Abstract
The 2020 SARS-CoV-2 pandemic is caused by a zoonotic coronavirus transmitted to humans, similar to earlier events. Whether the other, seasonally circulating coronaviruses induce cross-reactive, potentially even cross-neutralizing, antibodies to the new species in humans is unclear. The question is particularly relevant for people with immune deficiencies, as their health depends on treatment with immunoglobulin preparations that need to contain neutralizing antibodies against the pathogens in their environment. Testing 54 intravenous immunoglobulin preparations, produced from plasma collected in Europe and the United States, confirmed highly potent neutralization of a seasonal coronavirus; however, no cross-neutralization of the new SARS-CoV-2 was seen.
Keywords: primary immunodeficiency, SARS-CoV-2, SARS coronavirus 2 antibody titer, neutralizing antibodies, COVID-19, intravenous immunoglobulin, plasma
Intravenous immunoglobulins (IVIG) are produced from thousands of pooled plasma donations, and thus contain a wide variety of antibodies the donors have generated against infectious disease agents. IVIG can therefore protect people with immune deficiencies against circulating bacterial and viral infections.
When a new pathogen emerges, antibodies to the new agent only become detectable in IVIG preparations after a certain proportion of plasma donors have contracted the infection and successfully recovered from it. An even higher number of convalescent plasma donors is needed to result in neutralizing antibody (nAb) levels high enough for the resulting IVIG to afford protection against the new infectious agent. After the arrival of West Nile virus (WNV) in the United States, for example, it took several years before the prevalence of WNV nAbs reached approximately 0.5% in the plasma donor community, at which point they became detectable in IVIG lots produced from plasma donated in the United States. Thereafter, a significant proportion of IVIG lots even reached in vivo protective levels [1].
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) spread around the globe at unprecedented speed, infecting millions of people within the first 6 months of circulation. The virus belongs to the Coronaviridae family of viruses, which contains several species of importance for human health. The human coronaviruses (HCoVs) 229E, NL63, OC43, and HKU1 are in circulation as seasonal respiratory viruses that mostly cause self-limiting and mild infections but which can also lead to pneumonia and bronchiolitis [2–4], whereas the Middle East respiratory syndrome coronavirus (MERS-CoV) caused a prolonged outbreak mainly limited to the Arabian Peninsula, and the SARS-CoV and SARS-CoV-2 viruses have established global transmissions chains—the latter 3 associated with significant human mortality.
Due to the widespread and long-term circulation of HCoVs, and the pooling of plasma from thousands of donors for every lot, IVIGs contain significant levels of HCoV nAb levels, as was shown for example for HCoV-NL63 [5]. Whether these HCoV antibodies cross-react with, or even neutralize, the related SARS-CoV-2 has not been fully elucidated. To date, antibody binding assays have shown some cross-reactivity between different HCoVs and SARS-CoV-2; however, functional and therefore clinically more relevant virus neutralization assays have shown no or only very low levels of cross-reactive antibodies [6–8]. The question is of significant clinical relevance, as SARS-CoV-2 cross-neutralizing antibodies in IVIGs, if they were present, might afford some protection to people with immune deficiencies and may even represent a treatment option for coronavirus disease 2019 (COVID-19) patients.
The current study tested a representative number of IVIG lots for nAbs against SARS-CoV-2 and the longer-circulating HCoV-229E, to establish clarity about cross-neutralization of the pandemic virus by antibodies induced by earlier circulating seasonal coronaviruses. In addition, results from the ongoing monitoring of the plasma donor community for the development of SARS-COV-2 antibodies are presented.
METHODS
IVIG Preparations
A total of 54 IVIG lots fractionated from plasma collected prior to the circulation of SARS-CoV-2 were analyzed. The IVIG lots were manufactured from plasma either donated by plasmapheresis (source) or recovered from whole-blood donations (recovered), in the United States (Gammagard Liquid; Baxter Healthcare Corp.; n = 30) or central Europe, that is Austria, Germany, and Czech Republic (KIOVIG; Baxter AG; n = 24). These 54 IVIG lots were tested in 2 independent experiments for nAbs (1 European lot was in a single assay due to volume constraints).
Human Plasma Samples
Two prepandemic plasma donations were collected in April and May 2019 by BioLife Austria.
Human plasma pool samples were generated by the combination of 6 individual donations obtained in the same week at Austrian plasma donation centers (BioLife). The pools were assembled from donations collected in week 13 (last week of March; n = 40), week 14 (n = 80), week 15 (n = 80), week 16 (n = 80), week 20 (n = 100), week 24 (n = 80), and week 28 (first week of July; n = 100) of 2020, that is during the SARS-CoV-2 pandemic. Cumulative incidence of COVID-19 was calculated from data provided by the Austrian Federal Ministry for Social Affairs, Health, Care and Consumer Protection (www.sozialministerium.at) and Statistics Austria (www.statistik.at).
Detection of SARS-CoV-2 Neutralizing Antibodies
SARS-CoV-2 nAb titers were determined in IVIG and human plasma samples that were used undiluted, or prediluted with cell culture medium 1:4, 1:5, 1:10, or 1:20 depending on sample amount available, and then serially diluted in 2-fold steps. Equal volumes of sample dilutions were mixed with virus stock at 103.0 tissue culture infectious doses 50% per milliliter (TCID50/mL) SARS-CoV-2 (strain BavPat1/2020, kindly provided by C. Drosten and V. Corman, Charité Berlin, Germany) and incubated for 150 minutes ± 15 minutes, before titration on Vero cells (Cat. no. 84113001, European Collection of Authenticated Cell Cultures, Porton Down, Salisbury, UK) in 8-fold replicates per dilution. The virus-induced cytopathic effect was determined after 5–7 days of incubation. The reciprocal sample dilution resulting in 50% virus neutralization (NT50) was determined using the Spearman-Kärber formula, and the calculated neutralization titer for 50% of the wells reported as 1:X. The detection limits were as follows: <1:0.8 for undiluted, <1:3.1 for 1:4 prediluted, <1:3.9 for 1:5 prediluted, <1:7.7 for 1:10 prediluted, and <1:15.4 for 1:20 prediluted IVIG.
The neutralization assay (µNT) included several validity criteria, that is confirmatory titration of input virus infectivity, cell viability, and neutralization testing of an internal reference standard, all of which had to comply with defined ranges.
Detection of HCoV-229E Neutralizing Antibodies
The neutralization assay for HCoV-229E antibodies is essentially identical to the SARS-CoV-2, where samples were used undiluted or prediluted, then serially diluted in 2-fold steps and mixed 1:2 with 103.0 TCID50/mL HCoV-229E (Cat. no. VR-740, American Type Culture Collection [ATCC], Rockville, MD), incubated, and titrated on MRC-5 cells (Cat. no. CCL-171, ATCC, Rockville, MD). The virus-induced cytopathic effect was determined after 7–9 days of incubation.
Graphs and Statistical Analysis
Graphical illustration and statistical analysis (paired t tests) were done using GraphPad Prism v8.1.1 software.
RESULTS
The validity, specificity, and reliability of the SARS-CoV-2 neutralization assay used in the current study were demonstrated by the analysis of 100 convalescent plasma donations from polymerase chain reaction (PCR)-confirmed SARS-CoV-2 cases [9] and was the basis for the correlation of function against diverse binding assays [10]. As controls, 2 plasma samples collected before the emergence of SARS-CoV-2 did not contain SARS-CoV-2 nAbs, as expected, but neutralized HCoV-229E with NT50 values of 1:43 and 1:26, respectively.
Testing of IVIG
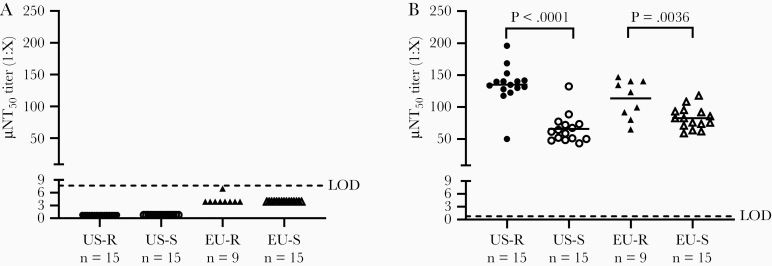
SARS-CoV-2 nAb titers were below the limit of detection for all 54 IVIG lots tested, irrespective of geographic origin of the plasma (Europe vs United States) and plasma collection modality (recovered vs source) (Figure 1A).
Figure 1.
Coronavirus neutralizing antibody titers in IVIG lots (n = 54) against (A) SARS-CoV-2 and (B) HCoV-229E. The IVIG lots were manufactured from plasma either donated by plasmapheresis (S), or recovered from whole blood donations (R), in the United States or central Europe. Each dot represents the mean of 2 independent experiments, except in (B) from 1 EU-R IVIG lot the titer of a single determination is shown. The lines represent the median in each group. Paired t tests were used for determination of significance. Abbreviation: EU, Europe; HCoV, human coronavirus; IVIG, intravenous immunoglobulin; LOD, limit of detection; µNT50, 50% neutralization titer; R, recovered; S, source; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
In contrast, HCoV-229E nAb titers between 1:43 and 1:196 (mean = 1:98) were measured for the 54 IVIG lots tested (Figure 1B). IVIG lots produced from recovered plasma contained significantly higher levels of nAb to HCoV-229E as compared to IVIG lots produced from source plasma, independent of the geographic origin. A significant, although quantitatively minor, difference was also found between IVIG lots manufactured from source plasma collected in either the United States or Europe.
Testing of Human Plasma
To evaluate the potential development of SARS-CoV-2 antibodies in the plasma donor community, samples of plasma pools of 6 donations each were tested. The use of pools enabled testing of a high amount of plasma donations for SARS-CoV-2 nAbs with the biosafety level-3 functional assay. As the mean SARS-CoV-2 µNT50 of plasma donations is rather high (approximately 1:230 [9]) even the nAbs of only 1 positive sample within a pool are detectable in this assay.
Testing a total of 560 plasma pools of 6 donations each, in total reflective of 3360 plasma donations, from week 13 (ie, last week of March) until week 28 (ie, first week of July) 2020 revealed that most of these pools had SARS-CoV-2 µNT titers below the limit of detection (Table 1). The first pool with detectable nAbs to SARS-CoV-2 was collected in week 14. Further positive pools were found in weeks 15, 16, 24, and 28. Up to 7% of the tested pools showed nAbs to SARS-CoV-2, which indicates that up to 1.17% of the plasma donors were positive for SARS-CoV-2 nAbs at a cumulative incidence of COVID-19 in Austria of 0.21% (Table 1).
Table 1.
SARS-CoV-2 Neutralizing Antibodies in Tested Plasma Pools
| Week in 2020 | |||||||
|---|---|---|---|---|---|---|---|
| Parameter | 13 | 14 | 15 | 16 | 20 | 24 | 28 |
| Plasma pools ≥LOD, % | 0.0 | 1.3 | 1.3 | 6.3 | 0.0 | 5.0 | 7.0 |
| µNT50 of plasma pool titers ≥LOD, 1:X | n.a. | 37 | 5 | 6, 18, 26, 34, 87 | n.a. | 7, 10, 20, 22 | 4, 7, 8, 9, 12, 18, 24 |
| Number of plasma pools tested | 40 | 80 | 80 | 80 | 100 | 80 | 100 |
| SARS-CoV-2 nAb positive plasma donors in Austria, % | 0.00 | 0.21 | 0.21 | 1.04 | 0.00 | 0.83 | 1.17 |
| Cumulative COVID-19 incidence in Austria, %a | 0.10 | 0.14 | 0.16 | 0.17 | 0.18 | 0.19 | 0.21 |
Abbreviations: µNT50, neutralization titer for 50% of the wells; COVID-19, coronavirus disease 2019; LOD, limit of detection; n.a., not applicable; nAb, neutralizing antibody; PCR, polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
aSARS-CoV-2 PCR-positive individuals per 100 000 population in Austria are described as cumulative COVID-19 incidence in percent.
DISCUSSION
Our analysis of IVIG lots revealed high nAb titers to HCoV-229E (Figure 1B), which confirmed the presence of functionally intact nAbs in these lots. It is interesting to note that in IVIG lots produced from recovered plasma significantly higher titers to HCoV-229E were found compared to IVIG lots produced from source plasma, independent of plasma origin. Recovered plasma is usually obtained from older donors [11]. A trend towards increasing probability of HCoV-229E infections with age has been detected in the Scottish [3] and US [4] population. Furthermore, higher HCoV-229E–specific nAb titers were found in older study participants (60–85 years) compared to younger ones (21–40 years) [12]. Thus, a higher infection rate with HCoV-229E in older people and consequently the generation of neutralizing HCoV-229E–specific antibodies in the older plasma donors would explain the higher HCoV-229E titers found in IVIG lots produced from recovered plasma.
Low levels of cross-neutralizing Abs have earlier been demonstrated between specific pairs of coronaviruses, specifically between SARS-CoV-2 sera and SARS-CoV [6] and SARS-CoV sera and MERS [13].
In clear contrast, testing the same lots of IVIG that were shown to contain high HCoV-229E nAb titers with a highly specific SARS-CoV-2 µNT did not detect SARS-CoV-2–specific nAbs. These results are entirely consistent with the absence of SARS-CoV-2 antibodies in the plasma used for production of these IVIG lots, as this plasma was donated well before the start of the SARS-CoV-2 pandemic.
The current study, as well as an earlier study that tested 21 IVIG lots (9 Gamunex C, 10 Gammagard Liquid, 2 other) with a SARS-CoV-2-specific enzyme-linked immunosorbent assay (ELISA; receptor-binding domain or spike protein) that was shown to correlate well with a neutralization test [14] revealed the absence of cross-reactive antibodies against SARS-CoV-2 in IVIG lots produced from prepandemic plasma. Currently available IVIGs can therefore not be expected to afford protection from SARS-CoV-2 infection. Nevertheless, several clinical trials currently investigate IVIG at high dosage in the treatment of COVID-19 patients (clinicaltrials.gov), with the expected benefit attributable to the anti-inflammatory and immunomodulatory capacity of IVIG, rather than an antiviral effect.
With increasing numbers of human infections, including in the plasma donor community, it is interesting to follow the development of antibodies against SARS-CoV-2 in plasma donations and, after the several months production cycle time between plasma donation and IVIG lot release, also in IVIG lots. A longitudinal study on this topic is currently in progress. In this context it is noteworthy that the mean nAb titers induced by WNV [1] and SARS-CoV-2 [9] infection are of similar magnitude. After the emergence of WNV in the United States, nAb titers became detectable in IVIGs after approximately 0.5% of the population had contracted and recovered from the infection. In Austria, testing of plasma pool samples indicated that up to 1.17% of plasma donors were positive for SARS-CoV-2 nAbs. Based on the current number of reported SARS-CoV-2 infections in the United States (approximately 4.3 million per 30 July 2020; www.cdc.gov), and an estimated rate of >40% asymptomatic infections [15], more than 7.2 million people in the United States could have been infected already, that is 2.2% of the approximately 330 million population. Based on these facts, the detection of SARS-CoV-2 nAbs in IVIG lots produced from US plasma, the major source for fractionation, is expected within the next few months.
Another, more immediately available possibility for the treatment of COVID-19 is production of a hyper-IVIG from the plasma of COVID-19 convalescent donors (CoVIg-19), and developmental work is currently under way through a large alliance of plasma stakeholders (https://www.covig-19plasmaalliance.org).
Notes
Acknowledgments. The contributions of the entire Global Pathogen Safety team, most notably Simone Knotzer, Melanie Graf, Jasmin de Silva, Julius Segui (neutralization assays), Veronika Sulzer, Sabrina Brandtner (cell culture), as well as Eva Ha and Alexandra Schlapschy-Danzinger (virus culture) are gratefully acknowledged. The team of Plasma Analytics, Takeda, Vienna prepared the human plasma pool samples. SARS-CoV-2 was sourced via EVAg (supported by the European Community) and kindly provided by Christian Drosten and Victor Corman (Charité Universitätsmedizin, Institute of Virology, Berlin, Germany).
Financial support. This work was supported by Baxter AG, now part of the Takeda group of companies, Vienna, Austria.
Potential conflicts of interest. Authors are employees of Baxter AG, now part of the Takeda group of companies, Vienna, Austria. M. K., C. A., M. R. F., and T. R. K. have Takeda stock interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Planitzer CB, Modrof J, Yu MY, Kreil TR. West Nile virus infection in plasma of blood and plasma donors, United States. Emerg Infect Dis 2009; 15:1668–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Greenberg SB. Update on human rhinovirus and coronavirus infections. Semin Respir Crit Care Med 2016; 37:555–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nickbakhsh S, Ho A, Marques DFP, McMenamin J, Gunson RN, Murcia PR. Epidemiology of seasonal coronaviruses: establishing the context for the emergence of coronavirus disease 2019. J Infect Dis 2020; 222:17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Killerby ME, Biggs HM, Haynes A, et al. Human coronavirus circulation in the United States 2014–2017. J Clin Virol 2018; 101:52–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pyrc K, Bosch BJ, Berkhout B, et al. Inhibition of human coronavirus NL63 infection at early stages of the replication cycle. Antimicrob Agents Chemother 2006; 50:2000–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Anderson DE, Tan CW, Chia WN, et al. Lack of cross-neutralization by SARS patient sera towards SARS-CoV-2. Emerg Microbes Infect 2020; 9:900–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Huang AT, Garcia-Carreras B, Hitchings MDT, et al. A systematic review of antibody mediated immunity to coronaviruses: antibody kinetics, correlates of protection, and association of antibody responses with severity of disease. medRxiv 20065771 [Preprint]. 14. March 2020. [cited 30 July 2020]. Available from: 10.1101/2020.04.14.20065771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Okba NMA, Müller MA, Li W, et al. Severe acute respiratory syndrome coronavirus 2-specific antibody responses in coronavirus disease patients. Emerg Infect Dis 2020; 26:1478–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jungbauer C, Weseslindtner L, Weidner L, et al. Characterization of 100 sequential SARS-CoV-2 convalescent plasma donations. Transfusion 2020; doi: 10.1111/trf.16119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Weidner L, Gänsdorfer S, Unterweger S, et al. Quantification of SARS-CoV-2 antibodies with eight commercially available immunoassays. J Clin Virol 2020; 129:104540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Farcet MR, Karbiener M, Rabel PO, Schirmer A, Ilk R, Kreil TR. Measles virus neutralizing antibodies in immunoglobulin lots produced from plasma collected in Europe or the United States. Vaccine 2019; 37:3151–3. [DOI] [PubMed] [Google Scholar]
- 12. Gorse GJ, Donovan MM, Patel GB. Antibodies to coronaviruses are higher in older compared with younger adults and binding antibodies are more sensitive than neutralizing antibodies in identifying coronavirus-associated illnesses. J Med Virol 2020; 92:512–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chan KH, Chan JF, Tse H, et al. Cross-reactive antibodies in convalescent SARS patients’ sera against the emerging novel human coronavirus EMC (2012) by both immunofluorescent and neutralizing antibody tests. J Infect 2013; 67:130–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Amanat F, Stadlbauer D, Strohmeier S, et al. A serological assay to detect SARS-CoV-2 seroconversion in humans. Nat Med 2020; 26:1033–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Oran DP, Topol EJ. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med 2020; 173:362–7. [DOI] [PMC free article] [PubMed] [Google Scholar]