Highlights
-
•
Symptoms of anxiety were more prevalent among farmer, people staying out of Beijing during the epidemic, poor sleep, and those who did not exercise.
-
•
The status of anxiety symptoms were significantly higher than usually, but it were lower than that during Ebola, influenza A and SARS outbreak.
-
•
Knowledge and perceptions of COVID-19, physical activity, and sleeping time are the main factors affecting anxiety.
Keywords: Anxiety, During the COVID-19 outbreak, Prevalence, Adults, Beijing
Abstract
Background
The outbreak of COVID-19 poses a challenge to psychological resilience. The aim of this study was to evaluate the prevalence of anxiety and identify risk and protective factors associated with the presence of anxiety symptoms in the face of COVID-19 among adults.
Methods
A cross-sectional online survey was conducted in adults from March 2nd to March 16th 2020. The self-rating anxiety scale (SAS) was used to measure the status of anxiety. Unconditional multivariate logistic regression was performed to identify the factors associated with anxiety.
Results
Among the 7144 respondents, 9.3% met the criteria for anxiety risk based on the SAS. Symptoms of anxiety were more prevalent among farmer (OR=1.43, 95%CI: 1.03-1.99), respondents lived in urban out of Beijing during the COVID-19 outbreak (OR=1.73, 95%CI: 1.14-2.63), and slept less than six hours per day (OR=2.64, 95%CI: 1.96-3.57). Compared to participants who didn’t exercise, a lower risk of anxiety was observed in those exercised 30-60 minutes/day (OR=0.62, 95%CI: 0.41-0.94) and more than 60 minutes/day (OR=0.57, 95%CI: 0.37-0.88). And compared with participants whose knowledge and perceptions of COVID-9 scores in lower quartile, the OR (95%CI) for the second, third and upper quartile were 0.58 (0.46, 0.73), 0.48 (0.37, 0.61) and 0.42(0.33, 0.52), respectively.
Limitations
No diagnostic interview for mental disorders was administered in the original studies limiting analysis of sensitivity and specificity of the Swahili PHQ-9.
Conclusion
There was a high level of anxiety in the face of COVID-19 among adults. The results point to characteristics of adults in particular need for attention to anxiety and suggest possible targets for intervention such as strengthening of physical activity and knowledge and perceptions of COVID-19.
1. Introduction
In December 2019, a cluster of pneumonia patients were reported in Wuhan city, Hubei province of China. On 7 January 2020, authorities in China confirmed that they had identified a novel (new) coronavirus as the cause of the pneumonia (Zhu et al., 2020), which is an infectious disease named Coronavirus disease (COVID-19) (Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention, 2020). The outbreak of COVID-19 was declared to be a pandemic due to the speed and scale of transmission. As of 15 May 2020, a total of 4,338,658 cases of 2019-nCov had been confirmed and caused 297,119 deaths in the world reported by the World Health Organization (WHO) (World Health Organization, 2020). The epidemic in China has been effectively controlled thanks to a series of strategic measures and the efforts of the whole society (Pan et al., 2020).
With the introducing measures to restrict movement as part of efforts to reduce the number of people infected with COVID-19, more and more of people are making huge changes to their daily routines. The new realities are working at home, home-schooling of children, and lacking of getting together with colleagues and friends. It might be challenging for most of the people in adapting the lifestyle changes, as well as managing the fear of the virus can be transmitted from one individual to another and prolonged home isolation. Several studies have reported the mental health problems of adolescents (Xiao et al., 2020; Zhou et al., 2020), COVID-19 patients (Lei et al., 2020), people in Hubei province (Ahmed et al., 2020), public and health care workers (Bao et al., 2020; Huang and Zhao, 2020; Kang et al., 2020; Wang et al., 2020) during the outbreak of COVID-19. Facing with a public health emergency, the public usually presents varying degrees of psychological response to the epidemic situation. If these reactions cannot be alleviated in time, they might lead to further irrational behaviors, such as the panic buying of materials during the outbreak of severe acute respiratory syndrome (SARS), the rush for salt during the Fukushima nuclear leak, and more serious violent behavior (Li et al., 2014).
Anxiety is one of the common negative reactions during the epidemics of infectious diseases (Steven S Coughlin, 2012; Peng et al., 2010). However, little epidemiological data available for general adults currently, and how best to respond to the challenges of mental health care during the outbreak is unknown (Xiang et al., 2020). Therefore, the aim of this study is to evaluate the prevalence of anxiety and identify risk and protective factors associated with the presence of anxiety symptoms in the face of COVID-19 among Beijing adults. This may assist healthcare professionals in safeguarding the psychological wellbeing of the general population and provide a basis for carrying out relevant health education to strengthen the prevention and control of diseases in the future.
2. Methods
2.1. Subjects
This was a cross-sectional online survey conducted on Wenjuanxing platform (https://www.wjx.cn) to assess mental health problems among adults in the face of COVID-19. From March 2nd to March 16th 2020, 7191 respondents aged 18 and over filled out and submitted the online questionnaire. A total of 47 questionnaires with data missing on the anxiety scale were deleted. Finally, 7144 participants were included in the following analysis. All the respondents provided online informed consent to participate in this study.
2.2. Patient and public involvement statement
All the respondents were recruited online. This study conformed to the requirements of medical ethics, and the questionnaire didn't involve any personal information such as name, which conforms to the requirements of relevant laws and regulations and competent authorities.
2.3. Measures
Data was collected using a self-made questionnaire consisting of three parts. The first part was socio-demographic information, including gender, living place when the outbreak occurred, census register, birthdate, occupation, education, exercise and sleeping time. The second part included knowledge and perceptions of COVID-19, attitudes and behaviors to COVID-19. The questions about the etiology of COVID-19, epidemiology information, prevention and control measures against COVID-19 were asked to evaluate the respondents’ knowledge and perceptions of COVID-19. It was composed of 13 single choices and 10 multiple choice questions, one point was awarded for each correct answer on each choice, and the total score was 83 points. The third part was screening instruments for anxiety and depression.
Self-rating anxiety scale (SAS) (Zung, 1971), consisting of 20 items, was used to evaluate the anxiety symptoms for participants. The Cronbach's alpha of SAS is 0.834 in our study and we think there's good internal consistency reliabilities. A 4-point response scale consisting of “none or only a little of the time” (coded as 1), “some of the time” (coded as 2), “good part of the time” (coded as 3), and “most or all of the time” (coded as 4) was used. Items 5, 9, 13, 17 and 19 were reversed scored. The time frame was “during the last two weeks”. Scale scores were calculated by summary items and then transformed into a standard score (multiplied by 1.25) range from 25 to 100, with higher scores indicating severer levels of anxiety (Olatunji et al., 2006). Here, the cutoff values of anxiety are as follows: normal range “<50”, mild level “50–59”, moderate anxiety level “60–69”, severe anxiety level “≥70”.
2.4. Statistical analyses
Scores of knowledge and perceptions of COVID-19 were calculated by summary the right answers of the question. A high score represents a high level of knowledge. Means and standard deviations (SD), though the distributions of the scores were skewed, had been presented in order to compare with other published data.
All statistical analyses were performed using the Statistical Analysis System (Version 9.4). The characteristics of participants were presented as percentages for categorical variables and mean±SD for continuous variables. Spearman correlation analysis was used to identify the correlation between anxiety scores and knowledge and perceptions of COVID-19 scores. The multivariate logistic regression was applied to calculate the odds ratio (OR) and 95% confidence interval (95%CI) to evaluate the factors that were related to the risk of anxiety or not. Statistical inferences were two-sided and P value less than 0.05 were considered as statistically significant.
2.5. Quality control
To ensure quality, the same IP address can only be answered once. The answering time of each questionnaire was automatically monitored in the background of the network questionnaire. If the answering time of the survey was less than 200 s, it would be regarded as invalid.
3. Results
3.1. Characteristics of the participants
As shown in Table 1 , among the 7144 participants, 69.4% were female. The mean age of participants was 41.23±5.67 years (range 19–72) and the majority of participants were in the age of 30 to 45 (75%). Over 60% of participants had a college degree or higher. The vast majority of participants (68.1%) were living in urban of Beijing and 27.0% were living in rural of Beijing during the COVID-19 outbreak. Nearly 65% of participants exercised at least 30 min per day, and 57.0% of participants slept six to eight hours per day. The mean±SD score for knowledge and perceptions of COVID-19 was 73.6 ± 6.4.
Table 1.
Characteristics of the participants (N = 7144), n (%).
| Variables | Urban (n = 5057) | Rural (n = 2087) | Total | P |
|---|---|---|---|---|
| Sex | 0.017 | |||
| Male | 1505 (29.8%) | 681 (32.6%) | 2186 (30.6%) | |
| Female | 3552 (70.2%) | 1406 (67.4%) | 4958 (69.4%) | |
| Age group | 0.024 | |||
| 18–29 | 108 (2.1%) | 61 (2.9%) | 169 (2.4%) | |
| 30–44 | 3766 (74.5%) | 1594 (76.4%) | 5630 (75.0%) | |
| 45–59 | 1164 (23.0%) | 424 (20.3%) | 1588 (22.2%) | |
| 60– | 19 (0.4%) | 8 (0.4%) | 27 (0.4%) | |
| Area | 0.003 | |||
| Beijing | 4387 (86.7%) | 1864 (89.3%) | 6251 (87.5%) | |
| Other | 670 (13.3%) | 223 (10.7%) | 893 (12.5%) | |
| Education | <0.001 | |||
| Primary | 21 (0.4%) | 53 (2.5%) | 74 (1.0%) | |
| Junior | 424 (8.4%) | 659 (31.6%) | 1083 (15.2%) | |
| Senior | 925 (18.3%) | 618 (29.6%) | 1543 (21.6%) | |
| College | 3448 (68.2%) | 722 (34.6%) | 4170 (58.4%) | |
| Postgraduate | 239 (4.7%) | 35 (1.7%) | 274 (3.8%) | |
| Occupation | <0.001 | |||
| Medicine | 252 (5.0%) | 38 (1.8%) | 290 (4.1%) | |
| Staff | 3140 (62.1%) | 789 (37.8%) | 3929 (55.0%) | |
| Self-employment/ Employee | 661 (13.1%) | 400 (19.2%) | 1061 (14.9%) | |
| Farmer | 93 (1.8%) | 404 (19.4%) | 497 (7.0%) | |
| Other | 911 (18.0%) | 456 (21.9%) | 1367 (19.1%) | |
| Excise | 0.002 | |||
| No | 162 (3.2%) | 55 (2.6%) | 217 (3.0%) | |
| < 30 min | 1671 (33.0%) | 654 (31.3%) | 2325 (32.5%) | |
| 30–60 min | 2191 (43.3%) | 869 (41.6%) | 3060 (42.8%) | |
| > 60 min | 1033 (20.4%) | 509 (24.4%) | 1542 (21.6%) | |
| Sleeping time | <0.001 | |||
| < 6 h | 237 (4.7%) | 76 (3.6%) | 313 (4.4%) | |
| 6–8 h | 2940 (58.1%) | 1133 (54.3%) | 4073 (57.0%) | |
| 8–10 h | 1770 (35.0%) | 801 (38.4%) | 2571 (36.0%) | |
| > 10 h | 110 (2.2%) | 77 (3.7%) | 187 (2.6%) | |
| Knowledge | <0.001 | |||
| Quartile 1 | 1024 (20.3%) | 741 (35.5%) | 1765 (24.7%) | |
| Quartile 2 | 972 (19.2%) | 447 (21.4%) | 1419 (19.9%) | |
| Quartile 3 | 1056 (20.9%) | 392 (27.1%) | 1448 (20.3%) | |
| Quartile 4 | 2005 (39.7%) | 507 (24.3%) | 2512 (35.2%) | |
| Anxiety | 0.004 | |||
| Normal | 4620 (91.4%) | 1857 (89.0%) | 6477 (90.7%) | |
| Mild | 359 (7.1%) | 176 (8.4%) | 535 (7.5%) | |
| Moderate | 59 (1.2%) | 42 (2.0%) | 101 (1.4%) | |
| Severe | 19 (0.4%) | 12 (0.6%) | 31 (0.4%) |
3.2. Proportion of participants with anxiety
The mean±SD anxiety score on SAS was 38.0 ± 8.7 and the overall proportion of participants with anxiety was 9.3%. According to the recommended cutoffs for the SAS, 7.5%, 1.4% and 0.4% of the participants had mild, moderate and severe anxiety symptoms, respectively. Participants with the age over 60 were almost two times more likely than participants with the age of 30 to 44 (18.5% versus 8.8%) to report anxiety. The proportion of participants lived in rural of other province with anxiety were twice than participants lived in urban of Beijing during the COVID-19 outbreak (17.7% versus 8.3%). The farmer had a much higher proportion of anxiety (17.1%) than those of other professionals. Participants who did not exercise were twice more likely to suffer from anxiety than those exercised at least 30 min a day (15.2% versus 7.7%). The proportion of respondents - who slept less than six hours a day reported anxiety was 21.7% (Table 2 ).
Table 2.
Distribution of anxiety according to demographic characteristics of the participants.
| Demographics | Score (mean±sd) | Normal N (%) | Mild N (%) | Moderate N (%) | Severe N (%) |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 38.0 ± 8.8 | 1989 (91.0%) | 154 (7.0%) | 34 (1.6%) | 9 (0.4%) |
| Female | 38.0 ± 8.7 | 4488 (90.5%) | 381 (7.7%) | 67 (1.4%) | 22 (0.4%) |
| Age group | |||||
| 18–29 | 38.5 ± 10.9 | 142 (84.0%) | 21 (12.4%) | 3 (1.8%) | 3 (1.8%) |
| 30–44 | 38.0 ± 8.6 | 4887 (91.2%) | 381 (7.1%) | 71 (1.3%) | 21 (0.4%) |
| 45–59 | 38.0 ± 8.8 | 1426 (89.8%) | 130 (8.2%) | 25 (1.6%) | 7 (0.4%) |
| 60– | 41.5 ± 10.7 | 22 (81.5%) | 3 (11.1%) | 2 (2.0%) | 0 (0.0%) |
| Area | |||||
| Urban-Beijing | 37.5 ± 8.5 | 4460 (91.7%) | 337 (6.9%) | 53 (1.1%) | 16 (0.3%) |
| Rural-Beijing | 39.0 ± 8.7 | 1727 (89.5%) | 158 (8.2%) | 34 (1.8%) | 10 (0.5%) |
| Urban-other | 39.7 ± 10.6 | 160 (83.8%) | 22 (11.5%) | 6 (3.1%) | 3 (1.6%) |
| Rural-other | 41.0 ± 11.0 | 130 (82.3%) | 18 (11.4%) | 8 (5.1%) | 2 (1.3%) |
| Education | |||||
| Primary | 41.2 ± 10.9 | 60 (81.1%) | 10 (13.5%) | 3 (4.1%) | 1 (1.4%) |
| Junior | 40.7 ± 9.2 | 933 (86.2%) | 107 (9.9%) | 32 (3.0%) | 11 (1.0%) |
| Senior | 38.5 ± 8.6 | 1408 (91.3%) | 106 (6.9%) | 22 (1.4%) | 7 (0.5%) |
| College | 37.2 ± 8.3 | 3833 (91.9%) | 291 (7.0%) | 38 (0.9%) | 8 (0.2%) |
| Postgraduate | 36.8 ± 10.6 | 243 (88.7%) | 21 (7.7%) | 6 (2.2%) | 4 (1.5%) |
| Occupation | |||||
| Medicine | 37.3 ± 7.8 | 270 (93.1%) | 18 (6.2%) | 2 (0.7%) | 0 (0.0%) |
| Staff | 37.7 ± 8.6 | 3588 (91.3%) | 274 (7.0%) | 50 (1.3%) | 17 (0.4%) |
| self-employment | 38.8 ± 8.7 | 966 (91.1%) | 77 (7.3%) | 14 (1.3%) | 4 (0.4%) |
| Farmer | 40.6 ± 9.8 | 412 (82.9%) | 60 (12.1%) | 20 (4.0%) | 5 (1.0%) |
| Other | 38.5 ± 8.4 | 1241 (90.8%) | 106 (7.8%) | 15 (1.1%) | 5 (0.4%) |
| Excise | |||||
| No | 40.6 ± 9.4 | 184 (84.8%) | 25 (11.5%) | 7 (3.2%) | 1 (0.5%) |
| < 30 min | 39.2 ± 9.0 | 2047 (88.0%) | 227 (9.8%) | 41 (1.8%) | 10 (0.4%) |
| 30–60 min | 37.4 ± 8.5 | 2819 (92.1%) | 191 (6.2%) | 36 (1.2%) | 14 (0.5%) |
| > 60 min | 37.1 ± 8.4 | 1427 (92.5%) | 92 (6.0%) | 17 (1.1%) | 6 (0.4%) |
| Sleeping time | |||||
| < 6 h | 43.0 ± 9.4 | 245 (78.3%) | 51 (16.3%) | 14 (4.5%) | 3 (1.0%) |
| 6–8 h | 37.9 ± 8.7 | 3712 (91.1%) | 294 (7.2%) | 46 (1.1%) | 21 (0.5%) |
| 8–10 h | 37.5 ± 8.4 | 2353 (91.5%) | 176 (6.9%) | 36 (1.4%) | 6 (0.2%) |
| > 10 h | 39.6 ± 9.3 | 167 (89.3%) | 14 (7.5%) | 5 (2.7%) | 1 (0.5%) |
3.3. Correlations between scores of anxiety and perceptions of COVID-19
The mean±SD anxiety score on SAS was 38.0 ± 8.8 for male and 38.0 ± 8.7 for female. There was a significant negative correlation between the SAS scores and the knowledge and perceptions of COVID-19 scores (r = −0.23, P<0.001). As the score of knowledge and perceptions of COVID-9 increased, the anxiety scores decreased. We divided the score of knowledge and perceptions of COVID-19 into four groups according to the quartile, and found that the results were similar for respondents lived in urban and rural when the outbreak occurred (Fig. 1 ).
Fig. 1.
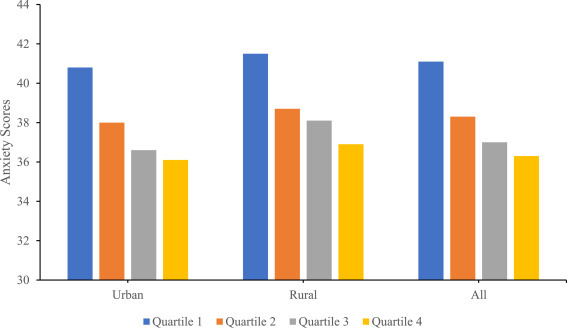
Distribution of anxiety score according to the quartile of knowledge and perceptions of COVID-19.
3.4. Factors associated with anxiety symptoms
Table 3 presents a number of potential factors which were included in the univariate and multivariate logistic regression analysis for anxiety symptoms of participants. Participants in age groups of 30–44 (OR=0.57, 95%CI: 0.36–0.89) and 45–59 (OR=0.61, 95%CI: 0.38–0.98) had a lower likelihood of experiencing anxiety symptoms than those in the age of 18 to 29. Those slept less than six hours per day were 2.6 times more likely to report anxiety symptoms than participants who slept six to eight hours per day (OR=2.64, 95%CI: 1.96–3.57). There was a little higher likelihood of anxiety symptoms in farmer (OR=1.43, 95%CI: 1.03–1.99), and participants who were living in urban out of Beijing during the COVID-19 outbreak (OR=1.73, 95%CI: 1.14–2.63). Compared to participants who did not exercise, a lower likelihood of anxiety symptoms was observed in those exercised 30–60 min/day (OR=0.62, 95%CI: 0.41–0.94) and more than 60 min/day (OR=0.57, 95%CI: 0.37–0.88). Besides, compared with participants whose knowledge and perceptions of COVID-9 scores in the lower quartile, a lower likelihood of anxiety symptoms was observed in participants with scores in the second quartile (OR=0.58, 95%CI: 0.46–0.73), third quartile (OR=0.48, 95%CI: 0.37–0.61) and upper quartile (OR=0.42, 95%CI: 0.33–0.52).
Table 3.
Factors associated with anxiety: univariate and multivariable analyses.
| Variables | Crude OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| Sex | ||
| Male | 1 | 1 |
| Female | 1.06 (0.89, 1.26) | 1.13 (0.94, 1.35) |
| Age group | ||
| 18–29 | 1 | 1 |
| 30–44 | 0.51 (0.33, 0.78)* | 0.57 (0.36, 0.89)* |
| 45–59 | 0.60 (0.38, 0.93)* | 0.61 (0.38, 0.98)* |
| 60– | 1.20 (0.42, 3.43) | 0.88 (0.29, 2.67) |
| Area | ||
| Urban-Beijing | 1 | 1 |
| Rural-Beijing | 1.29 (1.08, 1.54)* | 1.02 (0.83, 1.25) |
| Urban-other | 2.13 (1.43, 3.17)** | 1.73 (1.14, 2.63)* |
| Rural-other | 2.37 (1.55, 3.60)** | 1.50 (0.95, 2.36) |
| Education | ||
| Primary | 1 | 1 |
| Junior | 0.69 (0.38, 1.26) | 0.94 (0.50, 1.78) |
| Senior | 0.41 (0.22, 0.76)* | 0.77 (0.40, 1.47) |
| College | 0.38 (0.21, 0.68)* | 0.79 (0.41, 1.50) |
| Postgraduate | 0.55 (0.27, 1.09) | 0.91 (0.43, 1.92) |
| Occupation | ||
| Medicine | 0.78 (0.49, 1.24) | 0.88 (0.54, 1.41) |
| Staff | 1 | 1 |
| Self-employment/employee | 1.04 (0.82, 1.31) | 0.89 (0.68, 1.16) |
| Farmer | 2.17 (1.68, 2.81)** | 1.43 (1.03, 1.99)* |
| Other | 1.07 (0.86, 1.32) | 0.90 (0.71, 1.15) |
| Excise | ||
| No | 1 | 1 |
| < 30 min | 0.76 (0.51, 1.12) | 0.90 (0.60, 1.36) |
| 30–60 min | 0.48 (0.32, 0.71)** | 0.62 (0.41, 0.94)* |
| > 60 min | 0.45 (0.30, 0.68)** | 0.57 (0.37, 0.88)* |
| Sleeping time | ||
| < 6 h | 2.86 (2.14, 3.82)** | 2.64 (1.96, 3.57)** |
| 6–8 h | 1 | 1 |
| 8–10 h | 0.95 (0.80, 1.14) | 0.93 (0.78, 1.11) |
| > 10 h | 1.23 (0.77, 1.98) | 1.05 (0.64, 1.72) |
| Knowledge | ||
| Quartile 1 | 1 | 1 |
| Quartile 2 | 0.51 (0.41, 0.64)** | 0.58 (0.46, 0.73)** |
| Quartile 3 | 0.42 (0.33, 0.53)** | 0.48 (0.37, 0.61)** |
| Quartile 4 | 0.38 (0.31, 0.47)** | 0.42 (0.33, 0.52)** |
**P<0.001.
*P <0.05.
4. Discussion
The prevalence of anxiety (9.3%) and mean standard SAS score (38.0 ± 8.7) among our study participants was close to that reported in previous study that applied SAS to assess anxiety symptoms among people affected by versus people unaffected by quarantine during the COVID-9 epidemic in southwestern china (8.3%, 36.47±9.15) (Lei et al., 2020), and among the general population which sample size was 600 (6.33%, 36.92±7.33) (Wang et al., 2020). However, the prevalence was higher than that reported in studies of other time. The prevalence rates of anxiety in participants older than 60 years was 18.5% in this study, which is nearly threefold than the elderly in Xicheng district (6.3%) reported by Xiao, et al. (2014)). It shows that people's anxiety symptoms increased during the outbreak. On the contrary, the prevalence rates in our study were significantly lower than the results of Wang, et al., which reported that the prevalence of moderate to severe anxiety symptoms was 28.8% (Wang et al., 2020). Our results may differ owing to the different periods, their data were collected from 31 January to 2 February 2020, which WHO just declared the public health emergency of international concern and two weeks into the outbreak of COVID-19, while to March the outbreak had been take a turn for the better after the government taking quick and strong measures to ensure the safety of citizens and updating timely information of COVID-19, timely sharing information is an effective way to reduce public panic (Song and Karako, 2020); additionally the variation might be due to differences in the measurement, they use the anxiety and stress scale (DASS-21) to measure anxiety symptoms and we use SAS. Dunstan et al. reported that the cut-off point in the SAS used for classifying anxiety (raw scores of 50 and above) having a much lower sensitivity (31%) than the diagnostic sensitivity of DASS (74% for mild anxiety) (Dunstan et al., 2017). In spite of the existed variation, the status of anxiety symptoms among adults during the outbreak of COVID-19 were significantly higher than usual.
Compared with other health emergencies, the overall prevalence of anxiety symptoms in this study was relatively lower. For example, the prevalence rates of anxiety symptoms were 48% in general public after over one year of Ebola outbreak (Jalloh et al., 2018), 16% of the public felt anxiety during the influenza A outbreak (Bults et al., 2011), 57% of the general population reported irritability and 73% reported low mood during the outbreak of SARS (Lee et al., 2005), and 39% of residents reported anxiety symptoms about avian influenza in France (Saadatian-Elahi et al., 2010). Possible reasons for this difference might be as follows. First, anxiety was measured by different tools, for the study of SARS (Lee et al., 2005) and influenza A (Bults et al., 2011) outbreak, anxiety was evaluated by the respondents’ subjective feeling, and in the study of Ebola, Patient Health Questionnaire-4 (PHQ-4) was used to measure the symptoms of anxiety (Jalloh et al., 2018), while SAS was used in our study. Second, the Chinese government had swift response efforts, and taking quick and strong strategy and measures to ensure the safety of citizens, such as early identification and isolation of suspected and confirmed cases, establishment of isolation units and hospitals, contact tracing and monitoring, collection of biological samples from patients, timely provision of medical supplies and external expert teams to Hubei province. (Wang et al., 2020; Wang Xiaoyu, 2020) and updating timely information of COVID-19 played an important role. Third, the participants had a higher knowledge and perceptions of COVID-19 in our study, with the mean score of 73.6 ± 6.4 (the total score is 83), and the main channels for participants to acquire COVID-19 information were the news media (91.5%) and government agencies and professional authorities (89.8%). The knowledge of diseases in general public plays an important role in responses to an epidemic crisis ((Hong and Collins, 2006; Saadatian-Elahi et al., 2010), therefore, the timely release of professional, authoritative information on the epidemic by the government and the media had played an important role in the prevention and control of COVID-19. Lastly, the National Health Commission of China issued the notification of basic principles on the emergency psychological crisis intervention for the COVID-19 on Jan 26, 2020 (Disease Control and Prevention, 2020). And the psychological assistance system was quickly established, which might be an effective way to alleviate the public's negative emotions.
Similar to some previous studies, our results indicated that age, sleeping time, exercise, occupation, knowledge and perceptions of COVID-19 are associated with anxiety symptoms. Consistent with the previous results that people with sleeping problems were predisposed to anxiety (Cox et al., 2018; Difrancesco et al., 2019; Van Mill et al., 2010; Xiao et al., 2020), we found that participants slept less than six hours per day were 2.6 times more likely to report anxiety symptoms than participants who slept six to eight hours per day (OR=2.64, 95%CI: 1.96–3.57). Anxiety affects sleep quality also, the combination of anxiety and sleep disorders make it more difficult to fall asleep (Alvaro et al., 2013; Johnson et al., 2006). Additionally, physical exercise was also proved as an important risk factor for anxiety (Gong et al., 2014), approximately 35% of participants in our study did not exercise or exercised less than 30 min per day, compared to those, a lower likelihood of anxiety was observed in participant exercised 30–60 min/day (OR=0.62, 95%CI: 0.41–0.94) and more than 60 min/day (OR=0.57, 95%CI: 0.37–0.88). Therefore, we suggest that people can alleviate anxiety through exercise activities.
Moreover, we found that participants who lived in urban out of Beijing during the COVID-19 outbreak had a significantly higher likelihood of anxiety than those lived in Beijing urban (OR=1.73, 95%CI: 1.14–2.63), which is consistent with precious study (Zhou et al., 2020). However, due to the number of participants lived in urban out of Beijing during the outbreak were much smaller than those lived in Beijing urban, the results may need to be further verified. Additionally, our results showed that farmer had a higher likelihood of anxiety symptoms than staff (OR=1.43, 95%CI: 1.03–1.99), which might be closely related to their poor economic situation. Different from the results that the female had suffered from greater anxiety disorder (Liu et al., 2015), there was no difference in prevalence of anxiety between male and female in this study. Furthermore, our results indicated that the level of knowledge and perceptions of COVID-19 was a protective factor in the face of outbreak, compared with participants whose knowledge and perceptions of COVID-9 scores in lower quartile, a lower risk of anxiety symptoms was observed in participants with scores in second quartile (OR=0.58, 95%CI: 0.46–0.73), third quartile (OR=0.48, 95%CI: 0.37–0.61) and upper quartile (OR=0.42, 95%CI: 0.33–0.52), which means that strengthening the public's knowledge of COVID-19 can reduce the anxiety symptoms. This is consistent with the results of (Zhou et al. 2020 and Wang et al. 2020). However, false reports and false information can also aggravate anxiety and depressive symptoms in the general population. Therefore, government and authorities need to provide accurate health information to reduce the impact of the rumors during the epidemic (Rubin and Wessely, 2020).
4.1. Limitation
This study has several limitations. First, since this was a cross-sectional online survey conducted on Wenjuanxing platform, there was existing selection bias and the results was less generalizable to all the adults. There was study showed that during the outbreak, young people would have a higher risk of anxiety than older people (Wang et al., 2020), and with the development of society, more and more people will have a higher education. Our results would provide a basis for carrying out relevant health education to strengthen the prevention and control of diseases for population with similar characteristics in the future. It would be better to cover as wide population as possible to get more accurate results in the future. Second, the anxiety symptoms were measured by self-reported which may not be aligned with the assessment by mental health professionals. Last, we did not consider other factors which may confound the outcomes, such as the social support of family and friends, marital status, personal/family monthly income, diseases, and some other lifestyle factors like smoking and drinking, which were commonly considered to be associated with anxiety. Since majority of the participants’ age was under 45 which were lower risk in prevalence of illness, we think that there might little difference in the results without the illness status. Further studies of those issues are needed in the future. However, the strength of this study is its large number of respondents and its scientific importance for the healthcare professionals in safeguarding the psychological wellbeing of the general population.
5. Conclusion
This study aimed to evaluate the prevalence of anxiety and identify risk and protective factors associated with the presence of anxiety symptoms among Beijing adults in the face of COVID-19. The results showed that the prevalence of anxiety was increased during the outbreak of COVID-19, and the main factors associated with anxiety included age, area, occupation, excise, sleeping time, knowledge and perceptions of COVID-19. The next step in preventing and controlling the COVID-19 should be focused on public's mental health.
Role of the funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sections.
Availability of data and material
Data and survey materials will be made available upon request.
CRediT authorship contribution statement
Juan Xia: Formal analysis, Writing - original draft. Yi Meng: Data curation. Fuyuan Wen: Data curation. Hui Li: Data curation. Kai Meng: Project administration, Writing - review & editing. Ling Zhang: Project administration, Writing - review & editing.
Declaration of Competing Interest
All authors declare no competing interests.
Acknowledgments
We thank all the participants and staff for their efforts in conducting and collecting data throughout this investigation.
References
- Alvaro P.K., Roberts R.M., Harris J.K. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36(7):1059–1068. doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed M.Z., Ahmed O., Aibao Z., Hanbin S., Siyu L., Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bults M., Beaujean D.J., de Zwart O., Kok G., van Empelen P., van Steenbergen J.E., Richardus J.H., Voeten H.A. Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the influenza A (H1N1) pandemic in the Netherlands: results of three consecutive online surveys. BMC Public Health. 2011;11:2. doi: 10.1186/1471-2458-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox R.C., Sterba S.K., Cole D.A., Upender R.P., Olatunji B.O. Time of day effects on the relationship between daily sleep and anxiety: an ecological momentary assessment approach. Behav. Res. Ther. 2018;111:44–51. doi: 10.1016/j.brat.2018.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Difrancesco S., Lamers F., Riese H., Merikangas K.R., Beekman A., van Hemert A.M., Schoevers R.A., Penninx B. Sleep, circadian rhythm, and physical activity patterns in depressive and anxiety disorders: a 2-week ambulatory assessment study. Depress Anxiety. 2019;36(10):975–986. doi: 10.1002/da.22949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Disease Control and Prevention, 2020. National Health Commission of China Principles for Emergency Psychological Crisis Intervention for the New Coronavirus Pneumonia. http://www.nhc.gov.cn/jkj/s3577/202001/6adc08b966594253b2b791be5c3b9467.shtml (accessed 26 Jan 2020)
- Dunstan D.A., Scott N., Todd A.K. Screening for anxiety and depression: reassessing the utility of the Zung scales. BMC Psychiatry. 2017;17(1):329. doi: 10.1186/s12888-017-1489-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(2):145–151. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. [DOI] [PubMed] [Google Scholar]
- Gong Y., Han T., Chen W., Dib H.H., Yang G., Zhuang R., Chen Y., Tong X., Yin X., Lu Z. Prevalence of anxiety and depressive symptoms and related risk factors among physicians in China: a cross-sectional study. PLoS One. 2014;9(7) doi: 10.1371/journal.pone.0103242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong S., Collins A. Societal responses to familiar versus unfamiliar risk: comparisons of influenza and SARS in Korea. Risk Anal. 2006;26(5):1247–1257. doi: 10.1111/j.1539-6924.2006.00812. [DOI] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112954. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalloh M.F., Li W., Bunnell R.E., Ethier K.A., O'Leary A., Hageman K.M., Sengeh P., Jalloh M.B., Morgan O., Hersey S., Marston B.J., Dafae F., Redd J.T. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob. Health. 2018;3(2) doi: 10.1136/bmjgh-2017-00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson E.O., Roth T., Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J. Psychiatr. Res. 2006;40(8):700–708. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- Kang L., Li Y., Hu S., Chen M., Yang C., Yang B.X., Wang Y., Hu J., Lai J., Ma X., Chen J., Guan L., Wang G., Ma H., Liu Z. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7(3):e14. doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S., Chan L.Y., Chau A.M., Kwok K.P., Kleinman A. The experience of SARS-related stigma at Amoy Gardens. Soc. Sci. Med. 2005;61(9):2038–2046. doi: 10.1016/j.socscimed.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei L., Huang X., Zhang S., Yang J., Yang L., Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China. Med. Sci. Monit. 2020;26 doi: 10.12659/MSM.924609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L.J., Zhang D., Wu X.M. Progress on collective behavior in emergency public health events. Chin. J. Health Educ. 2014;30(7):631–633. CNKI:SUN:ZGJK.0.2014-07-017. [Google Scholar]
- Liu J., Yan F., Ma X., Guo H.L., Tang Y.L., Rakofsky J.J., Wu X.M., Li X.Q., Zhu H., Guo X.B., Yang Y., Li P., Cao X.D., Li H.Y., Li Z.B., Wang P., Xu Q.Y. Prevalence of major depressive disorder and socio-demographic correlates: results of a representative household epidemiological survey in Beijing, China. J. Affect. Disord. 2015;179:74–81. doi: 10.1016/j.jad.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olatunji B.O., Deacon B.J., Abramowitz J.S., Tolin D.F. Dimensionality of somatic complaints: factor structure and psychometric properties of the Self-Rating Anxiety Scale. J. Anxiety Disord. 2006;20(5):543–561. doi: 10.1016/j.janxdis.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Pan A., Liu L., Wang C., Guo H., Hao X., Wang Q., Huang J., He N., Yu H., Lin X., Wei S., Wu T. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323(19):1–9. doi: 10.1001/jama.2020.6130. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng E.Y., Lee M.B., Tsai S.T., Yang C.C., Morisky D.E., Tsai L.T., Weng Y.L., Lyu S.Y. Population-based post-crisis psychological distress: an example from the SARS outbreak in Taiwan. J. Formos. Med. Assoc. 2010;109(7):524–532. doi: 10.1016/S0929-6646(10)60087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin G.J., Wessely S. The psychological effects of quarantining a city. BMJ. 2020;368:m313. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- Saadatian-Elahi M., Facy F., Del Signore C., Vanhems P. Perception of epidemic's related anxiety in the general French population: a cross-sectional study in the Rhone-Alpes region. BMC Public Health. 2010;10:191. doi: 10.1186/1471-2458-10-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song P., Karako T. COVID-19: real-time dissemination of scientific information to fight a public health emergency of international concern. Biosci. Trends. 2020;14(1):1–2. doi: 10.5582/bst.2020.01056. [DOI] [PubMed] [Google Scholar]
- Coughlin S.S. Anxiety and depression: linkages with viral diseases. Public Health Rev. 2012;34(2):7. doi: 10.1007/BF03391675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Mill J.G., Hoogendijk W.J., Vogelzangs N., van Dyck R., Penninx B.W. Insomnia and sleep duration in a large cohort of patients with major depressive disorder and anxiety disorders. J. Clin. Psychiatry. 2010;71(3):239–246. doi: 10.4088/JCP.09m05218gry. [DOI] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- W. Xiaoyu, 2020. Coronavirus Outbreak: 444 New Cases Added on Friday. http://www.chinadaily.com.cn/a/202001/25/WS5e2bad63a310128217273336.html/ (updated 25 Jan 2020).
- Wang Y., Di Y., Ye J., Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 2020 doi: 10.1080/13548506.2020.1746817. Advance online publication. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2020. Coronavirus Disease (COVID-2019) Situation Report-116. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200515-covid-19-sitrep-116.pdf?sfvrsn=8dd60956_2/ (accessed 15 May 2020)
- Xiang Y.T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H., Zhang Y., Kong D., Li S., Yang N. The effects of social support on sleep quality of medical staff treating patients with Coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020;26 doi: 10.12659/MSM.923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao C.L., Chen B. Study on anxiety and depression of the elderly in Xicheng District, Beijing. Chin. General Pract. 2014;17(26):3113–3116. doi: 10.3969/j.issn.1007-9572.2014.26.018. [DOI] [Google Scholar]
- Zhou S.J., Zhang L.G., Wang L.L., Guo Z.C., Wang J.Q., Chen J.C., Lui M., Chen X., Chen J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry. 2020;29(6):749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W., China Novel Coronavirus Investigating and Research Team A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zung W.W. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data and survey materials will be made available upon request.


