Abstract
Background: In rare circumstances, patients with intracranial (dural arteriovenous fistulas) DAVFs could be complicated with brainstem engorgement, which might lead to delayed or false diagnosis and subsequent improper management.
Methods: On July 2th, 2019, a systematic search was conducted in the PubMed database for patients with intracranial DAVFs complicated with brainstem engorgement.
Results: Sixty-eight articles reporting of 86 patients were included for final analysis. The patients were aged from 20 to 76 years (57.10 ± 12.90, n = 82). The female to male ratio was 0.68 (35:51). Thirty-three (40.2%, 33/82) patients were initially misdiagnosed as other diseases. The specific location distributions were cranio-cervical junction, cavernous sinus, superior petrosal sinus, transverse and/or sigmoid sinus, tentorium, and other sites in 27 (32.5%), 11 (13.2%), 9 (10.8%), 10 (12.0%), 21 (25.3%), and 5 (6.0%) patients, respectively. The Cognard classification of DAVFs were II, III, IV, and V in 9 (10.7%, 9/84), 1 (1.2%, 1/84), 1 (1.2%, 1/84), and 73 (86.9%, 73/84) patients. Eighteen (22%, 18/82) patients were demonstrated to have stenosis or occlusion of the draining system distal to the fistula points. The mean follow-up period was 7.86 (n = 74, range 0–60 months) months. Fifty-four (70.1%, 54/77) patients experienced a good recovery according to the mRS score.
Conclusions: Intracranial DAVFs complicated with brainstem engorgement are rare entities. Initial misdiagnosis and delayed definite diagnosis are common in the past three decades. The treatment outcome is still unsatisfactory at present. Early awareness of this rare entity and efficiently utilizing the up to date investigations are of utmost importance.
Keywords: dural arteriovenous fistula, brainstem engorgement, transarterial embolization, transvenous embolization, open surgery
Introduction
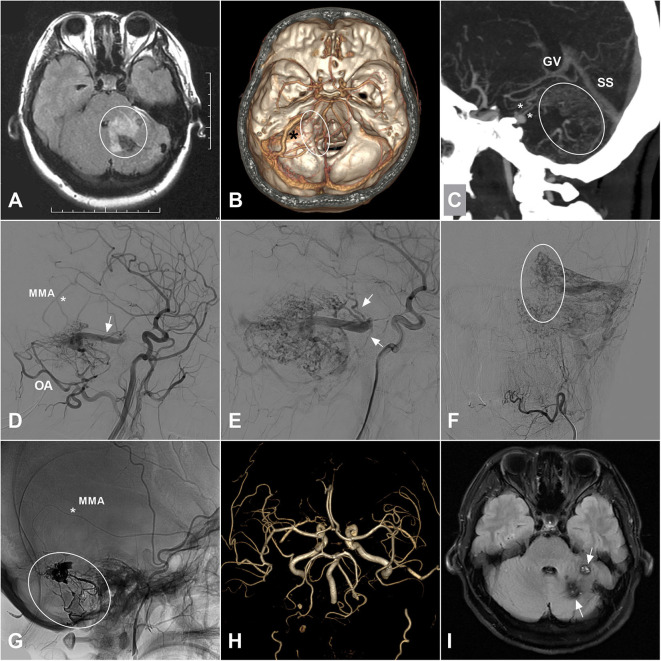
Dural arteriovenous fistula (DAVF) is a unique subtype of vascular malformations along the central nervous system, which is characterized by abnormal connections between meningeal/pial arteries and dural venous sinuses, meningeal veins, or cortical veins. The estimated detection rate was 0.29 per 100,000 persons per year according to a Japanese survey published in 2016 (1). In rare circumstances, patients with intracranial DAVFs could be complicated with brainstem engorgement, which might lead to delayed or false diagnosis and subsequent improper management (2–4). An illustrate case of intracranial DAVF with brainstem engorgement was presented in Figure 1. As a result of its rarity in occurrence, large case series in a single center is extremely hard to be anticipated. In order to explore the epidemiological, clinical, imaging, and prognostic characteristics of this specific entity, we conducted a systematic review of the literature.
Figure 1.
(A) A 35-years-old female was admitted for 3-days history of headache and vomiting. MRI on FLAIR sequence reveals a hyperintense left cerebellar lesion (white circle) with the adjacent brainstem involvement. Besides, vascular flow voids are also noted at the posterior fossa. (B) CTA shows an abnormally enlarged vein (asterisk) draining from the cerebellar surface to the brainstem. And some enlarged veins (ellipse) around the brainstem are also noted. (C) MIP of CTA shows the enlarged draining veins in the cerebellum (ellipse) and around the brainstem (asterisks). (D) Angiogram of the left ECA in lateral view shows a DAVF supplied by the MMA (asterisk) and OA and drained to the deep veins via an enlarged superficial vein (arrow). (E) Angiogram in late arterial phase shows the deep veins (arrow) around the brainstem. (F) Angiogram of the left ECA in anteroposterior view shows enlarged veins in the left cerebellar hemisphere. The ellipse indicates the midline veins. (G) Unsubtracted angiogram shows the DAVF is embolized with Onyx (ellipse) via the MMA (asterisk). (H) Follow-up MRA 1 month postoperatively shows disappearance of the DAVF. (I) Follow-up MRI on FLAIR sequence shows remission of the brainstem and cerebellar edema and deposition of hemosiderin (arrow). CTA, computed tomography angiography; DAVF, dural arteriovenous fistula; ECA, external carotid artery; FLAIR, fluid attenuated inversion recovery; MIP, maximum intensity projection; MMA, middle meningeal artery; MRA, magnetic resonance angiography; MRI, magnetic resonance imaging; OA, occipital artery.
Methods
On July 2th, 2019, a systematic search was conducted in the PubMed database for patients with intracranial DAVFs complicated with brainstem engorgement. Brainstem engorgement, brain stem engorgement, brainstem edema, brainstem oedema, brain stem edema, brain stem oedema, brainstem congestion, brain stem congestion, brainstem venous congestion, brain stem venous congestion, venous congestion of brain stem, venous congestion of brainstem, myelopathy, and dural arteriovenous fistula were used as key words in relevant combinations. Articles included were: (1) of which the full text could be obtained, or (2) sufficient data could be obtained from the abstract if the full text is inaccessible. Of note, studies reporting large case series were excluded from the final analysis if sufficient description of the individual clinical information was not provided. Manual searching of the reference lists of the identified articles were also performed for additional studies. We used modified Rankin Scale (mRS) for outcome assessment. An mRS score ≤ 3 was defined as good recovery.
Results
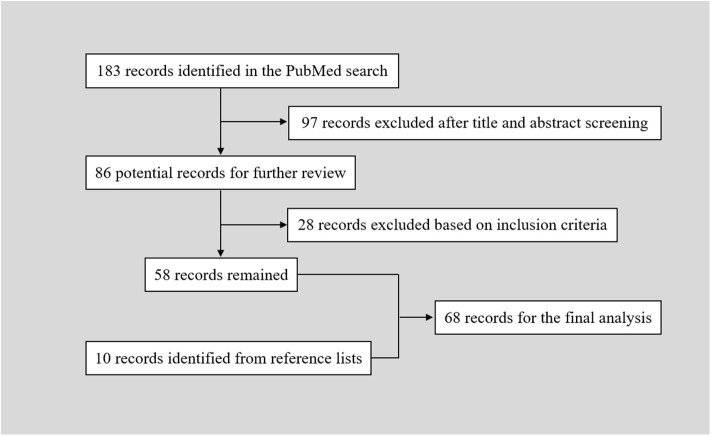
The PubMed search yielded 183 records. After a primary screening of the titles and abstracts, 97 records were excluded. After full text assessment of the 86 identified articles, 28 records were further excluded. We manually searched the reference lists of the remaining 58 articles. And 10 additional articles were identified. Finally, 68 articles reporting of 86 patients were included in the final analysis (Table 1) (2–69). The flow chart of searching strategy was presented in Figure 2. The patients were aged from 20 to 76 years (57.10 ± 12.90, n = 82). The female to male ratio was 0.68 (35:51).
Table 1.
Intracranial DAVFs complicated with brainstem engorgement.
| No. | Author/year | Age/sex | Presentation/interval to definite diagnosis | Initial misdiagnosis | DAVF location | Concurrent with venous sinus stenosis/occlusion | Signal alteration on MRI | Region of congestion | Feeding artery | Draining vein | Cognard classification | Treatment | Degree of DAVF obliteration | Follow-up period | Retreatment | Outcome (mRS) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1, T1 C+ | T2 | FLAIR | DWI, ADC | Abnormal vascular flow-void | ||||||||||||||||
| 1 | Probst et al. (5) | 40/F | Headache, nausea, and dnormalrientation/ NA/NM | Yes (brain tumor) | TS | Yes | NA/NM, inhomogeneous enhancement | Hyper | NA/NM | NA/NM, NA/NM | Yes | Pons, cerebellum, and thalamus | OA and branches of the ICA | Straight sinus → vein of Galen → pontomesencephalic vein → vein of Rosenthal | Type V | Endovascular + surgical | Completely | NA/NM | No | 0 |
| 2 | Uchino et al. (6) | 68/F | Gait disturbance, dysarthria, and urinary incontinence/4 years | No | CS | Yes | Hypo, enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Pons | Branches of ECA and ICA | Vein of Rosenthal, inferior anastomotic vein of Labbe, pontine venous congestion | Type IIB | Subtotal TAE of ECA branches with polyvinyl alcohol particles | Incompletely | 2 years | No | 5 |
| 3 | 74/M | Chemosis, proptosis, and gait disturbance/ NA/NM | No | CS | Yes | Hypo, enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Pons and cerebellum | Branches of ECA and ICA | Cortical veins of the posterior fossa, pontine venous congestion | Type IIA+B | Subtotal TAE of ECA branches with polyvinyl alcohol particles | Incompletely | 4 months | No | 2 | |
| 4 | Ernst et al. (7) | 71/M | Paraparesis, nausea, and vomiting/ NA/NM | No | SPS | No | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Hypoer medulla oblongata extending to the upper cervical cord | MHT of the ICA | PMV | Type V | Open surgery | Completely | 18 months | No | 1 |
| 5 | 58/F | Tetrapraresis/many years | No | CCJ | No | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the entire cervical cord | Ascending cervical artery of ECA, VA, ophthalmic artery | PMV | Type V | TAE with PVA and silk thread | Incompletely | 4 years | No | 4 or 5 | |
| 6 | Chen et al. (2) | 47/M | Tetrapareis, paresthesia, urinary retention/1 year | No | Torcular | No | NA/NM, NA/NM | NA/NM | NA/NM | NA/NM, NA/NM | Yes | Hypoer medulla oblongata extending to the upper cervical cord | Meningeal branch of the VA | Cerebellar vein → veins of the hypoer brainstem → PMV | Type V | Open surgery | Completely | 2 months | No | 4 or 5 |
| 7 | Ricolfi et al. (8) | 53/M | Paraparesis, paresthesia, urinary retention/several months | No | Tentorium | No | Hypo, non-enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Hypoer medulla oblongata extending to the upper cervical cord | MHT of the ICA, MMA | Lateral pontomesencephalic veins → cervical and thoracic PMV | Type V | TAE with NBCA via MMA and occluding ICA | Incompletely | 2 years | Yes/ coagulated the draining veins | 1 or 2 |
| 8 | 40/F | Tetrapareis, sphincter disturbance, bulbar signs/1 year | No | CS | No | Hypo, non-enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Hypoer medulla oblongata extending to the upper cervical cord | MHT of the ICA, MMA, sphenopalatine artery and AphA | Superior ophthalmic vein and SPS → lateral mesencephalic veins → PMV | Type V | TAE with NBCA via MMA and sphenopalatine arteries, with PVA particles via APhA | Completely | 5 days | No | Dead | |
| 9 | 75/M | Tetraplegia, sphincter disturbance, bulbar signs, dysautonomia/a few days | No | SPS | Yes | Hypo, non-enhanced | Hyper | NA/NM | NA/NM, NA/NM | No | Hypoer pons and medulla oblongata extending to the upper cervical cord | MMA | PMV | Type V | TAE with NBCA via MMA | Completely | 5 years | No | 0 | |
| 10 | 51/F | Paraparesis, sphincter disturbance, bulbar signs, dysautonomia/3 months | Yes (initial negative) | SS | Yes | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the upper cervical cord | OA, MMA | Lateral medullary vein → PMV | Type V | TAE with NBCA via MMA and OA | Completely | 1 year | No | 0 | |
| 11 | Bousson et al. (9) | 36/M | Tetrapraresis, paresthesia/4 months | No | Tentorium | No | NA/NM, intensely enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the entire cervical cord | OA | Vein around brainstem → PMV | Type V | TAE to occlude the OA | Incompletely | 2 weeks | No | NA/NM |
| 12 | Hurst et al. (10) | 54/M | Tetrapraresis/ NA/NM | No | CCJ | No | NA/NM, enhanced | Hyper | NA/NM | NA/NM/ NA/NM | Yes | Hypoer medulla oblongata extending to the upper cervical cord | Dural branch of VA | PMV | Type V | TAE with PVA via the dural branch of VA | Completely | 3 months | No | 3 |
| 13 | 50/M | Tetrapraresis, pain, hypoer CN deficits/ NA/NM | No | CCJ | No | Hypo/ NA/NM | Hyper | NA/NM | NA/NM/ NA/NM | Yes | Hypoer medulla oblongata extending to the upper cervical cord | AphA | PMV | Type V | TAE with polyvinyl alcohol via APhA | Completely | 12 months | No | 4 | |
| 14 | Takahashi et al. (11) | 49/M | Diplopia, vertigo/3 weeks | No | CS | Yes | Hypo, enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Pons and cerebellar hemisphere | MHT of the ICA | SPS → ophthalmic vein, petrosal vein → cortical venous reflux | Type IIA+B | TVE with coils | Completely | 3 months | No | 0 or 1 |
| 15 | 62/F | Loss of visual acuity, chemosis, exophthalmos/ NA/NM | No | CS | No | Hypo, markedly enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Pons and medulla oblongata | Branches of bilateral ECA and ICA | CS → superior ophthalmic vein | Type IIA+B | TVE with coils | Completely | 1 month | No | 2 | |
| 16 | Shintani et al. (12) | 65/F | Chemosis, CN (III, IV, VI) palsy, vertigo/8 months | No | CS | No | Hypo, markedly enhanced | Hyper | NA/NM | NA/NM, NA/NM | No | Pons | Branches of ICA | IPS | NA/NM | NA/NM | NA/NM | NA/NM | NA/NM | Dead |
| 17 | Wiesmann et al. (13) | 46/M | Paraparesis, dysarthria, urinary incontinence/4 days | No | CCJ | Yes | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | No | Pontomedullary region | NMB of AphA | Anterior median pontine and anterior medullary veins → anterior and posterior spinal veins | Type V | TAE with NBCA via AphA | Completely | 12 months | No | 1 |
| 18 | Kalamangalam et al. (14) | 68/M | Paraparesis, urinary incontinence/4 months | Yes (stroke) | CCJ (Clivus) | No | Normal, non-enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Hypoer medulla oblongata extending to the entire cervical cord | MHT of the ICA | Veins around brainstem → PMV of cervical spinal cord | Type V | Surgical clipping draining vein | Completely | 4 months | No | 3 |
| 19 | Weigele et al. (15) | 53/M | Cranial neuropathies, hemidysesthesia, and personality changes/several months | Yes (brainstem glioma) | Galen vein | No | Normal, non-enhanced | Hyper | Hyper | NA/NM, NA/NM | Yes | Pons, midbrain, and thalamus | MMA, NMB of AphA, marginal artery, vermin branch of SCA | Pontomedullary and anterior cortical veins → superior sagittal sinus | Type IV | TAE with NBCA via MMA and AphA | Completely | 6 months | No | 0 |
| 20 | Asakawa et al. (16) | 64/M | Tetrapraresis, urinary incontinence, respiratory insufficiency/2 weeks | No | CCJ (foramen magnum) | No | Hypo, enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Hypoer medulla oblongata extending to the upper thoracic cord | AphA | Spinal veins | Type V | Combined TAE and surgical interruption | Completely | 3 months | No | 4 |
| 21 | Lanz et al. (17) | 68/F | Diplopia, dysarthria, syncope, transient Paraparesis, respiratory insufficiency/1 year | No | SS | Yes | Normal, non-enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the upper cervical cord | MMA | SS → vein around brainstem → PMV | Type V | TAE with NBCA via MMA | Completely | NM | No | 0 |
| 22 | Kai et al. (18) | 56/F | Proptosis, double vision, visual disturbance, hemiparesis/2 weeks | No | CS | No | NA/NM, moderately enhanced | Hyper | NA/NM | NA/NM, NA/NM | No | Brainstem | Branches of the ECA | Petrosal vein → cerebellar veins | Type IIA+B | TVE via petrosal vein cannulation with coils | Incompletely | 1 month | No | 3 |
| 23 | 70/F | Double vision, chemosis, exophthalmos, ataxia/2 months | No | CS | Yes | Normal, non-enhanced | Hyper | NA/NM | NA/NM, NA/NM | No | Midbrain | Dural branches of the bilateral ICAs and ECAs | Sphenoparietal sinus → deep sylvian vein → pontomesencephalic veins | Type IIA+B | Packing of CS with sponges via open surgery | Completely | 1 months | No | 0 | |
| 24 | Li et al. (19) | 73/M | Tetrapraresis, unconsciousness and dyspnea/1 year | Yes (acute cerebral infarction) | TS | Yes | NA/NM, NA/NM | Hyper | Hyper | NA/NM, NA/NM | Yes | Temporal lobe and medulla oblongata extending to the upper thoracic cord | MMA, OA, AphA | Cortical vein, stenotic TS → anterior and posterior spinal vein | Type V | TVE with coiling the TS | Completely | 5 days | No | NA/NM |
| 25 | Pannu et al. (20) | 42/M | Tetrapraresis, bowel and urinary incontinence/1 year | No | Tentorium | No | NA/NM, NA/NM | Hyper | Hyper | NA/NM, NA/NM | Yes | Medulla oblongata extending to the upper cervical cord | MHT of the ICA | Superior petrosal vein → lateral medullary vein → the anterior and posterior spinal veins | Type V | Coagulating DAVF and draining vein | Completely | 12 months | No | 3 |
| 26 | Crum et al. (21) | 35/M | Paraparesis, ataxia, diplopia/several weeks | Yes (uncertain brainstem lesion) | CCJ (jugular foramen) | No | Normal, patchy enhancement | Hyper | Hyper | NA/NM, NA/NM | Yes | Medulla oblongata extending to the upper cervical cord | Branches of the VA and PICA | Spinal medullary veins | Type V | Coagulated and divided the DAVF and draining vein | Completely | 3 months | No | 1 |
| 27 | Oishi et al. (22) | 68/F | Disturbance of brainstem function/NA/NM | NA/NM | TS | NA/NM | NA/NM, NA/NM | Hyper | Hyper | NA/NM, NA/NM | Yes | Medulla oblongata | NA/NM | SPS → spinal PMV | Type V | TVE with coils | Completely | NA/NM | No | NA/NM |
| 28 | Satoh et al. (23) | 38/F | Tetrapraresis, nystagmus, Horner syndrome/NA/NM | No | TS-SS | Yes | Hypo, NA/NM | Hyper | Hyper | NA/NM, NA/NM | No | Medulla oblongata | MMA, OA, AphA, MHT of the ICA, PMA of the VA | SS → spinal PMV | Type V | TVE with coiling the SS | Completely | 1 month | No | 3 |
| 29 | Tanoue et al. (3) | 70/M | Tetrapraresis, sensory disturbance/2 years | No | CCJ (foramen magnum) | No | Normal, non-enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the entire cervical cord | Jugular branch of OA, NMH of AphA | Anterior condylar vein → inferior petrosal sinus → pontomesencephalic vein → anterior spinal vein | Type V | TAE with NBCA via AphA and OA | Incompletely | 14 months | No | 4 or 5 |
| 30 | Akkoc et al. (24) | 45/M | Paraparesis, urinary retention/2 months | Yes (brainstem ischemia or myelitis) | CCJ | No | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the entire cervical cord | OA, NMH of AphA | PMV | Type V | TAE with NBCA via OA | Completely | 3 months | Yes/repeated TAE with NBCA via AphA | 4 or 5 |
| 31 | Iwasaki et al. (25) | 71/F | Decreased abduction of the right eye/5 months | Yes (brain neoplasm) | CS | No | Normal, patchy-enhancement | Hyper | NA/NM | NA/NM, NA/NM | No | Upper pons | MMA, meningeal branch of the ICA | SPS → straight sinus → cerebellar cortical veins → anterior pontomesencephalic vein → PMV | Type V | Stereotactic radiosurgery | Completely | 3 years | No | 0 |
| 32 | Lagares et al. (26) | 65/M | Tetrapraresis, respiratory insufficiency/3 months | Yes (cerebellar infarction) | Torcular | No | NA/NM, NA/NM | Hyper | Hyper | Hypo, hyper | Yes | Medulla oblongata | OA, PMA of the VA | Cerebellar vein → petrosal vein and PMV | Type V | Open surgery | Completely | 6 months | No | 1 |
| 33 | van Rooij et al. (27) | 58/M | Tetrapraresis, bladder retention/3 months | Yes (NA/NM) | Tentorium | No | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the entire cervical cord | MHT of the ICA, MMA, AphA | Petrosal vein → PMV | Type V | TAE with NBCA via MMA | Completely | 1 years | No | 0 |
| 34 | 72/F | Tetrapraresis, paresthesias, bladder retention/2 years | Yes (NA/NM) | CCJ (foramen magnum) | No | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the middle thoracic cord | OA | PMV | Type V | TAE with NBCA via OA | Completely | 2 years | No | 4 or 5 | |
| 35 | Sakamoto et al. (28) | 65/F | Progressive mental and gait disturbance/1 month | No | TS-SS | Yes | Hypo, NA/NM | Hyper | NA/NM | Hetero-geneous, hyper | No | Brainstem and cerebellum | OA, NMH of AphA, posterior branch of MMA, anterior and posterior auricular arteries | NA/NM | TypeIIB | TVE with coils | Completely | NA/NM | No | 0 |
| 36 | Tsutsumi et al. (29) | 62/F | Tetraparesis, occipitalgia and bulbar symptoms/1 year | Yes (intramedullary glioma) | CCJ (foramen magnum) | No | Hypo, rim-like enhancement | Hyper | NA/NM | NA/NM, NA/NM | No | Medulla oblongata extending to the upper thoracic cord | NMH of AphA, meningeal branch of OA | Retrograde drainage to the inferior petrosal sinus → cavernous sinuses | Type IIA | TVE with coils | Completely | Immediately | No | NA/NM |
| 37 | Sugiura et al. (30) | 69/F | Vomiting, ataxia and weakness/2 months | No | SS | Yes | NA/NM, patchy-enhancement | Hyper | NA/NM | Normal, hyper | Yes | Medulla oblongata and hypoer pons | OA | Veins around brainstem → spinal PMV | Type V | TVE with coiling the SS | Completely | 3 weeks | No | 4 or 5 |
| 38 | Wang et al. (31) | 68/M | Focal motor deficit/ NA/NM | NA/NM | CCJ (foramen magnum) | No | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata | NMB of AphA | PMV and anteromedullary cervical veins | Type V | TAE with NBCA via AphA | Completely | 2 years | No | 4 or 5 |
| 39 | Khan et al. (32) | 20/F | Tetrapraresis, urinary retention and respiratory distress/1 month | Yes (demyelinating disease) | Tentorium | No | NA/NM, non-enhanced | Hyper | Hyper | NA/NM, NA/NM | Yes | Pons extending to the upper cervical cord | MHT of the ICA | Cerebellar vein and anterior spinal vein | Type V | Open surgery | Completely | 3 months | No | 3 |
| 40 | Ko et al. (33) | 54/M | Tetrapraresis, hypesthesia, diplopia/5 years | Yes (Tolosa-Hunt syndrome) | CS | No | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the upper cervical cord | MHT of the ICA, MMA | Pontomesencephalic vein → cervical PMV | Type V | TAE with NBCA via multiple feeders | Incompletely | 10 months | Yes/Second-stage embolization and gamma-knife radiosurgery | 4 or 5 |
| 41 | Kleeberg et al. (34) | 60/M | Difficulty to walk/6 weeks | No | Tentorium | No | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the hypoer cervical cord | MHT of the ICA | Cerebellar vein → PMV | Type V | Combined TAE and open surgery | Completely | Immediately | No | 1 or 2 |
| 42 | Patsalides et al. (35) | 53/M | Syncope attacks and tingling of the fingertips/3 months | Yes (NA/NM) | SPS | Yes | NA/NM, enhanced | Hyper | NA/NM | NA/NM, NA/NM | No | Medulla oblongata extending to the upper cervical cord | MHT of the ICA, MMA | Veins around brainstem → spinal veins | Type V | TAE with NBCA via MHT of the ICA | Completely | 6 months | No | 0 |
| 43 | Aixut Lorenzo et al. (36) | 67/F | Neck pain, Tetrapraresis, urinary retention/several days | No | Tentorium (petrosal ridge) | Yes | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the entire cervical cord | MMA, AphA, and OA | Vein around brainstem → spinal PMV | Type V | TAE with Onyx via OA | Completely | 12 months | Yes/TVE | 0 or 1 |
| 44 | Kim et al. (37) | 45/M | Tetrapraresis and respiratory distress/6 months | Yes (demyelinating disease) | Tentorium (petrosal ridge) | No | NA/NM, enhanced | Hyper | Hyper | Normal, NA/NM | No | Medulla oblongata extending to the upper cervical cord | Meningeal branches of bilateral ICAs | Cervical PMV | Type V | Open surgery | Completely | 2 weeks | No | 3 |
| 45 | Peltier et al. (38) | 58/F | Tetrapraresis, urinary retention and breathing difficulty/2 months | No | CCJ | No | NA/NM, enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the upper cervical cord | PMA of the VA | C1 radiculomedullary vein | Type V | Clipping and section of the venous stem | Completely | 6 months | No | 3 |
| 46 | Clark et al. (39) | 49/F | Dysarthric with monotonal hypophonia and ataxia/3 months | No | CS | No | NA/NM, NA/NM | Hyper | Hyper | NA/NM, NA/NM | Yes | Pons extending to the upper cervical cord | MHT of the ICA | NA/NM | NA/NM | TAE to coil the DAVF | Completely | 10 days | No | 2 or 3 |
| 47 | Ogbonnaya et al. (40) | 64/F | Paraparesis, unsteady gait/3 months | No | Tentorium | No | NA/NM, non-enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the upper cervical cord | MMA | PMV | Type V | TAE | Completely | Immediately | No | 4 or 5 |
| 48 | Kulwin et al. (41) | 44/F | Paraparesis, altered mental status, hypopneic/ NA/NM | Yes (brainstem stroke) | SPS | No | NA/NM, enhanced | NA/NM | Hyper | NA/NM, hyper | No | Pons and medulla oblongata | MMA, dural branch of VA | SPS → perimesencephalic vein → PMV | Type V | Surgical disconnection by clipping draining vein | Completely | Immediately | No | 4 or 5 |
| 49 | Clark et al. (42) | 65/F | Tetrapraresis, gastroenteritis, urinary retention/several days | No | SPS | No | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | No | Medulla oblongata and upper cervical spinal cord | MMA, MHT of the ICA | veins around brainstem → PMV | Type V | Combined TAE and surgical obliteration | Completely | Immediately | No | NA/NM |
| 50 | Mathon et al. (43) | 60/F | Progressive ascending myelopathy associated with autonomic dysfunction/NA/NM | No | SPS | No | NA/NM, NA/NM | Hyper | Hyper | NA/NM, NA/NM | Yes | medulla oblongata with cervical spinal cord, | Meningeal arteries of the posterior surface of the internal carotid artery, MMA | Dilated perimedullary veins. | Type V | TAE with glue via MMA | Completely | 1 month | No | 0 |
| 51 | Salamon et al. (44) | 43/M | Paraparesis, urinary retention, vomiting, hiccups/NA/NM | No | CCJ (foramen magnum) | No | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Hypoer medulla oblongata extending to the upper cervical cord | Meningeal branch from the VA | Cerebellar veins → venous drainage along the medulla → PMV | Type V | TAE with Onyx | Completely | 3 months | No | 0 |
| 52 | Singh et al. (45) | Middle-aged/M | Paraparesis, urinary retention, vomiting, hiccups/4 months | Yes (periodic paralysis) | Tentorium | No | NA/NM, NA/NM | Hyper | Hyper | NA/NM, NA/NM | Yes | Pons, medulla oblongata extending to the upper cervical cord | MHAs of the ICAs, MMA | Perimesencephalic vein and PMV | Type V | Open surgery | Completely | 3 months | No | 0 |
| 53 | El Asri et al. (46) | 48/M | Tetrapraresis, hypaesthesia, breathing difficulty/10 days | No | Tentorium | No | NA/NM, non-enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Hypoer medulla oblongata extending to the upper cervical cord | MHT of the ICA | Cerebellar veins → PMV | Type V | Open surgery | Completely | 2 years | No | 4 or 5 |
| 54 | Foreman et al. (47) | 59/F | Tetrapraresis, pain, urinary retention/3 weeks | Yes (infarction or contusion) | CCJ | No | NA/NM, non-enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata and entire cervical spinal cord | MHT of the ICA | Pontomesencephalic vein → PMV | Type V | Open surgery | Completely | Immediately | No | 4 or 5 |
| 55 | Gross et al. (48) | 69/M | Progressive hypoer extremity weakness and urinary retention/3 days | Yes (Guillian-Barre syndrome) | Tentorium | No | NA/NM, NA/NM | Hyper | Hyper | NA/NM, NA/NM | Yes | Pons, medulla, and upper cervical spine | MMA, tentorial branch of ICA, dural branches of OA and posterior auricular artery | Cervical spinal veins | Type V | TAE with Onyx | Completely | 10 weeks | No | 3 |
| 56 | 34/F | Progressive extremity weakness/1 week | Yes (transverse myelitis) | TS-SS | No | NA/NM, NA/NM | Hyper | Hyper | NA/NM, NA/NM | Yes | Brainstem and cervicomedullary junction | OA | SPS → petrosal vein and medullary vein → anterior spinal vein and cervicomedullary vein | Type V | TAE with Onyx | Completely | 3 months | No | 0 | |
| 57 | Wu et al. (49) | 46/F | Paraparesis, vertigo, vomiting and dysphagia/1 month | Yes (brainstem infarction) | CCJ | No | NA/NM, partial enhancement | Hyper | Hyper | NA/NM, NA/NM | Yes | Pons, medulla oblongata. | Meningeal branch from the radicular artery of the VA | Pontomesencephalic veins → basal vein and anterior spinal vein | Type V | TAE with Onyx | Completely | 6 months | No | 0 |
| 58 | Haryu et al. (50) | 62/M | Upper limb weakness and difficulty in walking/4 months | NA/NM | Tentorium (petrosal ridge) | NA/NM | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Cervical spinal cord and medulla oblongata | MMA | Petrosal vein into the anterior spinal veins | Type V | Open surgery | Completely | 18 months | No | 2 |
| 59 | 64/M | Myelopathy, bulbar palsy/NA/NM | Yes (NA/NM) | NA/NM | NA/NM | NA/NM, heterogeneously enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Cervical spinal cord and medulla oblongata | NA/NM | Spinal veins | Type V | NA/NM | NA/NM | NA/NM | NA/NM | 3 | |
| 60 | 68/M | Myelopathy, respiratory failure/NA/NM | NA/NM | NA/NM | NA/NM | NA/NM, non-enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Cervical spinal cord and medulla oblongata | AphA | Anterior spinal veins | Type V | Open surgery | NA/NM | NA/NM | NA/NM | 4 | |
| 61 | Roelz et al. (51) | 76/M | Nausea and vomiting, inability to walk, and blurred vision/8 months | Yes (brainstem glioma or lymphoma) | CCJ (Posterior jugular foramen) | No | NA/NM, enhanced | Hyper | Hyper | NA/NM, NA/NM | Yes | Pontomedullary junction extending to inferior cerebellar peduncle | MMA, AphA, PAA, and OA | Lateral medullary into the anterior perimedullary/perispinal veins | Type V | TAE with Onyx via MMA, AphA, PAA | Completely | 10 months | Yes/combined endovascular (via OA) and surgical approach | 2 |
| 62 | Le et al. (52) | 36/M | Headache, hypoesthesia, vomiting, ataxia/2 months | Yes (brainstem glioma) | Tentorium (petrosal apex) | No | Normal, punctiform enhancement | Hyper | Hyper | NA/NM, NA/NM | Yes | Medulla oblongata | MMAs, AphA, internal maxillary artery | Spinal PMV | Type V | TAE with NBCA | Completely | 1 year | No | 0 |
| 63 | Alvare et al. (53) | 69/M | Nausea, vomiting, paraparesis/NA/NM | Yes (encephalitis) | Tentorium (petrosal ridge) | No | NA/NM, enhanced | Hyper | Hyper | Normal, hyper | No | Pons and medulla oblongata | MMA, anterior inferior cerebellar artery | Veins of the cerebello-pontine angle → veins around the brainstem → spinal PMV | Type V | Combined TAE and clip and coagulate the draining vein | Completely | 3 months | No | 0 |
| 64 | Pop et al. (54) | 38/M | Seizure, tetraplegia, respiratory difficulty/1 month | Yes (Guillain-Barre syndrome) | CCJ (foramen magnum) | No | Low, non-enhanced | Hyper | Hyper | NA/NM, NA/NM | Yes | Medulla oblongata extending to the entire cervical cord | OA, AphA | Bidirectional drainage to cortical temporal vein and spinal veins | Type V | TAE with Onyx via OA | Completely | 6 months | No | 3 |
| 65 | Abud et al. (55) | 66/F | Tetraparesis/1 month | No | SS | No | NA/NM, non-enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the upper cervical cord | OA | Cerebellar cortical venous drainage → PMV | Type V | TAE with Onyx via OA | Completely | 3 months | No | 0 |
| 66 | Abdelsadg et al. (56) | 65/F | Tetraparesis, dizziness, urination difficulty/several days | No | CCJ | Yes | NA/NM, NA/NM | Hyper | Hyper | NA/NM, Hyper | No | Medulla oblongata extending to the upper cervical cord | MHT of the ICA, MMA, | SPS → brainstem and cervical PMV | Type V | TAE | Completely | 3 months | No | 3 |
| 67 | Enokizono et al. (57) | 50s/F | Tetraparesis, numbness of limbs, urination difficulty/1 month | No | CCJ | No | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the upper thoracic cord | Meningeal branch from the radicular artery of the VA | Anterior and posterior spinal veins | Type V | Open surgery | Completely | NA/NM | No | NA/NM |
| 68 | 60s/M | Tetraparesis, numbness of limbs, urination difficulty/7 months | No | Tentorium | No | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the upper thoracic cord | MHT of the ICA, MMA, accessory meningeal artery | Petrosal vein → veins around the brainstem → PMV | Type V | Open surgery | Completely | NA/NM | No | NA/NM | |
| 69 | 60s/M | Tetraparesis, numbness of limbs, respiratory difficulty/2 months | No | Tentorium | No | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the entire cervical cord | MMA | Petrosal vein → veins around the brainstem → PMV | Type V | Combined TAE and clip the draining vein | Completely | NA/NM | No | NA/NM | |
| 70 | Tanaka et al. (58) | 64/M | Paraparesis, bladder dysfunction/NA/NM | No | Occipital sinus | Yes | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | No | Medulla oblongata extending to the upper cervical cord | PMAs of the VAs | Occipital sinus → anterior spinal vein | Type V | TAE with Onyx via PMAs of the VAs | Completely | 8 months | No | 2 |
| 71 | Emmer et al. (59) | 65/M | Eye movement abnormalities, limb weakness, and gait instability/2 years | Yes (tumor) | CCJ | No | NA/NM, heterogeneously enhanced | Hyper | Hyper | NA/NM, NA/NM | Yes | Medulla oblongata and cerebellum | PMA of the VA | Cerebellar vein | Type III | TAE with NBCA via PMA | Completely | Immediately | No | 4 or 5 |
| 72 | Duan et al. (60) | 67/F | Paraparesis, headache and progressive Confusion/1 month | Yes (brainstem tumor) | SPS | No | NA/NM, partially enhanced | Hyper | Hyper | Hyper, NA/NM | No | Cerebellum and pons | MMA, OA | SPS → PMV | Type V | TAE | Completely | Immediately | No | 4 or 5 |
| 73 | Chen et al. (61) | 25/F | Paresthesias and paralysis of hypoer extremity, dyspnea/several days | Yes (encephalitis and myelitis) | Posterior fossa | No | NA/NM, enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Pons to C2/C3 | Posterior meningeal branch of VA | Anterior spinal vein | Type V | TAE | Completely | NA/NM | No | NA/NM |
| 74 | Bernard et al. (62) | 65/M | Progressive ataxia, swalhypoing dnormalrders, and bilateral tinnitus/5 months | Yes (glioma) | CCJ | No | NA/NM, enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla and hyper cervical cord | Branches of AphA | Cerebellar medullary vein (white arrowhead) reaching perimedullary veins | Type V | Open surgery | Completely | 1 month | No | 0 |
| 75 | Zhang et al. (4) | 33/M | Progressive weakness of the hypoer extremities and gait disturbance/2 months | Yes (transverse myelitis) | Tentorium | No | NA/NM, patchy enhancement | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata and cervical spinal cord | MHT of ICA | Perimedullary veins | Type V | TAE with Onyx | Completely | 1 month | No | 2 |
| 76 | Li et al. (63) | 54/F | Limb weakness and sphincter dysfunction/20 days | No | Tentorium (petrosal apex) | No | NA/NM, non- enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata and cervical spinal cord | MHT of ICA | Medullary into the perimedullary | Type V | Open surgery | Completely | 1 month | No | 1 |
| 77 | Wang et al. (64) | 53/M | Numbness of the limbs, gait disturbance and cough/NA/NM | No | CCJ | No | NA/NM, patchy enhancement | Hyper | Hyper | Hyper, NA/NM | Yes | Pons to medulla oblongata | OA of the VA | SS and cortical venous drainage | Type IIB | TAE with Onyx via OA | Completely | Immediately | No | 3 |
| 78 | 53/M | Tetrapraresis, hypaesthesia, swalhypoing difficulty/2 months | No | CCJ | No | Low, non- enhanced | Hyper | Hyper | Normal, NA/NM | Yes | Medulla oblongata | Dural branch of VA | Posterior spinal veins | Type V | Coagulating and cutting draining veins | Completely | Immediately | No | 4 or 5 | |
| 79 | Takahashi et al. (65) | 63/M | Tetraparesis, respiratory failure/5 months | No | CCJ | No | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata | OA, AphA | Anterior spinal vein | Type V | TAE | Completely | 2 months | No | 3 |
| 80 | Copelan et al. (66) | 59/M | Dizziness, nausea, and vomiting, vertigo/5 weeks | No | SPS | No | NA/NM, mild patchy enhancement | Hyper | Hyper | Mild hyper, hyper | Yes | Medulla oblongata extending to the upper cervical cord | MMA, OA, AphA | Petrosal vein → PMV | Type V | Combination of endovascular embolization and surgical resection | Completely | 3 years | No | 1 or 2 |
| 81 | 72/M | Slurred speech, and dysphagia/3 months | No | CCJ (anterior condylar vein) | No | NA/NM, enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata and cerebellar flocculus | AphA | Anterior condylar vein, petrosal vein and PMV | Type V | TAE with Onyx via AphA | Completely | 5 months | No | 1 or 2 | |
| 82 | 35/F | Progressive unsteady gait and paraparesis/1 month | No | SPS | No | NA/NM, mildly enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata | OA | SPS → PMV | Type V | TAE with Onyx | Completely | 3months | No | 2 | |
| 83 | 64/M | Tetraparesis/6 months | Yes (transverse myelitis) | SPS | No | NA/NM, enhanced | Hyper | NA/NM | NA/NM, NA/NM | Yes | Medulla oblongata extending to the upper cervical cord | MHT of ICA, OA | PMV | Type V | TAE and surgical resection | Completely | 12 months | No | 4 or 5 | |
| 84 | Rodriguez et al. (67) | 68/M | Progressive hypoer extremity weakness/NA/NM | No | Tentorium | No | NA/NM, NA/NM | NA/NM | NA/NM | NA/NM, NA/NM | No | Cervicomedullary junction to C7 | PMA | Doral and ventral perimedullary veins | Type V | TAE with 50% ethanol | Incompletely | NA/NM | Yes/open surgery | 3 |
| 85 | Shimizu et al. (68) | 75/M | Paraparesis, hypaesthesia, urinary retention/6 months | No | Anterior cranial fossa | Yes | NA/NM, NA/NM | Hyper | NA/NM | NA/NM, NA/NM | Yes | Cerebellum and hypoer pons extending to the upper cervical cord | Anterior ethmoidal artery | Olfactory vein → basal vein of Rosenthal → veins around the brainstem → PMV | Type V | Open surgery | Completely | 2 months | No | 4 or 5 |
| 86 | Chen et al. (69) | 66/M | Dizziness, truncal ataxia, impaired gait/1 month | Yes (NA/NM) | CCJ | No | NA/NM, partially enhanced | Hyper | NA/NM | Normal, hyper | Yes | Hypoer pons and medulla oblongata | OA, meningeal branch of VA | PMV, reflux into veins around the brainstem | Type V | TAE with Onyx | Completely | 3 months | No | 1 or 2 |
CCJ, cranio-cervical junction; CS, cavernous sinus; DAVF, dural arteriovenous fistula; ECA, external carotid artery; F, female; ICA, internal carotid artery; M, male; MHT, meningohypophysal trunk; MMA, middle meningeal; AphA, ascending pharyngeal artery; VA, vertebral artery; MRI, magnetic resonance imaging; mRS, modified Rankin scale; NA/NM, not applicable/not mentioned; NBCA, N-butyl-2-cyanoacrylate; NMB, neuromeningeal branch; OA, occipital artery; PAA, posterior auricular artery; PMA, posterior meningeal artery; PMV, perimedullary vein; PVA, polyvinyl alcohol; SPS, superior petrosal sinus; SS, sigmoid sinus; TAE, transarterial embolization; TS, transverse sinus; TVE, transvenous embolization; VA, vertebral artery.
Figure 2.
Flow chart of the searching strategy.
Interval From Symptom Onset to Definite Diagnosis
Of the 68 cases interval from symptom onset to definite diagnosis was provided, 15 (22.1%, 15/68) patients were definitely diagnosed with intracranial DAVFs in the 1st month since symptom onset. Nineteen (28.0%, 19/68) patients were definitely diagnosed between the 2nd and 3rd months. Sixteen (23.5%, 16/68) patients were between the fourth and 6th month. Six (8.8%, 6/68) patients were between the seventh and twelfth month. Twelve (17.6%, 12/68) patients were definitely diagnosed 1 year later from symptom onset. Thirty-three (40.2%, 33/82) patients were initially misdiagnosed as other diseases.
DAVFs Characteristics
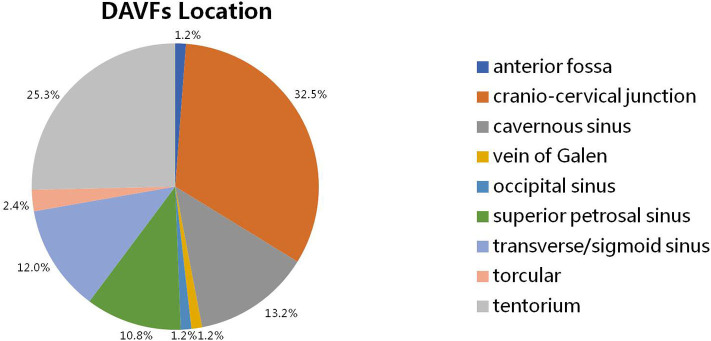
The intracranial location of DAVFs could be determined in 83 patients. The specific location distributions were anterior fossa, cranio-cervical junction, cavernous sinus, vein of Galen, occipital sinus, superior petrosal sinus, transverse/sigmoid sinus, torcular, and tentorium in 1 (1.2%), 27 (32.5%), 11 (13.2%), 1 (1.2%), 1 (1.2%), 9 (10.8%), 10 (12.0%), 2 (2.4%), and 21 (25.3%) patients, respectively (Figure 3). The Cognard classification of DAVFs were II, III, IV, and V in 9 (10.7%, 9/84), 1 (1.2%, 1/84), 1 (1.2%, 1/84), and 73 (86.9%, 73/84) patients (Figure 4). The feeding arteries were solely from the external carotid artery (ECA) in 32 (38.6%, 32/83) patients, solely from the internal carotid artery (ICA) in 14 (16.9%, 14/83) patients, solely from the vertebrobasilar artery (VBA) in 12 (14.5%, 12/83) patients, conjointly from ECA and ICA in 18 (21.7%, 18/83) patients, conjointly from ECA and VBA in 5 (6.0%, 5/83) patients, and conjointly from ECA, ICA, and VBA in 2 (2.4%, 2/83) patients.
Figure 3.
The specific location of intracranial DAVFs complicated with brainstem engorgement. DAVF, dural arteriovenous fistula.
Figure 4.
The Cognard classification of intracranial DAVFs complicated with brainstem engorgement. DAVF, dural arteriovenous fistula.
Findings on Imaging Modalities
Eighteen (22%, 18/82) patients were demonstrated to have stenosis or occlusion of the draining system distal to the fistula points during conventional angiography. The signals of the engorged brainstem were hypointense or normal on T1 weighted imaging (T1WI) of magnetic resonance imaging (MRI) in 15 (65.2%, 15/23) and 8 (34.8%, 8/23) patients, respectively. The engorged brainstem was enhanced on T1WI with different degrees in 37 (72.5%, 37/51) patients after gadolinium contrast. The signal was hyperintense in all of the 82 patients T2 weighted imaging (T2WI) sequence was provided. And the signal was also hyperintense for all of the 25 patients who had undergone fluid attenuated inversion recovery (FLAIR) sequence. The signals on diffusion weighted imaging (DWI) were heterogeneous, hyperintense, hypointense, and normal in 1 (10%), 3 (30%), 1 (10%), and 5 (50%) patients, respectively. All of the six patients showed hyperintensity on apparent diffusion coefficient (ADC) map. Besides, abnormal vascular flow voids could be identified in 69 (80.2%, 69/86) patients on MRI.
Treatment and Outcome
Forty-five (53.6%, 45/84) patients were treated solely with transarterial embolization, of which 7 (15.6%, 7/45) patients were incompletely embolized and 3 (6.7%, 3/45) patients experienced recurrence in spite of previous complete obliteration. Eight (9.5%, 8/84) patients underwent transvenous embolization, of which 1 (12.5%, 1/8) patient was incompletely embolized. Twenty-two (26.2%, 22/84) patients underwent open surgery, of which no recurrence was reported. One (1.2%, 1/84) patient underwent one-session successful stereotactic radiosurgery. Eight (9.5%, 8/84) patients were successfully treated conjointly with the endovascular and open surgical approaches. In general, the DAVFs were completely obliterated in 74 (89.2%, 74/83) patients during one hospitalization. Six (7.2%, 6/83) patients underwent retreatment. The mean follow-up period was 7.86 (n = 74, range 0–60 months) months. Fifty-four (70.1%, 54/77) patients experienced a good recovery according to the mRS score.
Discussion
The pathophysiology of intracranial DAVFs is still enigmatic. Though a small proportion of the DAVFs are demonstrated to be secondary to trauma, craniotomy, infection, or dural venous thrombosis, a substantial number of them are idiopathic (70). Some authors believe that progressive stenosis or thrombosis of the dural venous sinus might be the underlying mechanism of DAVF formation (61, 70). In this review, 22% of the patients with brainstem engorgement were definitely recorded to have stenosis or occlusion of the draining system distal to the fistula points. The actual occurrence of stenosis or occlusion of the draining system might be higher, as some reports did not give a detailed description of the draining system. According to a study by Luo et al. 7 (77.8%) of the nine patients with aggressive cavernous sinus DAVFs had inferior petrous sinus occlusion or stenosis, two patients (22.2%) had compartment of inferior petrous sinus-cavernous sinus (77). Hence, progressive insufficient drainage (stenosis, occlusion, or compartment) of the draining system might play an important role in the genesis of brainstem engorgement in patients with intracranial DAVFs.
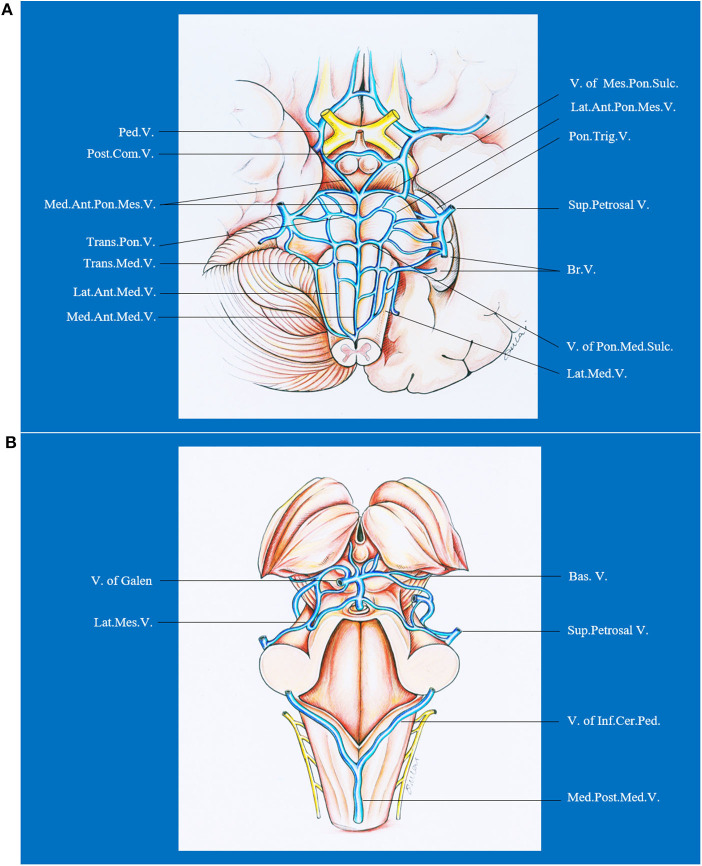
The brainstem has a complex venous draining system. In general, the veins of the brainstem can be divided into the transverse and longitudinal groups, which are named on the basis of the subdivision (mesencephalon, pons, or medulla), surface (median anterior, lateral anterior, or lateral), and the direction (transverse or longitudinal) of the brainstem drained (71). From cranial to caudal, the transverse groups are peduncular vein, posterior communicating vein, vein of pontomesencephalic sulcus, transverse pontine vein, vein of pontomedullary sulcus, and transverse medullary vein. From median to lateral, the longitudinal groups are median veins (median anterior pontomesencephalic vein, median anterior medullary vein), anterolateral veins (lateral anterior pontomesencephalic vein, lateral anterior medullary vein), and lateral veins (lateral mesencephalic vein, lateral medullary and retro-olivary veins). The veins of the transverse group have extensive anastomoses with those of the longitudinal group. Besides, the terminal end of the veins draining the brainstem and cerebellum form bridging veins that are divided into three groups: (1) a galenic group draining into the vein of Galen; (2) a petrosal group draining into the petrosal sinuses; and (3) a tentorial group draining into the sinuses converging on the torcula. Hence, DAVFs in the posterior fossa or even cavernous sinus could lead to brainstem engorgement. Venous drainage of the brainstem is presented in Figure 5.
Figure 5.
Ventral (A) and dorsal (B) venous drainage of the brainstem. Ant., anterior; Bas., basilar; Br., bridging; Cer., cerebellar; Com., communicating; Inf., inferior; Lat., lateral; Med., median, medullary; Mes., mesencephalic; Ped., peduncle; Pon., pontine; Post., posterior; Sul., sulcus; Sup., superior; Trans., transverse; Trig., trigeminal; V., vein.
The diagnosis of intracranial DAVFs with brainstem engorgement is still challenging. Patients that were diagnosed with neoplasm to undergo brainstem biopsy or given corticosteroids for misdiagnosing as myelitis were not uncommonly reported (4, 51). According to our analysis, 40.2% (33/82) of the patients were initially misdiagnosed as other diseases. Of note, the rate of initial misdiagnosis did not decrease in the past three decades (Figure 6). Considering the unspecific clinical manifestations of intracranial DAVFs with brainstem engorgement, meticulous and comprehensive interpretation of the auxiliary investigations is of utmost importance.
Figure 6.
The state of diagnosis and treatment of intracranial DAVFs complicated with brainstem engorgement in the past three decades.
While conventional angiography is the gold standard for definite diagnosis of intracranial DAVFs, taking good advantage of different sequences of MRI data could help screen out those patients with high suspicion. Abnormal vascular flow voids on MRI are reliable evidence highly suggestive of vascular lesions. Abnormal vascular flow voids could only be identified in 80.2% (69/86) of the patients in this survey, including those identified after repeated review of the MRI or those identified during multiple investigations of MRI after symptom aggravation. T2WI or FLAIR sequence is highly sensitive (in 100% of the patients) for the engorged brainstem but with low specificity. The signals on T1WI are so polytropic that 65.2% (15/23) of the analyzed patients presented with low hypointensity and 34.8% (8/23) of the patients were normal. The engorged brainstem was enhanced on T1WI with different degrees in 72.5% (37/51) of the patients after gadolinium contrast. DWI and ADC were rarely performed in these patients. All of the six patients with ADC map showed hyperintensity which denotes the vascular origin of brainstem edema. The signal of DWI is so variable that heterogeneous, hyper, hypo, and normal intensity could be in 1 (10%), 3 (30%), 1 (10%), and 5 (50%) of the 10 identified patients, which might reflect the different degree and duration of venous congestion around the brainstem. Furthermore, contrast-enhanced dynamic magnetic resonance angiography is more sensitive to find out occult vascular abnormalities (50, 72). T2*WI and susceptibility-weighted imaging are emerging sequences of MRI that are good at detecting fine vasculature and microbleeds (73). Hypointense signal could be noticed in the engorged brainstem on T2*WI and susceptibility-weighted imaging, for long-term venous congestion might lead to intraparenchymal microbleeding in the brainstem (57, 60). Besides, some authors also demonstrated decreased cerebral blood volume and prolongation of the mean transit time on magnetic resonance perfusion in the engorged brainstem (66). Hence, advanced MRI sequences could increase the sensitivity and specificity in differential diagnosis of lesion nature and avoid delayed treatment and unnecessary conventional angiography.
There is no consensus on the treatment option for intracranial DAVFs with brainstem engorgement. Of note, premature administration of corticosteroid could be dangerous even fatal in case of undiagnosed DAVFs with brainstem or spinal cord engorgement (74, 75). Hence, precise and comprehensive diagnosis is crucial for further treatment. The treatment should be based on the specific angioarchitecture, intracranial location, and technique availability. Generally speaking, the treatment strategies for DAVFs include open surgery, endovascular embolization, and radiotherapy. As the lag time of effect could be up to 3 years (76), radiotherapy is unsuitable for patients with brainstem engorgement. With the development of endovascular technique and materials, endovascular embolization has become the first-line choice for the majority of intracranial DAVFs (63, 70). Besides, endovascular treatment can be an adjunctive step of further open surgery. For patients with difficult arterial/venous access, incomplete fistula obliteration, recanalization after embolization, open surgery can be considered. Whereas, in patients where a transfemoral approach is impaired for the tortuosity of feeding arteries or the presence of isolated sinuses, percutaneous or intraoperative puncture of perforating arteries or draining veins and venous sinuses represent a new choice to facilitate distal access to the DAVFs (70, 77). In this review, 63.1% of the patients were treated endovascularly (transarterial or transvenous), 26.2% of the patients underwent open surgery, and 9.5% of the patients were treated conjointly with endovascular and open surgical approaches.
The prognosis of patients with DAVFs associated brainstem engorgement is still unsatisfactory, though slight increase in good recovery could be noted in the past three decades (Figure 3). Only 70% of the patients experienced a good recovery (mRS score ≤ 3). A substantial number of patients can have more or less neurological deficits. Except for the peculiar location of DAVFs, angioarchitecture, and surrounding neural structures, early diagnosis is the most important factor impacting prognosis. According to this review, correct diagnosis could be achieved in only 50% of the patients in the first 3 months after symptom onset. What's more, the rate of initial misdiagnosis did not decrease in the past three decades (Figure 3). Hence, early awareness of this rare entity and efficiently utilizing the up to date investigations are of utmost importance.
Limitations
The opinion of this review was deduced from retrospective review of the published case reports or small case series. The results would be biased by many factors. Firstly, the levels in diagnosis and treatment vary greatly between different centers. Secondly, due to the reporting customs among different authors, a lot of key information was missing. Thirdly, the mean follow-up period was only 7.86 (n = 74, range 0–60 months) months, which could impair the accuracy in outcome assessment. Of note, there were two studies reporting larger case series of DAVFs with brainstem engorgement (63, 77) that were not included in this analysis because so much information was missing according to our inclusion criteria.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Author Contributions
JY contributed to the conception and design of the manuscript. LQ and HL performed literature review. KH and GL wrote the manuscript. KX and JY critically revised the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Funding. This research received funding support from the Ninth Youth Scientific Research Funding of The First Hospital of Jilin University (jdyy92018035).
References
- 1.Kuwayama N. Epidemiologic survey of dural arteriovenous fistulas in japan: clinical frequency and present status of treatment. Acta Neurochir Suppl. (2016) 123:185–8. 10.1007/978-3-319-29887-0_26 [DOI] [PubMed] [Google Scholar]
- 2.Chen CJ, Chen CM, Lin TK. Enhanced cervical MRI in identifying intracranial dural arteriovenous fistulae with spinal perimedullary venous drainage. Neuroradiology. (1998) 40:393–7. 10.1007/s002340050609 [DOI] [PubMed] [Google Scholar]
- 3.Tanoue S, Goto K, Oota S. Endovascular treatment for dural arteriovenous fistula of the anterior condylar vein with unusual venous drainage: report of two cases. AJNR Am J Neuroradiol. (2005) 26:1955–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang S, Liu H, Li J. Cervical myelopathy caused by intracranial dural arteriovenous fistula with acute worsening after steroid administration. World Neurosurg. (2018) 120:328–30. 10.1016/j.wneu.2018.09.029 [DOI] [PubMed] [Google Scholar]
- 5.Probst EN, Christante L, Zeumer H. Brain-stem venous congestion due to a dural arteriovenous fistula in the posterior fossa. J Neurol. (1994) 241:175–7. 10.1007/BF00868346 [DOI] [PubMed] [Google Scholar]
- 6.Uchino A, Kato A, Kuroda Y, Shimokawa S, Kudo S. Pontine venous congestion caused by dural carotid-cavernous fistula: report of two cases. Eur Radiol. (1997) 7:405–8. 10.1007/s003300050175 [DOI] [PubMed] [Google Scholar]
- 7.Ernst RJ, Gaskill-Shipley M, Tomsick TA, Hall LC, Tew JM, Jr, et al. Cervical myelopathy associated with intracranial dural arteriovenous fistula: MR findings before and after treatment. AJNR Am J Neuroradiol. (1997) 18:1330–4. [PMC free article] [PubMed] [Google Scholar]
- 8.Ricolfi F, Manelfe C, Meder JF, Arrue P, Decq P, Brugieres P, et al. Intracranial dural arteriovenous fistulae with perimedullary venous drainage. Anatomical, clinical and therapeutic considerations. Neuroradiology. (1999) 41:803–12. 10.1007/s002340050846 [DOI] [PubMed] [Google Scholar]
- 9.Bousson V, Brunereau L, Vahedi K, Chapot R. Intracranial dural fistula as a cause of diffuse MR enhancement of the cervical spinal cord. J Neurol Neurosurg Psychiatry. (1999) 67:227–30. 10.1136/jnnp.67.2.227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hurst RW, Bagley LJ, Scanlon M, Flamm ES. Dural arteriovenous fistulas of the craniocervical junction. Skull Base Surg. (1999) 9:1–7. 10.1055/s-2008-1058166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takahashi S, Tomura N, Watarai J, Mizoi K, Manabe H. Dural arteriovenous fistula of the cavernous sinus with venous congestion of the brain stem: report of two cases. AJNR Am J Neuroradiol. (1999) 20:886–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Shintani S, Tsuruoka S, Shiigai T. Carotid-cavernous fistula with brainstem congestion mimicking tumor on MRI. Neurology. (2000) 55:1929–31. 10.1212/WNL.55.12.1929 [DOI] [PubMed] [Google Scholar]
- 13.Wiesmann M, Padovan CS, Pfister HW, Yousry TA. Intracranial dural arteriovenous fistula with spinal medullary venous drainage. Eur Radiol. (2000) 10:1606–9. 10.1007/s003300000382 [DOI] [PubMed] [Google Scholar]
- 14.Kalamangalam GP, Bhattacharya J, Teasdale E, Thomas M. Myelopathy from intracranial dural arteriovenous fistula. J Neurol Neurosurg Psychiatry. (2002) 72:816–8. 10.1136/jnnp.72.6.816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weigele JB, Chaloupka JC, Lesley WS. Galenic dural arteriovenous fistula: unusual clinical presentation and successful endovascular therapy. Case report. J Neurosurg. (2002) 97:467–70. 10.3171/jns.2002.97.2.0467 [DOI] [PubMed] [Google Scholar]
- 16.Asakawa H, Yanaka K, Fujita K, Marushima A, Anno I, Nose T. Intracranial dural arteriovenous fistula showing diffuse MR enhancement of the spinal cord: case report and review of the literature. Surg Neurol. (2002) 58:251–7. 10.1016/S0090-3019(02)00861-3 [DOI] [PubMed] [Google Scholar]
- 17.Lanz M, Thiemann U, Grzyska U, Ebke M, Schwendemann G, Kraus JA. Transient brainstem ischemia and recurrent syncope caused by a dural arteriovenous fistula. Neurology. (2003) 61:1152–3. 10.1212/WNL.61.8.1152 [DOI] [PubMed] [Google Scholar]
- 18.Kai Y, Hamada JI, Morioka M, Yano S, Ushio Y. Brain stem venous congestion due to dural arteriovenous fistulas of the cavernous sinus. Acta Neurochir. (2004) 146:1107–11. 10.1007/s00701-004-0315-3 [DOI] [PubMed] [Google Scholar]
- 19.Li J, Ezura M, Takahashi A, Yoshimoto T. Intracranial dural arteriovenous fistula with venous reflux to the brainstem and spinal cord mimicking brainstem infarction–case report. Neurol Med Chir. (2004) 44:24–8. 10.2176/nmc.44.24 [DOI] [PubMed] [Google Scholar]
- 20.Pannu Y, Shownkeen H, Nockels RP, Origitano TC. Obliteration of a tentorial dural arteriovenous fistula causing spinal cord myelopathy using the cranio-orbito zygomatic approach. Surg Neurol. (2004) 62:463–7. 10.1016/j.surneu.2004.01.017 [DOI] [PubMed] [Google Scholar]
- 21.Crum BA, Link M. Intracranial dural arteriovenous fistula mimicking brainstem neoplasm. Neurology. (2004) 62:2330–1. 10.1212/01.WNL.0000130342.68494.78 [DOI] [PubMed] [Google Scholar]
- 22.Oishi H, Horinaka N, Shmizu T, Ozaki Y, Arai H. A case of intracranial dural arteriovenous fistula presenting with brainstem infarction. No Shinkei Geka. (2005) 33:1095–9. 10.11477/mf.1436100147 [DOI] [PubMed] [Google Scholar]
- 23.Satoh M, Kuriyama M, Fujiwara T, Tokunaga K, Sugiu K. Brain stem ischemia from intracranial dural arteriovenous fistula: case report. Surg Neurol. (2005) 64:341–5. 10.1016/j.surneu.2004.12.029 [DOI] [PubMed] [Google Scholar]
- 24.Akkoc Y, Atamaz F, Oran I, Durmaz B. Intracranial dural arteriovenous fistula draining into spinal perimedullary veins: a rare cause of myelopathy. J Korean Med Sci. (2006) 21:958–62. 10.3346/jkms.2006.21.5.958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iwasaki M, Murakami K, Tomita T, Numagami Y, Nishijima M. Cavernous sinus dural arteriovenous fistula complicated by pontine venous congestion. A case report. Surg Neurol. (2006) 65:516–8. 10.1016/j.surneu.2005.06.044 [DOI] [PubMed] [Google Scholar]
- 26.Lagares A, Perez-Nunez A, Alday R, Ramos A, Campollo J, Lobato RD. Dural arteriovenous fistula presenting as brainstem ischaemia. Acta Neurochir. (2007) 149:965–7. 10.1007/s00701-007-1250-x [DOI] [PubMed] [Google Scholar]
- 27.van Rooij WJ, Sluzewski M, Beute GN. Intracranial dural fistulas with exclusive perimedullary drainage: the need for complete cerebral angiography for diagnosis and treatment planning. AJNR Am J Neuroradiol. (2007) 28:348–51. 10.1016/S0098-1672(08)70215-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sakamoto S, Ohba S, Shibukawa M, Kiura Y, Okazaki T, Kurisu K. Course of apparent diffusion coefficient values in cerebral edema of dural arteriovenous fistula before and after treatment. Clin Neurol Neurosurg. (2008) 110:400–3. 10.1016/j.clineuro.2007.12.010 [DOI] [PubMed] [Google Scholar]
- 29.Tsutsumi S, Yasumoto Y, Ito M, Oishi H, Arai H. Posterior fossa dural arteriovenous fistula as a probable cause of congestive myelopathy. Case report. Neurol Med Chir. (2008) 48:171–5. 10.2176/nmc.48.171 [DOI] [PubMed] [Google Scholar]
- 30.Sugiura Y, Nozaki T, Sato H, Sawashita K, Hiramatsu H, Nishizawa S. Sigmoid sinus dural arteriovenous fistula with spinal venous drainage manifesting as only brainstem-related neurological deficits without myelopathy: case report. Neurol Med Chir. (2009) 49:71–6. 10.2176/nmc.49.71 [DOI] [PubMed] [Google Scholar]
- 31.Wang HC, Lin WC, Kuo YL, Yang TM, Ho JT, Tsai NW, et al. Factors associated with brainstem congestive encephalopathy in dural arterio-venous fistulas. Clin Neurol Neurosurg. (2009) 111:335–40. 10.1016/j.clineuro.2008.11.004 [DOI] [PubMed] [Google Scholar]
- 32.Khan S, Polston DW, Shields RW, Jr, Rasmussen P, Gupta R. Tentorial dural arteriovenous fistula presenting with quadriparesis: case report and review of the literature. J Stroke Cerebrovasc Dis. (2009) 18:428–34. 10.1016/j.jstrokecerebrovasdis.2008.12.007 [DOI] [PubMed] [Google Scholar]
- 33.Ko SB, Kim CK, Lee SH, Yoon BW. Carotid cavernous fistula with cervical myelopathy. J Clin Neurosci. (2009) 16:1350–3. 10.1016/j.jocn.2008.12.031 [DOI] [PubMed] [Google Scholar]
- 34.Kleeberg J, Maeder-Ingvar M, Maeder P. Progressive cervical myelopathy due to dural craniocervical fistula. Eur Neurol. (2010) 63:374. 10.1159/000292430 [DOI] [PubMed] [Google Scholar]
- 35.Patsalides A, Tzatha E, Stubgen JP, Shungu DC, Stieg PE, Gobin YP. Intracranial dural arteriovenous fistula presenting as an enhancing lesion of the medulla. J Neurointerv Surg. (2010) 2:390–3. 10.1136/jnis.2009.001750 [DOI] [PubMed] [Google Scholar]
- 36.Aixut Lorenzo S, Tomasello Weitz A, Blasco Andaluz J, Sanroman Manzanera L, Macho Fernandez JM. Transvenous approach to intracranial dural arteriovenous fistula (Cognard v): a treatment option. A case report. Interv Neuroradiol. (2011) 17:108–14. 10.1177/159101991101700117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim NH, Cho KT, Seo HS. Myelopathy due to intracranial dural arteriovenous fistula: a potential diagnostic pitfall. Case report. J Neurosurg. (2011) 114:830–3. 10.3171/2010.5.JNS10128 [DOI] [PubMed] [Google Scholar]
- 38.Peltier J, Baroncini M, Thines L, Lacour A, Leclerc X, Lejeune JP. Subacute involvement of the medulla oblongata and occipital neuralgia revealing an intracranial dural arteriovenous fistula of the craniocervical junction. Neurol India. (2011) 59:285–8. 10.4103/0028-3886.79153 [DOI] [PubMed] [Google Scholar]
- 39.Clark SW, Dang T, Toth G, Pride GL, Greenberg B, Warnack W. Carotid cavernous fistula imitating brainstem glioma. Arch Neurol. (2011) 68:256–7. 10.1001/archneurol.2010.366 [DOI] [PubMed] [Google Scholar]
- 40.Ogbonnaya ES, Yousaf I, Sattar TM. Intracranial dural arterio-venous fistula presenting with progressive myelopathy. BMJ Case Rep. (2011) 2011:4828. 10.1136/bcr.09.2011.4828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kulwin C, Bohnstedt BN, Scott JA, Cohen-Gadol A. Dural arteriovenous fistulas presenting with brainstem dysfunction: diagnosis and surgical treatment. Neurosurg Focus. (2012) 32:E10. 10.3171/2012.2.FOCUS1217 [DOI] [PubMed] [Google Scholar]
- 42.Clark CN, Saifee TA, Cowley PO, Ginsberg L. Dural arteriovenous fistula of the medulla initially mimicking Guillain-Barre syndrome. Arch Neurol. (2012) 69:786–7. 10.1001/archneurol.2011.2934 [DOI] [PubMed] [Google Scholar]
- 43.Mathon B, Gallas S, Tuillier T, Bekaert O, Decq P, Brugieres P, et al. Intracranial dural arteriovenous fistula with perimedullary venous drainage: anatomical, clinical and therapeutic considerations about one case, and review of the literature. Neurochirurgie. (2013) 59:133–7. 10.1016/j.neuchi.2013.04.009 [DOI] [PubMed] [Google Scholar]
- 44.Salamon E, Patsalides A, Gobin YP, Santillan A, Fink ME. Dural arteriovenous fistula at the craniocervical junction mimicking acute brainstem and spinal cord infarction. JAMA Neurol. (2013) 70:796–7. 10.1001/jamaneurol.2013.1946 [DOI] [PubMed] [Google Scholar]
- 45.Singh D, Garg A, Gupta A, Goel G, Gupta R, Bansal A. Tentorial dural arteriovenous fistula presenting as episodic weakness mimicking periodic paralysis. J Neurointerv Surg. (2013) 5:e32. 10.1136/neurintsurg-2012-010281 [DOI] [PubMed] [Google Scholar]
- 46.El Asri AC, El Mostarchid B, Akhaddar A, Naama O, Gazzaz M, Boucetta M. Factors influencing the prognosis in intracranial dural arteriovenous fistulas with perimedullary drainage. World Neurosurg. (2013) 79:182–91. 10.1016/j.wneu.2012.09.012 [DOI] [PubMed] [Google Scholar]
- 47.Foreman SM, Stahl MJ, Schultz GD. Paraplegia in a chiropractic patient secondary to atraumatic dural arteriovenous fistula with perimedullary hypertension: case report. Chiropr Man Therap. (2013) 21:23. 10.1186/2045-709X-21-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gross R, Ali R, Kole M, Dorbeistein C, Jayaraman MV, Khan M. Tentorial dural arteriovenous fistula presenting as myelopathy: case series and review of literature. World J Clin Cases. (2014) 2:907–11. 10.12998/wjcc.v2.i12.907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wu Q, Wang HD, Shin YS, Zhang X. Brainstem congestion due to dural ateriovenous fistula at the craniocervical junction. J Korean Neurosurg Soc. (2014) 55:152–5. 10.3340/jkns.2014.55.3.152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haryu S, Endo T, Sato K, Inoue T, Takahashi A, Tominaga T. Cognard type V intracranial dural arteriovenous shunt: case reports and literature review with special consideration of the pattern of spinal venous drainage. Neurosurgery. (2014) 74:E135–42. 10.1227/NEU.0000000000000069 [DOI] [PubMed] [Google Scholar]
- 51.Roelz R, Van Velthoven V, Reinacher P, Coenen VA, Mader I, Urbach H, et al. Unilateral contrast-enhancing pontomedullary lesion due to an intracranial dural arteriovenous fistula with perimedullary spinal venous drainage: the exception that proves the rule. J Neurosurg. (2015) 123:1534–9. 10.3171/2014.11.JNS142278 [DOI] [PubMed] [Google Scholar]
- 52.Le Guennec L, Leclercq D, Szatmary Z, Idbaih A, Reyes-Botero G, Delattre JY, et al. Dural arteriovenous fistula mimicking a brainstem glioma. J Neuroimaging. (2015) 25:1053–5. 10.1111/jon.12220 [DOI] [PubMed] [Google Scholar]
- 53.Alvarez H, Sasaki-Adams D, Castillo M. Resolution of brainstem edema after treatment of a dural tentorial arteriovenous fistula. Interv Neuroradiol. (2015) 21:603–8. 10.1177/1591019915591741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pop R, Manisor M, Aloraini Z, Chibarro S, Proust F, Quenardelle V, et al. Foramen magnum dural arteriovenous fistula presenting with epilepsy. Interv Neuroradiol. (2015) 21:724–7. 10.1177/1591019915609783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Abud LG, Abud TG, Nakiri GS, Queiroz RM, Abud DG. Intracranial dural arteriovenous fistula with perimedullary drainage treated by endovascular embolization. Arq Neuropsiquiatr. (2016) 74:178–9. 10.1590/0004-282X20150171 [DOI] [PubMed] [Google Scholar]
- 56.Abdelsadg M, Kanodia AK, Keston P, Galea J. Unusual case of intracranial dural AV fistula presenting with acute myelopathy. BMJ Case Rep. (2016) 2016:bcr2016215227. 10.1136/bcr-2016-215227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Enokizono M, Sato N, Morikawa M, Kimura Y, Sugiyama A, Maekawa T, et al. “Black butterfly” sign on T2*-weighted and susceptibility-weighted imaging: A novel finding of chronic venous congestion of the brain stem and spinal cord associated with dural arteriovenous fistulas. J Neurol Sci. (2017) 379:64–8. 10.1016/j.jns.2017.05.066 [DOI] [PubMed] [Google Scholar]
- 58.Tanaka J, Fujita A, Maeyama M, Kohta M, Hosoda K, Kohmura E. Cognard type Vdural arteriovenous fistula involving the occipital sinus. J Stroke Cerebrovasc Dis. (2017) 26:e62–3. 10.1016/j.jstrokecerebrovasdis.2017.01.004 [DOI] [PubMed] [Google Scholar]
- 59.Emmer BJ, van Es AC, Koudstaal PJ, Roosendaal SD. Infratentorial dural arteriovenous fistula resulting in brainstem edema and enhancement. Neurology. (2017) 88:503–4. 10.1212/WNL.0000000000003569 [DOI] [PubMed] [Google Scholar]
- 60.Duan SS, Liu H, Wang WL, Zhao CB. A case of intracranial dural arteriovenous fistula mimicking brainstem tumor. Chin Med J. (2017) 130:2519–20. 10.4103/0366-6999.216398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chen PM, Chen MM, McDonald M, McGehrin K, Steinberg J, Handwerker J, et al. Cranial Dural Arteriovenous Fistula. Stroke. (2018) 49:e332–4. 10.1161/STROKEAHA.118.022508 [DOI] [PubMed] [Google Scholar]
- 62.Bernard F, Lemee JM, Faguer R, Fournier HD. Lessons to be remembered from a dural arteriovenous fistula mimicking medulla and high cervical cord glioma. World Neurosurg. (2018) 113:312–5. 10.1016/j.wneu.2018.02.161 [DOI] [PubMed] [Google Scholar]
- 63.Li J, Ren J, Du S, Ling F, Li G, Zhang H. Dural arteriovenous fistulas at the petrous apex. World Neurosurg. (2018) 119:e968–e76. 10.1016/j.wneu.2018.08.012 [DOI] [PubMed] [Google Scholar]
- 64.Wang XC, Du YY, Tan Y, Qin JB, Wang L, Wu XF, et al. Brainstem congestion due to dural arteriovenous fistula at the craniocervical junction: case report and review of the literature. World Neurosurg. (2018) 118:181–7. 10.1016/j.wneu.2018.06.243 [DOI] [PubMed] [Google Scholar]
- 65.Takahashi H, Ueshima T, Goto D, Kimura T, Yuki N, Inoue Y, et al. acute tetraparesis with respiratory failure after steroid administration in a patient with a dural arteriovenous fistula at the craniocervical junction. Intern Med. (2018) 57:591–4. 10.2169/internalmedicine.9115-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Copelan AZ, Krishnan A, Marin H, Silbergleit R. Dural arteriovenous fistulas: a characteristic pattern of edema and enhancement of the medulla on MRI. AJNR Am J Neuroradiol. (2018) 39:238–44. 10.3174/ajnr.A5460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rodriguez Rubio R, Chae R, Rutledge WC, De Vilalta A, Kournoutas I, Winkler E, et al. Clipping of a high-risk dural arteriovenous fistula of the posterior fossa: 3d operative video. World Neurosurg. (2019) 126:413. 10.1016/j.wneu.2019.03.101 [DOI] [PubMed] [Google Scholar]
- 68.Shimizu A, Ishikawa T, Yamaguchi K, Funatsu T, Ryu B, Nagahara A, et al. Brainstem venous congestion caused by perimedullary drainage in anterior cranial fossa dural arteriovenous fistula. World Neurosurg. (2019) 127:503–8. 10.1016/j.wneu.2019.04.204 [DOI] [PubMed] [Google Scholar]
- 69.Chen PY, Juan YH, Lin SK. An isolated unilateral pontomedullary lesion due to an intracranial dural arteriovenous fistula mimicking a brain tumor - case and review. J Nippon Med Sch. (2019) 86:48–54. 10.1272/jnms.JNMS.2019_86-9 [DOI] [PubMed] [Google Scholar]
- 70.Reynolds MR, Lanzino G, Zipfel GJ. Intracranial dural arteriovenous fistulae. Stroke. (2017) 48:1424–31. 10.1161/STROKEAHA.116.012784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rhoton AL, Jr. The posterior fossa veins. Neurosurgery. (2000) 47(Suppl.3):S69–92. 10.1093/neurosurgery/47.3.S69 [DOI] [PubMed] [Google Scholar]
- 72.Meckel S, Maier M, Ruiz DS, Yilmaz H, Scheffler K, Radue EW, et al. MR angiography of dural arteriovenous fistulas: diagnosis and follow-up after treatment using a time-resolved 3D contrast-enhanced technique. AJNR Am J Neuroradiol. (2007) 28:877–84. [PMC free article] [PubMed] [Google Scholar]
- 73.Di Ieva A, Lam T, Alcaide-Leon P, Bharatha A, Montanera W, Cusimano MD. Magnetic resonance susceptibility weighted imaging in neurosurgery: current applications and future perspectives. J Neurosurg. (2015) 123:1463–75. 10.3171/2015.1.JNS142349 [DOI] [PubMed] [Google Scholar]
- 74.Zalewski NL, Rabinstein AA, Brinjikji W, Kaufmann TJ, Nasr D, Ruff MW, et al. Unique gadolinium enhancement pattern in spinal dural arteriovenous fistulas. JAMA Neurol. (2018) 75:1542–5. 10.1001/jamaneurol.2018.2605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nasr DM, Brinjikji W, Rabinstein AA, Lanzino G. Clinical outcomes following corticosteroid administration in patients with delayed diagnosis of spinal arteriovenous fistulas. J Neurointerv Surg. (2017) 9:607–10. 10.1136/neurintsurg-2016-012430 [DOI] [PubMed] [Google Scholar]
- 76.Soderman M, Edner G, Ericson K, Karlsson B, Rahn T, Ulfarsson E, et al. Gamma knife surgery for dural arteriovenous shunts: 25 years of experience. J Neurosurg. (2006) 104:867–75. 10.3171/jns.2006.104.6.867 [DOI] [PubMed] [Google Scholar]
- 77.Luo CB, Chang FC, Teng MM, Lin CJ, Wang AG, Ting TW. Aggressive cavernous sinus dural arteriovenous fistula: angioarchitecture analysis and embolization by various approaches. J Chin Med Assoc. (2016) 79:152–8. 10.1016/j.jcma.2015.09.001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.