Abstract
Background and Objectives:
The purpose of the investigation was to compare clinical results and diagnostic accuracy for conventional multiport laparoscopic lymph node biopsy (MPLB) and single-port laparoscopic lymph node biopsy (SPLB) operations at a single institution.
Methods:
A set of 20 SPLB patients operated on from October 2016 to May 2019 were compared to an historical series of 35 MPLB patients. Primary endpoints were the time of surgery, estimated blood loss, surgical conversion, length of stay and morbidity. The secondary endpoint was the diagnostic accuracy of the technique.
Results:
SPLB was completed laparoscopically in all cases. Two MPLB patients (5.7%) experienced a surgical conversion due to intraoperative difficulties. Duration of surgery was similar in SPLB and MPLB groups respectively (84 ± 31.7 min vs. 81.1 ± 22.2; P = .455). A shorter duration of hospital stay was shown for patients operated on by SPLB compared to the MPLB group (1.7 ± 0.9 days vs. 2.1 ± 1.2 days; P = .133). The postoperative course was uneventful in both groups. In 95% of the SPLB and 97.1% of the MPLB cases respectively, LLB achieved the necessary information for the diagnosis.
Conclusion:
SPLB has shown good procedural and postoperative outcomes as well as a high diagnostic yield, comparable to traditional MPLB. Therefore, our results show that this approach is safe and effective and can be an equally valid option to MPLB to obtain a diagnosis or to follow the progression of a lymphoproliferative disease. Further studies are necessary to support these results before its widespread adoption.
Keywords: Laparoscopy, Lymph node, Abdominal biopsy, Lymphoma
INTRODUCTION
Over the past 10 years, studies have analyzed the outcomes of laparoscopic lymph node biopsy (LLB) versus percutaneous biopsy (PB). Studies have shown over time a superiority of LLB versus core-needle PB. In fact, when lymphoproliferative disease is suspected and when isolated abdominal lymphadenopathy is poorly accessible to percutaneous biopsy, laparoscopy is the key tool for making the diagnosis.1–3
In the face of greater invasiveness, LLB makes it possible to make diagnoses in cases where PB is not feasible due to proximity of the parenchyma, large vessels, or hollow viscera. The laparoscopic single-port approach has recently appeared. It represents a further evolution in laparoscopic surgery, born with the aim of further reducing surgical trauma by reducing the number of abdominal incisions.
Since the advent of the first single-incision laparoscopic cholecystectomy described in 1995 by Navarra et al,4 various other abdominal interventions have benefited from this approach.5–8 Numerous retrospective series on the single-port approach report improved cosmesis and less pain, even if sometimes results are controversial.9–10 To date, there is no documentation of the use of the laparoscopic single-port technique for intra-abdominal lymphoma diagnosis. The main experiences are those described by gynecologists for pelvic lymphadenectomy for surgical staging of early uterine cancer.11–12
The purpose of this work is to verify, in addition to the technical feasibility, if these proposed advantages are also present in the single-port LLB and especially if the value of diagnostic yield is preserved. For this purpose, a series of 20 SPLB patients were compared with a historical series of 35 MPLB patients.
METHODS
In Oct 2016 laparoscopic single-port surgery was introduced at our division. Since then, all the SPLB procedures (n = 20) performed until May 2019 were collected in a prospective database. Patients details included sex, age, previous abdominal surgery, and associated comorbidities. Thirty-five MPLB patients operated on before the use of the single-port technique were chosen to serve as the control group. All patients included in the study underwent surgery to establish a diagnosis or to follow the progression of a lymphoma. Intra-abdominal lymphadenopathy was present on computed tomography scan in all patients. All the SPLB and MPLB procedures were performed by the same senior surgeon (MC).
The operative time, estimated blood loss, associated operations, surgical conversion, trocar addition, abdominal drain positioning, length of hospitalization, and postoperative morbidity were the parameters taken into consideration to assess the outcome of the procedure.
Surgical Technique
The surgical technique for MPLB has been described elsewhere.13 For SPLB technique a single-port with four-channels (Single port, Unimax Medical Systems Inc., Taipei, Taiwan) is inserted through the umbilicus. For dissection, a reusable 5-mm hook and a 5-mm reusable prebent grasper (Olympus Medical Systems, Hamburg, Germany) are used. A radiofrequency device (Ligasure; Covidien Italia, Segrate (Mi), Italy) is often used for dissection as well.
No specimen retrieval bag is necessary as the Unimax system is designed so that the wound is protected. According to lymph node location the technique can be standardized according to two situations: supramesocolic and submesocolic lymphadenopathy. In case of supramesocolic lymphadenopathy (lymph nodes of the celiac axis, hepatic pedicle, splenic hilum, or periaortic position) the patient is placed in reverse Trendelenburg position with the surgeon between the patient’s legs. To obtain a better exposition, one percutaneous thread can be passed under the round ligament and used for retraction of the liver. Alternatively, liver retraction can be achieved using the VERSA LIFTER™ Band (Surgical Perspective SAS, Strasbourg, France) disposable suspension system, hooked to the right diaphragmatic pillar and to the abdominal wall. If the splenic hilum has to be exposed or in case of difficult access to the celiac axis or to periaortic position, the lesser sac can be opened at the gastrocolic ligament and stomach retracted through sutures passed on its greater curvature (Figure 1), according to the “puppeteering technique”.8 In case of submesocolic lymphadenopathy (lymph nodes of the mesentery, periaortic, and periiliac areas) the surgeon and camera holder stand on the right side of the patient (Figure 2). A right tilt and mild Trendelenburg position of the table allow to obtain a correct exposure of the root of the mesentery; periaortic lymphadenopathy can be reached as well through an incision of the peritoneum laterally to the ligament of Treitz.
Figure 1.
Intra-operative view. Gastric suspension through trans abdominal sutures passed on the greater curvature, according to the “puppeteering technique”.
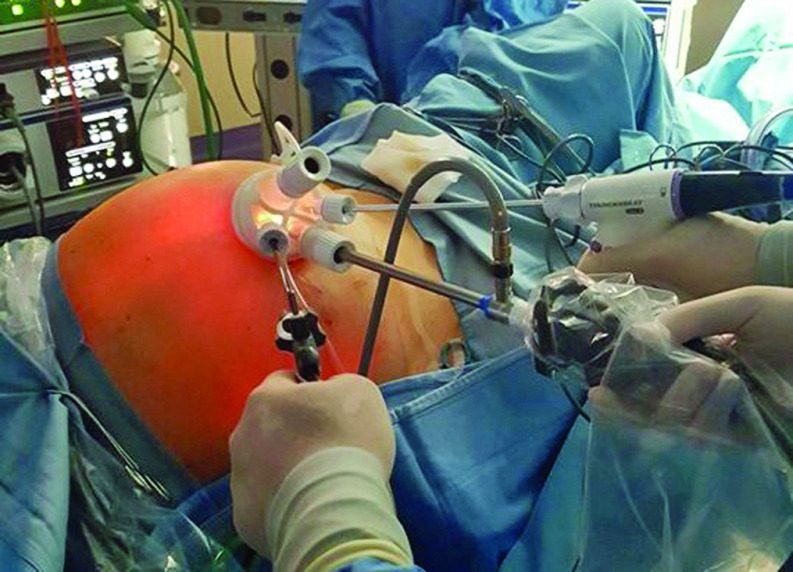
Figure 2.
The four-channel Unimax single-port device positioned at the umbilicus for a laparoscopic procedure in case of submesocolic lymphadenopathy.
Statistical Analysis
The nonparametric Mann Whitney U test for continuous variables and the χ2 test for binary variables were used to compare groups. A P value < 0.05 was considered statistically significant.
A logistic regression model was used to identify variables affecting the operative time and the hospital stay in univariate analysis. Statistical analysis was performed using the software package SPSS Version 13.0 (SPSS Inc, Chicago, IL, USA).
RESULTS
SPLB and MPLB groups were comparable with respect to age, gender, and associated comorbidities (Table 1). Previous abdominal surgery was not experienced in both groups. SPLB was completed laparoscopically in all cases. Two MPLB patients (5.7%) needed a surgical conversion to laparotomy due to intraoperative difficulties. In 1 patient the cause was an encapsulating peritonitis in a peritoneal dialysis patient, whereas in the second case it was due to incontrollable bleeding from a giant lymphatic mass at the aortic bifurcation. No conversions were reported in the SPLB group, the difference between the 2 groups was not statistically significant. (P = .284).
Table 1.
Characteristics of Patients and Postoperative Results Grouped for Laparoscopic Procedure
| Characteristic | SPLB (n = 20) | MPLB (n = 35) | P-Value |
|---|---|---|---|
| Sex, F/M | 8/12 | 12/23 | 0.678 |
| Age, years | 53.7 (13) | 51.5 (17) | 0.299 |
| Duration of surgery, min | 84 (31.7) | 81.1 (22.2) | 0.455 |
| Trocar addition, n (%) | 1 (5) | 0 | 0.188 |
| Surgery conversion, n (%) | 0 | 2 (5.7) | 0.284 |
| Abdominal drain positioning, n (%) | 0 | 1 (2.8) | 0.454 |
| Hospital stay | 1.7 (0.9) | 2.1 (1.2) | 0.455 |
| Morbidity, patients (%) | 1 (5) | 0 0 | 188 |
| Location of the disease (1/2/3/4)* | 8/3/7/5 | 12/8/11/10 | — |
| Diagnostic yield achievement, patients (%) | 19 (95) | 34 (97.1) | 0.689 |
Values are meant as median (SD) unless indicated otherwise.
SPLB, single-port laparoscopic lymph node biopsy; MPLB, multiport laparoscopic lymph node biopsy.
Location of the disease, 1 periaortic, 2 periiliac, 3 mesenteric, 4 gastrohepatic ligament.
One SPLB patient needed the addition of a trocar due to insufficient exposure of the gastrohepatic ligament despite lifting the liver by means of a transabdominal stay suture passed under the round ligament. An abdominal drain was positioned in the MPLB converted patient, none in the SPLB group, the difference between the 2 groups was not statistically significant (P = .454).
Estimated blood loss was 100 ml in 1 MPLB patient, it was < 50 ml in 5 SPLB and 2 MPLB patients, respectively, and it was absent in the remaining patients. Abdominal lymph node locations are listed in Table 2.f In both groups, the number of biopsies during the laparoscopic procedure were sometimes multiple (median: 2; range: 1–3). A liver biopsy was associated in 2 MPLB cases. Duration of surgery was similar in SPLB and MPLB groups respectively (84 ± 31.7 min vs. 81.1 ± 22.2 min; P = .455). Clinical parameters able to affect the operative time such as age, sex, associated comorbidities, and number of biopsies were tested in both groups without finding a significant correlation. A comparable length of hospitalization was observed in SPLB patients in comparison with the MPLB group (1.7 ± 0.9 days vs. 2.1 ± 1.2 days; P = .133), attaining an advantage of statistical significance of the former when a binary analysis was made ( = .004). Clinical parameters able to influence the hospital stay were analyzed in both groups and no significant correlations were found. On the postoperative course, 1 cutaneous infection managed conservatively was observed in the SPLB group vs. none in the MPLB group (P = .188).
In 95% of the SPLB and 97.1% of the MPLB cases, LLB achieved the correct diagnosis and subsequent therapeutic decisions. One case of false negative in the MPLB group was observed in a patient in which a specific inflammatory reaction was proven at histologic analysis. Due to a suspect past medical history, the laparoscopic biopsy was repeated and led to the diagnosis of large cell anaplastic lymphoma. Another case of false negative was seen in a 22-year-old SPLB patient despite an inadequate harvested tissue sample. Later, it required a CT-guided biopsy to establish the correct diagnosis of Hodgkin’s Lymphoma.
DISCUSSION
Surgical excision biopsies of lymph nodes for the diagnosis of lymphoma are recommended whenever possible.1 In fact, needle biopsies appear inferior to surgical biopsies at providing a correct diagnosis and at identifying lymphoma differentiations.14 That said, over the years the minimally invasive surgical approach to the diagnosis of abdominal lymphadenopathy has been imposed on traditional surgery due to the known advantages of laparoscopy such as pain reduction, hospitalization, an earlier resumption of work activity; and in the case of lymphoproliferative disorders, an earlier onset of chemotherapy.
Although in the gynecological field the use of single-port for pelvic lymphadenectomy for surgical staging of early uterine cancer is established,11–12 there are still no reports on the use of the laparoscopic single-port approach to make a diagnosis or to follow the progression of a lymphoproliferative disease. This is the reason why we wanted to investigate the feasibility and effectiveness of this approach in giving a valid diagnostic response when compared to traditional laparoscopy. Single-port laparoscopic approach has demonstrated its feasibility and efficacy in numerous procedures even if its diffusion has not been widespread due to the limited advantages for the patient in the face of greater technical difficulty.9,10,15
Wu et al.16 developed a training program to teach and validate the single-port procedure and technique for cholecystectomy. The authors concluded that although this approach has a “moderate learning curve” and it is easily learned and reproduced, it is certainly safer to perform a novel procedure in the laboratory first, before moving directly to patients.
In our report, no surgical conversions and 1 case (5%) of trocar addition were reported in the SPLB group. Moreover, a drain was left in only 1 case and blood loss was absent in 15 (75%) patients. These results testify to the possibility of managing the difficulties connected to the technique. The reason for the longer surgical times in single-port surgery are due to the use of instruments not appropriate to the technique and to the loss of ergonomics mainly due to the loss of triangulation of the instruments. Notwithstanding, in our study no significant differences were found in operative times between the SPLB and MPLB procedures, thus corroborating the validity of the single-port approach. Similarly, length of hospital stay was comparable for SPLB and MPLB patients. This represents a hopeful result aligned with the results of other studies where the single-port approach was used.17,18 Morbidity was practically absent in both groups.
The only complication that occurred in SPLB group was negligible and did not affect the length of stay. Our data on SPLB and MPLB surgical outcome are consistent with the experience reported by the literature. Most studies report a diagnostic accuracy in the 90.4%–95.5% range for LLB, a 5.94%–17.0% conversion rate, and a complication rate in the 1.0%–7.9% range, with no reported mortality.19,20 In our study, a high diagnostic yield was achieved with both procedures correlating with the best results of literature. In fact, in 95% of the SPLB and 97.1% of the MPLB patients, LLB achieved the correct information for diagnosis and classification.
Regarding the surgical technique, some positive considerations must be made on the SPLB approach. The "puppeteering technique" and the round ligament suspension are extremely useful in case of supramesocolic lymphadenopathy, as they allow excellent exposure of the operating field, avoid the use of other forceps, and consequently the clashing of instruments. Moreover, in case of difficulty, the conversion of a SPLB procedure requires only the addition of one or more trocars, thus avoiding a laparotomy and preserving the minimal invasiveness of the procedure itself. Finally, SPLB has the advantage of a single site for the positioning of the device, regardless of the location of the lymph node stations involved in the biopsy. This opportunity avoids the problem of finding the correct positioning of the trocars especially when multiple biopsies in different abdominal quadrants are planned for a MPLB procedure.
In regard to costs, economic benefits related to the use of the Unimax single-port device were assessed for single-port cholecystectomy technique when compared to the multiport approach; not only for the instrumentation, but also for the overall hospital costs.17
This advantage is also maintained in SPLB when compared to MPLB. In fact, the cost of the Unimax device is €122 compared to €201, that is the cost of 3 standard, disposable trocars.
There are several limitations to this case report. First, the small number of cases does not allow us to draw strong conclusions. Second, also because only 1 surgeon performed all the procedures, the outcomes reported may not necessarily be repeatable for all surgeons. Unfortunately, the lack of data in literature regarding the single port approach for LLB prevents us from expressing judgment on the potential advantages of this method. Further studies are necessary to support these results before its widespread adoption.
CONCLUSION
SPLB has shown good procedure and postoperative outcomes as well as a high diagnostic yield, comparable to traditional MPLB. Therefore, our results indicate that this approach is safe and effective in experienced hands and may represent a valid alternative to MPLB to diagnose or to restage a lymphoma.
Contributor Information
Marco Casaccia, Surgical Clinic Unit I, Department of Surgical Sciences and Integrated Diagnostics, Genoa University, Genoa, Italy..
Rosario Fornaro, Surgical Clinic Unit I, Department of Surgical Sciences and Integrated Diagnostics, Genoa University, Genoa, Italy..
Francesco Saverio Papadia, Surgical Clinic Unit I, Department of Surgical Sciences and Integrated Diagnostics, Genoa University, Genoa, Italy..
Tommaso Testa, Surgical Clinic Unit I, Department of Surgical Sciences and Integrated Diagnostics, Genoa University, Genoa, Italy..
Matteo Mascherini, Surgical Clinic Unit I, Department of Surgical Sciences and Integrated Diagnostics, Genoa University, Genoa, Italy..
Adalberto Ibatici, Hematology and Transplant Center Division, IRCCS Ospedale Policlinico San Martino, Genoa, Italy..
Chiara Ghiggi, Hematology and Transplant Center Division, IRCCS Ospedale Policlinico San Martino, Genoa, Italy..
Stefania Bregante, Hematology and Transplant Center Division, IRCCS Ospedale Policlinico San Martino, Genoa, Italy..
Franco De Cian, Surgical Clinic Unit I, Department of Surgical Sciences and Integrated Diagnostics, Genoa University, Genoa, Italy..
References:
- 1.Tilly H, Gomes da Silva M, Vitolo U, et al. Diffuse large B-cell lymphoma (dlbcl): esmo clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26(suppl 5):v116–25. [DOI] [PubMed] [Google Scholar]
- 2.Gilbert RWD, Bird BH, Murphy MG, O'Boyle CJ. Should laparoscopic lymph node biopsy be the preferred diagnostic modality for isolated abdominal lymphadenopathy?. Curr Oncol. 2019;26(3):e341–e345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daly SC, Klairmont M, Arslan B, et al. Laparoscopy has a superior diagnostic yield than percutaneous image-guided biopsy for suspected intra-abdominal lymphoma. Surg Endosc. 2015;29(9):2496–2499. [DOI] [PubMed] [Google Scholar]
- 4.Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. Short note: one wound laparoscopic cholecystectomy. Br J Surg. 1997;84(5):695–697. [PubMed] [Google Scholar]
- 5.Ponsky TA, Diluciano J, Chwals W, Parry R, Boulanger S. Early experience with single port laparoscopic surgery in children. J Laparoendosc Adv Surg Tech A. 2009;19(4):551–553. [DOI] [PubMed] [Google Scholar]
- 6.Saber AA, El-Ghazaly TH, Dewoolkar AV. Single-incision laparoscopic bariatric surgery: a comprehensive review. Surg Obes Relat Dis. 2010;6(5):575–582. [DOI] [PubMed] [Google Scholar]
- 7.Targarona EM, Balague C, Martinez C, Pallares L, Estalella L, Trias M. Single-port access: a feasible alternative to conventional laparoscopic splenectomy. Surg Innov. 2009;16(4):348–352. [DOI] [PubMed] [Google Scholar]
- 8.Chow AG, Purkayastha S, Zacharakis E, Paraskeva P. Single incision laparoscopic surgery for right hemicolectomy. Arch Surg. 2011;146(2):183–186. [DOI] [PubMed] [Google Scholar]
- 9.Arezzo A, Passera R, Bullano A, et al. Multi-port versus single-port cholecystectomy: results of a multi-centre, randomised controlled trial (MUSIC trial). Surg Endosc. 2017;31(7):2872–2880. [DOI] [PubMed] [Google Scholar]
- 10.Bucher P, Pugin F, Buchs NC, Ostermann S, Morel P. Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg. 2011;98(12):1695–1702. [DOI] [PubMed] [Google Scholar]
- 11.Barnes H, Harrison R, Huffman L, Medlin E, Spencer R, Al-Niaimi A. The adoption of single-port laparoscopy for full staging of endometrial cancer: surgical and oncology outcomes and evaluation of the learning curve. J Minim Invasive Gynecol. 2017;24(6):1029–1036. [DOI] [PubMed] [Google Scholar]
- 12.Kim SM, Park EK, Jeung IC, Kim CJ, Lee YS. Abdominal, multi-port and single-port total laparoscopic hysterectomy: eleven-year trends comparison of surgical outcomes complications of 936 cases. Arch Gynecol Obstet. 2015;291(6):1313–1319. [DOI] [PubMed] [Google Scholar]
- 13.Casaccia M, Torelli P, Cavaliere D, et al. Laparoscopic lymph node biopsy in intra-abdominal lymphoma: high diagnostic accuracy achieved with a minimally invasive procedure. Surg Laparosc Endosc Percutan Tech. 2007;17(3):175–178. [DOI] [PubMed] [Google Scholar]
- 14.Johl A, Lengfelder E, Hiddemann W, Klapper W, German Low-grade Lymphoma Study Group (GLSG). Core needle biopsies and surgical excision biopsies in the diagnosis of lymphoma-experience at the Lymph Node Registry Kiel. Ann Hematol. 2016;95(8):1281–1286. [DOI] [PubMed] [Google Scholar]
- 15.Marks JM, Phillips MS, Tacchino R, et al. Single-incision laparoscopic cholecystectomy is associated with improved cosmesis scoring at the cost of significantly higher hernia rates: 1-year results of a prospective randomized, multicenter, single blinded trial of traditional multiport laparoscopic cholecystectomy vs single-incision laparoscopic cholecystectomy. J Am Coll Surg. 2013;216(6):1037–1047. [DOI] [PubMed] [Google Scholar]
- 16.Wu AS, Podolsky ER, Huneke R, Curcillo PG. 2nd Initial surgeon training for single port access surgery: our first year experience. JSLS. 2010;14(2):200–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Casaccia M, Palombo D, Razzore A, Firpo E, Gallo F, Fornaro R. Laparoscopic single-port versus traditional multi-port laparoscopic cholecystectomy. JSLS. 2019;23(3):e2018.00102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahmed K, Wang T, Patel V, et al. The role of single-incision laparoscopic surgery in abdominal and pelvic surgery: a systematic review. Surg Endosc. 2011;25(2):378–396. [DOI] [PubMed] [Google Scholar]
- 19.Asoglu O, Porter L, Donohue JH, Cha SS. Laparoscopy for the definitive diagnosis of intra-abdominal lymphoma. Mayo Clin Proc. 2005;80(5):625–631. [DOI] [PubMed] [Google Scholar]
- 20.Mann GB, Conlon KC, LaQuaglia M, Dougherty E, Moskowitz CH, Zelenetz AD. Emerging role of laparoscopy in the diagnosis of lymphoma. J Clin Oncol. 1998;16(5):1909–1915. [DOI] [PubMed] [Google Scholar]