Brain metastasis (BM) of lung cancer is not rare in the course of tumor development. The overall survival (OS) of patients diagnosed with BM is only 3.6 months without radiotherapy. With rapid developments in treatment for BM, a median survival time (MST) of approximately 16 months could be achieved.[1] For patients with epidermal growth factor receptor mutations or anaplastic lymphoma kinase gene rearrangements, corresponding agents have been approved for treatment. In patients without driven genes mutation, radiation therapy remains the standard regimen for BM.
Whole-brain radiotherapy (WBRT) has been used to control BM for a few decades. However, the deterioration in neurological function caused by WBRT has attracted increasing attention. Studies have demonstrated that hippocampal-sparing WBRT (HS-WBRT) with simultaneous integrated boost (SIB) has the ability to avoid declines in neurocognitive function and increase the local control rate (LCR): with a 1-year intracranial LCR of 67%, only mild adverse effects are observed after radiation therapy.[2] Another phase II trial suggested that the local recurrence rate is 8.8% and intracranial recurrence rate is 21.3% at 1 year among patients who receive HS-WBRT with SIB, and this approach of radiotherapy decreases the probability of declines in delayed recall.[3] Stereotactic radiosurgery (SRS), which is characterized by fairly good efficacy and minimal influence on cognitive function, is recommended for limited BM (1–4 BM lesions).[4] A retrospective study indicated that among patients who receive SRS, the overall LCRs are 75% at 1 year and 66% at 2 years.[5] It is well known that the number of BM lesions affects the survival of patients significantly, whereas Nardone et al[6] elucidated that patients with a lower peritumor edema/gross tumor volume ratio may be more likely to receive additional WBRT, suggesting that tumor volume is the main factor affecting the choice of radiotherapy mode. To explore whether SRS can be performed in patients with more than four BM lesions, several clinical trials have been conducted. Rava et al[7] indicated that patients with more than ten brain lesions who are treated with SRS alone have a MST of 6.5 months. The median time to CNS failure is not statistically significant between patients who receive or do not receive initial WBRT. However, with an increase in the number of BM lesions, patients are more likely to receive salvage WBRT than undergo SRS.[8] Minniti et al[9] found that the addition of SRS to WBRT prolongs the MST and improves the LCR (MST of 10.3 vs. 7.3 months, P = 0.0005; median time to intracranial tumor progression of 10 vs. 7 months, P = 0.001). These findings are similar to those of Khan et al,[10] and there was no obvious difference in neurotoxicity between WBRT plus SRS and WBRT alone. Although the recurrence of brain tumors decreased significantly in patients who received WBRT plus SRS than in those who underwent SRS alone, no remarkable survival benefit was observed. The safety profile, including neurological function, was similar in the two groups.[11] This implies that upfront SRS with salvage WBRT or delayed WBRT may confer survival benefits.
Except for SRS and WBRT, other approaches of radiation therapy are emerging and developing for implementation. A retrospective study demonstrated that hypofractionated stereotactic radiotherapy (HSRT) is another suitable choice to control intracranial tumors and obtain survival benefits in patients with BM.[12] Furthermore, even though the long-term toxicity and survival associated with HSRT are the same as those associated with SRS, HSRT seems to be associated with a lower incidence of acute complications and better LCR according to previously reported results.[13] Volumetric-modulated arc therapy achieves considerable improvements in the LCR, especially for smaller BM lesions (diameter ≤2 cm).[14] Moreover, volumetric radiosurgery tends to be associated with a lower incidence of high-grade radionecrosis compared with that associated with SRS plus WBRT, which is observed in elderly patients, and the survival profile does not differ as the number of metastases increases.[15]
Chemotherapy is considered to have limited efficacy on BM because of the blood-brain barrier (BBB), but subsequent studies have demonstrated that a combination of radiation therapy and traditional chemotherapy can improve the survival of patients. Radiation may change the BBB and increase the permeability of drugs. Prior chemotherapy, on the other hand, increases the response rate of radiation therapy.[16] Li et al[17] reported that systemic therapy added to radiotherapy improved OS significantly. A greater number of cycles of pemetrexed combined with radiation therapy result in longer OS.[18] Another agent, temozolomide, has been shown to have good penetrating power across the BBB. The addition of temozolomide to WBRT can improve the objective response rate but fails to prolong OS.[19]
An increasing number of studies are investigating the availability of immunotherapy for BM. Kamath et al[20] published a case report describing a woman with a single BM lesion who had undergone prior SRS, chemotherapy, and maintenance treatment and was treated with pembrolizumab for 20 months. Surprisingly, the previous lesions were well controlled, and no new tumors appeared. Currently, the efficacy and safety of the combination of immunotherapy and radiotherapy has attracted our attention. The combination of programmed death-1 inhibitors and SRS prolongs the OS of patients with BM of NSCLC and achieves a higher LCR of brain lesions compared to that with sequential treatment or SRS alone.[21] More clinical trials are needed to explore the efficacy and safety of immunotherapy plus radiotherapy in patients with BM of NSCLC.
Aside from the aforementioned systematic treatment, surgery is usually recommended for symptomatic and limited BM, and radical resection of brain lesions confers a high LCR. Oertel et al[22] indicated that local radiotherapy after surgery is more favorable than WBRT or WBRT with SIB.
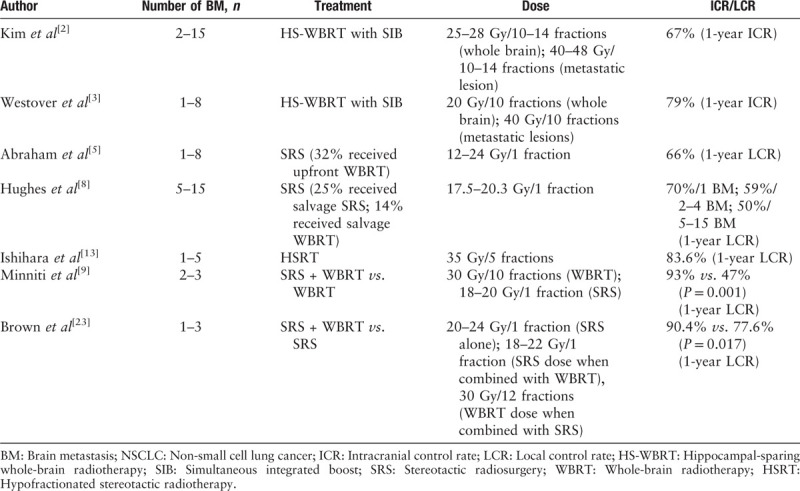
In conclusion, we summarized the main radiotherapy modes for BM from NSCLC in this article [Table 1]. Currently, the treatment of BM should not only pursue the LCR of lesions, but also patients’ quality of life. Radiation continues to play an indispensable role in the therapeutic strategy for BM, but SRS or WBRT alone is not the optimal strategy for patients with BM. Proper combination or sequential treatment may be more rational.
Table 1.
Several important studies on the radiotherapy modes of BM from NSCLC.
Funding
This work was supported by a grant from the Postgraduate Workstation of Oncology of Guizhou Province [Qian Jiao Ke He GZZ (2016) 06].
Conflicts of interest
None.
Footnotes
How to cite this article: Li PJ, Luo J, Liu GE, Liu DH, Shen SS, Li XJ, Ma H. Radiation therapy for patients with brain metastases from non-small cell lung cancer without driven gene mutation. Chin Med J 2020;133:2359–2361. doi: 10.1097/CM9.0000000000001044
References
- 1.Goncalves PH, Peterson SL, Vigneau FD, Shore RD, Quarshie WO, Islam K, et al. Risk of brain metastases in patients with nonmetastatic lung cancer: analysis of the Metropolitan Detroit Surveillance, Epidemiology, and End Results (SEER) data. Cancer 2016; 122:1921–1927. doi: 10.1002/cncr.30000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim KH, Cho BC, Lee CG, Kim HR, Suh YG, Kim JW, et al. Hippocampus-sparing whole-brain radiotherapy and simultaneous integrated boost for multiple brain metastases from lung adenocarcinoma: early response and dosimetric evaluation. Technol Cancer Res Treat 2016; 15:122–129. doi: 10.1177/1533034614566993. [DOI] [PubMed] [Google Scholar]
- 3.Westover KD, Mendel JT, Dan T, Kumar K, Gao A, Pulipparacharuv S, et al. Phase II trial of hippocampal-sparing whole brain irradiation with simultaneous integrated boost (HSIB-WBRT) for metastatic cancer. Neuro Oncol 2020; noaa092.doi: 10.1093/neuonc/noaa092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mazzola R, Corradini S, Gregucci F, Figlia V, Fiorentino A, Alongi F. Role of radiosurgery/stereotactic radiotherapy in oligometastatic disease: brain oligometastases. Front Oncol 2019; 9:206.doi: 10.3389/fonc.2019.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abraham C, Garsa A, Badiyan SN, Drzymala R, Yang D, DeWees T, et al. Internal dose escalation is associated with increased local control for non-small cell lung cancer (NSCLC) brain metastases treated with stereotactic radiosurgery (SRS). Adv Radiat Oncol 2018; 3:146–153. doi: 10.1016/j.adro.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nardone V, Nanni S, Pastina P, Vinciguerra C, Cerase A, Correale P, et al. Role of perilesional edema and tumor volume in the prognosis of non-small cell lung cancer (NSCLC) undergoing radiosurgery (SRS) for brain metastases. Strahlenther Onkol 2019; 195:734–744. doi: 10.1007/s00066-019-01475-0. [DOI] [PubMed] [Google Scholar]
- 7.Rava P, Leonard K, Sioshansi S, Curran B, Wazer DE, Cosgrove GR, et al. Survival among patients with 10 or more brain metastases treated with stereotactic radiosurgery. J Neurosurg 2013; 119:457–462. doi: 10.3171/2013.4.JNS121751. [DOI] [PubMed] [Google Scholar]
- 8.Hughes RT, Masters AH, McTyre ER, Farris MK, Chung C, Page BR, et al. Initial SRS for patients with 5 to 15 brain metastases: results of a multi-institutional experience. Int J Radiat Oncol Biol Phys 2019; 104:1091–1098. doi: 10.1016/j.ijrobp.2019.03.052. [DOI] [PubMed] [Google Scholar]
- 9.Minniti G, Salvati M, Muni R, Lanzetta G, Osti MF, Clarke E, et al. Stereotactic radiosurgery plus whole-brain radiotherapy for treatment of multiple metastases from non-small cell lung cancer. Anticancer Res 2010; 30:3055–3061. doi: 10.1002/maco.200403848. [PubMed] [Google Scholar]
- 10.Khan M, Lin J, Liao G, Tian Y, Liang Y, Li R, et al. Whole brain radiation therapy plus stereotactic radiosurgery in the treatment of brain metastases leading to improved survival in patients with favorable prognostic factors. Front Oncol 2019; 9:205.doi: 10.3389/fonc.2019.00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Qie S, Li Y, Shi HY, Yuan L, Su L, Zhang X. Stereotactic radiosurgery (SRS) alone versus whole brain radiotherapy plus SRS in patients with 1 to 4 brain metastases from non-small cell lung cancer stratified by the graded prognostic assessment: a meta-analysis (PRISMA) of randomized control trials. Medicine (Baltimore) 2018; 97:e11777.doi: 10.1097/MD.0000000000011777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kwon AK, Dibiase SJ, Wang B, Hughes SL, Milcarek B, Zhu Y. Hypofractionated stereotactic radiotherapy for the treatment of brain metastases. Cancer 2009; 115:890–898. doi: 10.1002/cncr.24082. [DOI] [PubMed] [Google Scholar]
- 13.Ishihara T, Yamada K, Harada A, Isogai K, Tonosaki Y, Demizu Y, et al. Hypofractionated stereotactic radiotherapy for brain metastases from lung cancer: evaluation of indications and predictors of local control. Strahlenther Onkol 2016; 192:386–393. doi: 10.1007/s00066-016-0963-2. [DOI] [PubMed] [Google Scholar]
- 14.Furutani S, Ikushima H, Sasaki M, Tonoiso C, Takahashi A, Kubo A, et al. Clinical outcomes of hypofractionated image-guided multifocal irradiation using volumetric-modulated arc therapy for brain metastases. J Radiat Res 2019; 60:134–141. doi: 10.1093/jrr/rry091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gregucci F, Fiorentino A, Corradini S, Figlia V, Mazzola R, Ricchetti F, et al. Linac-based radiosurgery or fractionated stereotactic radiotherapy with flattening filter-free volumetric modulated arc therapy in elderly patients: a mono-institutional experience on 110 brain metastases. Strahlenther Onkol 2019; 195:218–225. doi: 10.1007/s00066-018-1405-0. [DOI] [PubMed] [Google Scholar]
- 16.Peereboom DM. Chemotherapy in brain metastases. Neurosurgery 2005; 57:S54–S65. doi: 10.1227/01.neu.0000182740.39014.9a. [DOI] [PubMed] [Google Scholar]
- 17.Li B, Dai ZX, Chen YD, Liu YW, Liu S, Gu XN, et al. Systemic therapy after radiotherapy significantly reduces the risk of mortality of patients with 1-3 brain metastases: a retrospective study of 250 patients. Chin Med J 2017; 130:2916–2921. doi: 10.4103/0366-6999.220296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yu X, Fan Y. Effect of pemetrexed on brain metastases from nonsmall cell lung cancer with wild-type and unknown EGFR status. Medicine (Baltimore) 2019; 98:e14110.doi: 10.1097/MD.0000000000014110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu Y, Fu L, Jing W, Guo D, Kong L, Yu J. Effectiveness of temozolomide combined with whole brain radiotherapy for non-small cell lung cancer brain metastases. Thorac Cancer 2018; 9:1121–1128. doi: 10.1111/1759-7714.12795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kamath SD, Kumthekar PU, Kruser TJ, Mohindra NA. Intracranial response to anti-programmed death 1 therapy in a patient with metastatic non-small cell lung cancer with leptomeningeal carcinomatosis. Oncologist 2018; 23:e159–e161. doi: 10.1634/theoncologist.2018-0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schapira E, Hubbeling H, Yeap BY, Mehan WA, Jr, Shaw AT, Oh K, et al. Improved overall survival and locoregional disease control with concurrent PD-1 pathway inhibitors and stereotactic radiosurgery for lung cancer patients with brain metastases. Int J Radiat Oncol Biol Phys 2018; 101:624–629. doi: 10.1016/j.ijrobp.2018.02.175. [DOI] [PubMed] [Google Scholar]
- 22.Oertel M, Baehr A, Habibeh O, Haverkamp U, Stummer W, Eich HT, et al. Effect of postoperative radiotherapy for brain metastases: an analysis. Oncol Res Treat 2019; 42:256–262. doi: 10.1159/000499323. [DOI] [PubMed] [Google Scholar]
- 23.Brown PD, Jaeckle K, Ballman KV, Farace E, Cerhan JH, Anderson SK, et al. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 2016; 316:401–409. doi: 10.1001/jama.2016.9839. [DOI] [PMC free article] [PubMed] [Google Scholar]


