Abstract
Purpose
The widespread coronavirus disease 2019 (COVID-19) pandemic has resulted in significant changes in care delivery among radiation oncology practices and has demanded the rapid incorporation of telehealth. However, the impact of a large-scale transition to telehealth in radiation oncology on patient access to care and the viability of care delivery are largely unknown. In this manuscript, we review our implementation and report data on patient access to care and billing implications. Because telehealth is likely to continue after COVID-19, we propose a radiation oncology–specific algorithm for telehealth.
Methods and Materials
In March 2020, our department began to use telehealth for all new consults, posttreatment encounters, and follow-up appointments. Billable encounters from January to April 2020 were reviewed and categorized into 1 of the following visit types: in-person, telephonic, or 2-way audio-video. Logistic regression models tested whether visit type differed by patient age, income, or provider.
Results
There was a 35% decrease in billable activity from January to April. In-person visits decreased from 100% to 21%. Sixty percent of telehealth appointments in April were performed with 2-way audio-video and 40% by telephone only. In-person consultation visits were associated with higher billing codes compared with 2-way audio-video telehealth visits (P < .01). No difference was seen for follow-up visits. Univariate and multivariable analysis identified that older patient age was associated with reduced likelihood of 2-way audio-video encounters (P < .01). The physician conducting the telehealth appointment was also associated with the type of visit (P < .01). Patient income was not associated with the type of telehealth visit.
Conclusions
Since the onset of the COVID-19 pandemic, we have been able to move the majority of patient visits to telehealth but have observed inconsistent utilization of the audio-video telehealth platform. We present guidelines and quality metrics for incorporating telehealth into radiation oncology practice, based on type of encounter and disease subsite.
Introduction
Since its initial onset at the end of 2019, severe acute respiratory syndrome coronavirus 2 has caused a pandemic that has transformed health care across the continuum. The widespread coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 has resulted in rapid and significant change in care delivery among radiation oncology practices everywhere. Our health system, located in the New York City metropolitan area, is within the epicenter of the COVID-19 outbreak. We alone have diagnosed over 40,000 patients with COVID-19, managed 14,000 hospitalized patients, and discharged over 10,000 of those cases.1 The health system's crisis management program implemented a comprehensive action plan on March 13, 2020, with multiple policies designed to protect staff and manage the surge in patient volume. As the volume of COVID-19–positive patients started to overwhelm the health system, policies implemented in radiation medicine allowed for safe, high-quality medical care to continue throughout our multiple locations.2,3 In May 2020, although new COVID-19 cases have decreased in New York, it is apparent that health care has changed permanently. New approaches to care, including telehealth, were adopted during this period and will redefine how health care is provided worldwide.
Telehealth, as defined by the Office for the Advancement of Telehealth, comprises the use of telecommunications and information technologies to share information and to provide clinical care, education, public health, and administrative services at a distance.4 Technological improvements have made synchronous telehealth more feasible, defined as the delivery of a live, interactive video connection that transmits information in both directions during the same period.5 Before COVID-19, widespread adoption was slow owing to barriers including limited reimbursement, regulatory restrictions, privacy issues, and lack of patient and provider comfort and preference.6,7 However, this abruptly changed with the onset of the COVID-19 pandemic.
The COVID-19 crisis created an acute transition to telehealth to maintain safe operations for patients and health care providers alike. The US government relaxed the regulatory requirements for telehealth, and the Center for Medicare and Medicaid Services (CMS) greatly expanded financial coverage, paving the way for private insurers to follow suit.8 The simultaneous removal of these 2 significant barriers, coupled with the availability of various telehealth platforms already in the market and the government's decision to waive the requirement to use Health Insurance Portability and Accountability Act (HIPAA)-compliant communication platforms, catalyzed telehealth's widespread adoption into the clinic setting.9 Although the reimbursement parity enacted by CMS and private payers was initially limited to the duration of the COVID-19 pandemic response, CMS has said widespread use of telehealth is likely to continue in postpandemic care.10
For telehealth to continue, it must enhance patient access and outcomes, clinical efficiency, or both. In pursuing these goals, there is much to learn regarding the effective use of telehealth in radiation oncology. Poor implementation and execution of telehealth pose potential risks to the patient owing to the complexity of cancer care and the nuances involved with radiation therapy. Telehealth practice carries the risk of exacerbating disparities of patient access to care for those who do not have access to high-speed Internet or video calling.11 Furthermore, continued widespread use of telehealth depends on identifying feasible business models for its use. We must recognize that the rapid adoption of this technology in radiation oncology during COVID-19 has been done with limited data, and we must be careful of unintended consequences.12 Currently, there are no guidelines for optimal and appropriate use of telehealth in radiation oncology, and no quality metrics have been established.
In our academic multisite radiation oncology department, we rapidly implemented telehealth as the COVID-19 pandemic unfolded. In this manuscript, we review our implementation process, outline lessons learned about patient access and billing, and use these data to propose a radiation oncology–specific algorithm for moving forward with telehealth.
Methods and Materials
Our department consists of 7 outpatient radiation oncology facilities with 20 full-time faculty spread throughout the New York metropolitan area. Before March 2020, we exclusively saw patients in person. Our health system had deployed a telehealth strategy over the preceding 3 years but only on a trial basis. As COVID-19 crisis management planning took hold in mid-March 2020, our department began preparing for full implementation of telehealth. A HIPAA-compliant platform, Amwell Telehealth (American Well Corporation, Boston MA), was selected to deliver telehealth care. This platform was purchased by our health system for use throughout all outpatient sites before the pandemic. We promptly purchased the necessary equipment and began credentialing physicians for a 2-way audio-video software package. Simultaneously, we trained our secretarial and billing teams to be integrated into the department's telehealth workflow process. Secretarial teams were asked to schedule patients for telehealth visits and assist them in accessing the platform. Midlevel providers and resident trainees were also trained and incorporated into the telehealth workflow. In general, midlevel providers and residents would initiate telehealth encounters and troubleshoot any technical difficulties with patients. Upon completion of their assigned clinical tasks, the encounter would be transferred to the attending physician. By March 28, 2020, all providers had been credentialed and provided guidance to use telehealth in their practices. Our initial roll-out was to use telehealth for all new consults, posttreatment encounters, and follow-up appointments. Telehealth was to be conducted with a 2-way audio-video platform, with telephone-only appointments reserved for situations in which 2-way audio-video was not feasible. In-person on-treatment visits (OTVs) continued as per our usual prepandemic workflow.
Billable encounters, representing consultation and follow-up appointments, from 6 of our radiation oncology offices between January 1 and May 1, 2020, were available for review in our HIPAA-compliant administrative database. Each encounter was categorized into 1 of the following visit types: in-person, telephonic, or 2-way audio-video. The patient's zip code and provider name were recorded. Patient income was estimated by using data from the 2018 census that estimates median income by zip code. Age was calculated at date of encounter (available at 4 of the 6 facilities).
SPSS was used for statistical calculations. The association between type of telehealth visit and charged level of visit was calculated using the independent sample t test. Logistic regression tested differences in visit type by patient characteristics including age, income, and provider. All tests were 2-sided and were considered to be statistically significant at P < .05. Analyses were conducted using SPSS (SPSS, Chicago, IL).
Results
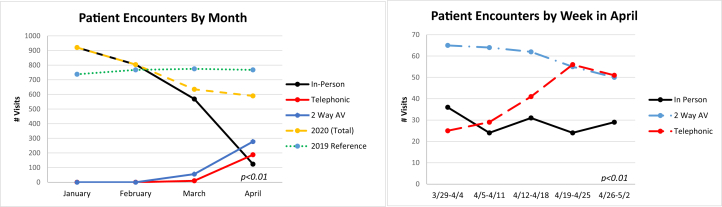
Between January 1 and May 1, 2020, 2997 billable evaluation and management encounters occurred (Fig 1). Overall, there was a 35% decrease in billable activity from January to April. In-person visits represented 100% of visits in January and February, 90% of visits in March, and 21% of visits in April. Sixty percent of telehealth appointments in April were performed with 2-way audio-video and 40% by telephone only. Since the initiation of our telehealth program, there has been a steady increase in telephone-only encounters (P < .01).
Figure 1.
The number of billable consult and follow-up appointments by method of encounter (in-person vs telephonic vs 2-way audio-video). In-person visits became a small portion of our care in April. In April, telephonic-only visits increased compared with 2-way audio-video and in-person visits.
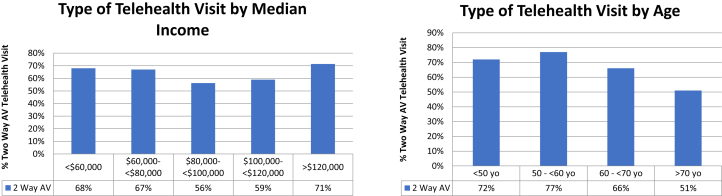
For patients using telehealth, the median age was 71 years (range, 22-93 years). Median income by zip code was $88,815 (range, $26,239-$168,902). We reviewed clinical and demographic variables to assess the likelihood to complete a 2-way audio-video versus telephone-only appointment (Fig 2). Univariate analysis identified that older patient age by year (P < .01; odds ratio, 0.97) was associated with reduced likelihood of 2-way audio-video encounters. The physician conducting the appointment was also associated with the type of telehealth appointment selected (P < .01), and the percentage of 2-way audio-video usage varied from 22% to 100%. Patient income was not associated with the type of telehealth visit (P = .48). On multivariable analysis, when controlling for median income, physician, and age, the physician conducting the visit (P < .01) and older patient age (P = .01; odds ratio, 0.97) continued to be associated with lower usage of telehealth appointments.
Figure 2.
Factors affecting the type of telehealth visit that was conducted (2-way audio-video vs telephonic only). Median income was not associated with type of telehealth visit (P = .48). Older age was associated with increased telephonic-only visit (P < .01).
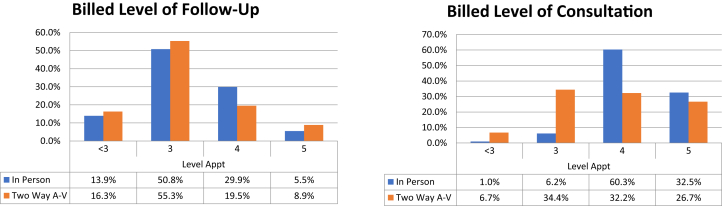
In-person visits can be billed based on both time and complexity whereas 2-way audio-video encounters are billed only based on time. We identified that for consultations, in-person visits were associated with higher billing codes compared with 2-way audio-video encounters (P < .01). No difference was seen for follow-up visits (P = .36, Fig 3).
Figure 3.
The effect of 2-way audio-video telehealth on level of visit charges. The level of appointment charged for telehealth appointments was not different for follow-up appointments (P = .36). For consultation appointments, patients were more frequently billed a lower level of visit than for an in-person visit (P < .01).
Discussion
The COVID-19 pandemic has resulted in the immediate initiation of telehealth for evaluation and management visits in our radiation oncology department. We were able to successfully move the majority of visits to telehealth while permitting the option of in-person appointments for those who could not participate in telehealth. This rapid implementation allowed us to continue providing patients with access to radiation oncology physicians while reducing patient exposures from travel and in-office visits. Our results support the continued use of telehealth after the pandemic, but whether it should be used for only specific patients or types of visits remains to be determined.
Challenges of rapidly implementing 2-way audio-video telehealth
We observed inconsistent utilization of the audio-video telehealth platform and increased use of backup telephonic visits over time. To improve the use of telehealth going forward, it is crucial to understand why this was the case. Although the various platforms for telehealth have been in place for some time, many of the factors needed to establish a successful interface remain less than ideal. Successful implementation of telehealth requires (1) appropriate access to the correct technology (smartphone or computer with appropriate high-speed Internet access) and (2) understanding of and comfort in using the technology. Our suggested workflow during the initial incorporation of telehealth was for our administrative staff to provide instructions to the patient on how to use the telehealth platform at the time of scheduling. They would also record the phone number and/or email that would be used for the telehealth appointment. If the patient stated that they were unable to access the telehealth platform due to technological limitations, they were scheduled for a telephonic visit or, if preferred, an in-person visit. Clinicians were responsible at the time of the scheduled appointment for sending a web link for the appointment based on the information recorded by the administrative staff and for addressing any technical difficulties that may occur.
Our experience found that older patients were less likely to navigate 2-way audio-video encounters. With the hypothesis that this may be due to less comfort with the technology, we will be asking administrative staff to call all patients the day before their visit to perform a test visit. Alternatively, if additional training and assistance do not help them use this technology, it may be that some older patients may not be suitable to be assessed via telehealth. Regardless of age, it is unclear why we saw reduced use of audiovisual and increased use of telephone visits over time. We expect that the platform interfaces will continue to improve with easier access for patients and that patients will become more familiar with the technology and embrace telehealth for their medical care. However, we do recognize that certain patients simply prefer in-person visits and may represent the subgroup that has had difficulty navigating a 2-way audio-video encounter. As we move forward from the pandemic, we will be expanding in-person appointments, giving patients the opportunity to select the type of visit most appropriate for them.
In addition to patient-specific factors, we found that physician preference (adopters vs nonadopters) independently predicted the method of telehealth encounter. We plan to revisit the physician training process, which may help modify provider behavior and improve utilization of 2-way audio-video telehealth. Given the issues associated with the audio-video platform, we were pleased that on April 30, 2020, CMS extended payment of telehealth to include telephonic visits. Nevertheless, we continue to recommend 2-way audio-video encounters as the standard of telehealth care to the extent possible; we believe the video aspect of the visit is a very valuable component of being able to offer appropriate clinical advice and establish a patient-physician relationship.
We found that the average level of visit charged for telehealth consultations using the 2-way audio-video telehealth encounter was lower than that charged for in-person visits. Our data show that >90% of new consultations done in-person are typically charged as a level 4 or 5 visit compared with only approximately 60% of new consultations seen using 2-way audio-video telehealth. Among other reasons, the lower levels of visit charges are likely reflective of telehealth visits being shorter in duration than in-person visits and the lack of a comprehensive physical examination being performed. Although we expect that with experience and training, providers will be able to learn more effective ways to perform better physical examinations via telehealth, some level of discrepancy between charge levels will likely persist between these types of visits. Based on evaluation and management Medicare fee schedule, our data suggest that this difference translates to an approximately 11% decrease in revenue per new visit. The average difference will be greater with increased use of telephonic-only visits. This may be important for some practices to consider. In our experience, many of the patients seen for initial consultation with telehealth required an in-person visit for further education and physical examination before simulation and were charged for a 15-minute in-person follow-up visit, reducing the deficit seen from the consultation charges.
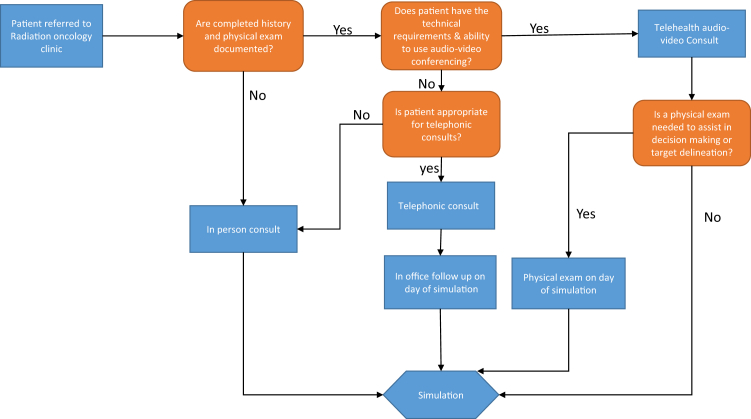
For telehealth to continue as a successful model of care delivery, it must improve patient access to care, patient outcomes, and care efficiency, and ideally it could improve all of these metrics. Given current billing limitations for telehealth, our data show that reliance on telehealth for all care may not be financially sustainable for clinics to implement. It is also not likely to be appropriate for every clinical encounter. Although telehealth was rapidly adopted into our radiation oncology department, the limited literature and overall experience within our discipline mandate that we carefully examine implementation and outcomes.13 We convened a department task force to define the optimal use of telehealth and created guidelines for incorporating telehealth for future evaluation and management visits (Table 1). We created separate recommendations based on type of encounter (new consultation, on-treatment visit, posttreatment encounter, follow-up visit). Workflows for new consultation appointments are described in Figure 4. Follow-up recommendations were based on the disease subsite and perceived suitability for telehealth (Table 2). We recognize that the transition to telehealth must be done in tandem with the collection of data on quality measures. The National Quality Forum suggested 4 domains that may be used as a framework for measuring the effectiveness of telehealth: access to care, financial impact/cost, experience, and effectiveness. As such, we propose quality measures applicable to radiation oncology using this framework to measure implementation and outcomes (Table 3).
Table 1.
Telehealth recommendations by type of encounter
| Visit type | Recommendations |
|---|---|
| Consult | Patient have option of booking their initial consult via 2-way audio-video telehealth (see Fig 3) |
| Coordinate in-person follow-up or physical examination with simulation | |
| Telephonic-only consult is discouraged | |
| OTVs | OTVs should continue in person |
| Telehealth can be used as a secondary tool to provide additional clinical care | |
| Posttreatment evaluation | Patient have option of booking PTE via telehealth, except for head and neck, gynecologic, and anal cancer |
| In-person examinations can be scheduled after telehealth as clinically indicated | |
| Follow-up | Multidisciplinary team discussion to coordinate telehealth visits to reduce duplicated physical examinations and visits |
| Recommendations are made based on disease subsite, incorporating NCCN recommendations for follow-up and in consideration of (1) the necessity of a physical examination finding to assess treatment response and (2) requirement of an in-person physical examination for cancer surveillance (see Table 2) |
Abbreviations: NCCN = National Comprehensive Cancer Network; OTV = on-treatment visits; PTE = posttreatment encounters.
Figure 4.
Framework for incorporating telehealth into consult workflow.
Table 2.
Recommendations regarding appropriateness of telehealth for follow-up care with minimum number of in-person examinations
| Appropriateness | Disease site | Minimum site-specific in-person examinations |
|---|---|---|
| High | CNS Breast Lung GI (except anal cancer) GU/prostate Soft tissue sarcoma Skin |
Year 1-2: 1 to 2 examinations annually Year 3-5: as clinically indicated |
| Moderate | GI/anal cancer (after complete response) Lymphoma |
Year 1-2: 2 examinations annually Year 3-5: annual examination |
| Low | Head and neck cancer Gyn-endometrial Gyn-cervical |
Year 1-2: every 3-6 months Year 3-5: every 6-12 months |
Abbreviations: CNS = central nervous system; GI = gastrointestinal; GU = genitourinary; Gyn = gynecologic.
Table 3.
Radiation oncology–specific telehealth quality metrics
| Domain | Measures |
|---|---|
| Access to care | Time from referral to consult |
| Time from consult to simulation | |
| Access to care for underserved patients | |
| Simulation cancellation rate | |
| Financial impact | Cost of telehealth implementation and maintenance |
| Number of second opinion consults | |
| Difference in reimbursement | |
| Cost savings to patients – direct and indirect | |
| Cost savings from care coordination | |
| User experience | Patient satisfaction |
| Provider satisfaction | |
| Time required for technical troubleshooting | |
| Clinical effectiveness | Documentation of pain or KPS |
| Rate of unexpected hospital admissions | |
| Effectiveness in coordination and shared care | |
| Patient adherence to recommended follow-up schedule | |
| Clinical outcomes |
Abbreviation: KPS = Karnofsky Performance Status.
Framework for incorporating telehealth into consultation visits
We see significant opportunities in incorporating telehealth for consultation visits (Fig 3). Telehealth approaches can include telehealth consults through audio-video platforms or telephonic consults supplemented by in-office follow-up where needed (eg, for older patients who cannot access or use audio-video platforms). Radiation oncology is uniquely amenable to telehealth because most of the diagnostic workup is often completed before the consultation, and simulation requires patients to travel on-site, thereby giving the clinician a built-in opportunity to meet the patient in-person before the initiation of treatment.
A potential benefit to incorporating telehealth into the consult workflow includes the ease of scheduling, particularly for vulnerable and elderly populations that are dependent on caregivers.14 An Australian study showed that 52% of patients reported concern regarding treatment delays in at least 1 treatment phase of their oncology care, including 31% who expressed concern regarding the time interval between deciding to have radiation therapy and commencement of radiation therapy.15 Shorter time from diagnosis to treatment improves patient outcomes,16 reduces patient anxiety,15 and improves patients' satisfaction and their perception of the quality of care.17 Telehealth removes many of the logistical barriers required to schedule appointments, and we anticipate that it will shorten the interval from referral to consult and expedite scheduling for treatments. The benefit of faster appointment times has been seen in other disciplines; a notable example is the Veterans Affairs liver transplant experience, in which the use of telehealth resulted in a substantial reduction in time from referral to initial evaluation and placement on the liver transplant waitlist.18 We believe that similar benefits will be seen in oncology patients in all geographic areas.
We recognize that telehealth can be disruptive and that, in some disease sites, the inability to perform an in-person physical examination may make it difficult for the provider to offer a comprehensive recommendation. For these disease sites, we think it is reasonable to consider the consultation appointment as an opportunity to triage the patient while maintaining the benefits of early access, convenience, and early care coordination. An in-person visit can be scheduled immediately before simulation to allow for a more detailed examination. This system can also facilitate telehealth-based care for patients with certain difficulties (eg, significant cognitive or communication impairment) that necessitate in-person evaluation. We do believe that with training and innovation, certain aspects of the physical examination can become more accessible to telehealth, especially with devices that link through the virtual visit. As an example, multiple online resources exist to guide providers in how to conduct a neurologic examination using 2-way audio-video conferencing.19,20
Framework for incorporating telehealth into on-treatment and follow-up care
Posttreatment, we recommend including telehealth as part of routine follow-up care as early as safely possible. Telehealth permits discussion of laboratory and imaging results, as well as side effect management. Any concerning findings during a telehealth visit should always prompt an in-person visit. Certain cancer subsites are more dependent on in-person physical examinations for assessment of treatment response and surveillance; these considerations are built into our cancer site–specific recommendations. For all disease sites, telehealth should always be used to prevent duplicated clinic visits and examinations by different providers in the multidisciplinary team.
We continue to recommend in-person weekly OTVs. Because patients must travel to the radiation oncology facility for treatment, telehealth for OTVs would not reduce the logistical burden placed on a patient. Furthermore, we believe that weekly in-person assessments of patients, including a physical examination and vital signs, are necessary to provide optimal care during treatment. These visits allow us to assess tolerability of the prescribed treatment and to identify symptoms that, if not managed appropriately, may result in an emergency department visit or hospital admission. Preventing avoidable hospital and emergency department usage has been of utmost importance to us during the acute phase of the pandemic when our hospital system had limited capacity to manage non-COVID patients.3 We do recognize that in extreme situations in which physician shortages may arise, a reverse telehealth model could be considered. In this scenario, the patient can be seen and examined by a midlevel provider in the clinic before being connected to the physician remotely via a telehealth platform.
Benefits and challenges of telehealth as part of routine care
Since the implementation of our telehealth program, we have observed unanticipated benefits. For example, we have seen more multidisciplinary consultation and follow-up appointments. Before COVID-19, our institution was actively establishing multidisciplinary clinics, although the logistics of such visits have historically been complicated. Since the implementation of telehealth, providers believe that telehealth has made it easier to coordinate multidisciplinary visits with other providers because these visits do not require the providers to be physically present at the same location at a given time. An additional benefit providers have reported is the unique perspective they gain by seeing a patient in their home environment, often surrounded by family members who otherwise would have been unable to accompany the patient to the consult. Telehealth has provided an opportunity for providers to better understand the challenges patients may encounter in their home environment.
We have also identified potential challenges, most notably ensuring that patients have access to the same ancillary services and educational materials that they have with an in-person consultation. It will be important for departments to identify opportunities to bridge this gap. We are working on integrating our social workers, nutritionists, and patient navigators to our telehealth platform so they can participate in the consult. In addition, we are working on digitizing our educational material, which we plan to share with patients on-screen during the consult and make available for access digitally after the clinical encounter.
Another challenge of telehealth is ensuring that patient-clinician communication is not negatively affected. Essential components of effective communication include nonverbal cues, providing adequate time for patient questions, and the ability to build rapport and demonstrate empathy. Studies have emphasized the importance of maintaining effective communication and actively engaging patients during video conferencing.21, 22, 23 However, the majority of clinicians are not trained in effectively conducting a telehealth visit, and some may have more difficulty with the transition. Institutions that plan to adopt telehealth should make training programs and resources available for clinicians to sharpen their communication skills over telehealth.
Conclusions
Telehealth has been an imminent disruptive innovation in health care for many years, and few could have anticipated the velocity at which it has been implemented during the COVID-19 pandemic. Our experience has shown that telehealth has many potential benefits if used thoughtfully and systematically. Our department intends to use telehealth broadly, and we have created guidelines for our physicians to use when scheduling visits. At the same time, we understand the limitations and challenges of telehealth and have outlined when telehealth should not be used. The impact of this new approach must be studied, and we propose quality metrics to measure the outcomes of these interventions carefully. The large-scale adoption of telehealth nationally will generate much-needed experience, which will help guide us moving forward. We must carefully examine the data gathered and lessons learned during this unprecedented time. We believe that the appropriate use of telehealth can improve access and outcomes and complement the existing clinic-centered model of care. As health care providers, we must adapt to and continually improve the use of telehealth, with the ultimate goal of providing patient-centered, feasible, and effective care for all patients with cancer.
Footnotes
Sources of support: This work had no specific funding.
Disclosures: none.
Research data are stored in an institutional repository and will be shared upon request to the corresponding author.
Supplementary material for this article can be found at https://doi.org/10.1016/j.adro.2020.09.015.
Supplementary Materials
References
- 1.Richardson S., Hirsch J.A., Narasimhan M. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parashar B., Chen W.C., Herman J.M., Potters L. Disease site-specific guidelines for curative radiation treatment during 'limited surgery' and 'hospital avoidance': A radiation oncology perspective from the epicenter of COVID-19 pandemic. Cureus. 2020;12:e8190. doi: 10.7759/cureus.8190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen W.C., Teckie S., Somerstein G., Adair N., Potters L. Guidelines to reduce hospitalization rates for patients receiving curative-intent radiation therapy during the COVID-19 pandemic: Report from a multicenter New York area institution. Adv Radiat Oncol. 2020;5:621–627. doi: 10.1016/j.adro.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwamm L.H., Chumbler N., Brown E. Recommendations for the implementation of telehealth in cardiovascular and stroke care: A policy statement from the American Heart Association. Circulation. 2017;135:e24–e44. doi: 10.1161/CIR.0000000000000475. [DOI] [PubMed] [Google Scholar]
- 5.American Telemedicine Association. Available at: https://www.americantelemed.org/resource/why-telemedicine/. Accessed May 23, 2020.
- 6.Dorsey E.R., Topol E.J. State of telehealth. N Engl J Med. 2016;375:154–161. doi: 10.1056/NEJMra1601705. [DOI] [PubMed] [Google Scholar]
- 7.Wade V.A., Eliott J.A., Hiller J.E. Clinician acceptance is the key factor for sustainable telehealth services. Qual Health Res. 2014;24:682–694. doi: 10.1177/1049732314528809. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Medicare & Medicaid Services Medicare Telemedicine Health Care Provider Fact Sheet. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet Available at:
- 9.US Department of Health and Human Services OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency. https://www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html Available at:
- 10.The Editorial Board The Doctor Will Zoom You Now. https://www.wsj.com/articles/the-doctor-will-zoom-you-now-11587935588 Available at:
- 11.Sabin S. Experts: Efforts to Expand Telehealth in Pandemic Still Leaving Rural U.S. Behind. https://morningconsult.com/2020/03/24/telehealth-coronavirus-rural-america/ Available at:
- 12.Hamilton E., Van Veldhuizen E., Brown A., Brennan S., Sabesan S. Telehealth in radiation oncology at the Townsville Cancer Centre: Service evaluation and patient satisfaction. Clin Transl Radiat Oncol. 2019;15:20–25. doi: 10.1016/j.ctro.2018.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rising K.L., Ward M.M., Goldwater J.C., Bhagianadh D., Hollander J.E. Framework to advance oncology-related telehealth. JCO Clin Cancer Inform. 2018;2:1–11. doi: 10.1200/CCI.17.00156. [DOI] [PubMed] [Google Scholar]
- 14.Zarcos-Pedrinaci I., Fernandez-Lopez A., Tellez T. Factors that influence treatment delay in patients with colorectal cancer. Oncotarget. 2017;8:36728–36742. doi: 10.18632/oncotarget.13574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paul C., Carey M., Anderson A. Cancer patients' concerns regarding access to cancer care: perceived impact of waiting times along the diagnosis and treatment journey. Eur J Cancer Care (Engl) 2012;21:321–329. doi: 10.1111/j.1365-2354.2011.01311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wyatt R.M., Jones B.J., Dale R.G. Radiotherapy treatment delays and their influence on tumour control achieved by various fractionation schedules. Br J Radiol. 2008;81:549–563. doi: 10.1259/bjr/94471640. [DOI] [PubMed] [Google Scholar]
- 17.Bleustein C., Rothschild D.B., Valen A., Valatis E., Schweitzer L., Jones R. Wait times, patient satisfaction scores, and the perception of care. Am J Manag Care. 2014;20:393–400. [PubMed] [Google Scholar]
- 18.John B.V., Love E., Dahman B. Use of telehealth expedites evaluation and listing of patients referred for liver transplantation. Clin Gastroenterol Hepatol. 2020;18:1822–1830. doi: 10.1016/j.cgh.2019.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ansary A.M., Martinez J.N., Scott J.D. The virtual physical exam in the 21st century. J Telemed Telecare. 2019 doi: 10.1177/1357633X19878330. [DOI] [PubMed] [Google Scholar]
- 20.American Academy of Neurology Telemedicine and COVID-19 Implementation Guide. https://www.aan.com/siteassets/home-page/tools-and-resources/practicing-neurologist%97administrators/telemedicine-and-remote-care/20-telemedicine-and-covid19-v103.pdf Available at:
- 21.Orlando J.F., Beard M., Kumar S. Systematic review of patient and caregivers' satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients' health. PLoS One. 2019;14 doi: 10.1371/journal.pone.0221848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lorie A., Reinero D.A., Phillips M., Zhange L., Riess H. Culture and nonverbal expressions of empathy in clinical settings: A systematic review. Patient Educ Couns. 2017;100:411–424. doi: 10.1016/j.pec.2016.09.018. [DOI] [PubMed] [Google Scholar]
- 23.Ruberton P.M., Huynh H.P., Miller T.A., Kruse E., Chancellor J., Lyubomirsky S. The relationship between physician humility, physician-patient communication, and patient health. Patient Educ Couns. 2016;99:1138–1145. doi: 10.1016/j.pec.2016.01.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.