Significance
The elderly in the United States report less pain than those in midlife—suggesting, perhaps, that once people move into old age, their morbidity will fall. Unfortunately, assessing pain by age at one point in time masks the fact that each successive birth cohort reports more pain at any given age than the cohorts that came before it. We cannot use the experience of the elderly today to project pain prevalence of the elderly tomorrow. Today’s elderly have experienced less pain throughout their lives than those in midlife today, who will be tomorrow’s elderly. If these patterns continue, pain prevalence will continue to increase for all adults; tomorrow’s elderly will be sicker than today’s elderly, with serious implications for healthcare.
Keywords: pain prevalence, birth cohort analysis, educational divide, international comparison
Abstract
There is an expectation that, on average, pain will increase with age, through accumulated injury, physical wear and tear, and an increasing burden of disease. Consistent with that expectation, pain rises with age into old age in other wealthy countries. However, in America today, the elderly report less pain than those in midlife. This is the mystery of American pain. Using multiple datasets and definitions of pain, we show today’s midlife Americans have had more pain throughout adulthood than did today’s elderly. Disaggregating the cross-section of ages by year of birth and completion of a bachelor’s degree, we find, for those with less education, that each successive birth cohort has a higher prevalence of pain at each age—a result not found for those with a bachelor’s degree. Thus, the gap in pain between the more and less educated has widened in each successive birth cohort. The increase seen across birth cohorts cannot be explained by changes in occupation or levels of obesity for the less educated, but fits a more general pattern seen in the ongoing erosion of working-class life for those born after 1950. If these patterns continue, pain prevalence will continue to increase for all adults; importantly, tomorrow’s elderly will be sicker than today’s elderly, with potentially serious implications for healthcare.
Pain can be an important signal of damage, but it is rarely welcome; it directly undermines quality of life and, instrumentally, can harm the ability to lead a good life (1). The many manifestations of pain compromise both leisure and work for the ∼100 million Americans who experience it (2). It is a prominent factor in the opioid epidemic in the United States today, used to justify both the approval and prescription of opioids (3); it is implicated in suicide (4); and alcohol is often used to dull pain. There is a sharp difference in the pain experienced by the less and more educated (5), with those with less schooling reporting significantly higher levels of pain throughout adulthood (6, 7). Pain is a key player in the ongoing epidemic of rising “deaths of despair” from suicides, drugs, and alcoholic liver disease concentrated among Americans with less than a bachelor’s degree (8). Together with a stalling in previously falling mortality rates from heart disease, these deaths brought a 3-y decline in life expectancy at birth, from 2014 through 2017, for the first time in a century.
There is an expectation that, on average, pain will increase with age, through accumulated injury, physical wear and tear, and an increasing burden of disease. However, in America today, the elderly report less pain than those in middle age. Looking across different ages at a single point in time, a “snapshot,” pain increases through adulthood until late middle age, and declines thereafter. This pattern is found in multiple US datasets and for multiple definitions of pain, but is not present in other rich countries. To unravel this mystery, we show that today’s midlife Americans have had more pain throughout their adult lives than did today’s elderly. When we disaggregate the cross-section of ages by year of birth and by completion of a bachelor’s degree, we find that, for those with less education, each birth cohort has a higher level of pain throughout their adult life than the previous cohort. Within each birth cohort, pain does indeed rise with age, except for a postretirement pause for less-educated people, which is followed by a resumption of pain increases in older age. That pain is higher for later-born cohorts explains why cross-sectional data show the elderly in less pain than those in middle age, but does not explain the steadily worsening pain levels among less-educated Americans. Notably, this is exclusively an American phenomenon; there is no excess midlife pain among those who live in other rich countries, nor among those with a BA in the United States.
Measures of Pain
Pain is measured here through the reports of individuals who experience it, and its prevalence is measured by the fraction of the population reporting pain. As the Institute of Medicine reported in 2011, “[t]here is no standardization of methods, definitions, and survey questions regarding pain used in population-based studies across and within agencies” in the United States (2). To assess age−pain profiles in the United States and internationally, we use data from four nationally representative repeated cross-sectional surveys: the Gallup Health and Wellbeing Index (United States, n = 1,925,388), the Gallup World Poll (n = 234,785), the National Health Interview Survey (NHIS, n = 217,752), and the European Health Interview Survey (EHIS, n = 149,453). We restrict our sample to adults ages 25 y to 79 y and, in the US, to Black non-Hispanics and White non-Hispanics. We also draw on two US longitudinal surveys, the Medical Expenditure Panel Survey (MEPS, n = 118,305) and the Health and Retirement Study (HRS, n = 203,471). SI Appendix, Table S1 provides details on the surveys used and the pain questions asked. There is no reason to expect pain prevalence levels to be the same across surveys—the questions, time periods, and country composition are all different. Our interest here is in the shape of the age profile; the diversity of pain assessment adds to the generalizability of the results.
Results
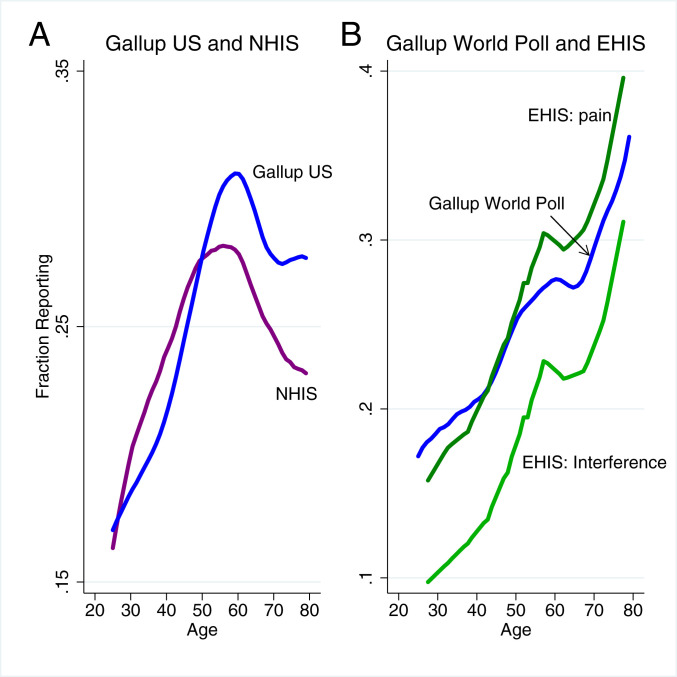
Fig. 1 plots the prevalence of self-reported pain against age in the United States (Fig. 1A), and other rich countries (Fig. 1B); here and in later figures, the raw data are smoothed using linear locally weighted polynomial regression (9, 10); the graphs are not otherwise adjusted, e.g., for the effects of covariates.* The figure plots the fraction reporting pain for men and women taken together; when separated by gender, more women report pain than men (11), but the age patterns shown in Fig. 1 appear for both. The pattern also holds for Black and White non-Hispanics analyzed separately (SI Appendix, Fig. S1).
Fig. 1.
Cross-sectional “snapshot” reports of pain with age in the United States and internationally. A plots, by age, the fraction of US Black and White non-Hispanic adults ages 25 y to 79 y who report pain in the Gallup Health and Wellbeing Index, pooled over years 2008–2017 (n = 1,925,388), and in the NHIS 1997–2018 (n = 217,752). B plots, by age, the fraction of adults ages 25 y to 79 y who report pain in other wealthy countries in the Gallup World Poll 2006–2018 (n = 234,785) and in the EHIS 2013–2015 (n = 149,453). B also plots, from the EHIS 2013–2015, the fraction of adults in other wealthy countries who report that pain interferes with daily life (n = 148,240).
In the United States, both the Gallup and NHIS data show pain prevalence rising with age until the late 50s and falling thereafter, with some leveling off after age 70 y. SI Appendix, Fig. S2 shows the same pattern, of rise and fall with age, in two other nationally representative US surveys, the MEPS and the HRS.† Four different surveys, each with its own pain questions, all yield the same unexpected age pattern. The decline in pain that begins in late middle age in these multiple cross-sectional snapshots is the primary object of our inquiry.
In contrast to the United States, Fig. 1B shows that, on average in 20 rich countries in the Gallup World Poll, as well as in 16 rich European countries in the EHIS, there is no decrease in the prevalence of pain after midlife, although the increase in pain prevalence pauses around age 60 y.‡ The concordance between the Gallup World Poll and EHIS in Fig. 1—that the two different surveys display similar age patterns of pain prevalence for other wealthy countries—together with the replicability of the American results over four surveys with different pain measures lays bare the mystery of US pain.
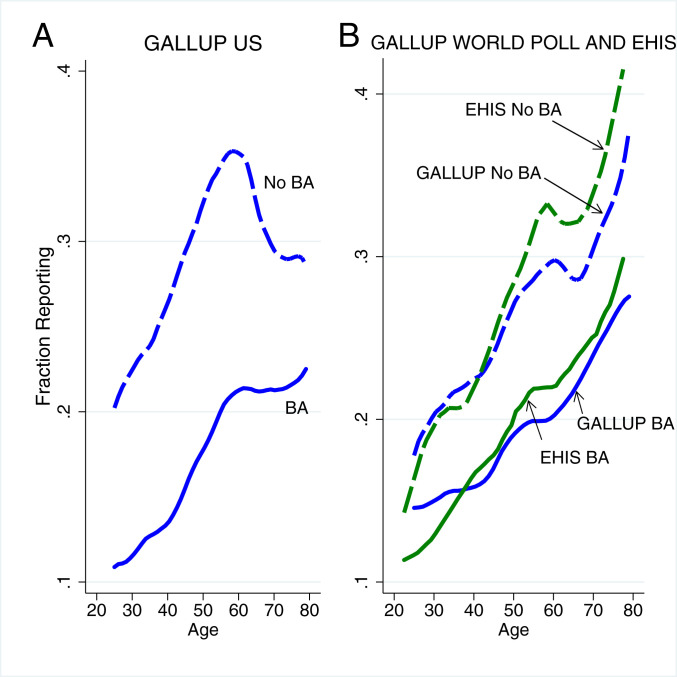
Fig. 2 shows that education is central to understanding this phenomenon. The age profiles in the (US) Gallup Health and Wellbeing Index (Fig. 2A) and international data (Fig. 2B) are shown separately for those with and without a bachelor’s degree in the United States or some tertiary education in other countries. Less-educated people report more pain in all settings.§ In Fig. 2A, for the United States, the midlife pain peak is confined to the less educated; for Americans with a bachelor’s degree, there is a slowdown in the rate of increase of pain with age after age 60 y. In the other wealthy countries, shown in Fig. 2B, less-educated people show a pause in the increase of pain around retirement age, but the increase resumes thereafter. For the more educated in other countries, the prevalence of pain rises smoothly with age. Once again, the Gallup World Poll and EHIS data yield similar pictures. Beyond retirement ages, pain prevalence among educated Americans changes little in either the Gallup data or the NHIS data (SI Appendix, Fig. S3), in contrast to a continuing rising prevalence in the other rich countries; the latter is more in line with the expectation that pain rises with age, so there is a secondary mystery among the oldest educated Americans which we investigate below.¶
Fig. 2.
Pain prevalence by educational attainment in the United States and internationally. A plots, by age, the fraction of Black and White non-Hispanic respondents ages 25 y to 79 y in the Gallup Health and Wellbeing Index data who report pain, separately for those with and without a bachelor’s degree (n = 1,038,550 with no BA, n = 879,761 with BA). B plots, by age, the fraction of respondents in the Gallup World Poll reporting pain, separately by attainment of some tertiary education (n = 141,726 without, and n = 70,891 with tertiary education). In addition, B plots, by age, the fraction of respondents in the EHIS reporting pain, by tertiary education (n = 99,493 without, n = 48,553 with tertiary education).
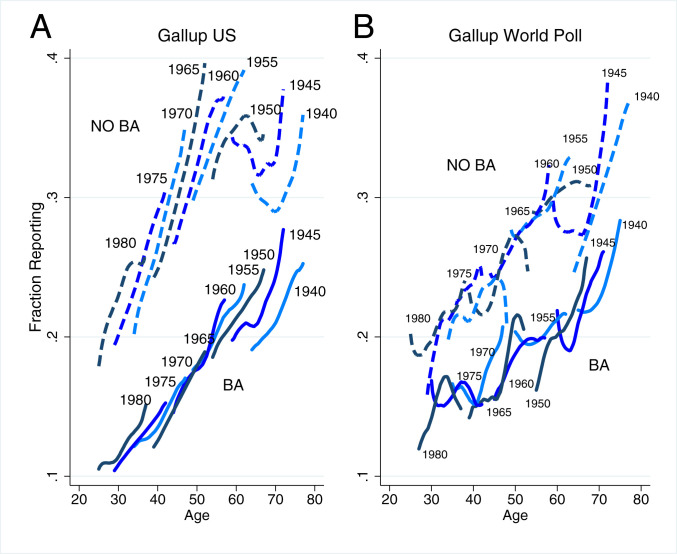
To better see why the elderly in the United States report less pain in a cross-sectional snapshot than do prime-aged adults, Fig. 3 retains the educational split but further disaggregates the Gallup data by birth cohort. Fig. 3A is again from the Gallup Health and Wellbeing Index (United States), and Fig. 3B is for the average of 20 wealthy countries the Gallup World Poll. The Gallup data follow birth cohorts for 13 y (2006−2018) in the World Poll, and for 10 y in the United States (2008–2017).
Fig. 3.
Pain by education and birth cohort in Gallup US and Gallup World Poll data. A plots reports of pain by age in the United States for every 5-y birth cohort from those born 1940–1944 through those born 1980–1984. Plots are drawn separately for those with and without a BA, using the Gallup Health and Wellbeing Index. B plots reports of pain in other wealthy countries analogously using the Gallup World Poll.
Fig. 3 A and B shows a series of birth cohorts as they age. In both panels, the age−pain profiles for birth years are presented for 5-y birth cohorts from 1940 to 1980; we aggregate to 5-y birth cohorts to reduce noise in the figure. Each is labeled by the first birth year in the cohort. For the United States, the youngest birth cohort (born in 1980−1984) is observed between the ages of 25 y and 37 y, and the oldest birth cohort (born in 1940−1944) between ages 64 y (in 2008) and 77 y (in 2017).
As in Fig. 2, at any given age, those with less education are more likely to report pain than those with more education. Fig. 3 demonstrates that, in addition, for those in the United States without a BA, at any given age, each cohort reports more pain than previous (earlier-born) cohorts. For example, for those who are age 52 y with less education, there are three cohorts with people at this age: the cohorts of 1955, 1960, and 1965. Forty percent of the 1965 cohort reported pain at age 52 y compared with 32% of the 1955 cohort. For these less-educated cohorts, each year of age is associated with an increase in pain prevalence of around one percentage point per year. Between ages 60 y and 70 y, this increase is put on pause, and rises thereafter. We discuss this pause below.
The main finding of Fig. 3A is the cohort by cohort upward shift of pain prevalence, from oldest to youngest cohort, for those without a BA. For Americans with a BA, only the cohorts born before 1950 show any such shift. For all more-educated cohorts, pain prevalence increases with age at around half a percentage point per year, about half the rate for those without a BA. Because they lack the cohort by cohort pain shift, the BA cohorts approximately coincide with the cross-sectional line from Fig. 2, again except for the two earliest-born cohorts. For these two cohorts, there are small intercohort increases in pain prevalence.#
Birth cohort pain profiles appear to lie along a single age trajectory in other wealthy countries, for both the more and less educated, although the samples are smaller than in the United States and the cohort profiles are noisier (Fig. 3B). The slopes of the two sets show pain prevalence increasing by about four percentage points for each decade of age.
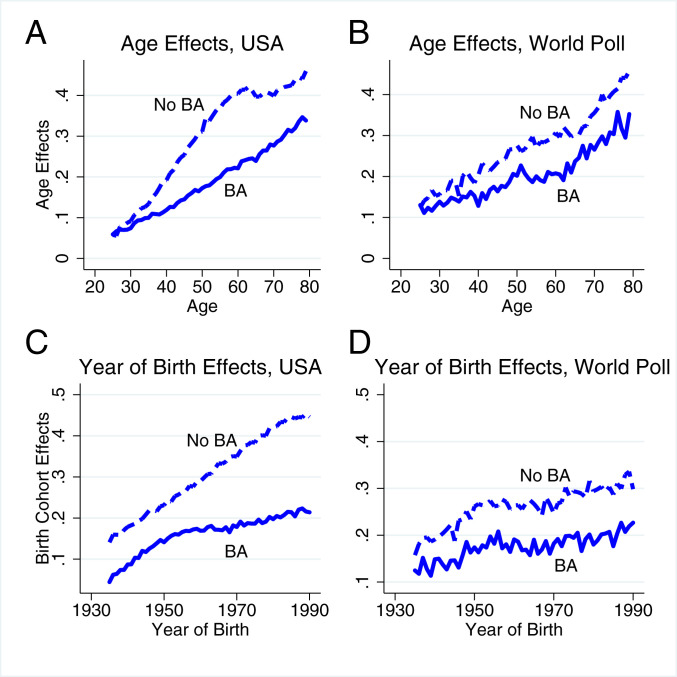
A compact and instructive way of examining the age−pain profiles and year of birth patterns in pain is possible by reverting to the full data, with single years of birth, and decomposing pain in both the Gallup United States and World Poll surveys into age effects and year of birth effects. We use linear regression to project expected pain at ages 25 y to 79 y and birth cohorts 1930–1990 onto a full set of single year of age and single year of birth cohort indicators.||
We estimate these age and birth cohort effects separately by level of education, for the United States and for the rest of the wealthy world, and present results in Fig. 4. Fig. 4 A and C use the Gallup US data. (Results for the United States using NHIS and HRS data are very similar; SI Appendix, Fig. S4.) For those without a BA, from ages 25 y to 63 y, pain prevalence rises by 1.1 percentage point with each year of age. From ages 64 y to 70 y, pain prevalence plateaus for this group, the “postretirement pause,” after which pain rises again. The rise of pain with age prior to retirement age, for those with less education, is twice the increase experienced for those with a BA (1.1 versus 0.5 percentage points). Beyond age 70 y, pain increases at approximately six-tenths of a percentage point with each year of age for both the less and more educated.
Fig. 4.
Pain prevalence age and year of birth effects in Gallup US and World Poll data. A and B present the estimated age effects from regressions of pain on a complete set of age indicators and year of birth indicators, for those aged 25 y to 79 y, born between 1935 and 1990, using data on Black and White non-Hispanics from (A) the Gallup Health and Wellbeing Index and (B) the Gallup World Poll. C and D present the estimated birth cohort effects from the same regressions. The regressions are run separately by level of education. (A and C: n = 984,800 with no BA; n = 853,132 with BA. B and D: n = 137,686 without tertiary education, n = 69,706 with tertiary.)
Pain prevalence rises more slowly with age in other wealthy countries (Fig. 4B). The increase averages 0.5 percentage points per year of age for those without, and 0.4 percentage points per year of age for those with, tertiary education. A postretirement pause in the rise of pain is also seen in this group of 20 countries, after which pain again begins to rise.**
Year of birth effects for the United States (Fig. 4C), show that each successive birth cohort reports more pain, with the trend markedly larger for those without a bachelor’s degree. For those with a BA, pain prevalence rises in parallel to that for those without a BA until the 1950 birth cohort, and rises more slowly thereafter; the steeper slope before the cohort of 1950 corresponds to the three rightmost cohorts in Fig. 2A. For cohorts born after 1950, pain prevalence rises at a rate of 0.6 percentage points per year of birth for those without a BA, and 0.2 percentage points for those with a BA. In all three US surveys—Gallup, NHIS, HRS—there has been a widening of the gap between birth cohort effects for the less and more educated, a widening that dates at least as far back as the mid-20th century.
Birth cohort effects in other wealthy countries (Fig. 4D) stand in sharp contrast to those found for the United States. There is a small increase in pain prevalence between the birth cohorts of 1935 and 1950, for both those with more and those with less education. Beyond the cohort of 1950, pain rises 0.15 percentage points per year of birth for those with less education (0.07 percentage points for those with tertiary education).
Discussion
The mystery of American pain can be resolved, not by looking at a snapshot (Fig. 1), but by tracking the average prevalence of pain by birth cohort over time (Figs. 3 and 4). For less-educated Americans, pain prevalence has been rising by cohort over time, so that later-born cohorts are in more pain at every age than are earlier-born cohorts.†† In other wealthy countries, those without tertiary education saw an increase in pain prevalence of four percentage points between the cohort born in 1950 and that born in 1990. Over that span of birth years, the fraction of Americans without a bachelor’s degree reporting pain increased by 21 percentage points. With a bachelor’s degree, the increase in the United States is more muted, with a rise of eight percentage points between the cohorts of 1950 and 1990.
An important implication of our analysis is that we cannot use the pain experience of the elderly today to project pain prevalence of the elderly tomorrow. Today’s elderly have experienced less pain throughout their lives than the middle-aged people today who will be tomorrow’s elderly. If these patterns continue, the average levels of morbidity among the elderly are set to increase, with potentially serious implications for health care.
Cohort by cohort increases in pain are only one of the many interrelated misfortunes that have befallen less-educated Americans; in addition to increases in pain, younger cohorts have seen more social isolation; more-fragile home lives, with less marriage, more divorce, and more out of wedlock childbearing; falling labor force participation, and falling wages. They have also seen rising deaths of despair, from suicide, drug overdose, and alcoholic liver disease (8). The epidemic of deaths of despair has barely touched more-educated Americans, and appears among the less educated only beginning around the cohort born in 1950—the point in Fig. 4 at which we begin to see a widening in the gap in pain between the less and more educated in any given birth cohort. The rising prevalence of pain is part of the deterioration of the social and economic conditions faced by less-educated Americans (15, 16).
This does not explain the rise in pain prevalence for those with a BA, in Figs. 3 and 4. The better educated have done well economically and have not suffered any such social dislocation. The increase in pain between the oldest cohorts, for both educational groups, calls for a different explanation, perhaps related to increasing educational levels, which we discuss below. The increase in pain among the elderly has been previously noted in the literature (17), and, while this earlier work rules out a number of explanations, such as changing demographic composition and mortality selection, it does not provide an explanation. In line with our account here, earlier work (5) shows that, among the earliest-born cohorts, the intercohort rise in pain generates an artifactual plateau of pain in a cross-sectional snapshot.
Rising pain in the population—here shown to be across cohorts—is implicated in the opioid epidemic, certainly as a cause of the increase in prescriptions. There are also indications that prolonged opioid use can worsen pain (18) even as it relieves it in the short run; some of the pain increase may be both a cause and a consequence of the opioid epidemic. There is evidence that pharma companies, particularly Purdue Pharmaceuticals, targeted areas of labor market disintegration (3, 19, 20), so that the social collapse and opioid explanations are not independent of one another. Opioids continue to be better controlled in Europe.
We end by noting alternative accounts and caveats. There are three immediate possible explanations for increasing pain prevalence among less-educated Americans. First, pain may not have changed in the United States, but Americans may be reporting more minor pain than in the past. Second, Americans have become heavier, which could lead to more pain. Third, they have moved out of good jobs into less good jobs, where less good jobs bring tasks that are more painful to perform or bring an increased risk of injury. The last explanation has been extensively investigated (21) and can be ruled out; the new jobs may indeed be worse in terms of satisfaction, promotion possibilities, or earnings—which might bring psychological pain, or even lower pain thresholds—but they do not involve more risk of physical pain. Assembly lines or coal mines are more dangerous than call centers, fast food restaurants, or Amazon warehouses.
We cannot rule out that pain reporting has changed in the United States, although it is not clear why this would occur only among those without a 4-y college degree. The issue of obesity must be taken seriously: Americans, like people in most other rich countries, are becoming heavier. Carrying additional weight brings additional musculoskeletal pain. However, SI Appendix, Fig. S5 shows that, even conditional on body mass index (BMI), the pain prevalence curve for lower back pain for those without a BA has moved upward significantly between 1997 and 2018, so that, even if no one had become heavier, pain would still have risen. For those with a BA, there was no statistically significant change in the relationship of lower back pain and BMI. The increase in BMI over this period can explain about a quarter of the increase in pain for those without a BA.
Two selection issues may also distort Figs. 3 and 4. First, the fraction of people who have a bachelor’s degree was higher among later-born cohorts, so that, when we look across cohorts, we are not comparing like with like. Second, when we follow any given cohort over time, some of its members may die, and deaths are likely to be higher among those who experience more pain, so that the prevalence of pain will rise less rapidly than would have been the case had there been no mortality.
Starting with mortality selection, the biggest effect of mortality selection would occur in the extreme case where all deaths are among those reporting pain. If cohort at age reports pain prevalence of , and if the mortality rate is , then the average pain prevalence among the survivors is . For the cohort born in 1940, and observed at age 77 y in 2017, the mortality rate was 3.5%, which would turn a pain prevalence of 25% at age 77 y into 22% at age 78 y. In reality, pain prevalence rises with age among the survivors, so pain-selective mortality makes the increase smaller than it would otherwise be. The downward pressure on reported pain would be smaller if (as is almost certainly true) there are deaths among those not in pain, and it is smaller at younger ages, where mortality rates are substantially lower.‡‡ The effect would be larger for higher mortality rates, for men rather than women, and for people without a BA.
The selection effect operates in the other countries as well as in the United States, so it can do nothing to explain the difference in patterns observed between the United States and other countries. In any case, given the size of the mortality selection effect, mortality selection has little effect on the general patterns in Figs. 3 and 4.
The second selection issue is that the rising fraction of Americans going to college affects the comparisons between cohorts. The standard argument here is that, over time, there is differential selection on some unmeasured characteristic, say, that is positively related to health, ability, or other factors that promote both health and education. For the earlier-born cohorts, where going to college was unusual, many high- people did not get a BA, and, as the BA became more common, the average declined, both among those without a BA, who are losing their highest- people, and among those with a BA, whose new recruits have lower than the previous average among those with a BA. As a result, for both BA and non-BA cohorts in Figs. 3 and 4, later-born cohorts are more adversely selected, potentially increasing pain. The increase in education across cohorts may explain some of the increase in pain between the earliest-born cohorts in Figs. 3 and 4, across whom educational attainment was rising most rapidly. Over men and women jointly, the fraction of the 5-y birth cohorts with a BA rose from 25% for the cohort of 1940 to 37% for the cohort of 1980. This, however, masks the fact that there was almost no change in college completion among men, but a doubling in completion among women. Yet, if we redraw the US panels of Figs. 3 and 4 for men and women separately, we get the same pattern for both, so the educational selection effect, if it exists, is not a good candidate to explain our findings.
Supplementary Material
Acknowledgments
We are grateful to Camilla Adams for expert research assistance and to Gallup, Inc. for granting us access to their data. A.C., A.D., and A.A.S. acknowledge funding from the National Institute on Aging: A.C. and A.D., Award 5R01AG060104-0; A.A.S., Award R37-AG057685.
Footnotes
Competing interest statement: A.D. and A.A.S. are Senior Scientists with Gallup, Inc. A.A.S. is a consultant with Adelphi Values, Inc.
*Locally kernel-weighted polynomial regressions are here superior to other commonly used smoothing techniques, such as LOWESS or kernel regression.
†The MEPS is a multiwave survey of households originally selected for the NHIS, and is thus not fully independent, but uses different pain questions than the NHIS.
‡Hadjiat et al. (12) analyzed a (0,1) question on whether respondents experienced pain in the last 12 mo, in the 2015 French internet-based National Health and Wellness Survey, finding that pain prevalence diminished at older ages. In contrast, in both the Gallup World Poll and the EHIS, we find that pain prevalence rises with age into old age in France.
§Statistical tests showing the significance of this difference are reported in SI Appendix. To keep Fig. 2 clear, an analogous figure, showing the education patterns for the NHIS, appears as SI Appendix, Fig. S2. Consistent with the findings from the Gallup US data, pain falls markedly with age after age 60 y for those with less than a BA, and pain prevalence flattens for those with a BA.
¶Consistent with work by Graham and Pinto (13), we find less-educated White non-Hispanics are significantly more likely to report having experienced pain “a lot of the day yesterday” than are less-educated Black non-Hispanics (SI Appendix, Fig. S3). However, the age patterns for Blacks and Whites analyzed separately mirror those presented in Fig. 2.
#We have investigated pain among these oldest cohorts using the HRS, which collects longitudinal data for older Americans. These data confirm the pain patterns in Fig. 3 for the oldest birth cohorts.
||Cohort and age effects are not unique in the presence of period effects. Fig. 4 can be reinterpreted by adding period effects; for example, for less-educated Americans in Fig. 4, the upward trend in the cohort effects can be eliminated and reinterpreted as age effects that grow more slowly and a time trend. Note that the cohort plot in Fig. 3 shows the raw data for 5-y birth cohorts and represents their experience independently of any interpretation, but the upward movement for each cohort could be reinterpreted as the effect of aging plus the effect of a general time trend that affects all ages. This reinterpretation does nothing to solve the original mystery, but relabels it as a time trend, a trend that is not present for better-educated Americans nor for those in other rich countries.
**In the Gallup World Poll countries taken together, the increase in pain with age steepens beyond age 65 y for those with and without tertiary education. Disaggregating the data by country, for those without tertiary education, we find a significant increase in the slope of age effects beyond age 65 y in 8 of the 20 countries, and in 7 countries for those with tertiary education. Additional analysis on this change in slope is warranted.
††The midlife dip in life satisfaction that has been found in many studies may be related to the midlife peak in pain in our cross-sectional analysis. Additional life satisfaction analysis by birth cohort may be illuminating (14).
‡‡For example, in the Gallup US data, at age 55 y, pain prevalence over the period 2008–2017 averaged 29.8%. The mortality rate at age 55 y was 0.6% over this period. If all those who died were in pain at age 55 y, pain prevalence would fall to 29.4% between ages 55 y and 56 y.
See online for related content such as Commentaries.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2012350117/-/DCSupplemental.
Data and Materials Availability.
The European and US official data are publicly available, although the European data require permission from Eurostat. The US data can be freely downloaded from the Web. We have prepared code that can be used to replicate our results. The underlying Gallup data are proprietary, and are not publicly available. We have prepared a replication dataset, containing all of the data that will allow replication of the results. Gallup will hold these data, but researchers can obtain permission from Gallup, and Gallup will give them access to the data for replication or further research. Please contact permissions@gallup.com for more information.
References
- 1.Benjamin D. J., Kimball M. S., Heffetz O., Szembrot N., Beyond happiness and satisfaction: Toward well-being indices based on stated preference. Am. Econ. Rev. 104, 2698–2735 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Institute of Medicine (US), Committee on Advancing Pain Research Care and Education , Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research, (National Academies Press, Washington, DC, 2011). [PubMed] [Google Scholar]
- 3.McGreal C., American Overdose: The Opioid Tragedy in Three Acts, (Public Affairs, New York, ed. 1, 2018). [Google Scholar]
- 4.Case A., Deaton A., “Suicide, age, and wellbeing: an empirical investigation” in Insights in the Economics of Aging, Wise D., Ed. (University of Chicago Press, Chicago, 2017), pp. 307–334. [Google Scholar]
- 5.Grol-Prokopczyk H., Sociodemographic disparities in chronic pain, based on 12-year longitudinal data. Pain 158, 313–322 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Case A., Deaton A., Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc. Natl. Acad. Sci. U.S.A. 112, 15078–15083 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Case A., Deaton A., Mortality and morbidity in the 21st century. Brookings Pap. Econ. Act. 2017, 397–476 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Case A., Deaton A., Deaths of Despair and the Future of Capitalism, (Princeton University Press, Princeton, NJ, 2020). [Google Scholar]
- 9.Fan J., Local linear regression smoothers and their minimax efficiencies. Ann. Stat. 21, 196–216 (1993). [Google Scholar]
- 10.Fan J., Gijbels I., Local Polynomial Modelling and Its Applications. Monographs on Statistics and Applied Probability, (Chapman & Hall, London, United Kingdom, ed. 1, 1996). [Google Scholar]
- 11.Case A., Paxson C., Sex differences in morbidity and mortality. Demography 42, 189–214 (2005). [DOI] [PubMed] [Google Scholar]
- 12.Hadjiat Y. et al., Pain associated with health and economic burden in France: Results from recent National Health and Wellness Survey data. Clinicoecon. Outcomes Res. 10, 53–65 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Graham C., Pinto S., Unequal hopes and lives in the USA: Optimism, race, place, and premature mortality. J. Popul. Econ. 32, 665–733 (2019). [Google Scholar]
- 14.Blanchflower D. G., Oswald A. J., Is well-being U-shaped over the life cycle? Soc. Sci. Med. 66, 1733–1749 (2008). [DOI] [PubMed] [Google Scholar]
- 15.Graham C., Happiness for All? Unequal Hopes and Lives in Pursuit of the American Dream, (Princeton University Press, Princeton, NJ, 2017). [Google Scholar]
- 16.Blanchflower D. G., Oswald A. J., Unhappiness and pain in modern America: A review essay, and further evidence, on Carol Graham’s Happiness for All? J. Econ. Lit. 57, 385–402 (2019). [Google Scholar]
- 17.Zimmer Z., Zajacova A., Persistent, consistent, and extensive: The trend of increasing pain prevalence in older Americans. J. Gerontol. B Psychol. Sci. Soc. Sci. 75, 436–447 (2020). [DOI] [PubMed] [Google Scholar]
- 18.Ballantyne J. C., Mao J., Opioid therapy for chronic pain. N. Engl. J. Med. 349, 1943–1953 (2003). [DOI] [PubMed] [Google Scholar]
- 19.Eyre E., Death in Mud Lick: A Coal Country Fight against the Drug Companies that Delivered the Opioid Epidemic, (Simon & Schuster, New York, NY, 2020). [Google Scholar]
- 20.Macy B., Dopesick: Dealers, Doctors, and the Drug Company that Addicted America, (Little, Brown, New York, NY, ed. 1, 2018). [Google Scholar]
- 21.Kaplan G., Schulhofer-Wohl S., The changing (Dis-)utility of work. J. Econ. Perspect. 32, 239–258 (2018). [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The European and US official data are publicly available, although the European data require permission from Eurostat. The US data can be freely downloaded from the Web. We have prepared code that can be used to replicate our results. The underlying Gallup data are proprietary, and are not publicly available. We have prepared a replication dataset, containing all of the data that will allow replication of the results. Gallup will hold these data, but researchers can obtain permission from Gallup, and Gallup will give them access to the data for replication or further research. Please contact permissions@gallup.com for more information.