Abstract
The reduced development of COVID-19 for children compared to adults provides some tantalizing clues on the pathogenesis and transmissibility of this pandemic virus. First, ACE2, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) receptor, is reduced in the respiratory tract in children. Second, coronavirus associated with common colds in children may offer some protection, due to cross-reactive humoral immunity and T cell immunity between common coronaviruses and SARS-CoV-2. Third, T helper 2 immune responses are protective in children. Fourth, surprisingly, eosinophilia, associated with T helper 2, may be protective. Fifth, children generally produce lower levels of inflammatory cytokines. Finally, the influence of the downturn in the global economy, the impact of living in quarters among families who are the most at risk, and factors including the openings of some schools, are considered. Those most disadvantaged socioeconomically may suffer disproportionately with COVID-19.
Keywords: COVID-19, children, SARS-CoV-2, ACE2
Our children, often a source of hope and optimism, have provided one of the few encouraging notes, a “silver lining” perhaps, in the dismal landscape of the current pandemic. Children have thus far been relatively protected from developing severe COVID-19 pneumonia. Understanding the basis for why children have generally done better than adults provides important insights into the pathogenesis of COVID-19, which may guide our understanding of susceptibility to infection and may provide further clues for therapeutics.
In the United States, through April 2, 2020, 2% of the reported COVID-19 cases were in children less than 18 y of age, according to the Centers for Disease Control and Prevention (CDC) (1). However, as of August 6, 2020, the American Academy of Pediatrics reported 9.1% of all cases of COVID-19 were children in states reporting cases by age. This figure represents 380,000 children in the United States, who have tested positive for COVID-19 since the onset of the pandemic (2). This increase over 4 mo is noteworthy. Whatever the underlying reasons for this increase may be, this trend serves to remind us that we are in an early phase of understanding the impact of this virus on children.
The CDC reported through the first week of August 2020 that, since March 1, 2020, there have been 576 pediatric COVID-19–associated hospitalizations, reported through the CDC’s COVID-NET (3). Studies from China, Italy, Spain, and North America all indicate that children are less frequently hospitalized with COVID-19 than adults (1–7). Evidence from the North American study (6) shows that many of the children who did require inpatient care due to acute COVID-19 had preexisting medical problems, including conditions that required long-term dependence on technologic support for their underlying diseases, as well as comorbidities that included obesity, immune suppression, and cancer (6). Hispanic or Latino (Hispanic) children and non-Hispanic Black children were hospitalized at rates approximately eightfold and fivefold higher than non-Hispanic White children (3).
Although relatively rare, a multisystem inflammatory syndrome in children (abbreviated MIS-C) has been reported from pediatric departments in hospitals. A large majority of children with MIS-C were positive, with PCR or with serologic testing, for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (7). It is unclear, at this point, whether the pathogenesis reflects active infection, given the variable presence of a positive PCR, but, more likely, the syndrome reflects predominately a postinfectious immune response. The percentage of Black and Hispanic children with MIS-C in the United States was higher than seen in the overall US population (8, 9). Thankfully, mortality related to this complication of SARS-CoV-2 has remained low (∼2%) (8).
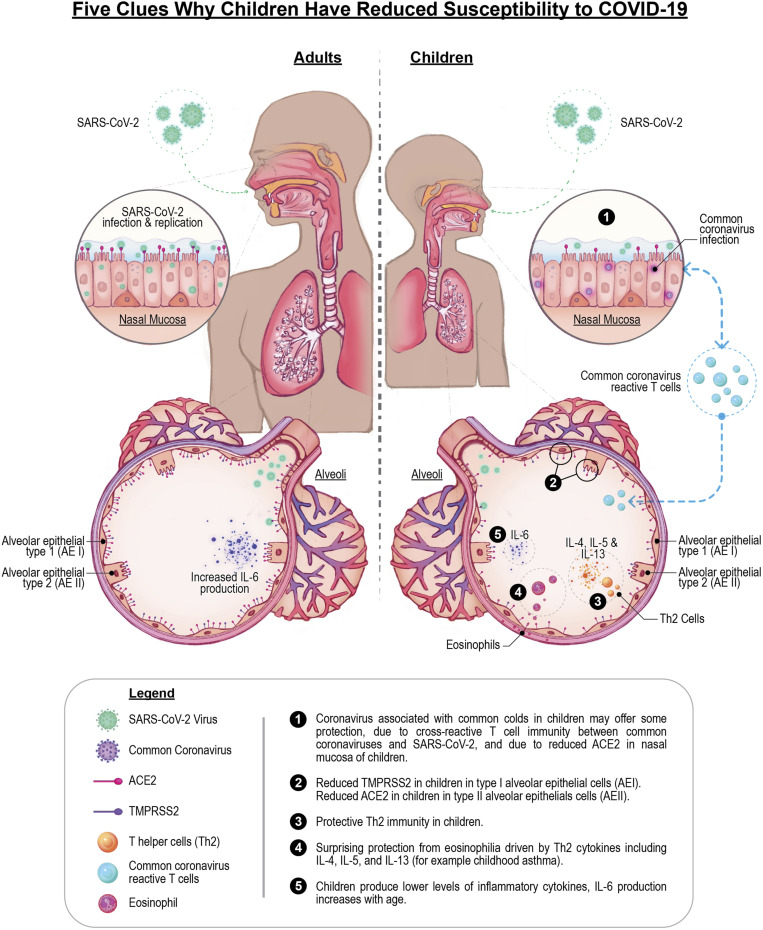
Exploring why the pediatric population is generally far less likely to develop COVID-19, even though their rate of infection is similar to adults (10), may offer productive clues, enabling strategies for targeting key pathogenic mechanisms in our efforts to contain and eradicate transmission of the virus. Here we review some of these intriguing areas that may help illuminate why children might be more resistant to serious outcomes following exposure to SARS-CoV-2 (Fig. 1).
Fig. 1.
(1) Coronavirus associated with common colds in children may offer some protection due to cross-reactive T cell immunity and cross-reactive antibody immunity between common coronaviruses and SARS-CoV-2, and due to reduced ACE2 in nasal mucosa of children. (2) Reduced TMPRSS2 in children in type I alveolar cells (AEI). Reduced ACE2 in children in type II alveolar cells (AEII). (3) Protective Th2 immunity in children. (4) Surprising protection from eosinophilia driven by Th2 cytokines including IL-4, IL-5 and IL-13 (for example childhood asthma). (5) Children produce lower levels of inflammatory cytokines, IL-6 production increases with age.
ACE2 Expression Is Lower in the Respiratory Tracts of Children
Both the first SARS virus, SARS-CoV-1 discovered in 2003, and the SARS-CoV-2 virus bind to angiotensin-converting enzyme 2 (ACE2) (11, 12). The renin angiotensin system, originally known for its critical role in blood pressure and hypertension, is also a critical trigger of inflammation in various organ systems. ACE converts the 10-amino acid angiotensin I peptide into the 8-amino acid peptide, known as angiotensin II. ACE2 then converts angiotensin II to the 7-amino acid peptide known as angiontensin1–7. Angiotensin-II, when binding to the angiotensin type (AT) 1 receptor, is proinflammatory in multiple organ systems including the lungs, the heart, the kidneys (13, 14), and the brain (15). In contrast, angiotensin1–7 is antiinflammatory when it binds to the Mas receptor (14).
Coronaviruses are enveloped single-stranded RNA viruses that cause enteric and respiratory tract infections in mammals and birds that can range from mild to severe (16). After the spike protein of SARS-CoV-2 binds to cells in the respiratory tract via ACE2 (11–13, 17, 18), the virus enters the cell via proteolytic cleavage involving two proteases, the transmembrane protease serine 2 (TMPRSS2) and cathepsin L (CTSL). In recent studies (17, 18) researchers analyzed the levels of RNA in cells of the respiratory tract, including nasal, airway, and lung parenchyma. Both of these studies showed that expression of ACE2 increases with age in the respiratory tract.
Wang et al. (17) analyzed gene expression in healthy lung tissue from three different age groups: approximately age 30 gestational weeks, approximately age 3 y, and approximately age 30 y. They analyzed gene expression with two platforms at single nuclear (sn) resolution, using snRNA sequencing (snRNA-seq) and sn assay for transposase−accessible chromatin (snATAC-seq), enabling the researchers to analyze specific genes and neighboring (cis-) regions that control cell-type expression of gene modules involved in processes like inflammation.
The respiratory tract has diverse cell types including alveolar epithelial type 1 (AEI) cells, that are responsible for the air−blood barrier in lung, and alveolar epithelial type 2 (AEII) cells that are critical for secreting pulmonary surfactant (17, 18). The cellular distribution of ACE2 and TMPRSS2 was distinct from CTSL. While ACE2 and TMPRSS2 were primarily in AEI, AEII, and airway cells such as club, ciliated, and basal cells, CTSL expression was found in epithelial cells, mesenchymal cells, endothelial cells, and macrophages. It is the alveolar cells that are the anatomic site of acute respiratory distress syndrome.
Wang et al. (17) noted “an increase in the proportion of alveolar epithelial cells expressing ACE2 and TMPRSS2 in adult compared to young lungs.” The investigators observed marked differences, particularly in AE cells (17), with the percentage of ACE2+ AEII cells increasing with age from the samples from those age 3 y upward to the samples from those age 30 y. Similar findings were seen for the TMPRSS2+ cells.
Analysis of the regulatory elements related to TMPRSS2+ cells revealed modules related to activation of an immune response in the lungs with a correlation related to increasing age. Noteworthy immune factors included interferon (IFN) regulatory molecules for both type 1 and type 2 IFNs, and signal transducer and activator of transcription molecules involved in activating inflammatory cytokine molecular pathways. Expression of TMPRSS2 was highest in ciliated cells and AEI. Expression of TMPRSS2 increased with age in mice and humans (19). For SARS-CoV-1, TMPRSS2 was shown to promote viral spread, with its protease activity serving to reduce viral recognition by neutralizing antibodies. Whether TMPRSS2 plays a similar role in the spread of SARS-CoV-2 is a subject of current investigation (19).
Muus et al. (18) analyzed gene expression in more than 4 million cells derived from 107 single-cell RNA expression studies, including 22 studies focusing on datasets from the lung and airways in both adults and children. In this large metaanalysis of multiple RNA expression studies, the researchers compiled data on cells from “nasal, airway, and lung parenchyma samples from 164 donors spanning fetal, childhood, adult, and elderly age groups.” They found ACE2, TMPRSS2, and CTSL coexpressed at low levels in alveolar cells of children compared to adults. The researchers were able to confirm these results directly with triple fluorescence in situ hybridization in specific cell types. They concluded that there was “particularly low” ACE2 in the pediatric samples (18).
Although the number of samples of young children was limited in this study (18), the researchers found that “strikingly, ACE2 expression is very low in normal lungs of newborns, the one ∼3 months’ lung sample, and the 3-year-old lungs.” These data were supported on a second platform known as scTHS-Seq, single-cell chromatin accessibility by transposome hypersensitive site sequencing, from human pediatric samples with no lung disease, collected at day 1 of life, at 14 mo, at 3 y, and at 9 y. They found “no signal was present at birth, it was low in the 9-year-old and 3-year-old sample, and higher in the 14 month-old.” The researchers concluded that “these patterns may be important in understanding why children are more resistant to COVID-19” (18).
There was an association of cells expressing both ACE2 and TMPRSS2 that were more frequent with increasing age (18). Cells expressing both TMPRSS2 and ACE2 in children are quite rare (18). These double-positive cells were particularly notable for expression of associated modules mediating viral and immune responses. These double-positive cells were the likely locus where an exuberant inflammatory response emerges. In these double-positive cells in lung epithelium, expression of interleukin 6 (IL-6) and IL-6R was increased. In so-called cytokine storms, where there is overactivation of the immune system in the alveoli, activation of these associated gene modules may underlie the pathophysiologic response (18). Monoclonal antibodies targeting inflammatory cytokines including IL-6 and its receptor, as well as tumor necrosis factor (TNF), are in therapeutic trials for cytokine storm in COVID-19.
A reasonable conjecture might be that, if ACE2 and/or TMPRSS2 expression is diminished in children, then viral infection of respiratory cells by SARS-CoV-2 might be less likely at any given viral load, and, additionally, there might be reduced expression of associated inflammatory modules. It is known that, in healthy children, there is an age-related increase in the production of IFN-γ and TNF-α. For IL-6, there was a trend for lower IL-6 concentrations in children below 2 y of age compared to older children (20). Thus, children have a lowered propensity to transcribe inflammatory cytokines in lung cells, and this may reduce the chance for an explosive immune reaction within the lungs resulting in the so-called “cytokine storm.”
Impact of Frequent Respiratory Infections in Childhood and Virologic and Immunologic Interference
Numerous studies (21–23) show that children younger than 2 y of age have five or more respiratory infections per year, and spend a median of 44 d with mild upper respiratory illnesses (21). The activation of adaptive immunity to common coronaviruses as well as the activation of the innate immune system in the respiratory tract may indeed provide some protection from microbial infection, including SARS-CoV-2. The frequent respiratory infections in children may provide further clues to why children are resistant. One line of reasoning is based on the phenomenon of viral interference. A second line of reasoning is based on the concept of immune interference.
Viral Interference.
Often, children are infected by more than one viral agent (21, 22). Viral interference is a well-known phenomenon where one virus interferes with the replication of a second virus (23). There is some evidence for coinfections in COVID-19 patients, including coinfection with other coronaviruses (24, 25). Kim et al. (24) reported on both hospitalized and nonhospitalized cases from Northern California, including children. They found more than 20% were positive for a second viral infection, including infection with other coronaviruses. In contrast, Nowak et al. (25) reported concurrent viral infection in only 3% of 1,204 SARS-CoV-2−positive patients from the New York metropolitan area who were also tested with a respiratory virus panel or a test for influenza and respiratory syncytial virus (RSV). In comparison, of 7,418 patients who tested negative for SARS- CoV-2, 845 were tested with the same multiplex panels, and 13% were positive for at least one non-SARS-CoV-2 respiratory viral pathogen (25). The increase in at least one non-SARS-CoV-2 viral pathogen in those who tested negative for SARS-CoV-2 may be due, in part, to viral interference.
An intriguing potential mechanism of resistance in children is that common coronaviruses associated with mild illnesses like colds and more severe illness like croup and bronchiolitis are associated with decreased expression of ACE2. For example, human coronavirus (HCoV) NL63, associated with common colds and croup, induces a down-regulation of ACE2 (26). A reduction in the viral receptor for SARS-CoV-2 therefore might help explain why children who carry such viruses in their nose and upper portions of their respiratory tracts are hospitalized less frequently than adults. The first site of encounter in the respiratory tract for the SARS-CoV-2 is in the nose. Investigators studying a cohort of 305 patients aged 4 y to 60 y found that “older children (10 y to 17 y old; n = 185), young adults (18 y to 24 y old; n = 46), and adults (≥25 y old; n = 29) all had higher expression of ACE2 in the nasal epithelium compared with younger children (4 y to 9 y old; n = 45)” (27).
Despite diminished expression of ACE2 and/or TMPRSS2 in children, “symptomatic infants have higher nasopharyngeal SARS-CoV-2 viral loads at presentation but develop less severe disease than older children and adolescents” (28). Moreover, children less than 5 y old “with mild to moderate COVID-19 have high amounts of SARS-CoV-2 viral RNA in their nasopharynx compared with older children and adults” (29).
Taken together, these data imply that, although the viral load in the nasopharynx may be higher in symptomatic children, overall, children remain markedly more resistant to viral infection of the lower respiratory tract leading to COVID-19. All this raises the likelihood that, although children are, fortunately, less susceptible to viral infection of the lungs, they can still serve as good disseminators of the SARS-CoV-2 virus that lurks in their nasal mucosa.
Detailed contact tracing from the Korean CDC revealed that household contacts of COVID-19−positive children ages 10 y to 19 y were the most likely to become infected with the SARS-CoV-2 virus compared to household contacts of people of all other ages. In contrast, household contacts of positive children aged 0 y to 9 y were the least likely to become infected. Taken together, these data need further substantiation, and might have implications for spread of infection at home, in daycare, and in schools (30). These data all emphasize that there is much to learn and to consider on the spread from children in various environments. It will also be important to stratify children by age, as infants, young children, and adolescents have different propensities for communicating viral infection.
Immunological Interference.
IFNs, first described in 1957 by Isaacs and Lindemann, bind to three distinct types of IFN receptors (31). Mapping of immune response modules in the respiratory tract shows that gene modules triggered by both type 1 and type 2 IFN responses are prominent (17, 18, 32, 33). The type 1 IFN response is vital for viral killing. Type 1 IFN, however, stimulates expression of the ACE2 receptor for the SARS-CoV-2 virus (33). Thus, the virus drives an increase in type 1 IFN expression, which then enhances expression of its receptor in the airway (33). In contrast, coronaviruses that frequently infect children with common colds down-regulate ACE2 as described above (26). Thus, children may benefit from a virtuous cycle with decreased ACE2 leading to less induction of the IFN response, which, in turn, further attenuates ACE2 expression. In contrast, adults suffer from a vicious cycle in which increased ACE2 expression drives a more robust IFN response.
The adaptive immune response to common coronavirus infection in children could provide some protection to COVID-19 since they share considerable degrees of homology with coronaviruses associated with the common cold. For example, spike proteins of the common HCoV share 30% amino acid identity with these viruses when one performs Basic Local Alignment Search Tool searches comparing these viruses. A detailed mapping of known T and B cell epitopes on SARS-CoV-2 indicates that adaptive immune reactivity at the T cell and antibody level targets not just the spike region but also other viral proteins (34).
A study in adult donors, age currently greater than 20 y, tested whether there was detectable immunity to SARS-CoV-2 and to common cold viruses attributed to coronavirus strains HCoV-OC43, HCoV-HKU1, HCoV-NL63, and HCoV-229E. Donors were recruited between 2015 and 2018, obviating exposure to SARS-CoV-2. Unexposed donors had T cell immunity to both spike and nonspike proteins in SARS-CoV-2 (34). The immunity may have emanated from shared regions on the common cold virus and SARS-CoV-2. Investigators tested immunity to one betacorononavirus HCoV-OC43 and to one alphacoronavirus NL63, and showed that these unexposed donors, n = 11, all had IgG to the receptor-binding domain of these common cold viruses. These nonexposed donors also had vigorous T cell responses to both spike and nonspike proteins in SARS-CoV-2 (35). Additional studies have been reported demonstrating widespread immunity in healthy individuals to cross-reactive regions of SARS-CoV-2 that share peptide sequence homology with endemic coronaviruses that cause common colds like HCoV-OC43, HCoV-229E, HCoV-NL63, and HCoV-HKU1 (36, 37). Humoral, antibody immunity to SARS-CoV-2 is widely detected in individuals, including children, who were not exposed to SARS-CoV-2 (38). Immunity to earlier exposures to both alpha and beta coronaviruses may thus engender protective humoral and cellular immunity for children who are heavily exposed to these common cold viruses.
A publication (39) from the Department of Defense examining the effect of the 2017–2018 seasonal influenza vaccine on respiratory infections produced some intriguing results. Investigators showed that the seasonal influenza immunization protected against influenza, as it was intended to do, and protected against some other respiratory viruses. However, they noted a small but statistically significant increase in individuals testing positive to metapneumovirus and coronaviruses. If future influenza vaccines, for example the 2020–2021 seasonal influenza vaccine, also provide increased occurrence of common coronaviruses, this phenomenon may actually afford some protection to SARS-CoV-2. Recent studies show that those with immunity to common coronaviruses do have adaptive immunity to SARS-CoV-2 via the mechanism of cross-reactive immunity (35–37).
There is some precedent for this phenomenon. Some immunizations induce protection against other infections outside of the intended target of the vaccine itself (40). A study from the Mayo Clinic indicated that “polio, Hemophilus influenzae type-B (HIB), measles-mumps-rubella (MMR), varicella, pneumococcal conjugate (PCV13), geriatric flu, and hepatitis A/hepatitis B (HepA-HepB) vaccines administered in the past 1, 2, and 5 y are associated with decreased SARS-CoV-2 infection rates” (41).
Some antiviral vaccines like the MMR vaccine contain components that have structural similarities with SARS-CoV-2 (42, 43). There is a 29% amino acid sequence homology between the ADP ribose-1-phosphatase domains of SARS-CoV-2 and rubella virus, including surface-exposed conserved residues shared between SARS-CoV-2 and the attenuated rubella virus in MMR (42). Patients with COVID-19 infection had raised levels of rubella IgG, but did not have increased rubella IgM, nor did they have increased levels of antibody to varicella zoster. The investigators interpret these results as indicative of a cross-reactive recall antibody response, common to regions shared between rubella and SARS-CoV-2, that may modulate the course of disease in COVID-19 (42). Whether or not such an immune response is protective or whether such an immune response might potentially enhance disease are outcomes under investigation (42).
A Surprising Potential Protective Benefit of Th2 Immunity in Children
There are three major arms of the immune response characteristics of human T helper cells, named Th1, Th2, and Th17 (33). The Th1 arm described above is mediated by gamma IFN. The Th2 arm is associated with allergic disease, and is mediated by IL-4, IL-5, and IL-13 (44). Sajuthi et al. (33) reported on gene expression studies on 695 children with asthma and healthy controls from the Genes-Environment & Admixture in Latino Americans study, an ongoing case-control study of asthma in Latino children and adolescents. They found that TMPRSS2 is part of a mucus secretory network, driven by Th2 inflammation via the actions of IL-13 (33). They found that Th2 responses driven by IL-4, IL-5, and IL-13 “dramatically” reduced ACE2 in the respiratory tract and are associated with better clinical outcomes with COVID-19, while the type 1 IFN response to respiratory viruses increased ACE2 expression (33).
Th2 cytokines drive an increase of a cell type called the eosinophil in the blood and tissues. Eosinophilia is a hallmark of Th2 inflammation in the airways, most notably in asthma (33, 45). Sajuthi et al. (33) concluded that, at least “provisionally… T[h]2 inflammation may predispose individuals to experience better COVID-19 outcomes through a decrease in airway levels of ACE2 that override any countervailing effect from increased expression of TMPRSS2.” It is indeed surprising that the Th2 immune type associated with allergic diseases including asthma, and with eosinophilia, provides some protection to COVID-19 in children. These findings from Sajuthi et al. (33) on 695 children and adolescents may help explain why low levels of eosinophilia were seen in fatalities in the elderly. Du et al. (45) reported that, in a study of 85 fatal COVID-19 adult subjects, 81.2% exhibited very low levels of blood eosinophils. A connection between knowledge gained in studying children (33) versus studying older adults, may help explain surprising outcomes in the elderly (45). This is one of the unexpected benefits of investigations on the “extremes of outcome” based on comparing children with the elderly populations at highest risk.
Another independent verification of the possible protective role of Th2 immunity was seen in a study on MIS-C. The very low IgE levels seen in individuals with MIS-C indicate that they may have lacked an adequate Th2 response to attenuate the increased inflammation associated with this hyperinflammatory complication in children (46).
One important caveat about the potential protective effect of eosinophilia comes from studies done 50 y ago in making a vaccine against RSV. “In 1967, infants and toddlers immunized with a formalin-inactivated vaccine against RSV experienced an enhanced form of RSV disease characterized by high fever, bronchopneumonia, and wheezing when they became infected with wild-type virus in the community. Hospitalizations were frequent, and two immunized toddlers died upon infection with wild-type RSV. The enhanced disease was initially characterized as a ‘peribronchiolar monocytic infiltration with some excess in eosinophils’” (47). As new SARS-CoV2 vaccines are tested, the potential appearance of Th2 immunity and eosinophilia must be scrutinized through a lens of caution. Although Th2 responses appear to be associated with some degree of protection to COVID-19, based on the experience with development of a novel vaccine to RSV 50 y ago, the dreaded development of immune enhancement, rather than immunization, must be assessed.
Unanswered Questions and Lessons to Learn
Although children have milder outcomes, thus far in the first few months of the COVID-19 pandemic, much remains unknown (1–10). The list of questions is considerable. We do not know, at this point, whether children who are asymptomatic and who are major carriers of virus can spread disease. When children leave a “shelter-in-place” environment and return to school, how will this impact more-vulnerable populations? Recent reports of outbreaks at summer camps and schools raise serious concerns (48).
The emergence of MIS-C is particularly worrisome, and it is unclear whether there will be long-term sequelae of SARS-CoV-2 infection in patients who were asymptomatic or mildly symptomatic, in those who developed severe COVID-19, or in those who subsequently developed MIS-C (5–9, 49). Other pandemics have been associated with postinfectious phenomena including postencephalitic Parkinson’s in the 1918 influenza pandemic (50). However, the simultaneous emergence of MIS-C in this current pandemic may allow elucidation of the pathophysiological underpinnings of this COVID-19 syndrome with systemic manifestations. Studies on MIS-C might provide insightful comparisons with the Kawasaki syndrome that has some clinical similarities. It is important to remember that intense inflammation activates the coagulation cascade, driving it in a procoagulant direction. Coagulation disorders and thrombosis are seen in MIS-C (51, 52). Autopsy studies on adults have revealed intense thrombotic microangiopathy with accompanying abnormalities in the coagulation cascade (52). The nexus between the coagulation cascade and the inflammatory response perhaps deserves increased attention for the possible therapeutic modalities that emerge from such a perspective (53, 54). Increased research emphasis on the connection between coagulation and inflammation is recommended.
The types of comorbidity underlying those at risk for COVID-19 accentuate some major differences between adults and children. Although children, like adults, with COVID-19 had a high incidence of comorbid conditions, there were significant differences in the types of comorbidity. The most common comorbidity in children, 40%, was those who were dependent on technological support. These children on technological support had congenital conditions, including developmental delay and genetic anomalies (4). In contrast, the comorbid conditions in adults are often considered acquired, including hypertension, pulmonary disease from smoking, and obesity. One comorbidity common to adults and children is obesity. Obesity was considered a risk factor in 48% of adults, while a lower percentage, 20.5%, of children with COVID-19 were obese (6, 55).
We should remember that, although there is widespread relief that children are hospitalized far less frequently than adults due to COVID-19 infection, we do not know how the carrier status of children affects their caregivers. We again have some relief that studies on pregnant women who test positive for the SARS-CoV-2 virus show that they and their offspring have, so far, done well. There appears to be negligible intrauterine transmission of disease, although larger studies are necessary to exclude this dreaded possibility (56).
While it seems that children are spared the most severe disease manifestations of COVID-19, they will undoubtedly be seriously impacted in many domains, beyond the direct effects of the pathogen. These potential negative impacts include how the pandemic and social distancing from other children affect psychological health, how it impacts education, and how it affects body weight and childhood obesity when getting sufficient exercise is more difficult during shelter-in-place and safe-distancing restrictions. One wonders how closure of playgrounds may further impact the obesity epidemic in children. Active programs to reduce childhood obesity have been designed so that this comorbidity does not further exacerbate the risk of COVID-19 in children (57). How the pandemic has changed routine medical and dental care, including immunizations to other preventable illnesses, needs to be examined.
The economic crisis associated with the pandemic has its own toll on children, as it is well known that deterioration in social determinants of health has significant adverse effects on children (https://www.cdc.gov/socialdeterminants/). Finally, sheltering in place and social distancing may even impact the frequency of infections typically seen in children (21–23). We shall learn, for example, whether these frequent respiratory infections had provided some benefit to children as they form their immune repertoires and gain immune memory.
Dedicating adequate resources to understand the molecular and immune underpinnings of COVID-19 in children may answer many of these questions and potentially allow development of novel therapeutic strategies for enhancement of host resistance to viral infections. We might consider that we may learn as much or more about this virus, from studying the relative resistance to COVID-19 in children, as we will learn from studying the vastly increased level of susceptibility in adults. There is still much to learn.
Acknowledgments
We were inspired by the efforts of those working in the front line and by the efforts of those behind the front lines, who are supporting one another during this pandemic. We thank Jason Ooi for his creativity, inspiration, and persistence in working with us on the figures. The work was funded by the NIH. L.S. is the Zimmermann Chair of Pediatrics and Neurological Sciences at Stanford. N.K. is the Boehringer Ingelheim Professor of Critical Care and Sleep Medicine at Yale.
Footnotes
Competing interest statement: N.K. has consulted with Biogen Idec, Boehringer Ingelheim, Third Rock, Pliant, Samumed, NuMedii, Indaloo, Theravance, LifeMax, Three Lake Partners, RohBar, and reports a grant from Veracyte. N.K. has patents on New Therapies in Pulmonary Fibrosis and Peripheral Blood Gene Expression Biomarkers. All these consultations are outside of this work. L.S. has consulted with Roche, Novartis, Tolerion, Atreca, TG Therapeutics, and Atara Biopharma. All these consultations are outside of the scope of this work.
This article is a PNAS Direct Submission.
Data Availability.
All study data are included in the article.
References
- 1.Centers for Disease Control and Prevention , Coronavirus disease 2019 in children—United States, February 12–April 2, 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm6914e4.htm. Accessed 26 August 2020.
- 2.American Academy of Pediatrics , Children and COVID-19: State-level data report. https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/. Accessed 11 August 2020.
- 3.Kim L., et al. , Hospitalization rates and characteristics of children aged <18 years hospitalized with laboratory-confirmed COVID-19 — COVID-NET, 14 states, March 1–July 25, 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm6932e3.htm. Accessed 26 August 2020.
- 4.Parri N., Lenge M., Buonsenso D.; Coronavirus Infection in Pediatric Emergency Departments (CONFIDENCE) Research Group , Children with covid-19 in pediatric emergency departments in Italy. N. Engl. J. Med. 383, 187–190 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richardson S. et al.; Northwell COVID-19 Research Consortium , Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA 323, 2052–2059 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shekerdemian L. S., et al. , Characteristics and outcomes of children with coronavirus disease 2019 (COVID-19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr., 10.1001/jamapediatrics.2020.1948 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheung E. W., et al. , Multisystem inflammatory syndrome related to COVID-19 in previously healthy children and adolescents in New York City. JAMA., 10.1001/jama.2020.10374 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dufort E. M. et al.; New York State and Centers for Disease Control and Prevention Multisystem Inflammatory Syndrome in Children Investigation Team , Multisystem inflammatory syndrome in children in New York state. N. Engl. J. Med. 383, 347–358 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feldstein L. R. et al.; Overcoming COVID-19 Investigators and the CDC COVID-19 Response Team , Multisystem inflammatory syndrome in U.S. children and adolescents. N. Engl. J. Med. 383, 334–346 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bi Q., et al. , Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: A retrospective cohort study. Lancet Infect. Dis. 20, 911–919 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li W., et al. , Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature 426, 450–454 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walls A. C., et al. , Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell 181, 281–292.e6 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Imai Y., Kuba K., Penninger J. M., The discovery of angiotensin-converting enzyme 2 and its role in acute lung injury in mice. Exp. Physiol. 93, 543–548 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verdecchia P., Cavallini C., Spanevello A., Angeli F., The pivotal link between ACE2 deficiency and SARS-CoV-2 infection. Eur. J. Intern. Med. 76, 14–20 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lanz T. V., et al. , Angiotensin II sustains brain inflammation in mice via TGF-beta. J. Clin. Invest. 120, 2782–2794 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fehr A. R., Perlman S., Coronaviruses: An overview of their replication and pathogenesis. Methods Mol. Biol. 1282, 1–23 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang A., et al. , Single nucleus multiomic profiling reveals age-dynamic regulation of host genes associated with SARS-CoV-2 infection. bioRxiv:10.1101/2020.04.12.037580 (14 April 2020).
- 18.Muus C., et al. , Integrated analyses of single-cell atlases reveal age, gender, and smoking status associations with cell type-specific expression of mediators of SARS-CoV-2 viral entry and highlights inflammatory programs in putative target cells. bioRxiv:10.1101/2020.04.19.049254 (20 April 2020).
- 19.Schuler B. A. et al.; Vanderbilt COVID-19 Consortium Cohort; HCA Lung Biological Network , Age-related expression of SARS-CoV-2 priming protease TMPRSS2 in the developing lung. bioRxiv:2020.05.22.111187 (23 May 2020).
- 20.Decker M. L., Grobusch M. P., Ritz N., Influence of age and other factors on cytokine expression profiles in healthy children—A systematic review. Front Pediatr. 5, 255 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Toivonen L., et al. , Burden of recurrent respiratory tract infections in children: A prospective cohort study. Pediatr. Infect. Dis. J. 35, e362–e369 (2016). [DOI] [PubMed] [Google Scholar]
- 22.Chonmaitree T., et al. , Viral upper respiratory tract infection and otitis media complication in young children. Clin. Infect. Dis. 46, 815–823 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kumar N., Sharma S., Barua S., Tripathi B. N., Rouse B. T., Virological and immunological outcomes of coinfections. Clin. Microbiol. Rev. 31, e00111-17 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim D., Quinn J., Pinsky B., Shah N. H., Brown I., Rates of co-infection between SARS-CoV-2 and other respiratory pathogens. JAMA 323, 2085–2086 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nowak M. D., Sordillo E. M., Gitman M. R., Paniz Mondolfi A. E., Co-infection in SARS-CoV-2 infected patients: Where are influenza virus and rhinovirus/enterovirus? J. Med. Virol., 10.1002/jmv.25953 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dijkman R., et al. , Replication-dependent downregulation of cellular angiotensin-converting enzyme 2 protein expression by human coronavirus NL63. J. Gen. Virol. 93, 1924–1929 (2012). [DOI] [PubMed] [Google Scholar]
- 27.Bunyavanich S., Do A., Vicencio A., Nasal gene expression of angiotensin-converting enzyme 2 in children and adults. JAMA 323, 2427–2429 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zachariah P., et al. , Symptomatic infants have higher nasopharyngeal SARS-CoV-2 viral loads but less severe disease than older children. Clin. Infect. Dis. ciaa608 (2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Heald-Sargent T., et al. , Age-related differences in nasopharyngeal severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) levels in patients with mild to moderate coronavirus disease 2019 (COVID-19). JAMA Pediatr., 10.1001/jamapediatrics.2020.3651 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park Y. J. et al.; COVID-19 National Emergency Response Center, Epidemiology and Case Management Team , Contact tracing during coronavirus disease outbreak, South Korea, 2020. Emerg. Infect. Dis., 10.3201/eid2610.201315 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gale M., Jr, Interference with virus infection. J. Immunol. 195, 1909–1910 (2015). [DOI] [PubMed] [Google Scholar]
- 32.Ziegler C. G. K. et al.; HCA Lung Biological Network. Electronic address: lung-network@humancellatlas.org; HCA Lung Biological Network , SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell 181, 1016–1035.e19 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sajuthi S. P., et al. , Type 2 and interferon inflammation strongly regulate SARS-CoV-2 related gene expression in the airway epithelium. bioRxiv:2020.04.09.034454 (10 April 2020). [DOI] [PMC free article] [PubMed]
- 34.Grifoni A., et al. , A sequence homology and bioinformatic approach can predict candidate targets for immune responses to SARS-CoV-2. Cell Host Microbe 27, 671–680.e2 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grifoni A., et al. , Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell 181, 1489–1501.e15 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mateus J., et al. , Selective and cross-reactive SARS-CoV-2 T cell epitopes in unexposed humans. Science 37, eabd3871 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Braun J., et al. , SARS-CoV-2-reactive T cells in healthy donors and patients with COVID-19. Nature, 10.1038/s41586-020-2598-9 (2020). [DOI] [PubMed] [Google Scholar]
- 38.Ng K. W., et al. , Pre-existing and de novo humoral immunity to SARS-CoV-2 in humans. bioRxiv:10.1101/2020.05.14.095414 (15 May 2020).
- 39.Wolff G. G., Influenza vaccination and respiratory virus interference among Department of Defense personnel during the 2017-2018 influenza season. Vaccine 38, 350–354 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Benn C. S., Netea M. G., Selin L. K., Aaby P., A small jab–a big effect: Nonspecific immunomodulation by vaccines. Trends Immunol. 34, 431–439 (2013). [DOI] [PubMed] [Google Scholar]
- 41.Pawlowski C., et al. , Exploratory analysis of immunization records highlights decreased SARS-CoV-2 rates in individuals with recent non-COVID-19 vaccinations. medRxiv:10.1101/2020.07.27.20161976 (29 July 2020). [DOI] [PMC free article] [PubMed]
- 42.Franklin R., et al. , Homologus protein domains in SARS-CoV-2 and measles, mumps and rubella viruses: Preliminary evidence that MMR vaccine might provide protection against COVID-19. medRxiv:10.1101/2020.04.10.20053207 (10 April 2020).
- 43.Gold J. E., Tilley L. P., Baumgartl W. H., MMR vaccine appears to confer strong protection from COVID-19: few deaths from SARS-CoV-2 in highly vaccinated populations. Researchgate:10.13140/RG.2.2.32128.25607 (10 May 2020).
- 44.Steinman L., A brief history of T(H)17, the first major revision in the T(H)1/T(H)2 hypothesis of T cell-mediated tissue damage. Nat. Med. 13, 139–145 (2007). [DOI] [PubMed] [Google Scholar]
- 45.Du Y., et al. , Clinical features of 85 fatal cases of COVID-19 from Wuhan. A retrospective observational study. Am. J. Respir. Crit. Care Med. 201, 1372–1379 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gruber C., et al. , Mapping systemic inflammation and antibody responses in multisystem inflammatory syndrome in children (MIS-C). medRxiv:10.1101/2020.07.04.20142752 (6 July 2020). [DOI] [PMC free article] [PubMed]
- 47.Acosta P. L., Caballero M. T., Polack F. P., Brief history and characterization of enhanced respiratory syncytial virus disease. Clin. Vaccine Immunol. 23, 189–195 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Szablewski C. M., et al. , SARS-CoV-2 transmission and infection among attendees of an overnight camp–Georgia, June 2020. MMWR Morb. Mortal. Wkly. Rep. 69, 1023–1025 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jones V. G., et al. , COVID-19 and Kawasaki disease: Novel virus and novel case. Hosp. Pediatr. 10, 537–540 (2020). [DOI] [PubMed] [Google Scholar]
- 50.Henry J., Smeyne R. J., Jang H., Miller B., Okun M. S., Parkinsonism and neurological manifestations of influenza throughout the 20th and 21st centuries. Parkinsonism Relat. Disord. 16, 566–571 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Son M. B., Friedman K., Coronavirus disease 2019 (COVID-19): Multisystem inflammatory syndrome in children. Up to Date (2020). https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19-multisystem-inflammatory-syndrome-in-children?topicRef=127488&source=see_link. Accessed 26 August 2020.
- 52.Bryce C., et al. , Pathophysiology of SARS-CoV-2: Targeting of endothelial cells renders a complex disease with thrombotic microangiopathy and aberrant immune response. The Mount Sinai COVID-19 autopsy experience. medRxiv:10.1101/2020.05.18.20099960 (22 May 2020).
- 53.Han M. H., et al. , Proteomic analysis of active multiple sclerosis lesions reveals therapeutic targets. Nature 451, 1076–1081 (2008). [DOI] [PubMed] [Google Scholar]
- 54.Steinman L., Platelets provide a bounty of potential targets for therapy in multiple sclerosis. Circ. Res. 110, 1157–1158 (2012). [DOI] [PubMed] [Google Scholar]
- 55.Garg S., et al. , Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019–COVID-NET, 14 states, March 1–30, 2020. MMWR Morb. Mortal. Wkly. Rep. 69, 458–464 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schwartz D. A., An analysis of 38 pregnant women with COVID-19, their newborn infants, and maternal-fetal transmission of SARS-CoV-2: Maternal coronavirus infections and pregnancy outcomes. Arch. Pathol. Lab Med. 144, 799–805 (2020). [DOI] [PubMed] [Google Scholar]
- 57.Baidal J. A. W., et al. , Zooming towards a telehealth solution for vulnerable children with obesity during coronavirus disease 2019. Obesity (Silver Spring) 33, 1184–1186 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All study data are included in the article.