Abstract
Efficient strategies for testing large numbers of patients must be developed to limit the spread of coronavirus disease 2019 (COVID-19). We demonstrate that our drive-through model is an efficient method of testing large numbers of patients during a pandemic. In the drive-through, cost per patient and personal protective equipment use were significantly less than in 3 brick-and-mortar clinics providing testing. We provide an example of effective nurse practitioner leadership in a drive-through testing site and demonstrate that nurse practitioners are ideally suited to provide leadership given their adaptability, ability to function in a variety of settings, and extensive experience with care coordination and logistics.
Keywords: COVID-19, drive-through, efficiency, nurse practitioner, testing
Background
Initially classified as unexplainable cases of pneumonia appearing in December 2019 in Wuhan, China, coronavirus disease 2019 (COVID-19), also known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), quickly spread throughout China and the globe.1 On January 30, 2020, the World Health Organization (WHO) announced a public health emergency of international concern, which was shortly followed by the declaration of a global pandemic on March 11, 2020.1 Currently, there are more than 6.5 million total reported cases of COVID-19 and more than 190,000 deaths in the United States.2
Efficient processes for rapidly testing large numbers of individuals for COVID-19 must be developed that reduce the risk for transmission between patients and health care personnel. One approach is drive-through testing, which maintains social distancing and reduces exposure.3, 4, 5 Drive-through testing allows for rapid testing of large numbers of patients while using fewer resources, such as personal protective equipment (PPE) and staff, than a traditional clinic setting.3, 4, 5 These testing efforts require strong clinical leadership by members of the health care profession who are willing to adapt successfully in a constantly changing pandemic landscape. We demonstrate that nurse practitioners (NPs) are an ideal choice for clinical leadership in a drive-through COVID-19 testing site.
In South Korea, drive-through testing for COVID-19 was proven to be a safe and efficient intervention.4 Major benefits included reduced waiting and screening times, largely because there was no need to clean the specimen collection room between patients. Additionally, the drive-through method reduced PPE use and required fewer staff, yielding significant cost savings. Limitations did include the potential for contamination of PPE between patients, challenges of inclement weather, need for personal transportation, potential waste of resources with repeated testing, and the lack of resources available for medically unstable patients.4
During the 2009 influenza pandemic, a mock drive-through clinic at Stanford University demonstrated that the model could be a successful alternative to traditional care by mitigating the spread of disease and reducing the burden placed on emergency departments.5 The median length of stay was 26 minutes and was not affected by increased patient volume. It was again noted that negating the need for examination room cleaning between patients increased throughput significantly. Finally, a pediatric-focused drive through COVID-19 testing site deployed in Philadelphia in March 2020 further supports the argument for efficiency as they were able to perform almost 10% of all tests performed city-wide at that time.3 These studies all support the argument that a drive-through testing model can reduce cost, increase throughput, and maintain social distancing.
Rationale
In preparation for a predicted surge of patients with COVID-19, the University of California, San Francisco (UCSF) health system created Respiratory Screening Clinics (RSC) to redirect patients away from the emergency department (ED). There was a large group of low-acuity patients who did not require further evaluation by a provider, yet still needed a quick and safe way to get tested. This included front-line employees with mild symptoms or those who had a known exposure and required immediate testing. Testing volume quickly overwhelmed the RSC testing capacity and created a backlog, which prevented these employees from returning to work in a timely manner.
Specific Aims
A drive-through testing site was developed with the aim of efficiently screening a large volume of high-risk/low-acuity employees for COVID-19. NPs who had seen a decrease in work demands were chosen to provide clinical leadership to maintain patient safety in this unique remote environment. The drive-through model was expected to reduce testing waiting time and decrease the risk of viral transmission. Cleaning between patient encounters, which can be time consuming and costly, is not needed. Capacity for testing is increased, and risk of staff exposure is reduced given that the tester does not have to enter the vehicle. There are no parking logistics, and check-in and testing occurs almost simultaneously, reducing visit time. Additionally, it was expected that supply, namely PPE, and labor needs would be less than in a typical clinic setting, resulting in significant cost reduction.
Methods
Context
Multiple logistical and environmental factors required consideration during the initial construction of the drive-through testing site. An open parking lot attached to a health system office building was chosen as the drive-through site due to limited traffic in the area. An affiliated medical group simultaneously set up a drive-through testing site at this location, which simplified logistics and allowed for splitting of some set-up costs. Before construction of the testing site, a special event permit was obtained from the city fire marshal as well as permission from the property landlord. The surrounding community was notified of the plan for a drive-through testing site to maintain community relationships and generate buy-in.
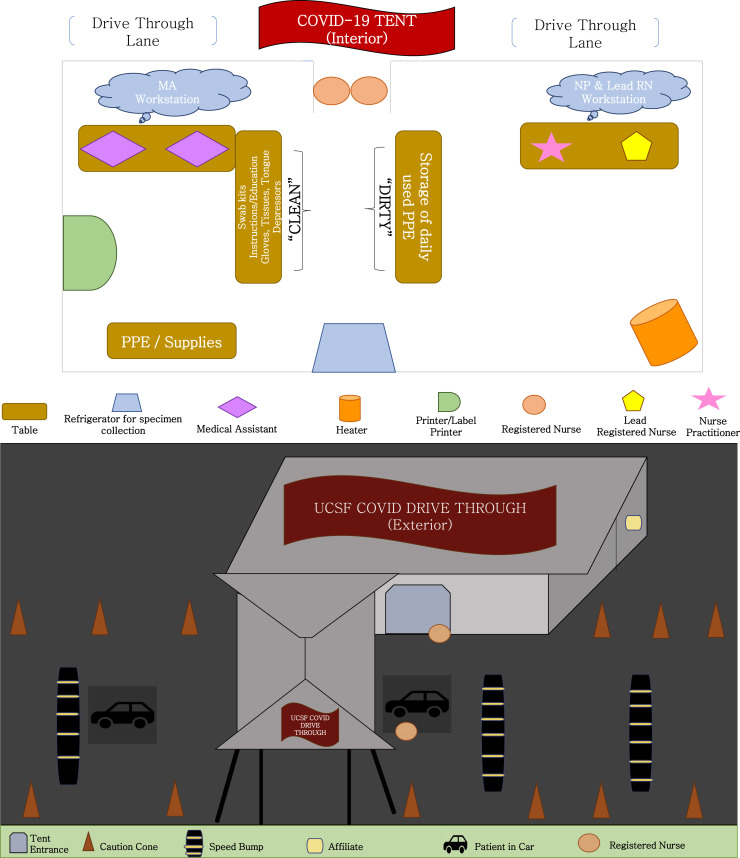
A plan for the interior and exterior layout of the tent was developed (Figure 1 ). There was only 1 entrance and exit to the parking lot to simplify traffic control. The interior of the tent was divided into “dirty” and “clean” sides, with the medical assistants (MAs) and spare supplies on the clean side of the tent. The dirty side of the tent included a table with individually marked bins for registered nurses (RNs) to store their masks and face shields when on breaks. The RNs performing the testing wore an N95 mask, face shield, coverall/gown, and gloves. They did not pass the entrance of the tent when testing patients to not contaminate the clean area. The remainder of the staff worse surgical masks always and gloves when handling specimens in accordance with infection control recommendations.
Figure 1.
Interior and exterior layout of the drive-through COVID-19 testing site (MA = medical assistant; NP = nurse practitioner; PPE = personal protective equipment; RN = registered nurse).
The need for shelter, heat, electricity, internet access, trash removal, and storage space was anticipated and required a multidisciplinary effort to coordinate. Shelter, heat, and electricity were contracted out to local event companies. Essential equipment was stored in a building approximately 100 feet from the drive-through site. This building also provided an indoor break space and restrooms for drive-through site staff. Environmental services came to the site grounds daily to discard waste and clean the restrooms. A supply chain was created to ensure equipment, such as PPE, hand sanitizers, antibacterial wipes, swab kits, and general office supplies were stocked appropriately (Table 1 ). Testing kits were sourced from pre-existing stock and did not add any costs to the drive-through site.
Table 1.
List of Essential Supplies Required for the Drive-Through COVID-19 Testing Site
| General Supplies | Documentation | Patient Care | Traffic/Safety Control | PPE/Cleaning | Provided Staff Needs |
|---|---|---|---|---|---|
| Tables with covers | Laptops with access to Epic softwarea | Tissues | Traffic cones | Hand sanitizer | Water bottles |
| Chairs | Discharge instructions/education | NP/OP swab kits | Speed bumps | N95 respirator masks | Bathroom access |
| Trash Bins | Contact information for “walk-ups” | Surgical mask for usage postdischarge | Signage for entry/exit | Eye shields/protective eyewear | Snacks |
| Extension cords and outlets | Laboratory slips with patient identification | Tongue depressors | UCSF medical signage and banner | Disposable isolation gowns | Jackets |
| Telephones | Printer for printouts of daily patient schedule, discharge instructions, etc | Disposable pulse oximeters | Fire extinguishers | Disposable isolation coveralls | Breakfast provided from UCSF Nutritional Services Dept |
| Tent/canopy | Education sheets for RN staff on how to don/doff isolation and PPE wear | Thermometer | Hydrogen peroxide wipes | Room for breaks and lunch | |
| Heating lamp | Education sheets on efficient NP/OP swab | Thermometer probe covers | Biohazard bags | ||
| Heater | Binder of contact phone numbers/information for emergencies, questions, concerns, etc | Refrigerator storage for NP/OP sample collections | Gloves | ||
| Shelving | Personal health information shred-it container | Video mobile interpreter device | Surgical masks | ||
| Storage bins | Label printer for the specimen | ||||
| Refrigerator | |||||
| Lighting |
NP = nasopharyngeal; OP = oropharyngeal; PPE = personal protective equipments; RN = registered nurse; UCSF = University of California, San Francisco.
Epic, Verona, Wisconsin.
Staffing of the drive-through testing site required a multidisciplinary approach playing to the strengths of each professional’s role. The NP supervised RN staff to ensure proper testing technique and monitored for adherence to PPE guidelines disseminated by the health system. The NPs were also responsible for assessing patients who presented to the drive-through more ill than expected. Although on-site monitoring equipment was limited, if a patient’s vital signs were abnormal or they appeared unwell on assessment, the NP was to call emergency services and have the patient transported to the closest emergency department. This escalation of care was not necessary during the time of data collection. Additionally, many patients had complex health histories, and it was necessary for the NP to review each patient’s medical history and indication for testing. This was done in preparation for potential emergencies as well as to evaluate for barriers to testing, such as history of head and neck surgery. Orders for the COVID-19 test were ideally placed in the electronic medical record before the patient arrived; however, the NP was also on-site to place orders in real time if necessary.
A clinical lead RN assisted with supply chain management, staffing, and communication with executive leadership. Two MAs were required each shift to facilitate the appointment check-in and check-out process and proper labeling and storage of the specimens. Two RNs were responsible for sample collection, patient education, and notifying the NP about any patients who appeared more ill than expected (ie, short of breath, diaphoretic, lethargic). In addition to clinical staff, successful tent operation required the daily coordination of environmental services, laboratory couriers, on-site security, and executive leadership.
Interventions
COVID-19 testing at the drive-through site was available by appointment only. Patients were required to first call the health system COVID-19 hotline, which was staffed by occupational health department nurses who screened patients for acuity and need for testing based on an algorithm developed by the health system. If determined to be low acuity, patients were scheduled at the drive-through testing site. Higher-acuity patients were scheduled for telehealth or in-person visits with a provider.
Patients would arrive at the drive-through site and check-in with a greeter, a role filled by a staff member from the affiliate medical group, who would direct them to the UCSF of the affiliate medical group drive-through lane. The patient would then be greeted by an RN, who would obtain the patient’s name and date of birth. The MA would check-in the patient via the electronic medical record and prepare the swab kit, while the RN gave a surgical mask and discharge instructions to the patient. Discharge instructions were provided in 6 languages commonly spoken in the area (Spanish, Tagalog, Cantonese, Hindi, Russian, and Mandarin). Additionally, an on-site “Interpreter on Wheels” provided face-to-face real-time translation with a live interpreter via an interpreter service contracted with the health system.
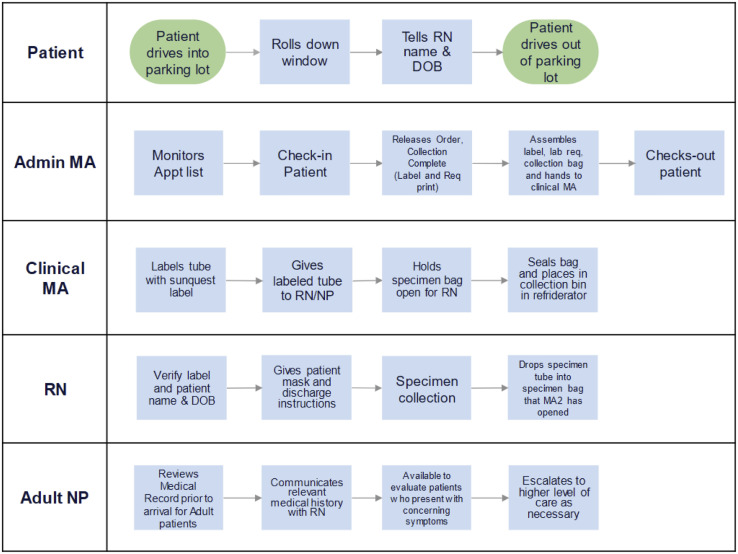
Brief education about the sampling process was provided to the patient, then the RN obtained the specimen sample and deposited it into an open biohazard specimen bag. The testing process took approximately 4 minutes, which included arrival at the site, direction to the appropriate lane, appointment check-in, patient education, and specimen collection (Figure 2 ). Results reporting was centralized through the occupational health department for employees and the electronic medical record for patients.
Figure 2.
Drive-through COVID-19 testing site workflow (DOB = date of birth; MA = medical assistant; NP = nurse practitioner; RN = registered nurse; UCSF = University of California, San Francisco).
Study of the Interventions
We demonstrate that a drive-through testing site is an efficient method of rapidly testing low-acuity patients for COVID-19. Efficiency has been defined by the Institute of Medicine (IOM) as the use of resources, “to get the best value for the money spent” and is considered “the opposite of waste.”6 However, quality must not be sacrificed to achieve efficiency, and thus, to understand whether an intervention is truly efficient, cost of care and clinical outcomes both needed to be examined.6, 7, 8 Furthermore, we demonstrate that NPs are able to quickly adapt and define their role in a new and remote setting, allowing for not only successful daily operation but also the maintenance of patient and staff safety.
Measures
Clinical outcomes were measured by the number of tests performed each day. Cost of care was calculated by totaling the startup, monthly, and daily operating costs for the drive-through testing site. These costs were compared with the number of patients seen each day to determine cost per patient, which was used as an indicator of efficiency. A portion of the startup costs were split with the affiliate medical group operating a drive-through site adjacent to the UCSF site. Environmental services and some supplies, such as tables and chairs and COVID-19 test kits, were not included in the drive-through budget because they were already accounted for by other budgets in the health system.
Daily costs were composed of labor, which were averaged from reported hourly wage data by discipline obtained from the human resources database. Providers (MDs, advanced practice providers), RNs, and “support staff” (generally MAs) were each assigned an average hourly rate that was multiplied by the open hours of operation to yield a daily total labor cost.
Analysis
Data collection occurred during first month of operation between March 25 and April 25, 2020, which totaled 27 operational days. Total startup, monthly, and daily operating costs of the drive-through were calculated and compared with the daily patient census to yield a daily cost per patient. To provide a basis for comparison, labor costs of each RSC and the drive-through testing site were estimated based on the daily staffing needs of each site. This method of cost comparison obviously did not account for total operating costs of each location. It was beyond the scope of the study to understand the total operating cost of each RSC because they each attached to larger medical centers, and the operating costs of each clinic are absorbed into the overall medical center operating costs. Total daily labor costs were used to calculate an average cost per patient to demonstrate one area in which the drive-through testing site generated considerable cost savings. Additionally, to further represent cost differences between the RSCs and the drive-through testing site, total PPE use was compared between each location.
Ethical Considerations
Extreme rationing of test kits has been necessary to ensure that those at highest risk are able to get tested during the coronavirus pandemic. In this study, testing ability was limited to current employees and health system patients. This, unfortunately, excluded large portions of the population, specifically low-income groups, those without access to health care, and the homeless population. Those same groups, as well those who live in congregate settings (ie, prison, long-term care facilities) are the ones at highest risk for contraction and transmission of the virus as well as those most difficult to perform contact tracing on.9 This was a quality improvement project and not subject to institutional review board oversight.
Results
During the data collection period, the drive-through site tested 1,322 patients for COVID-19 with a maximum capacity of 96 patients per day. The number of patients seen daily ranged from 14 to 91, with a mean of 49 patients per day and median of 46 patients per day. The average waiting time for each patient was 1 to 2 minutes, if at all. Total startup and monthly costs totaled to $96,847, which was $3,586.92 per day, excluding labor (Table 2 ). The number of staff required in the tent remained consistent regardless of the number of patients seen per day. Total labor costs averaged $3,519 per day. Mean daily cost per patient, accounting for startup costs, monthly costs, and daily labor costs, was $164. Average cost per patient in the drive-through site continued to trend downward as the daily census increased to meet the demand for testing.
Table 2.
Drive-Through COVID-19 Testing Site Operations Budget, Including Startup and Monthly Costs
| Operational Days |
27 |
|||
|---|---|---|---|---|
| Variable | One-Time Setup | Estimated Monthly Expenses | Tent Portion Ratio | Estimated Tent Costs Total |
| Nonlabor expenses (facilities) | ||||
| Design/permits/coordination | $13,000 | $0 | 50% | $6,500 |
| Tent/furnishing | $0 | $23,556 | 50% | $10,600 |
| Additional tenting/carport wind shield | $358 | $885 | 50% | $577 |
| Additional heater and tent walls w/sandbag | $1,287 | $630 | 50% | $927 |
| Power install/equipment | $14,368 | $3,650 | 50% | $8,827 |
| Generator/reserved on-call | $0 | $2,600 | 50% | $1,170 |
| Electrical engineering | $9,000 | $0 | 50% | $4,500 |
| Laboratory courier service | $0 | $2,200 | 100% | $1,980 |
| Campus services | ||||
| Security services from campus | $0 | $12,980 | 100% | $11,682 |
| Environmental services to drive through from campus | $0 | $0 | 100% | $0 |
| Waste disposal service | $0 | $0 | 100% | $0 |
| Signage (directional signs, advertisements, traffic cones/speed bumps) | $19,400 | $0 | 75% | $14,550 |
| Information technology services/equipment | $34,599 | $0 | 100% | $34,599 |
| Miscellaneous | ||||
| Trash can liners | $0 | $30 | 100% | $27 |
| Indoor table/chairs in annex | $0 | $0 | 100% | $0 |
| Catering | $0 | $360 | 100% | $324 |
| Nonlabor expenses (testing and PPE) | ||||
| Variable expenses | Total Cost to Date, $ | Monthly Upkeep, $ | ||
| Supplies: PPE, sanitation | $584 | $0 | 100% | $584 |
| COVID swabs/test kits | $0 | $0 | 100% | $0 |
| Testing | $0 | $0 | 100% | $0 |
| One Time Setup Total | Monthly Upkeep Total | Operational Total | ||
| Total expenses | $92,596 | $46,891 | $96,847 | |
| Daily operational cost (excluding labor) | $3,586.92 | |||
PPE = personal protective equipment.
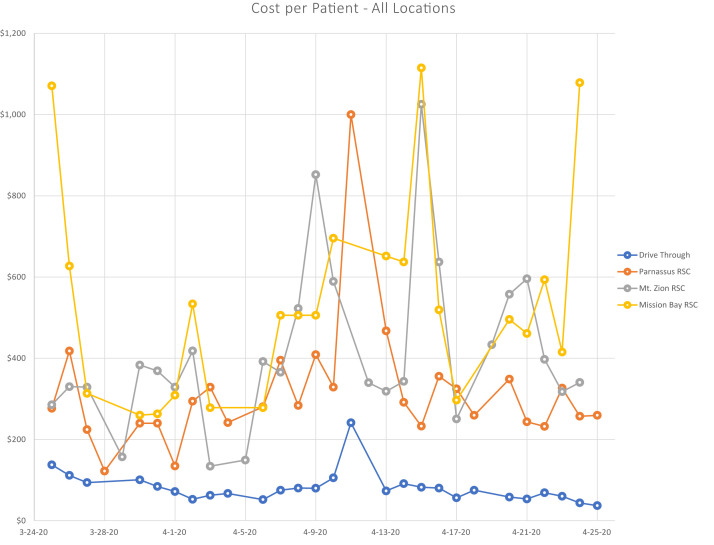
The average cost per patient based on labor costs alone for the drive-through site was $81. This was significantly lower than the cost per patient of any of the RSCs, which averaged $315 to $540. An important limitation of this cost comparison is that it is limited only to cost of labor. The cost per patient at all RSCs began to trend upward toward the later part of the data collection period as increased numbers of patients were directed exclusively to the drive-through. From the initial deployment of the drive-through testing site, the average cost per patient based on labor costs was significantly less than the RSCs, even when the sites were seeing similar numbers of patients (Figure 3 ).
Figure 3.
Cost per patient comparison between the drive through COVID-19 testing site and three respiratory screening clinics (RSC= Respiratory Screening Clinics).
Another aspect of cost reduction and resource use that indicated efficiency was the difference in PPE use between the drive-through site and the RSCs. During the data collection period, the drive-through site ordered $547.54 of PPE, compared with $756.40 and $1,241.84 at 2 of the RSCs. Only $254.48 of PPE was ordered at the third RSC; however, the order for that period did not include any N95 masks or gowns due to pre-existing stock. The reduced PPE use at the drive-through site is because only the RNs testing the patient are required to be in full PPE, which includes a gown or coverall, N95 mask, face shield, and gloves. Although this cost savings further supports the argument for efficiency, it is critical to note that no health care workers have experienced symptoms or tested positive for COVID-19 while working in the drive-through site.
Modifications
The implementation of the drive-through testing site was an evolving process responding to the needs of the community. Within days of opening, testing appointments were quickly shortened from every 15 minutes to every 5 minutes in response to demand. By week 2, asymptomatic bone marrow transplant patients became eligible for testing for preprocedural rule out. By week 3, services were expanded to all patients who met COVID-19 testing criteria as well as essential nonlocal caregivers of hospitalized children. Testing at week 4 was expanded to all health system patients for preprocedural COVID-19 rule out.
By week 3, based on best practice data, the method of swabbing was changed from nasopharyngeal only to both oropharyngeal and nasopharyngeal. This required retraining of RN staff by the NP for the new sampling technique. Finally, by week 3, the option to send respiratory viral panels and rapid flu in addition to the COVID-19 test was added.
Discussion
Our drive-through testing site differs from other drive-through interventions described in the literature because clinical leadership was provided by NPs instead of physicians. NPs are uniquely qualified to function in this environment given their extensive experience as a liaison among the multidisciplinary team and demonstrated ability to function in a variety of settings across health care.10 From parking lots to intensive care units, the adaptable and flexible nature of the NP is critical for the continued provision of quality care in an incredibly overburdened health care system.
In the UCSF COVID-19 drive-through testing site, the NPs led by example, often performing jobs they were not accustomed to—from directing traffic to taking out the trash—in addition to providing clinical supervision. Given the uncertainty of the virulence and symptom progression of COVID-19 as well as the remote nature of the drive-through site, an on-site NP was critical to ensure patient safety. NPs’ advanced assessment skills, ability to diagnose, and experience designing and managing treatment plans was necessary to provide support to the testing RNs.10 RNs have the skills to perform excellent patient assessments; however, while they are able enact treatment plans, they cannot design them. In practice, the RN would see a patient drive up who concerned him or her and would request that the NP evaluate the patient and provide a diagnosis and treatment plan if necessary. Finally, as leaders in health care with a responsibility to remain up to date on evidence-based care,10 including COVID-19, the site NPs were a valuable source of knowledge for staff and patients.
Our NP-led drive-through COVID-19 testing model is an efficient method of testing large numbers of low-acuity patients. Operational costs remained stable as daily patient volume increased, indicating quality was not sacrificed to achieve cost reduction. Additionally, the drive-through model requires less use of PPE without increasing risk for exposure, further reducing costs while maintaining quality. Increased testing capacity allowed the health system to more efficiently provide care for patients suspected of having COVID-19 as well as facilitated the reintroduction of elective procedures through rapid preprocedure COVID-19 screening.
Important differences exist between our drive-through model and other models described in the literature. Implementation of the other drive-through sites described included on-site patient registration, assessment, and triage.4 , 5 In our model, these processes were done before patient arrival via a hotline, which saved time by simplifying the testing process. The model described at Stanford5 demonstrated a median visit length of approximately 26 minutes, whereas in our model the average visit length was approximately 4 minutes per patient. The model implemented in Korea4 was of a similar structure to our drive-through testing model and similarly demonstrated the ability of a drive-through model to test large numbers of patients. However, an important difference in that model was that patients were required to swab themselves, rather than being swabbed by staff. Finally, the study conducted in Philadelphia used a similar staffing model, with RNs performing testing and MAs performing administrative work, yet leadership was provided by physicians.3
Limitations
Several limitations affected our ability to fully evaluate the efficiency of the drive-through testing site. Given that the drive through site remains operational, cost information is approximate and likely incomplete. Additionally, comparison of cost per patient between the drive-through and RSCs was based only on labor costs and did not account for the full operating costs of the RSCs.
Another limitation was the limited quantity of testing kits available, which restricted testing eligibility and prevented us from truly understanding the maximum capacity of the drive-through site.
Third, certain specimen vials leaked or cracked for unknown reasons, causing multiple patients to require repeat testing.
A fourth limitation was the delay in printing the patient identification label due to connectivity issues that could not be resolved given the remote nature of the site.
A final limitation of the drive-through testing model is that it excludes those do not have access to a vehicle. This likely disproportionately affects vulnerable groups, such as the economically disadvantaged, racial and ethnic minorities, those with chronic conditions, the elderly, and the homeless, among others. Although walk-ups were accepted, these numbers were limited because at the time of implementation, large portions of public transportation were not operational. Strategies for addressing this issue will need to be developed in future versions of drive-through testing sites, with emphasis placed on constructing these sites in areas accessible to these vulnerable groups.
Conclusion
A drive-through testing site is an efficient method of safely and rapidly testing large numbers of patients for COVID-19. NPs are ideally suited to provide leadership in these sites. Our model can be used as a blueprint for other drive-through testing efforts and could be scaled up to test larger numbers of patients, even in remote and resource-poor areas. Although the startup costs were significant, the daily operating costs remain relatively predictable and are less than a standard clinic.
Large-scale community testing will help slow the spread quickly, especially for those in the community who are asymptomatic yet infectious.11 Recommendations for further study include expanding the drive-through model to test for other infectious diseases as well as performing routine screenings and providing mass vaccinations. Finally, we recommend that appropriate further pandemic response interventions be developed and studied with the use of NP leadership as a central focus.
Biography
Both authors are at the University of California, San Francisco, San Francisco, California. Kathryn Schultz Dippel, MSN, AGACNP-BC, is a nurse practitioner fellow and can be contacted at Kathryn.Dippel@ucsf.edu., Emily Katherine Kelly, MSN, AGACNP-BC is a nurse practitioner fellow.
Footnotes
In compliance with national ethical guidelines, the authors report no relationships with business or industry that would pose a conflict of interest.
References
- 1.Yen M.H., Schwartz J., Chen S.Y., King C.C., Yang G.Y., Hsueh P.R. Interrupting COVID-19 transmission by implementing enhanced traffic control bundling: implications for global prevention and control efforts. J Microbiol Immunol Infect. 2020;53(3):377–380. doi: 10.1016/j.jmii.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention United States COVID-19 Cases and Deaths by State. 2020. https://covid.cdc.gov/covid-data-tracker/#cases Accessed August 4, 2020.
- 3.Flynn E.F., Kuhn E., Shaik M., Tarr E., Scattolini N., Ballatine A. Drive-through COVID-19 testing during the 2020 pandemic: A safe, efficient and scalable model for pediatric patients and health care workers. Acad Pediatr. 2020;20(6):753–755. doi: 10.1016/j.acap.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kwon K.T., Ko J.H., Shin H., Sung M., Kim J.Y. Drive-through screening center for COVID-19: A safe and efficient screening system against massive community outbreak. J Korean Med Sci. 2020;35(11):e123. doi: 10.3346/jkms.2020.35.e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weiss E.A., Ngo J., Gilbert G.H., Quinn J.V. Drive-through medicine: a novel proposal for rapid evaluation of patients during an influenza pandemic. Ann Emerg Med. 2010;55:268–273. doi: 10.1016/j.annemergmed.2009.11.025. [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine . National Academies Press; 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. [PubMed] [Google Scholar]
- 7.Krumholz H.M., Keenan P.S., Brush J.E., et al. Standards for measures used for public reporting of efficiency in healthcare. J Am Coll Cardiol. 2008;52:1518–1526. doi: 10.1016/j.jacc.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Spivey BE, McDonald WJ. The Measurement of Health Care Performance: A Primer From the CMSS. Council of Medical Specialty Societies. November 2007. Accessed August 4, 2020. https://www.entnet.org/sites/default/files/MeasurementofHealthcarePerf.pdf
- 9.Gandhi R, Lynch J, Carlos R. Mild or moderate COVID-19. N Engl J Med. Published online April 24, 2020. https://doi.org/10.1056/NEJMcp2009249 [DOI] [PubMed]
- 10.American Association of Nurse Practitioners Scope of Practice for Nurse Practitioners. Last revision, 2019. https://www.aanp.org/advocacy/advocacy-resource/position-statements/scope-of-practice-for-nurse-practitioners Accessed August 4, 2020.
- 11.Pan A., Liu L., Wang C., et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323(19):1915–1923. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]