supply of child psychiatrists (β = .035; 95% CI: 0.002 to 0.067; P = .04), and no evidence of an association with pediatrician supply (P > .05). These effects expanded in magnitude in additional years subsequent to mandate introduction.
FIGURE 3.
Event study model: effect of state insurance mandate on health provider levels. The y-axis represents the natural log of health providers per 100 000 children, a measure of provider levels. On the x-axis, time to the left of 0 refers to periods before the adoption of state insurance mandates, and time to the right indicates periods after adoption. One year before adoption (−1) served as the reference year and is there presented as the midpoint between 2 years before adoption (−2) and the year of adoption (0). Vertical bars represent the 95% CIs, adjusted for state-level clustering. All values were estimated jointly by using multivariable regression, including state fixed effects, time fixed effects, and other covariates.
Multivariable linear regression models used to examine the role of mandate generosity (range: 0–4) on provider levels indicated a significant association between mandate generosity and increased number of BCBAs per 100 000 children (β = .05; 95% CI: 0.02 to 0.08; P = .002), with a similar but smaller relationship observed for child psychiatrists (β = .02, 95% CI: 0.003 to 0.04; P = .02): mandate generosity level was not significantly associated with change in the supply of pediatricians (95% CI: −0.0003 to 0.01; P = .06).
Discussion
We examined the relationship between the introduction of state insurance mandates and US workforce supply of providers who offer health care services to children with ASD: BCBAs, child psychiatrists, and pediatricians. We found evidence that the introduction of state mandates was associated with growth in the workforce supply of BCBAs: an ∼16% increase in the number of BCBAs per 100 000 children over the period. By contrast, the association between mandate introduction and the supply of child psychiatrists was much smaller, and there was no indication of a relationship with the supply of pediatricians.
In total, the associated marginal effect of insurance mandates translated to ∼1 additional BCBA for every 2000 children with ASD over the period. Although caseloads for BCBAs are much smaller than this number, it is a meaningful contribution. This relationship between state insurance mandates and supply of BCBAs can be viewed from two vantage points. First, given that a preponderance of state mandates included a coverage requirement for ABA,14 BCBAs stood to gain uniquely from law passage.27 This is further supported by our finding that more generous mandates were associated with even greater increases in BCBAs. Second, introduction of mandates occurred during a rapidly emerging market for ABA therapy28: we found a >20-fold increase in BCBAs from 2003 to 2017. BCBAs entering the workforce over this period could therefore choose to reside in environments that offered more favorable reimbursement conditions. By comparison, physician levels have remained stable over this period.29 Moreover, child psychiatrists and pediatricians have higher salaries and can selectively choose among insurance types or seek out-of-pocket payment.17,18
The finding that insurance mandates were associated with a modest increase in child psychiatrists is, on its face, more surprising. It may be the case that passage of insurance mandates is a general bellwether for environments that are more supportive of child mental health services.30–33 Alternatively, it is possible that child psychiatrists with a desire to practice in lower-resource settings felt more able to do so after mandate passage on the basis of improved reimbursement rates. In future work, researchers could answer this by studying whether types of accepted insurance among child psychiatrists expand as a function of insurance mandates or whether there is greater movement among child psychiatrists in counties that border state lines.
The broader takeaway in the context of child psychiatrists is that the magnitude of change in child psychiatrists, as a function of mandate introduction, was small: state insurance mandates do not appear to have markedly influenced a profession for which there is a significant shortage.11,15 It should be noted from the supplementary event study analyses, however, that the magnitude of change in child psychiatrists grew at 2- and 3-year postimplementation. We placed less emphasis on these findings because other (confounding) policies may have been introduced during broader time intervals.
Lastly, we found that the supply of pediatricians in the United States was not significantly associated with introduction of state insurance mandates. This finding was expected: pediatricians typically provide primary care for children rather than specialty care, and many pediatricians do not feel adequately trained to provide autism-related health care services.34–36 Moreover, similar to the findings regarding child psychiatrists, a high demand and stable salaries for pediatricians before insurance mandates are likely to have undercut the effect of introducing laws.37
Overall, the pattern of results we observe across provider types is consistent with our hypothesis that state insurance mandates are unlikely to substantially increase health care use and spending when there are significant workforce limitations that impede access. Theoretically, state insurance mandates should stimulate demand for health care services by reducing financial barriers; this, in turn, should lead to growth in the workforce.38 In practice, however, mandates may not be highly effective when care is generally unavailable or when the existing workforce supply is already overstretched. This comports with previous findings revealing that mandates have generated a relatively modest effect on health care use and spending. For instance, spending as a function of mandates has increased by ∼$77 per month, but the cost of care is closer to $1500 to $2500 per month.39 Families that are unable to find care have also paid the price in the form of depreciated parental employment and earnings.40 However, it is comparatively more promising that specific mandate provisions for ABA therapy, coupled with a growing job market for BCBAs, were associated with larger mandate effects on BCBAs. We should also note that results from our sensitivity analysis indicate that the magnitude of mandate effects, particularly on BCBAs, appears to have increased in years subsequent to mandate introduction.
The broader policy landscape is also likely to have exerted influence on the supply of autism-related services in conjunction with state insurance mandates over the period of our analysis. As noted in the introduction, state insurance mandates have contained important exemptions including for self-insured employer-sponsored health plans.2 Such exemptions are liable to have created a more muted policy impact, both in terms of who is eligible for benefits and workforce response. As a second example, the Patient Protection and Affordable Care Act (2010) introduced a set of 10 categories of essential health benefits that marketplace health insurance plans must cover, one of which includes mental health services.41 Although this provision has allowed states to receive federal support for broadened benefits offered by marketplace plans, states have flexibility in the way benefits are defined, which may have influenced workforce supply. Our approach to analysis addressed these external influences by examining the local effect of mandate introduction in the one-year period after ratification, relative to general growth trends in workforce supply that may have been shaped by other legislation such as the Patient Protection and Affordable Care Act. However, it is nevertheless possible that the introduction of such legislation shaped the content of state insurance mandates themselves.
Several limitations should be noted. First, our study is observational. Although the approach to analyses may be considered quasi-experimental, we have refrained from language suggestive of causality. Second, we did not have exact locations of practice for providers nor information on the level of engagement in practice by providers. It may be the case that unmet need is higher or lower as a function of provider engagement in practice. Third, our decision to examine mandate effects one year after implementation was to allow time for the mandates to have an effect on the labor market. Limiting to one year reduces the likelihood that confounding policies and programs could have played a role in shaping our results but also implies that the observed impacts of mandates are smaller and more conservative. In the event study models we ran, 2- and 3-year lagged effects were larger (and statistically significant) for BCBAs and child psychiatrists.
Conclusions
We find that the introduction of state insurance mandates was associated with a measurable increase in the supply of BCBAs in the United States, an ∼16% increase in a profession that is critical for providing services to children with ASD. The relationship between these mandates and the supply of child psychiatrists was much smaller, and no significant relationship was observed with the supply of pediatricians. Our findings are in concert with evidence that overall supply of child mental health services for children with ASD in the United States is inadequate to address existing needs32,42 and indicate the need for new policies that explicitly address child health care workforce shortages in many parts of the United States.
Glossary
- ABA
applied behavioral analysis
- ASD
autism spectrum disorder
- BCBA
board-certified behavioral analyst
- CI
confidence interval
Footnotes
Dr McBain conceptualized and designed the study, conducted the initial analyses, and drafted the initial manuscript; Dr Cantor assisted with analyses and drafting of the initial manuscript; Mr Kofner led data gathering and aggregation efforts and helped draft the initial manuscript; Dr Stein conceptualized the study and drafted the initial manuscript; Dr Yu obtained research funding, conceptualized and designed the study, and drafted the initial manuscript; and all authors reviewed and revised the manuscript, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the National Institute of Mental Health (R01 MH112760). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.American Speech Language Hearing Association. State insurance mandates for autism spectrum disorder. 2019. Available at: https://www.asha.org/Advocacy/state/States-Specific-Autism-Mandates/. Accessed November 13, 2019
- 2.Autism Speaks. Self-funded health benefit plans. 2018. Available at: https://www.autismspeaks.org/self-funded-health-benefit-plans. Accessed April 13, 2020
- 3.Baio J, Wiggins L, Christensen DL, et al. . Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2014 [published correction appears in MMWR Morb Mortal Wkly Rep. 2018;67(45):1279]. MMWR Surveill Summ. 2018;67(6):1–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muhle RA, Reed HE, Stratigos KA, Veenstra-VanderWeele J. The emerging clinical neuroscience of autism spectrum disorder: a review. JAMA Psychiatry. 2018;75(5):514–523 [DOI] [PubMed] [Google Scholar]
- 5.Behavioral Analyst Certification Board Applied behavior analysis treatment of autism spectrum disorder: practice guidelines for healthcare funders and managers. 2014. Available at: https://casproviders.org/asd-guidelines. Accessed November 13, 2019
- 6.Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–929 [DOI] [PubMed] [Google Scholar]
- 7.Barry CL, Epstein AJ, Marcus SC, et al. . Effects of state insurance mandates on health care use and spending for autism spectrum disorder. Health Aff (Millwood). 2017;36(10):1754–1761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saloner B, Barry CL. Changes in spending and service use after a state autism insurance mandate. Autism Int J Res Pract. 2019;23(1):167–174 [DOI] [PubMed] [Google Scholar]
- 9.Barry CL, Kennedy-Hendricks A, Mandell D, Epstein AJ, Candon M, Eisenberg M. State mandate laws for autism coverage and high-deductible health plans. Pediatrics. 2019;143(6):e20182391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Candon MK, Barry CL, Epstein AJ, et al. . The differential effects of insurance mandates on health care spending for children’s autism spectrum disorder. Med Care. 2018;56(3):228–232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McBain RK, Kofner A, Stein BD, Cantor JH, Vogt WB, Yu H. Growth and distribution of child psychiatrists in the United States: 2007–2016. Pediatrics. 2019;144(6):e20191576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cantor J, McBain RK, Kofner A, Stein BD, Yu H. Fewer than half US mental health treatment facilities provide services for children with autism spectrum disorder. Health Aff (Millwood). 2020;39(6):968–974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deochand N, Fuqua RW. BACB certification trends: state of the states (1999 to 2014). Behav Anal Pract. 2016;9(3):243–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Conference of State Legislatures. Autism and insurance coverage: state laws. 2019. Available at: www.ncsl.org/research/health/autism-and-insurance-coverage-state-laws.aspx. Accessed November 13, 2019
- 15.Bridgemohan C, Bauer NS, Nielsen BA, et al. . A workforce survey on developmental-behavioral pediatrics. Pediatrics. 2018;141(3):e20172164. [DOI] [PubMed] [Google Scholar]
- 16.Callaghan T, Sylvester S. Autism spectrum disorder, politics, and the generosity of insurance mandates in the United States. PLoS One. 2019;14(5):e0217064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Behavior Analyst Certification Board Behavior analyst certification board. 2019. Available at: https://www.bacb.com/services/o.php?page=100155. Accessed December 5, 2019
- 18.US Census Bureau. American Community Survey (ACS). 2017. Available at: https://www.census.gov/programs-surveys/acs. Accessed February 21, 2019
- 19.US Department of Commerce Commerce data hub. 2019. Available at: https://data.commerce.gov/. Accessed April 3, 2020
- 20.Judd CM, McClelland GH, Culhane SE. Data analysis: continuing issues in the everyday analysis of psychological data. Annu Rev Psychol. 1995;46:433–465 [DOI] [PubMed] [Google Scholar]
- 21.Meyer J. Poisson or negative binomial? Using count model diagnostics to select a model. 2018. Available at: https://www.theanalysisfactor.com/poisson-or-negative-binomial-using-count-model-diagnostics-to-select-a-model/. Accessed June 29, 2019
- 22.Wooldridge JM. Introductory Econometrics: A Modern Approach, 5th ed Boston, MA: Cengage Learning; 2012 [Google Scholar]
- 23.StataCorp. Stata Statistical Software: Release 15. Margins. College Station, TX: StataCorp LCC; 2014. Available at: https://www.stata.com/manuals13/rmargins.pdf. Accessed November 19, 2019
- 24.Abouk R, Pacula RL, Powell D. Association between state laws facilitating pharmacy distribution of naloxone and risk of fatal overdose. JAMA Intern Med. 2019;179(6):805–811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fry CE, Nikpay SS, Leslie E, Buntin MB. Evaluating community-based health improvement programs. Health Aff (Millwood). 2018;37(1):22–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kothari SP, Warner JB. Econometrics of Event Studies In: Eckbo BE, ed.. Handbook of Empirical Corporate Finance. Handbooks in Finance. Amsterdam, Netherlands: Elsevier; 2007:3–36 [Google Scholar]
- 27.Johnson RA, Danis M, Hafner-Eaton C. US state variation in autism insurance mandates: balancing access and fairness. Autism. 2014;18(7):803–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Behavioral Analyst Certification Board US employment demand for behavior analysts: 2010–2018. 2019. Available at: https://www.bacb.com/wp-content/uploads/2020/05/US-Employment-Demand-for-Behavior-Analysts_2019.pdf. Accessed August 11, 2020
- 29.US Bureau of Labor Statistics. Occupational Outlook Handbook: physicians and surgeons: job outlook. Available at: https://www.bls.gov/ooh/healthcare/physicians-and-surgeons.htm#tab-6. Accessed November 17, 2019
- 30.Cama S, Malowney M, Smith AJB, et al. . Availability of outpatient mental health care by pediatricians and child psychiatrists in five US cities. Int J Health Serv. 2017;47(4):621–635 [DOI] [PubMed] [Google Scholar]
- 31.Bishop TF, Press MJ, Keyhani S, Pincus HA. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176–181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Whitney DG, Peterson MD. US national and state-level prevalence of mental health disorders and disparities of mental health care use in children. JAMA Pediatr. 2019;173(4):389–391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cummings JR, Allen L, Clennon J, Ji X, Druss BG. Geographic access to specialty mental health care across high- and low-income US communities. JAMA Psychiatry. 2017;74(5):476–484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McBain RK, Kareddy V, Cantor JH, Stein BD, Yu H. Systematic review: United States workforce for autism-related child healthcare services. J Am Acad Child Adolesc Psychiatry. 2020;59(1):113–139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carbone PS, Behl DD, Azor V, Murphy NA. The medical home for children with autism spectrum disorders: parent and pediatrician perspectives. J Autism Dev Disord. 2010;40(3):317–324 [DOI] [PubMed] [Google Scholar]
- 36.Nolan R, Walker T, Hanson JL, Friedman S. Developmental behavioral pediatrician support of the medical home for children with autism spectrum disorders. J Dev Behav Pediatr. 2016;37(9):687–693 [DOI] [PubMed] [Google Scholar]
- 37.Basco WT, Rimsza ME; Committee on Pediatric Workforce; American Academy of Pediatrics . Pediatrician workforce policy statement. Pediatrics. 2013;132(2):390–397 [DOI] [PubMed] [Google Scholar]
- 38.Madrian B. The U.S. Health Care System and Labor Markets. Cambridge, MA: : National Bureau of Economic Research; 2006 [Google Scholar]
- 39.Buescher AVS, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 2014;168(8):721–728 [DOI] [PubMed] [Google Scholar]
- 40.Cidav Z, Marcus SC, Mandell DS. Implications of childhood autism for parental employment and earnings. Pediatrics. 2012;129(4):617–623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.National Conference of State Legislatures. State insurance mandates and the ACA essential benefits provisions. 2018. Available at: https://www.ncsl.org/research/health/state-ins-mandates-and-aca-essential-benefits.aspx#Understanding. Accessed April 13, 2020
- 42.Ghandour RM, Sherman LJ, Vladutiu CJ, et al. . Prevalence and treatment of depression, anxiety, and conduct problems in US children. J Pediatr. 2019;206:256.e3-267.e3 [DOI] [PMC free article] [PubMed] [Google Scholar]