Abstract
Background
Telemedicine refers to various modalities for remote care, including telephone calls, imaging review, and real-time video teleconferencing visits. Although it has not been widely used in outpatient neurosurgery settings, the COVID-19 (coronavirus disease 2019) pandemic has necessitated a broader adoption. Our goal is to show the level of patient satisfaction with their telemedicine care.
Methods
We prospectively studied consecutive telemedicine patients who scheduled outpatient neurosurgery visits from May 15 to June 8, 2020. Patients were seen by the surgeon via real-time video conferencing using Google Meet, and then completed a telemedicine satisfaction survey. Our primary outcome was telemedicine satisfaction scores. We compared satisfaction scores between new and established patients and between patients within and outside of a 15-mile radius of the nearest clinic location. Sensitivity analyses were performed to account for the nonrespondents. Descriptive and univariate analyses were performed. A P value of <0.05 was considered significant.
Results
Five-hundred and ninety patients completed a telemedicine visit during the study period. One patient from out of state was excluded. Three-hundred and ten patients (52.6%) responded. The average age was 60.9 ± 13.60 years; 59% were female, 20.6% were new patients; the average distance to the clinic was 28.03 ± 36.09 km (17.42 ± 22.43 miles). The mean overall satisfaction score was 6.32 ± 1.27. Subgroup analyses by new/established patient status and distance from their home to the clinic showed no significant difference in mean satisfaction scores between groups.
Conclusions
Telemedicine provided a viable and satisfactory option for neurosurgical patients in the outpatient setting during the COVID-19 pandemic.
Key words: COVID-19 pandemic, Neurosurgery, Patient satisfaction, Telehealth, Telemedicine, Virtual visit
Abbreviations and Acronyms: COVID-19, Coronavirus disease 2019; HIPAA, Health Insurance Portability and Accountability Act
Introduction
Telemedicine refers to the use of technology to remotely care for patients. This definition ranges from delivering care via a telephone call or e-mail to viewing imaging to real-time audiovisual virtual visits. Here, we refer to telemedicine or telehealth as the use of real-time video conferencing for virtual appointments.
Historically, telemedicine has mainly been used to provide health care to rural populations for the management of chronic medical and psychological conditions.1, 2, 3, 4 In neurosurgery, real-time visits in the acute care setting have been used for remote triage of patients with stroke or trauma with little application in the outpatient setting.3 , 5 The use of telemedicine had not been widely adopted by practitioners in the United States due to a lack of well-proven need, patients’ limited access to technology, privacy concerns, financial disincentive, and state-specific licensing restrictions.1, 2, 3 , 5 , 6 With the COVID-19 (coronavirus disease 2019) pandemic and subsequent shelter-in-place orders, there was an urgent need to provide outpatient care for patients who were unable or reluctant to visit their providers.
The Coronavirus Preparedness and Response Supplemental Appropriations Act, signed into law on March 6, 2020, provides a waiver of specific Medicare telemedicine payment requirements during the public health emergency. Specifically, the Act allows for reimbursement of telemedicine visits in nonrural settings, and from the patient’s residence using non-HIPAA (Health Insurance Portability and Accountability Act)–compliant video conferencing platforms.
Few studies have examined patient satisfaction with the use of telemedicine for neurosurgical patients in the outpatient setting.3 , 5 In light of the ongoing COVID-19 pandemic, understanding patients’ satisfaction with this care modality is essential for justification and expansion of its use. In this study, we sought to prospectively determine the level of patient satisfaction with neurosurgery telemedicine visits during the COVID-19 pandemic. In addition, we hypothesized that patients with an established relationship with their surgeon and patients living farther from the clinic than closer would have higher satisfaction scores.
Methods
From May 15, 2020, to June 8, 2020, consecutive patients who were seen in the neurosurgery outpatient clinic for either brain or spine disease via telemedicine visits were prospectively included in a patient satisfaction survey. We excluded patients from out of state. All physicians (5 neurosurgeons and 1 orthopedic spine surgeon) and ancillary staff worked remotely.
At the time of appointment scheduling, the patient was sent a link with a date and time confirmation and a link to a virtual meeting using the HIPAA-compliant platform Google Meet (Google, Mountain View, California, USA). Patients also had the option to use FaceTime (Apple Inc., Cupertino, California, USA). An electronic calendar event was automatically generated and sent to the patient with the appointment confirmation e-mail. Imaging and other clinical documentation were collected before the appointment in the usual manner.
Using their devices from home, patients accessed the virtual meeting room, where a member of the intake staff greeted the patient. Any technological issues were addressed and resolved at this point. Simulating the in-person visit process, a medical assistant took a history from the patient and then left the virtual room. The patient was then met by the surgeon, who was joined by a medical scribe. After completion of the visit with the surgeon, the patient was attended by office staff, who completed the checkout process. Immediately after the telemedicine visit, each patient was sent an e-mail with a link to complete the online satisfaction survey. After 72 hours, research staff called patients to remind them to complete the survey or to complete the survey with the patient.
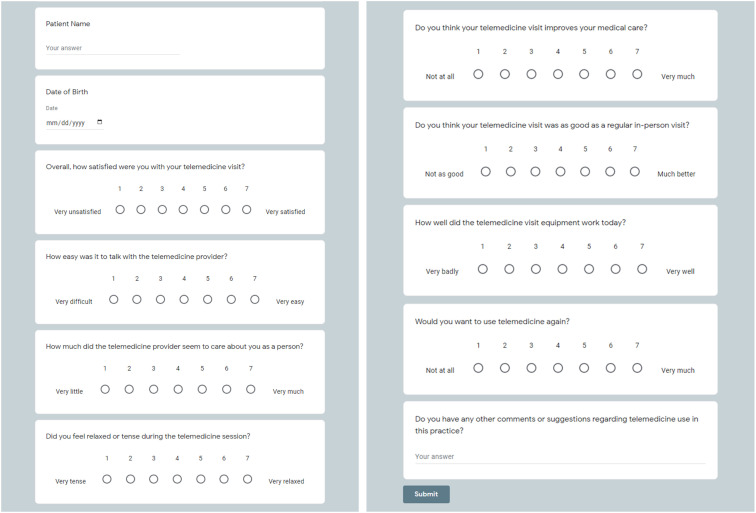
The telemedicine satisfaction survey was conducted using a Google Form consisting of 8 Likert scale questions, as published by Hicks et al.7 Answer choices ranged from 1, representing “very unsatisfied,” to 7, representing “very satisfied” (Supplementary Figure 1). In addition, there was 1 open-ended question for any applicable patient comments. Responses were recorded in a password-protected, HIPAA-compliant electronic database. Demographic, medical history, and visit data were collected from the electronic medical record.
Supplementary Figure 1.
Satisfaction Survey Google Form.
Our primary outcome was telemedicine satisfaction scores. Our secondary outcome was disposition after telemedicine visits. Descriptive statistics were used. A Mann-Whitney U test was used to compare satisfaction scores between new and established patients and between patients within and outside a 24.14-km (15-mile) radius of the nearest clinic location. Sensitivity analyses were performed to account for the nonresponders. Data were analyzed using SPSS for Windows version 25.0 (IBM Corp., Armonk, New York, USA). A P value <0.05 was considered significant.
Results
The survey link was sent to 590 patients who completed a telemedicine visit from May 15 to June 8, 2020. One patient with a primary address in Florida was excluded. Of the 589 patients, 310 patients (52.6%) completed the satisfaction survey. The average time to survey completion was 15.19 ± 10.5 days (range, 0.40–36.5 days). Demographic data are shown in Table 1 . The average distance to the nearest clinic location was 28.03 ± 36.09 km (17.42 ± 22.43 miles). Five patients lived >160 km (100 miles) away. Sixty-four visits (20.6%) were for new patients. A total of 109 patients (35.2%) were working full time; 25 (8.1%) working part time; 110 (35.5%) retired; 12 (3.9%) unemployed; 38 (12.3%) on disability; and 16 (5.2%) patients’ employment status was unknown. A total of 122 patients (39.4%) had private insurance; 157 (50.6%); government insurance; 29 (9.4%) auto or workers’ compensation insurance, and 2 (0.6%) self-pay/other.
Table 1.
Patient Demographics (N = 310)
| Value | |
|---|---|
| Age (years) | 60.89 ± 13.60 |
| Distance (km) | 28.03 ± 36.09 (17.42 ± 22.43 miles) |
| Sex | |
| Male | 127 (41.0) |
| Female | 183 (59.0) |
| Visit type | |
| New patient | 64 (20.6) |
| Return patient | 217 (70.0) |
| Postoperative appointment | 29 (9.4) |
| Insurance | |
| Government | 157 (50.6) |
| Private | 122 (39.4) |
| Auto/workers' compensation | 29 (9.4) |
| Self-pay/other | 2 (0.6) |
| Employment status | |
| Working full time | 109 (35.2) |
| Working part time | 25 (8.1) |
| Retired | 110 (35.5) |
| Unemployed | 12 (3.9) |
| Disability | 38 (12.3) |
| Unknown | 16 (5.2) |
Continuous data are presented as mean ± standard deviation. Categorical data are presented as n (%).
Satisfaction scores for individual survey questions are shown in Table 2 . In response to overall patient satisfaction with the visit, the average score was 6.32 ± 1.27 out of 7. Visit disposition after the telemedicine visit is shown in Table 3 . Eighty-four patients (27.1%) scheduled surgery, 175 patients (56.5%) scheduled follow-up visits, 94 patients (30.3%) had imaging ordered, and 1 patient (0.3%) was sent to the emergency department for direct hospital admissions.
Table 2.
Satisfaction Outcomes
| Patient Satisfaction Scores, 1–7 (N = 310) | Mean ± Standard Deviation |
|---|---|
| Overall, how satisfied were you with your telemedicine visit? | 6.32 ± 1.27 |
| How easy was it to talk with the telemedicine provider? | 6.51 ± 1.17 |
| How much did the telemedicine provider seem to care about you as a person? | 6.70 ± 0.85 |
| Did you feel relaxed or tense during the telemedicine session? | 6.38 ± 1.27 |
| Do you think your telemedicine visit improves your medical care? | 5.51 ± 1.83 |
| Do you think your telemedicine visit was as good as a regular in-person visit? | 4.55 ± 2.12 |
| How well did the telemedicine visit equipment work today? | 6.12 ± 1.55 |
| Would you want to use telemedicine again? | 5.56 ± 1.93 |
Table 3.
Visit Disposition After Telemedicine Visit
| Visit Disposition (N = 310) | n (%) |
|---|---|
| Follow-up scheduled | 175 (56.5) |
| Surgery scheduled | 84 (27.1) |
| Imaging ordered | 94 (30.3) |
| Referral given | 70 (22.6) |
| Medication prescribed | 49 (15.8) |
| Return as needed | 61 (19.7) |
| Return to work | 9 (2.9) |
| Disability paperwork | 17 (5.5) |
| Direct admission to emergency room | 1 (0.3) |
We compared the satisfaction scores between new patients and returning patients (Table 4 ).There was no significant difference in mean scores between the groups for any of the survey questions. We compared the satisfaction scores between patients living within a 24.14-km (15-mile) radius of our closest clinic and living farther than 24.14-km (15 miles) away. Comparing the <24.14-km (15-mile) group with the >24.14-km (15-mile) group, the mean distance from the patients’ home to our closest clinic was 13.79 ± 5.82 km (8.57 ± 3.62 miles) and 41.40 ± 20.72 km (25.73 ± 12.88 miles) after we removed 5 patients who lived >160 km (100 miles) away from our nearest clinic. The median of the overall satisfaction scores for these 5 patients were 6.5 (range, 6.25–7). There was no statistically significant difference between the scores of these 2 groups of patients (Table 5 ).
Table 4.
Satisfaction by Visit Type
| New Patients (n = 64), Mean ± SD | Returning Patients (n = 246), Mean ± SD | Δ Mean | 95% Confidence Interval | P Value | |
|---|---|---|---|---|---|
| Overall, how satisfied were you with your telemedicine visit? | 6.30 ± 1.29 | 6.33 ± 1.27 | –0.032 | –0.39 to 0.33 | 0.858 |
| How easy was it to talk with the telemedicine provider? | 6.38 ± 1.42 | 6.54 ± 1.10 | –0.17 | –0.55 to 0.21 | 0.376 |
| How much did the telemedicine provider seem to care about you as a person? | 6.67 ± 0.87 | 6.71 ± 0.84 | –0.04 | –0.28 to 0.20 | 0.746 |
| Did you feel relaxed or tense during the telemedicine session? | 6.25 ± 1.31 | 6.41 ± 1.26 | –0.16 | –0.52 to 0.20 | 0.376 |
| Do you think your telemedicine visit improves your medical care? | 5.38 ± 1.72 | 5.55 ± 1.85 | –0.17 | –0.66 to 0.31 | 0.481 |
| Do you think your telemedicine visit was as good as a regular in-person visit? | 4.44 ± 2.05 | 4.59 ± 2.14 | –0.15 | –0.72 to 0.43 | 0.611 |
| How well did the telemedicine visit equipment work today? | 5.98 ± 1.54 | 6.15 ± 1.56 | –0.17 | –0.60 to 0.26 | 0.434 |
| Would you want to use telemedicine again? | 5.56 ± 1.81 | 5.56 ± 1.97 | 0.01 | –0.51 to 0.52 | 0.983 |
P < 0.05 was considered significant.
SD, standard deviation.
Table 5.
Satisfaction by Distance From Site
| New Patients (n = 64), Mean ± SD | Returning Patients (n = 246), Mean ± SD | Δ Mean | 95% Confidence Interval | P Value | |
|---|---|---|---|---|---|
| Overall, how satisfied were you with your telemedicine visit? | 6.28 ± 1.31 | 6.39 ± 1.22 | –0.11 | –0.40 to 0.18 | 0.461 |
| How easy was it to talk with the telemedicine provider? | 6.51 ± 1.12 | 6.51 ± 1.25 | –0.004 | –0.28 to 0.27 | 0.975 |
| How much did the telemedicine provider seem to care about you as a person? | 6.67 ± 0.91 | 6.76 ± 0.75 | –0.09 | –0.28 to 0.10 | 0.325 |
| Did you feel relaxed or tense during the telemedicine session? | 6.47 ± 1.16 | 6.24 ± 1.41 | 0.22 | –0.08 to 0.53 | 0.148 |
| Do you think your telemedicine visit improves your medical care? | 5.39 ± 1.96 | 5.71 ± 1.58 | –0.33 | –0.72 to 0.07 | 0.110 |
| Do you think your telemedicine visit was as good as a regular in-person visit? | 4.51 ± 2.16 | 4.63 ± 2.07 | –0.12 | –0.60 to 0.36 | 0.624 |
| How well did the telemedicine visit equipment work today? | 6.16 ± 1.54 | 6.05 ± 1.58 | 0.11 | –0.24 to 0.47 | 0.530 |
| Would you want to use telemedicine again? | 5.48 ± 1.96 | 5.68 ± 1.89 | –0.20 | –0.64 to 0.24 | 0.380 |
P < 0.05 was considered significant.
SD, standard deviation.
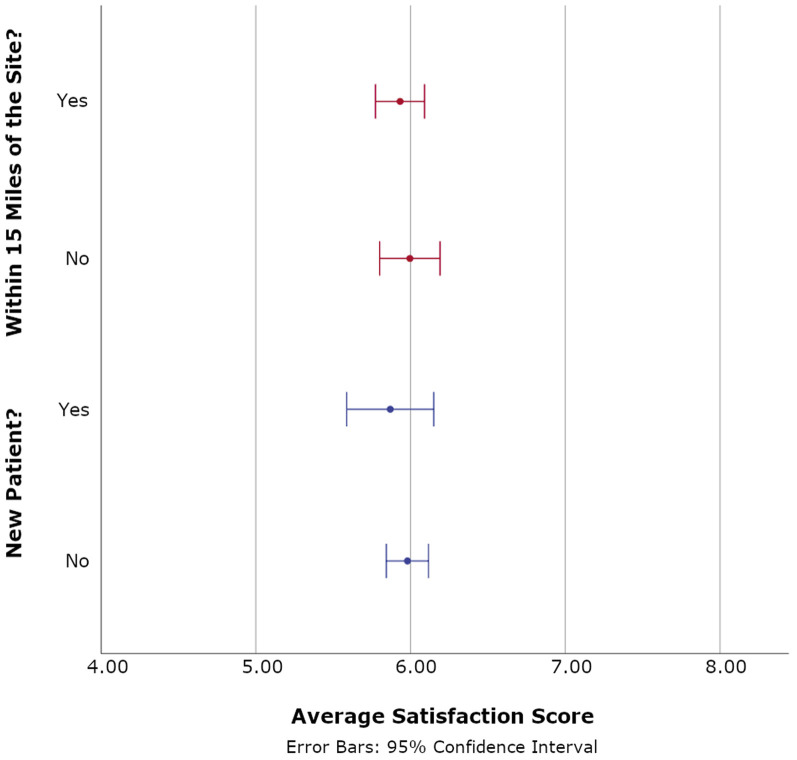
We repeated the comparison analyses between these 2 pairs by using the average satisfaction scores of all 8 questions in each survey. We considered the patients to be generally “satisfied” with their telemedicine visit when their average response of all survey questions was ≥4. We considered them generally “not satisfied” when their average response of all survey questions was <4. When comparing new and returning patients, the proportion of patients satisfied with the telemedicine visit was 93.8% versus 94.7%. When comparing patients living within a 24.14-km (15-mile) radius of our closest clinics and those living farther, the proportion of patients satisfied with the telemedicine visit was 93.7% versus 95.5% (Table 6 ). There was no statistical significance in either comparison (Figure 1 ).
Table 6.
Overall Satisfaction by Visit Type and Distance From Site (N = 310)
| Satisfied, n (%) | Not Satisfied, n (%) | P Value | |
|---|---|---|---|
| Visit type | 0.762 | ||
| New patient (n = 64) | 60 (93.8) | 4 (6.3) | — |
| Returning patient (n = 246) | 233 (94.7) | 13 (5.3) | — |
| Distance | 0.403 | ||
| ≤24.14 km (15 miles) (n = 189) | 177 (93.7) | 12 (6.3) | — |
| >24.14 km (15 miles) (n = 121) | 116 (95.9) | 5 (4.1) | — |
P < 0.05 was considered significant.
Figure 1.
Average Satisfaction Score by Distance from Site and Type of Visit.
We performed a sensitivity analysis to account for 47.4% of nonrespondents (Table 7 ). Assuming that all missing patients were satisfied, the overall satisfaction rate was 97.1% (572/589). Assuming that all missing patients were unsatisfied, the overall satisfaction rate was 50.3% (296/589).
Table 7.
Compliance and Sensitivity Analyses of Satisfaction Scores
| Observed Values | |
| Compliance rate | 310 (52.6) |
| Number satisfied | 293 (94.5) |
| Number dissatisfied | 17 (5.5) |
| Average satisfaction score | 5.96 ± 1.09 |
| Missing values | |
| Loss of follow-up | 279 (47.4) |
| Satisfaction assuming all missing patients are satisfied | 572 (97.1) |
| Dissatisfaction assuming all missing patients are dissatisfied | 296 (50.3) |
Continuous data are presented as mean ± standard deviation. Categorical data are presented as n (%).
Patients were considered “satisfied” with their telemedicine visits when their average response of all survey questions was ≥4.
Discussion
The Value of Telemedicine
There has been tentative evidence regarding the cost-effectiveness of telemedicine.2 , 3 , 5 , 6 Although telemedicine involves initial startup costs for the provider, the net benefits for patients were clear. Telemedicine saved money for patients and their caregivers in travel expenses and time away from work.3 , 6 , 8, 9, 10, 11 In the setting of the COVID-19 pandemic, telemedicine is a safer option, particularly for vulnerable patients at greater risk of COVID-19-related morbidity or mortality.
Studies involving the use of telemedicine for neurosurgical patients in the postoperative setting have shown safety and satisfaction. One prospective study by Reider-Demer et al.11 showed no significant difference in readmission or emergency department visit rates when using telemedicine for postoperative visits after elective craniotomies. The study also showed that 100% of patients reported satisfaction with their telemedicine visit, and 85% of patients responded that they would prefer telemedicine to an in-person appointment for future postoperative visits.
In our respondents, the overall satisfaction with telemedicine was high, with an average score of 5.96 ± 1.09 out of 7 points. In addition, 94.5% of respondents were overall satisfied (average survey response ≥4) with their telemedicine visit. This finding is consistent with the results of previous studies showing high satisfaction for telemedicine visits.5 , 7 , 9 A few patients commented that they would prefer an in-person meeting. However, given the circumstances, these patients believed that telemedicine was a satisfactory alternative to delayed care. A similar sentiment has been seen in previous studies.5 , 7 , 9 Although patients may prefer an in-person visit, they would choose telemedicine over traveling a long distance to an appointment.10 Although the lowest-rated question was regarding whether patients believed that their telemedicine visit was as good as an in-person visit, the rating was still positive overall, with an average score of 4.55 ± 2.12 out of 7.
We hypothesized that new patients would report lower satisfaction with telemedicine compared with returning patients. The lowest scored question (4.44 ± 2.05), “Do you think your telemedicine visit was as good as a regular in-person visit?,” was scored among new patients. However, comparing the 2 groups, there was no significant difference in satisfaction scores for individual survey questions or the proportion of patients being overall satisfied. The failure to achieve statistical significance may be due to imbalance of the groups, with 64 new patients compared with 246 returning patients. Between the 2 groups, the satisfaction scores for each question were similar. Our finding is in contrast to a previous study8 that found that patients familiar with telemedicine scored higher satisfaction. A larger sample size and a more balanced patient type distribution could help further clarify this issue.
We expected that patients who lived farther from our closest clinics would be more likely to prefer telemedicine based on previous studies showing a high degree of satisfaction when patients saved time and money by avoiding extensive travel.3 , 6 , 8, 9, 10, 11 Our highest scored question (6.76 ± 0.75), “How much did the telemedicine provider seem to care about the patient as a person?,” was scored among patients living farther than 24.14 km (15 miles) from our closest clinics. Although statistically insignificant, patients living farther than 24.14 km (15 miles) from our closest clinics gave a higher score (5.68 ± 1.89) in response to the desire to use telemedicine again compared with those living within 24.14 km (15 miles) (5.48 ± 1.96). One reason for this result is the conversion of the distance variable into a binary variable using 24.14 km (15 miles) as the cutoff. The mean distance from the patients’ home to our closest clinic location was 13.79 ± 5.82 km (8.57 ± 3.62 miles) in the <24.14 km (15 miles) group and 41.40 ± 20.72 km (25.73 ± 12.88 miles) with the >24.14 km (15 miles) group after we excluded the 5 patients who lived >160 km (100 miles) away. The mean distance of 28.03 ± 36.09 km (17.42 ± 22.43 miles) from the patient’s home to our closest clinic had a significantly right-skewed distribution, with 84% of the patients living within 64.13 km (39.85 miles) of our closest clinic.
Strengths
This is the largest study to evaluate patient satisfaction with telemedicine visits in neurosurgical patients in the United States. In addition, our response rate of 52.6% is consistent with the literature. Although survey response rates are not widely available, 2 studies reported 34.5% and 83%, respectively.11 , 12 A review of 717 surveys13 reported an average response rate of 49.8% (range, 16.1%–80%). Another review of 210 studies of patient satisfaction14 reported an average response rate of 72.1%; however, the investigators noted that this review included surveys that recruited patients in-person, which had statistically significantly higher response rates. In the setting of telemedicine, the response rate could be improved by close monitoring of survey completion and facilitation by electronic reminders by SMS (short message service), push notifications, or e-mail.
We showed a high level of patient satisfaction with telemedicine given a wide range of interval to completion. This finding is consistent with the available data suggesting mixed effects of time to survey on patient satisfaction.15, 16, 17, 18
Limitations
The telemedicine survey used in this survey is not a validated instrument. Nevertheless, it is the instrument used in another telemedicine satisfaction study.7 The expediency required by the COVID-19 pandemic necessitated its adoption in our study. Another distinction is that the data were collected during the COVID-19 pandemic, when health care providers have been viewed in a positive light, which could have improved satisfaction scores.
Future Directions
A large study of >1500 neurosurgical patients by Dadlani et al.4 reported that the use of telemedicine was associated with 100% sensitivity and 94% specificity in the identification of postoperative complications using telemedicine. In identifying preoperative problems through virtual physical examination via telemedicine, several nonneurosurgical studies have shown accuracy.10 , 19, 20, 21 However, this problem has not been widely addressed in neurosurgical patients. We anticipate that the difficulty in identifying subtle neurologic deficits through the physical examination will contribute to the limitations of telemedicine in the neurosurgery. Although gross cranial nerve deficits may be observable through Internet video platforms, more subtle deficits (e.g., sternocleidomastoid and trapezius weakness) would be challenging to detect virtually. Subtle differences in muscle strength, reflexes, and cerebellar signs would also be difficult to detect via telemedicine.
Future studies would benefit from surveying patients using more in-depth questions, questions specific to neurosurgical disease, and a validated instrument for patient satisfaction in the setting of telemedicine. In the next phase of our study, we will compare patient satisfaction and diagnostic accuracy between patients in telemedicine and in-person settings, during and outside of the pandemic when applicable.
Patient satisfaction with telemedicine may be influenced by the individual’s comfort with video technology and Internet access. Some studies showed that low income and elderly populations were less likely to use the Internet or to have Internet access. With the COVID-19 pandemic, the federal government has allocated funds for improving data connections and providing hardware to patients and providers to facilitate further adoption of telemedicine.22 Centers for Medicare and Medicaid Services approved the use of non-HIPAA–compliant platforms, which allowed patients to use popular platforms such as FaceTime, Skype, or Google Hangouts/Google Meet. In a study of postoperative patients, respondents who had already used a telemedicine protocol reported high satisfaction, presumably because of familiarity with the technology.8 As patients continue to grow more comfortable with telemedicine, we anticipate that the use of telemedicine will become more widespread in health care.
Conclusions
The COVID-19 pandemic has provided an opportunity for telemedicine to be more widely used in neurosurgery. Telemedicine is a valuable tool to reduce the risk of patient exposure and deliver the care that they require. However, patient satisfaction with telemedicine has not been fully studied. With 310 patients prospectively studied, our high level of patient satisfaction strongly supported the use of telemedicine care in neurosurgical outpatient care, regardless of the patient’s geographic location and visit type. Further telemedicine studies are warranted to evaluate its use outside the pandemic and regarding clinical outcomes.
CRediT authorship contribution statement
Elise J. Yoon: Methodology, Investigation, Writing - original draft, Writing - review & editing. Doris Tong: Conceptualization, Methodology, Formal analysis, Writing - review & editing, Visualization. Gustavo M. Anton: Conceptualization, Investigation, Writing - original draft, Writing - review & editing. Jacob M. Jasinski: Validation, Writing - review & editing. Chad F. Claus: Conceptualization, Writing - review & editing. Teck M. Soo: Conceptualization, Resources, Writing - review & editing. Prashant S. Kelkar: Conceptualization, Methodology, Resources, Writing - review & editing.
Acknowledgments
The authors would like to thank Connor Hanson and Madeline Fugate for their help with this study.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Data
References
- 1.Flodgren G., Rachas A., Farmer A.J., Inzitari M., Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015;2015:CD002098. doi: 10.1002/14651858.CD002098.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gilman M., Stensland J. Telehealth and Medicare: payment policy, current use, and prospects for growth. Medicare Medicaid Res Rev. 2013;3 doi: 10.5600/mmrr.003.04.a04. mmrr.003.04.a04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thakar S., Rajagopal N., Mani S. Comparison of telemedicine with in-person care for follow-up after elective neurosurgery: results of a cost-effectiveness analysis of 1200 patients using patient-perceived utility scores. Neurosurg Focus. 2018;44:E17. doi: 10.3171/2018.2.FOCUS17543. [DOI] [PubMed] [Google Scholar]
- 4.Dadlani R., Mani S., Jai Ganesh A.U. The impact of telemedicine in the postoperative care of the neurosurgery patient in an outpatient clinic: a unique perspective of this valuable resource in the developing world–an experience of more than 3000 teleconsultations. World Neurosurg. 2014;82:270–283. doi: 10.1016/j.wneu.2014.05.027. [DOI] [PubMed] [Google Scholar]
- 5.Kahn E., La Marca F., Mazzola C. Neurosurgery and telemedicine in the United States: assessment of the risks and opportunities. World Neurosurg. 2016;89:133–138. doi: 10.1016/j.wneu.2016.01.075. [DOI] [PubMed] [Google Scholar]
- 6.Blue R., Yang A.I., Zhou C. Telemedicine in the era of coronavirus disease 2019 (COVID-19): a neurosurgical perspective. World Neurosurg. 2020;139:549–557. doi: 10.1016/j.wneu.2020.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hicks L.L., Boles K.E., Hudson S. Patient satisfaction with teledermatology services. J Telemed Telecare. 2003;9:42–45. doi: 10.1258/135763303321159684. [DOI] [PubMed] [Google Scholar]
- 8.Gunter R.L., Chouinard S., Fernandes-Taylor S. Current use of telemedicine for post-discharge surgical care: a systematic review. J Am Coll Surg. 2016;222:915–927. doi: 10.1016/j.jamcollsurg.2016.01.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davis L.E., Coleman J., Harnar J., King M.K. Teleneurology: successful delivery of chronic neurologic care to 354 patients living remotely in a rural state. Telemed J E Health. 2014;20:473–477. doi: 10.1089/tmj.2013.0217. [DOI] [PubMed] [Google Scholar]
- 10.Sudan R., Salter M., Lynch T., Jacobs D.O. Bariatric surgery using a network and teleconferencing to serve remote patients in the Veterans Administration Health Care System: feasibility and results. Am J Surg. 2011;202:71–76. doi: 10.1016/j.amjsurg.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 11.Reider-Demer M., Raja P., Martin N., Schwinger M., Babayan D. Prospective and retrospective study of videoconference telemedicine follow-up after elective neurosurgery: results of a pilot program. Neurosurg Rev. 2018;41:497–501. doi: 10.1007/s10143-017-0878-0. [DOI] [PubMed] [Google Scholar]
- 12.Becevic M., Boren S., Mutrux R., Shah Z., Banerjee S. User satisfaction with telehealth: study of patients, providers, and coordinators. Health Care Manag. 2015;34:337–349. doi: 10.1097/HCM.0000000000000081. [DOI] [PubMed] [Google Scholar]
- 13.Perneger T.V., Peytremann-Bridevaux I., Combescure C. Patient satisfaction and survey response in 717 hospital surveys in Switzerland: a cross-sectional study. BMC Health Serv Res. 2020;20:1–8. doi: 10.1186/s12913-020-5012-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sitzia J., Wood N. Response rate in patient satisfaction research: an analysis of 210 published studies. Int J Qual Health Care. 1998;10:311–317. doi: 10.1093/intqhc/10.4.311. [DOI] [PubMed] [Google Scholar]
- 15.Bjertnaes O.A. The association between survey timing and patient-reported experiences with hospitals: results of a national postal survey. BMC Med Res Methodol. 2012;12:13. doi: 10.1186/1471-2288-12-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deutsch A., Heinemann A.W., Cook K.F. Inpatient rehabilitation quality of care from the patient’s perspective: effect of data collection timing and patient characteristics. Arch Phys Med Rehabil. 2019;100:1032–1041. doi: 10.1016/j.apmr.2018.10.019. [DOI] [PubMed] [Google Scholar]
- 17.Jensen H.I., Ammentorp J., Kofoed P.-E. User satisfaction is influenced by the interval between a health care service and the assessment of the service. SocSci Med. 2010;70:1882–1887. doi: 10.1016/j.socscimed.2010.02.035. [DOI] [PubMed] [Google Scholar]
- 18.Saal D., Nuebling M., Husemann Y., Heidegger T. Effect of timing on the response to postal questionnaires concerning satisfaction with anaesthesia care. Br J Anaesth. 2005;94:206–210. doi: 10.1093/bja/aei024. [DOI] [PubMed] [Google Scholar]
- 19.Asiri A., Al Bishi S., Al Madani W., El Metwally A., Househ M. The use of telemedicine in surgical care: a systematic review. Acta Inform Med. 2018;26:201–206. doi: 10.5455/aim.2018.26.201-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robie D.K., Naulty C.M., Parry R.L. Early experience using telemedicine for neonatal surgical consultations. J Pediatr Surg. 1998;33:1172–1177. doi: 10.1016/s0022-3468(98)90554-1. [DOI] [PubMed] [Google Scholar]
- 21.Wood E.W., Strauss R.A., Janus C., Carrico C.K. Telemedicine consultations in oral and maxillofacial surgery: a follow-up study. J Oral Maxillofac Surg. 2016;74:262–268. doi: 10.1016/j.joms.2015.09.026. [DOI] [PubMed] [Google Scholar]
- 22.Contreras C.M., Metzger G.A., Beane J.D., Dedhia P.H., Ejaz A., Pawlik T.M. Telemedicine: patient-provider clinical engagement during the COVID-19 pandemic and beyond. J Gastrointest Surg. 2020;24:1692–1697. doi: 10.1007/s11605-020-04623-5. [DOI] [PMC free article] [PubMed] [Google Scholar]