Abstract
Aims
The influence of the COVID-19 pandemic on attendance to out-of-hospital cardiac arrest (OHCA) has only been described in city or regional settings. The impact of COVID-19 across an entire country with a high infection rate is yet to be explored.
Methods
The study uses data from 8629 cases recorded in two time-series (2017/2018 and 2020) of the Spanish national registry. Data from a non-COVID-19 period and the COVID-19 period (February 1st–April 30th 2020) were compared. During the COVID-19 period, data a further analysis comparing non-pandemic and pandemic weeks (defined according to the WHO declaration on March 11th, 2020) was conducted. The chi-squared analysis examined differences in OHCA attendance and other patient and resuscitation characteristics. Multivariate logistic regression examined survival likelihood to hospital admission and discharge. The multilevel analysis examined the differential effects of regional COVID-19 incidence on these same outcomes.
Results
During the COVID-19 period, the incidence of resuscitation attempts declined and survival to hospital admission (OR = 1.72; 95%CI = 1.46–2.04; p < 0.001) and discharge (OR = 1.38; 95%CI = 1.07–1.78; p = 0.013) fell compared to the non-COVID period. This pattern was also observed when comparing non-pandemic weeks and pandemic weeks. COVID-19 incidence impinged significantly upon outcomes regardless of regional variation, with low, medium, and high incidence regions equally affected.
Conclusions
The pandemic, irrespective of its incidence, seems to have particularly impeded the pre-hospital phase of OHCA care. Present findings call for the need to adapt out-of-hospital care for periods of serious infection risk.
Study registration number
ISRCTN10437835.
Keywords: Covid 19, Out-of hospital cardiac arrest, Emergency services, Survival
Introduction
Since its outbreak, the pandemic due to the Sars-CoV-2 virus has resulted in high morbidity and mortality all over the world. The effects of the pandemic, together with the containment measures adopted by the majority of countries, has led to modifications in how health services function and in the care provided to patients. Such modifications have affected health care and cardiovascular emergencies, amongst other aspects.1, 2, 3
Scientific evidence on the impact of COVID-19 on out-of-hospital cardiac arrest (OHCA) care is still limited. Some local level studies have been published on the incidence and outcomes of OHCA during the COVID-19 pandemic, specifically in New York, Paris, and the Italian region of Lombardy.4, 5, 6, 7 However, whilst existing studies focus on heavily hit settings they are limited to defined regions or cities and there are, therefore no national or global studies. This prevents the examination and comparison of areas with significant differences in the impact of the pandemic.
Spain is one of the countries with the highest COVID-19 incidence (455/100,000), mortality (52.5/100,000) and excess mortality (59%) rates worldwide.8, 9, 10, 11
On January the 31st 2020 the first positive COVID-19 case was reported in Spain.12 By March the 3rd there were a total of 150 cases, with the country reaching its daily peak on March the 20th, with 10,786 cases being diagnosed. In response, the government decreed a state of alarm on March the 14th, enforcing strict confinement and other social distancing measures throughout the country.
The objective of the present study is to analyze the influence of the COVID-19 pandemic on OHCA response and survival in Spain, whilst also comparing differences between regions based on their infection incidence.
Methods
The Spanish OHCA Registry (OSHCAR) is a prospective register of consecutive OHCA resuscitation attempts by public emergency medical services (EMS) in Spain. Data are collected periodically according to non-continuous time-series. There are 17 EMS, one in each region. All Spanish EMS are publicly funded and have a physician on board their ambulances and at their respective dispatch centres (http://www.epes.es/?publicacion=los-servicios-de-emergencias-y-urgencias-extrahospitalarias-en-espana). The methods used for the OHSCAR registry have been previously described.13
Inclusion criteria: all consecutive OHCA cases in which an emergency team performed resuscitation manoeuvres or post-resuscitation care following cardiopulmonary resuscitation (CPR) attempts by a first responder. Cases were excluded if the emergency team suspended resuscitation on-site due to confirmation of futility criteria during resuscitation. An attempt at CPR was considered futile when new data during resuscitation showed that it was not indicated (terminal disease, prolonged arrest time prior to EMS arrival, “do not resuscitate” orders).
OHSCAR records variables relating to the patient, event, care factors prior to emergency team arrival, treatment carried out by emergency team, final on-site state, hospital treatment and survival. All variables were recorded according to Utstein definitions.14
Study period and data sources
The analysis used data collected from two time periods. The COVID-19 period was defined as events between February 1st and April 30th 2020. This spanned the first documented infection in Spain, peak growth, and flattening and decline of the incidence curve. The OHSCAR does not collect data continuously. Therefore, the control period (non-COVID-19) was drawn from the last available data in the OHSCAR prior to the pandemic which covered April 1st 2017 and March 31st 2018. The control period comprised data from 1st February 2018 to 31st March 2018 and 1st April 2017 to 30th April 2017. Data from the entire 2017–2018 time-series is compared with COVID period data in Tables S2 and S3 in the Supplementary Appendix.
We defined a second period for analysis according to the WHO declaration of a pandemic on March the 11st. This allowed us to further differentiate into non-pandemic (NPW: data from 2018 and 2020 collected between February 1st and March 10th) and pandemic weeks (PW: data collected between March 11st and April 30th 2020).
Data on COVID-19 incidence during the study period were sourced from the Spanish Ministry of Health. Data are available at: https://cneCovid-19.isciii.es/Covid-1919/#documentaci%C3%B3n-y-datos.
Setting
EMS from 10 regions, with a total population of 30,298,000 inhabitants, participated in this study. (Table S1 in the Supplementary Appendix).
OHSCAR received approval from the Ethics Committee of Navarra and La Rioja. Informed consent was not required. OHSCAR uses STROBE guidelines for data reporting.15
Statistical analysis
The dependent variables used in analyses were response to OHCA (frequency or incidence where relevant), hospital admission with return of spontaneous circulation (ROSC) and survival to hospital discharge. The independent variable was COVID-19 which was examined according to the following two different comparisons. The first compared data collected during the non-COVID period with that from the COVID period.
In response to the second objective, we classified regions into low, medium and high incidence groups, according to cumulative COVID-19 incidence tertiles, up-to-date as of April 30th, 2020.
Descriptive statistics are reported as mean (standard deviation), median (interquartile range) or frequency (percent), where relevant. Between-group comparisons were made for general patient characteristics, events, and pre- and in-hospital care. The Kruskal–Wallis test or ANOVA was used to make comparisons between continuous variables depending on the distribution of the variable under analysis. χ2 analyses were used for categorical comparisons. All statistical tests were two-tailed with significance set at p < 0.05. The statistical software SPSS version 26.0 was used for all analyses.
In order to analyze whether a change existed in the profile of cases attended to during the study period, the 4 sub-groups recommended by Utstein14 were compared.
Official population census data for 2018 and 202016 were used to calculate resuscitation attempts per 105 inhabitants for the non-COVID period and COVID period, respectively.
Given the assumption that accumulated COVID-19 incidence could impact OHCA response over time, changing trends in resuscitation attempts and survival over the 13 weeks between February the 1st and April the 30th 2020 (COVID period) were examined using join point regression. The 13 weeks of the non-COVID period were also examined as a form of control.
Overall survival from OHCA to hospital admission and discharge was examined using logistic regression. Odds ratios for survival per treatment group were adjusted for age and gender. The influence of resuscitation characteristics on survival rates before and during the COVID-19 pandemic, and during NPW and PW, was examined via stratification.
Finally, given the implications of the current COVID-19 pandemic on health resources, a multilevel logistic regression model adjusted for age and gender was developed to examine the influence of COVID-19 incidence on resuscitation attempts and survival, clustered according to regions. Regional analysis was carried out in two ways. In an initial multilevel analysis, the cumulative incidence of each region was used. Subsequently, regions were categorically analyzed according to their aforementioned incidence classification (Table S1 in the Supplementary Appendix).
Results
OHCA resuscitation attempts
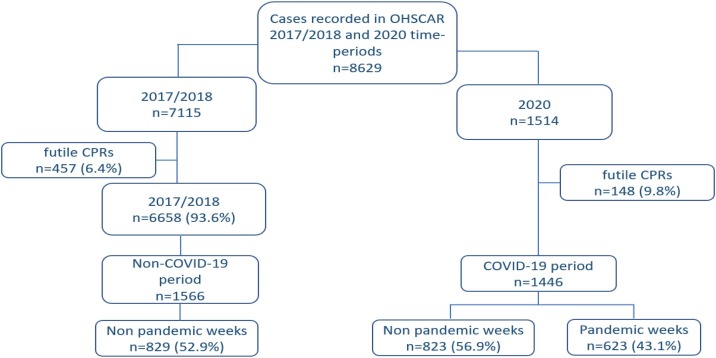
A flowchart of included cases is shown in Fig. 1 . There were more futile resuscitations in the COVID period in comparison with the non-COVID period (9.8% vs 6.4%; p < 0.001).
Fig. 1.
Participant flow diagram. All cases included in the study were registered in the OHSCAR database in one of two time-series (April 1st 2017 to March 31st 2020 or February 1st 2020 to April 31st 2020). Non-COVID-19 period data includes cases collected between February 1st and April 31st from the 2017/2018 time-series. COVID-19 period data includes all data collected from the 2020 time-series.
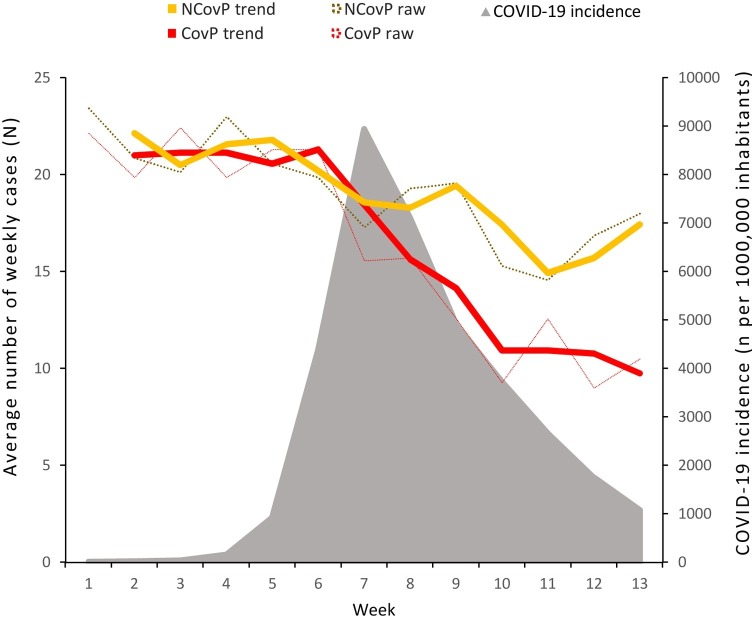
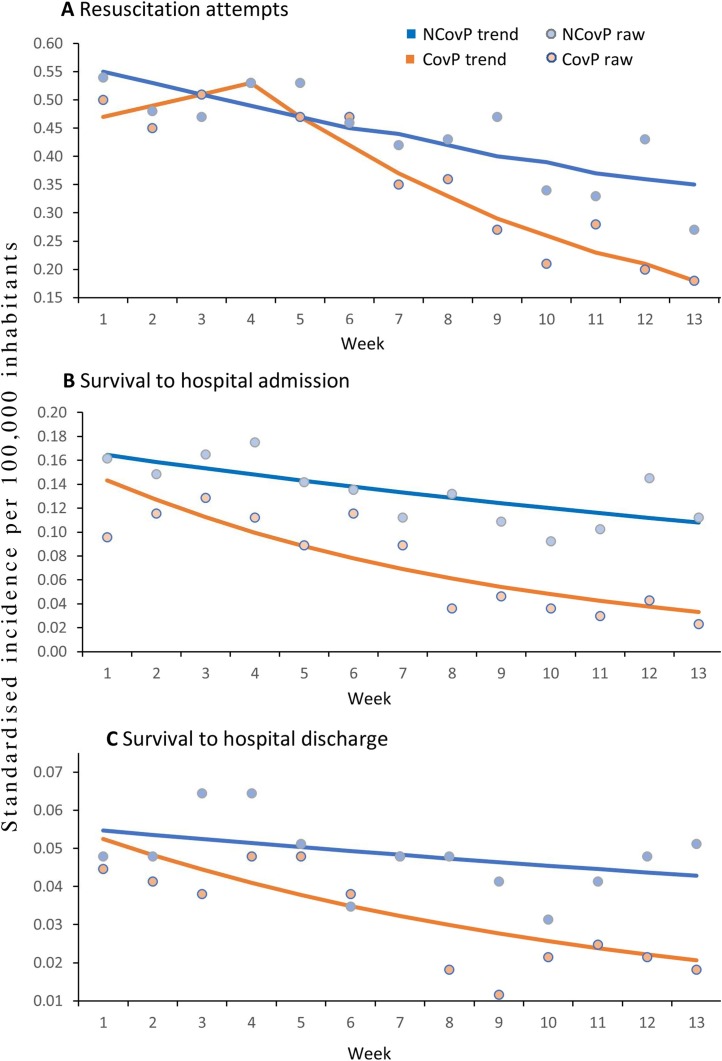
A total of 3169 resuscitation attempts were made between February 1st and April 30th in the two periods studied. More cases were attended to during the non-COVID period (n = 1723) than the COVID period (n = 1446; p < 0.001). The number of OHCAs resuscitation attempts performed during the non-COVID period and COVID period are shown in Fig. 2 , together with the evolution of the incidence of the COVID-19 pandemic. Further, no significant change in resuscitation trends occurred over time during the non-COVID period but a significant drop in resuscitation attempts was seen from week 4 onwards during the COVID period (t = −2.52; SE = 0.06; p < 0.05) (Fig. 3 , 3A).
Fig. 2.
Average number of weekly resuscitation attempts in a non-COVID-19 period (NCovP) and the COVID-19 period (CovP), and daily COVID-19 incidence. Data collected between February the 1st and April the 30th. Solid lines and area (COVID-19 incidence) present 2 week moving average. Dashed lines present raw data.
Fig. 3.
Weekly trends in resuscitation attempts (A), survival to hospital admission (B) and hospital discharge (C) in a non-COVID-19 period (NCovP) and the COVID-19 period (CovP) between February the 1st and April the 30th. In A there is a significant (p = 0.036) change in trend for the CovP at week 4. Solid lines represent trends. Dots represent raw data.
For the comparison of non-pandemic weeks and pandemic weeks, a sample of 2275 resuscitation attempts was used. More resuscitation attempts were made during non-pandemic weeks (n = 1652; standardized incidence = 0.50) than pandemic weeks (n = 623; standardized incidence = 0.30; p < 0.001) (Table 1 ).
Table 1.
Resuscitation characteristics compared between a non-COVID-19 period (2017/2018) and the COVID-19 period (2020), and non-pandemic weeks (pre-COVID-19 period/COVID-19 period February the 1st to March the 10th) and pandemic weeks (COVID-19 period March 11th to April 30th). Data collected between February the 1st and April the 30th.
| Time period |
Type of weeks (data collected between February 1st and April 30th) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | non-COVID-19 (2017/2018) | Missing | COVID-19 (2020) | Missing | p-value | Non-pandemic weeks (NPW) | Missing | Pandemic weeks (PW) | Missing | p-value | |
| All resuscitations, N (%) | 3169 (100.0) | 1723 (54.4) | 1446 (45.6) | 0.000 | 1652 (0.50a) | 623 (0.30a) | 0.000 | ||||
| Female, N (%) | 931 (29.4) | 513 (29.8) | 2 (0.1) | 418 (28.9) | 1 (0.1) | 0.588 | 479 (29.0) | 0 (0.0) | 190 (30.5) | 1 (0.2) | 0.469 |
| Age (years), mean (SD) | 65.04 (16.7) | 65.61 (16.9) | 5 (0.3) | 64.36 (16.5) | 4 (0.3) | 0.036 | 65.40 (17.3) | 4 (0.2) | 63.73 (15.5) | 2 (0.4) | 0.027 |
| Aged 14 and under | 43 (1.4) | 22 (1.3) | 5 (0.3) | 21 (1.5) | 4 (0.3) | 0.671 | 26 (1.6) | 4 (0.2) | 8 (1.3) | 2 (0.4) | 0.613 |
| Aged 75 and over | 1023 (32.4) | 588 (34.2) | 5 (0.3) | 435 (30.32) | 4 (0.3) | 0.015 | 569 (34.5) | 4 (0.2) | 156 (25.1) | 2 (0.4) | 0.000 |
| OHCA at home, N (%) | 2030 (64.2) | 1042 (60.8) | 9 (0.5) | 988 (68.3) | 0 (0.0) | 0.000 | 1003 (60.9) | 6 (0.4) | 478 (76.7) | 0 (0.0) | 0.000 |
| Witnessed OHCA, N (%) | 2468 (77.9) | 1331 (77.2) | 0 (0.0) | 1137 (78.6) | 0 (0.0) | 0.351 | 1291 (78.1) | 0 (0.0) | 493 (79.1) | 0 (0.0) | 0.610 |
| Bystander CPR performed, N (%)b | 1326 (47.3) | 788 (51.1) | 0 (0.0) | 538 (42.6) | 0 (0.0) | 0.000 | 694 (46.9) | 0 (0.0) | 230 (42.8) | 0 (0.0) | 0.103 |
| AED used, N (%)b | 286 (10.2) | 173 (11.2) | 0 (0.0) | 113 (9.0) | 5 (0.4) | 0.051 | 150 (10.2) | 3 (0.2) | 43 (8.0) | 2 (0.4) | 0.153 |
| Shockable initial rhythm, N (%) | 668 (21.9) | 386 (23.1) | 48 (3.1) | 282 (20.5) | 54 (4.3) | 0.083 | 347 (21.8) | 56 (3.8) | 118 (19.9) | 23 (4.3) | 0.334 |
| Airway isolation | 2638 (88.4) | 1441 (92.4) | 163 (9.5) | 1197 (84.1) | 23 (1.6) | 0.000 | 1392 (89.4) | 95 (5.8) | 500 (81.7) | 11 (2.0) | 0.000 |
| Orotracheal intubation | 2082 (78.9) | 1224 (84.9) | 163 (9.5) | 858 (71.7) | 23 (1.6) | 0.000 | 1139 (81.8) | 95 (5.8) | 320 (64.0) | 11 (2.0) | 0.000 |
| Supraglottic device | 271 (10.3) | 103 (7.1) | 163 (9.5) | 168 (14.0) | 23 (1.6) | 0.000 | 105 (7.5) | 95 (5.8) | 110 (22.0) | 11 (2.0) | 0.000 |
| Median call to arrival time, min (IQR)b | 13.0 (9.0−20.0) | 12.0 (8.0−19.0) | 102 (6.6) | 14.0 (9.0−22.0) | 358 (28.3) | 0.000 | 13.0 (9.0−20.0) | 235 (15.9) | 15.0 (9.0−23.0) | 170 (31.7) | 0.002 |
| Ambulance arrived within 8 minb | 535 (22.8) | 389 (27.0) | 102 (6.6) | 146 (16.1) | 358 (28.3) | 0.000 | 275 (22.1) | 235 (15.9) | 48 (13.1) | 170 (31.7) | 0.000 |
| Ambulance arrived within 15 minb | 1451 (61.9) | 936 (65.0) | 102 (6.6) | 515 (56.9) | 358 (28.3) | 0.000 | 760 (61.1) | 235 (15.9) | 199 (54.2) | 170 (31.7) | 0.018 |
| Utstein subgroup | |||||||||||
| Witnessed by emergency services personnel (subgroup 1) | 365 (11.5) | 182 (10.6) | 0 (0.0) | 183 (12.7) | 0 (0.0) | 0.066 | 173 (10.5) | 0 (0.0) | 86 (13.8) | 0 (0.0) | 0.026 |
| Shockable initial rhythm and bystander witnessed (subgroup 2a) | 514 (16.4) | 291 (17.0) | 12 (0.7) | 223 (15.7) | 28 (1.9) | 0.336 | 271 (16.7) | 25 (1.5) | 95 (15.5) | 11 (2.0) | 0.518 |
| Shockable initial rhythm and bystander CPR (subgroup 2b) | 363 (11.5) | 208 (12.1) | 5 (0.3) | 155 (10.8) | 28 (1.9) | 0.253 | 199 (12.1) | 20 (1.2) | 60 (9.7) | 11 (2.0) | 0.103 |
| Non-shockable initial rhythm and bystander witnessed (subgroup 2c) | 1549 (49.5) | 846 (49.4) | 12 (0.7) | 703 (49.6) | 26 (1.8) | 0.941 | 822 (50.5) | 22 (1.3) | 301 (49.2) | 12 (2.2) | 0.572 |
| Patients with ROSC admitted to hospital N (%) | 815 (27.6) | 525 (32.1) | 5 (0.3) | 290 (22.0) | 13 (0.9) | 0.000 | 441 (28.9) | 6 (1.5) | 107 (18.4) | 9 (0.5) | 0.000 |
| Patients with ongoing CPR admitted to hospital | 143 (4.5) | 38 (2.2) | 5 (0.3) | 105 (7.3) | 13 (0.9) | 0.000 | 87 (5.3) | 6 (1.5) | 37 (5.9) | 9 (0.5) | 0.000 |
| Donation in asystole | 53 (1.7) | 46 (2.6) | 5 (0.3) | 7 (0.5) | 13 (0.9) | 0.000 | 28 (1.7) | 6 (1.5) | 0 (0.0) | 9 (0.5) | 0.000 |
| In hospital treatment | |||||||||||
| Treatment with thrombolysis, N (%) | 13 (1.6) | 8 (1.5) | 0 (0.0) | 5 (1.7) | 0 (0.0) | 0.827 | 0 (0.0) | 0 (0.0) | 9 (2.0) | 0 (0.0) | 0.136 |
| Treatment with PCI, N (%) | 198 (24.3) | 119 (22.7) | 0 (0.0) | 79 (27.2) | 0 (0.0) | 0.145 | 28 (26.2) | 0 (0.0) | 102 (23.1) | 0 (0.0) | 0.507 |
| Treatment with ICD implant | 35 (4.3) | 24 (4.6) | 0 (0.0) | 11 (3.8) | 0 (0.0) | 0.600 | 4 (3.7) | 0 (0.0) | 18 (4.1) | 0 (0.0) | 0.871 |
| Treatment with TTM, N (%) | 56 (6.9) | 33 (6.3) | 0 (0.0) | 23 (7.9) | 0 (0.0) | 0.374 | 6 (5.6) | 0 (0.0) | 32 (7.3) | 0 (0.0) | 0.547 |
| Survival at hospital discharge | 276 (8.7) | 168 (9.8) | 0 (0.0) | 108 (7.5) | 0 (0.0) | 0.023 | 146 (8.8) | 0 (0.0) | 42 (6.7) | 0 (0.0) | 0.105 |
Average weekly incidence of OHCA resuscitation attempts per 100,000 inhabitants.
Cases witnessed by emergency services personnel were excluded from this analysis.
Patient, resuscitation and treatment characteristics
Participant and OHCA characteristics and differences between the non-COVID period and COVID period, and NPW and PW are presented in Table 1. No baseline gender differences were found, with average representation across time-periods being 70.6% male and 29.4% female. Patients from the COVID period were significantly younger than those from the non-COVID period. Pandemic week patients were also younger than non-pandemic weeks patients, with fewer patients aged 75 and older being treated during PW.
Relative to the non-COVID period, OHCA was more likely to occur at home and bystander CPR was less likely during the COVID period, with these differences remaining even when cardiac arrest was witnessed. More OHCAs also occurred at home during PW than NPW. The time-interval between call placement and ET arrival was longer during PW than NPW, with ambulances also being less likely to arrive within 8 and 15 min, respectively.
Airway isolation was less often performed during the COVID period than the non-COVID period, with an increase in the use of supraglottic devices and a decline in orotracheal intubation. This same pattern was seen when comparing non-pandemic weeks and pandemic weeks. Only one difference emerged in the profile of cases treated regarding Utstein subgroups with more OHCAs being witnessed by emergency team during pandemic weeks than non-pandemic weeks.
No differences regarding in-hospital care, percutaneous coronary intervention, hypothermia treatment, implantable cardioverter-defibrillator implant or thrombolysis treatment use were found between any of the groups
Survival following OHCA
Odd ratios, confidence intervals and p-values are provided in Table 2 . Odds of ROSC upon hospital admission were more favourable in the non-COVID period than the COVID period and in non-pandemic weeks than in pandemic weeks. These differences remained when only arrests witnessed by emergency teams or by a bystander but without a shockable initial rhythm were considered. Survival to discharge was more likely in the non-COVID period than the COVID period both overall for all patients and when cardiac arrest was witnessed by ET. Relative to pandemic weeks, survival to hospital discharge was more likely in non-pandemic weeks when OHCA was witnessed and when no shockable initial rhythm was present.
Table 2.
Comparison of overall survival odds between a non-COVID-19 period (2017/2018) and the COVID-19 period (2020), and non-pandemic weeks (non-COVID-19 period/COVID-19 period February the 1st to March the 10th) and pandemic weeks (COVID-19 period March 11th to April 30th). Data is presented overall and stratified according to resuscitation characteristics. Data collected between February the 1st and April the 30th.
| Survival to hospital admission | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Non-COVID-19 period (NCovP) | COVID-19 period (CovP) | NCovP v CovP, OR (95%CI) | p-value | Non-pandemic weeks (PW) | Pandemic weeks (NPW) | NPW v PW, OR (95%CI) | p-value | ||
| All patients | 525/1634 (32.1) | 290/1321 (22.0) | 1.72 (1.46−2.04) | 0.000 | 441/1528 (28.9) | 107/580 (18.4) | 1.82 (1.44−2.32) | 0.000 | |
| OHCA at home | Yes | 250/994 (25.2) | 164/915 (17.9) | 1.57 (1.26−1.97) | 0.000 | 204/936 (21.8) | 80/450 (17.8) | 1.33 (1.00−1.78) | 0.053 |
| No | 274/632 (43.4) | 126/406 (31.0) | 1.70 (1.31−2.22) | 0.000 | 236/587 (40.2) | 27/130 (20.8) | 2.52 (1.59−3.97) | 0.000 | |
| Witnessed OHCA | Yes | 453/1252 (36.2) | 261/1034 (25.2) | 1.73 (1.44−2.08) | 0.000 | 387/1186 (32.6) | 98/457 (21.4) | 1.82 (1.41−2.35) | 0.000 |
| No | 72/382 (18.8) | 29/287 (10.1) | 2.10 (1.32−3.34) | 0.002 | 54/342 (15.8) | 9/123 (7.3) | 2.35 (1.12−4.95) | 0.024 | |
| Bystander CPRa | Yes | 260/745 (34.9) | 133/497 (26.8) | 1.49 (1.16−1.91) | 0.002 | 204/643 (31.7) | 53/219 (24.2) | 1.47 (1.04−2.10) | 0.031 |
| No | 187/721 (25.9) | 125/682 (18.4) | 1.59 (1.23−2.06) | 0.000 | 180/743 (24.2) | 43/291 (14.8) | 1.85 (1.28−2.66) | 0.001 | |
| AED useda | Yes | 59/166 (35.5) | 30/102 (29.4) | 1.33 (0.78−2.26) | 0.298 | 38/136 (27.9) | 15/42 (35.7) | 0.69 (0.33−1.45) | 0.324 |
| No | 388/1300 (29.8) | 225/1072 (21.0) | 1.63 (1.35−1.97) | 0.000 | 344/1247 (27.6) | 80/466 (17.2) | 1.85 (1.41−2.43) | 0.000 | |
| Shockable initial rhythm | Yes | 211/363 (58.1) | 119/246 (48.4) | 1.53 (1.10−2.13) | 0.011 | 170/308 (55.2) | 50/108 (46.3) | 1.45 (0.93−2.26) | 0.100 |
| No | 302/1222 (24.7) | 156/1019 (15.3) | 1.84 (1.48−2.28) | 0.000 | 252/1161 (21.7) | 53/449 (11.8) | 2.11 (1.53−2.91) | 0.000 | |
| Utstein subgroup | |||||||||
| Witnessed by emergency services personnel | 78/168 (46.4) | 32/142 (22.5) | 3.29 (1.98−5.48) | 0.000 | 57/142 (40.1) | 11/70 (15.7) | 3.81 (1.81−8.02) | 0.000 | |
| Shockable initial rhythm and bystander witnessed | 153/271 (56.5) | 96/199 (48.2) | 1.42 (0.98−2.06) | 0.063 | 128/244 (52.5) | 43/87 (49.4) | 1.14 (0.70−1.87) | 0.600 | |
| Shockable initial rhythm and bystander CPR | 112/197 (56.9) | 70/133 (52.6) | 1.18 (0.75−1.85) | 0.470 | 98/177 (55.4) | 29/54 (53.7) | 1.04 (0.56−1.93) | 0.902 | |
| Non-shockable initial rhythm and bystander witnessed | 216/801 (27.0) | 123/668 (18.4) | 1.67 (1.30−2.14) | 0.000 | 190/776 (24.5) | 42/291 (14.4) | 2.03 (1.40−2.94) | 0.000 | |
| Survival to hospital discharge | |||||||||
| All patients | 168/1723 (9.8) | 108/1446 (7.5) | 1.38 (1.07−1.78) | 0.013 | 146/1652 (8.8) | 42/623 (6.6) | 1.37 (0.96−1.97) | 0.083 | |
| OHCA at home | Yes | 65/1042 (6.2) | 49/988 (5.0) | 1.31 (0.89−1.92) | 0.172 | 50/1003 (5.0) | 24/478 (5.0) | 1.04 (0.63−1.72) | 0.873 |
| No | 103/672 (15.3) | 59/458 (12.9) | 1.28 (0.90−1.81) | 0.173 | 96/643 (14.9) | 18/145 (12.4) | 1.21 (0.70−2.08) | 0.493 | |
| Witnessed OHCA | Yes | 149/1331 (11.2) | 100/1137 (8.8) | 1.39 (1.06−1.82) | 0.016 | 135/1291 (10.5) | 37/493 (7.5) | 1.50 (1.02−2.20) | 0.037 |
| No | 19/392 (4.8) | 8/309 (2.6) | 1.99 (0.85−4.64) | 0.111 | 11/361 (3.0) | 5/130 (3.8) | 0.78 (0.26−2.31) | 0.648 | |
| Bystander CPRa | Yes | 87/788 (11.0) | 52/538 (9.7) | 1.21 (0.84−1.74) | 0.315 | 66/694 (9.5) | 22/230 (9.6) | 0.98 (0.59−1.64) | 0.948 |
| No | 50/753 (6.6) | 38/725 (5.2) | 1.38 (0.89−2.14) | 0.151 | 51/785 (6.5) | 15/307 (4.9) | 1.42 (0.78−2.57) | 0.252 | |
| AED useda | Yes | 21/173 (12.1) | 16/113 (14.2) | 0.85 (0.42−1.72) | 0.852 | 15/150 (10.0) | 9/43 (20.9) | 0.42 (0.17−1.04) | 0.062 |
| No | 116/1368 (8.5) | 74/1145 (6.5) | 1.41 (1.04−1.92) | 0.026 | 102/1326 (7.7) | 28/492 (5.7) | 1.42 (0.92−2.19) | 0.117 | |
| Shockable initial rhythm | Yes | 211/363 (58.1) | 119/246 (48.4) | 1.53 (1.10−2.13) | 0.011 | 170/308 (55.2) | 33/118 (28.0) | 1.45 (0.93−2.26) | 0.100 |
| No | 302/1222 (24.7) | 156/1019 (15.3) | 1.84 (1.48−2.28) | 0.000 | 252/1161 (21.7) | 252/1161 (21.7) | 2.11 (1.53−2.91) | 0.000 | |
| Utstein subgroup | |||||||||
| Witnessed by emergency services personnel | 31/182 (17.0) | 18/183 (9.8) | 2.06 (1.10−3.87) | 0.025 | 29/173 (16.8) | 5/86 (5.8) | 3.67 (1.35−10.02) | 0.011 | |
| Shockable initial rhythm and bystander witnessed | 84/291 (28.9) | 56/223 (25.1) | 1.25 (0.84−1.86) | 0.281 | 70/271 (25.8) | 28/95 (29.5) | 0.83 (0.49−1.41) | 0.498 | |
| Shockable initial rhythm and bystander CPR | 62/208 (29.8) | 40/155 (25.8) | 1.23 (0.77−1.97) | 0.394 | 50/199 (25.1) | 19/60 (31.7) | 0.70 (0.37−1.33) | 0.276 | |
| Non-shockable initial rhythm and bystander witnessed | 33/846 (3.9) | 19/703 (2.7) | 1.53 (0.86−2.72) | 0.149 | 30/822 (3.6) | 3/301 (1.0) | 4.01 (1.21−13.29) | 0.023 | |
Cases witnessed by emergency services personnel were excluded from this analysis.
Further, no change in survival trends at hospital admission and at hospital discharge when comparing Covid period versus Non-Covid period (Fig. 3B and 3 C respectively).
Regional comparison of the COVID period according to infection level
Regional comparisons of all participant and OHCA characteristics are presented in Table 3 with few meaningful differences emerging.
Table 3.
Resuscitation characteristics compared between non-pandemic weeks (February 1st to March 10th 2020) and pandemic weeks (March 11th to April 30th 2020), stratified according to COVID-19 incidence.
| Non-pandemic weeks |
Pandemic weeks |
|||||||
|---|---|---|---|---|---|---|---|---|
| COVID-19 incidence |
COVID-19 incidence |
|||||||
| Low | Medium | High | p-value | Low | Medium | High | p-value | |
| All resuscitations† | 152 (0.49) | 416 (0.49) | 255 (0.49) | 0.343 | 107 (0.29) | 321 (0.30) | 195 (0.30) | 0.330 |
| Female, N (%) | 38 (25.0) | 125 (30.0) | 65 (25.5) | 0.313 | 31 (29.0) | 102 (31.9) | 57 (29.2) | 0.759 |
| Age (years), mean (SD) | 62.36 (15.4) | 65.32 (17.5) | 65.49 (17.9) | 0.152 | 61.81 (15.8) | 64.92 (15.6) | 62.83 (15.0) | 0.124 |
| Aged 14 and under | 0 (0.0) | 7 (1.7) | 6 (2.4) | 0.182 | 1 (0.9) | 4 (1.3) | 3 (1.5) | 0.905 |
| Aged 75 and over | 34 (22.7)a | 145 (34.9)b | 100 (39.2)b | 0.003 | 24 (22.6) | 92 (28.7) | 40 (20.5) | 0.091 |
| OHCA at home, N (%) | 88 (57.9) | 252 (60.6) | 170 (66.7) | 0.150 | 75 (70.1) | 248 (77.3) | 155 (79.5) | 0.172 |
| Witnessed OHCA, N (%) | 120 (78.9) | 317 (76.2) | 207 (81.2) | 0.309 | 91 (85.0) | 246 (76.6) | 156 (80.0) | 0.168 |
| Bystander CPR performed, N (%)+ | 58 (40.8)a | 123 (35.0)a | 127 (54.5)b | 0.000 | 28 (31.8)a | 92 (33.3)a | 110 (63.6)b | 0.000 |
| AED used, N (%)+ | 17 (12.1)a, b | 24 (6.8)b | 29 (12.6)a | 0.042 | 4 (4.5)a | 13 (4.7)a | 26 (15.0)b | 0.000 |
| Shockable initial rhythm, N (%) | 39 (26.9) | 69 (17.8) | 56 (22.1) | 0.059 | 25 (26.0) | 53 (17.5) | 40 (20.7) | 0.178 |
| Airway isolation | 134 (88.2) | 353 (86.9) | 210 (83.0) | 0.251 | 92 (86.0) | 249 (78.8) | 159 (84.1) | 0.147 |
| Orotracheal intubation | 81 (60.4)a | 275 (77.9)b | 182 (86.7)c | 0.000 | 44 (47.8)a | 159 (63.9)b | 117 (73.6)c | 0.000 |
| Supraglottic device | 12 (9.0) | 28 (7.9) | 18 (8.6) | 0.878 | 20 (21.7) | 51 (20.5) | 39 (24.5) | 0.958 |
| Median call to arrival time, min (IQR)+ | 17.5 (12.0−33.0)a | 15.0 (9.0−21.0)b | 11.0 (8.0−18.5)c | 0.000 | 16.5 (10.0−27.5) | 14.0 (9.0−23.0) | 15.0 (10.0−22.0) | 0.757 |
| Ambulance arrived within 8 min+ | 4 (8.0)a | 46 (17.0)a, b | 48 (22.1)b | 0.050 | 3 (13.6) | 22 (12.0) | 23 (14.3) | 0.182 |
| Ambulance arrived within 15 min+ | 21 (42.0)a | 146 (53.9)a | 149 (68.9)b | 0.000 | 11 (50.0) | 103 (56.0) | 85 (52.8) | 0.772 |
| Utstein subgroup | ||||||||
| Witnessed by emergency services personnel (subgroup 1) | 10 (6.6)a | 65 (15.6)b | 22 (8.6)a | 0.002 | 19 (17.8) | 45 (14.0) | 22 (11.3) | 0.292 |
| Shockable initial rhythm and bystander witnessed (subgroup 2a) | 29 (19.6) | 57 (14.1) | 42 (16.6) | 0.270 | 18 (17.5) | 44 (14.0) | 33 (17.0) | 0.547 |
| Shockable initial rhythm and bystander CPR (subgroup 2b) | 28 (18.7)a | 31 (7.5)b | 36 (14.2)a | 0.000 | 8 (7.5) | 26 (8.2) | 26 (13.3) | 0.112 |
| Non-shockable initial rhythm and bystander witnessed (subgroup 2c) | 77 (52.0)a,b | 184 (45.4)a | 141 (55.7)b | 0.031 | 50 (48.5) | 151 (47.9) | 100 (51.5) | 0.724 |
| Patients with ROSC admitted to hospital N (%) | 30 (24.8) | 87 (22.8) | 66 (27.6) | 0.405 | 16 (17.8)a,b | 41 (13.7)a | 50 (26.3)b | 0.002 |
| Patients with ongoing CPR admitted to hospital | 26 (17.1)a | 30 (7.2)b | 12 (4.7)b | 0.000 | 13 (12.1)a | 20 (6.2)b | 4 (2.1)c | 0.000 |
| Donation in asystole | 0 (0.0) | 4 (1.0) | 3 (1.2) | 0.441 | 0 (0.0) | 0 (0.0) | 0 (0.0) | – |
| In hospital treatment | ||||||||
| Treatment with thrombolysis, N (%) | 1 (1.8) | 1 (0.9) | 3 (3.8) | 0.339 | 0 (0.0) | 0 (0.0) | 0 (0.0) | – |
| Treatment with PCI, N (%) | 10 (17.9) | 29 (24.8) | 23 (29.5) | 0.306 | 5 (17.2) | 20 (32.8) | 12 (22.2) | 0.219 |
| Treatment with ICD implant | 0 (0.0) | 3 (2.6) | 4 (5.1) | 0.202 | 0 (0.0) | 2 (3.3) | 3 (5.6) | 0.417 |
| Treatment with TTM, N (%) | 1 (1.8) | 14 (12.0) | 6 (7.7) | 0.075 | 0 (0.0) | 5 (8.2) | 3 (5.6) | 0.284 |
| Survival at hospital discharge | 15 (9.9) | 30 (7.2) | 21 (8.2) | 0.580 | 7 (6.5) | 17 (5.3) | 18 (9.2) | 0.224 |
The reference population for all included regions was 30,298,000 (low incidence regions: 8,819,000; medium incidence regions: 11,327,000; high incidence regions: 10,152,000).
Superscript denotes statistically significant differences between adjacent cells.
Average weekly incidence of OHCA resuscitation attempts per 100,000 inhabitants.
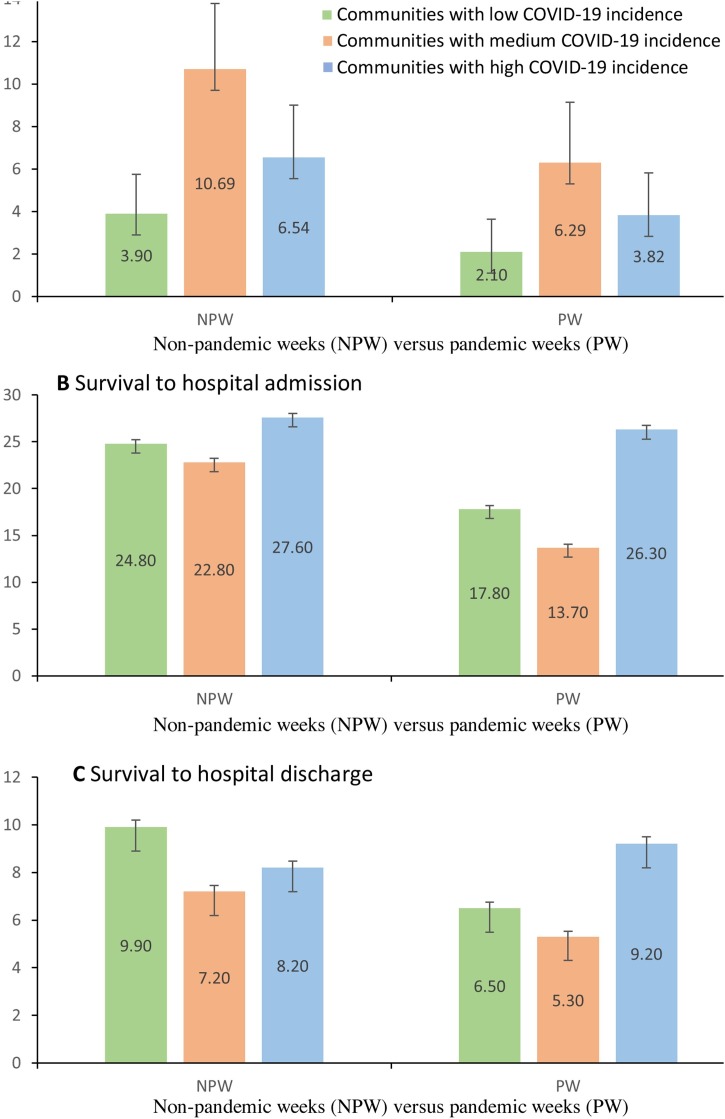
The multilevel model pertaining to accumulated COVID-19 incidence showed that higher incidence within different regions overall (Z = 2.05; p = 0.040; SE = 0.33) led to fewer resuscitation attempts being made (B = −0.004; t = −55.84; p = 0.000). Thus, another model was developed with the aim of identifying whether there were differential effects within regions with low, medium and high Covid-19 incidence. This model showed that all three COVID-19 incidence groups (low, medium and high) predicted fewer resuscitation attempts relative to the absence of COVID-19, however, similar coefficients were seen for each of the three groups (low: B = −2.51; p = 0.000; medium: B = −2.45; p = 0.000; high: B = −2.51; p = 0.000). Further, overall regional effects were no longer significant. Resuscitation attempts and survival according to low, medium and high COVID-19 incidence regions are presented in Fig. 4 A, B and C. No regional effects pertaining to survival emerged.
Fig. 4.
Average resuscitation attempts (A), survival to hospital admission (B) and survival to hospital discharge (C) during pandemic weeks (PW) and non-pandemic weeks (NPW) of 2020, stratified according to autonomous community grouped according to COVID-19 incidence (low/medium/high).
Discussion
During the COVID-19 pandemic, OHCA resuscitation attempts, survival to hospital admission and survival at discharge declined. These effects were independent of infection incidence in different regions.
Previous studies have reported important increases in the number of OHCAs,4, 5, 7 however, worryingly some of these studies have also identified that a lower percentage of resuscitation attempts are being perfomed4, 5. Further, one of these studies outlined that a greater proportion of resuscitation attempts end up being terminated on-scene.5 In comparison with other countries, Spain typically reports a lower percentage of resuscitation attempts for OHCA. This observation may be explained by EMS organizational (with physician on board), epidemiological and legal and social characteristics.13, 17, 18 In the present study, the drop in OHCA resuscitation attempts is highly significant, especially during the weeks from which the pandemic was declared by WHO (March 11th) and the Spanish government established the lockdown (March 14th). This important decrease in the number of cases attended may well have contributed to the excess mortality reported in Spain over the same period and could be equivalent to the excess on-site mortality reported in the articles from Lombardy, Paris and New York. This decline occurred in all of the regions studied, regardless of their infection level. This could indicate a degree of social reluctance to seek help, in addition to purely care-related factors. These factors may include the saturation of health resources, country-level inequality, longer EMS response times (indicated through the significant drop seen in response times of 8 min and less) and reduced bystander resuscitation. The combined effect of experiencing a higher proportion of arrests at home, response delays and decreased bystander PCR could lead to a decrease in the number of indicated resuscitations. Indeed, the number of futile resuscitations significantly increased during the study period.
With regards to the profile of treated patients, they were somewhat younger and fewer resuscitations were performed within the over 75 s age group during PW. No meaningful changes were found according to Utstein subgroups.
A change in attitudes of emergency teams is also suggested regarding airway management, with a clear increase in the use of supraglottic devices in accordance with guidelines laid out by leading scientific societies.19, 20, 21 Similarly, during the pandemic, emergency teams did not include cases in asystolic organ donation programs.
The final results offer cause for concern when comparing both periods. Hospital admission with ROSC fell to 22.0 % during the COVID period, a decrease from Non-COVID period levels of 32.1%. Survival at discharge was also found to be at just 7.5%, declining from 9.8% prior to the pandemic. Similar outcomes emerged when comparing PW and NPW, with drops of more than 10% in ROSC at hospital and 2% in survival at discharge, although differences in survival at hospital discharge were not significant.
The present results are expected given the importance of the location of CPR at home21, 22 and adequate execution of the first links in the chain of survival.23 Indeed, survival in patient groups with shockable initial rhythm or CPR witnessed by emergency team members were similar. This was not the case in those who were bystander witnessed and without a shockable initial rhythm, with this sub-group demonstrating much worse survival rates during pandemic weeks. This group accounts for a large number of patients, approximately half of all cases, has a worse overall prognosis and is even more susceptible to the timing of intervention and bystander CPR. Actual survival achieved within this group, 1%, would lead it to be considered a futile action if it did not incorporate so many cases.24
The most relevant aspect of our study is the influence that the pandemic has had on all participating communities, regardless of infection level. A significant fall is seen in the number of resuscitation attempts and in successful outcomes. Significant differences did not always emerge, however, clear trends did emerge and the lack of significance was likely due to loss of statistical power due to the decline in patients treated. In some instances, greater detriment was seen in communities with low and medium infection rates. This suggests that the presence of the disease per se, rather than its intensity, in addition to the strict social distancing measures adopted have dictated this negative influence on health care.
Beyond the formal aspects of each of the examined variables, the COVID-19 pandemic has, overall, led to important set-backs in the main determinants of survival following OHCA. Key initiatives are required to increase the number of resuscitation attempts. Citizen engagement to promote immediate initiation of resuscitation, public access to early defibrillation and quick response capacity of emergency services have all been significantly affected, regardless of the level of infection. OHCA treatment during times of a health pandemic must reconsider specific measures for each patient, alongside the most appropriate health and social strategies for this public health issue. Studies and close monitoring will be needed to see if this impact remains over time and successful strategies must be modified.25, 26, 27
The COVID-19 pandemic has also had a negative impact on processes favouring a network approach, in other words, processes running from the pre-hospital stage to in-hospital treatment. Response networks for ST-elevation myocardial infarction and stroke have seen a decline in the number of patients attended and a worsening of the outcomes obtained for response times and complications.28, 29, 30 Since there was no difference in hospital treatment, despite the disparity in hospital resource saturation in some of the regions, the present data makes it apparent that the COVID-19 pandemic has had a particularly negative influence on pre-hospital care.
Although other data are not yet available to verify these effects on emergency services in other countries and in other health models, our findings call for the need to adapt out-of-hospital care for citizens and health professionals during periods of serious infection risk.
Limitations
Our results reflect experiences and implications of the COVID-19 pandemic in relation to OHCA in a country with a specific physician-led pre-hospital care model. It would be enlightening to collect data from other countries with other care models in relation to OHCA. OHSCAR registers reanimation attempts for OHCA and so we cannot know, as has been reported in other registers, know whether the number of OHCAs for which it was decided not to initiate resuscitation manoeuvres increased. We are also unable to establish the reasons for stopping advanced life support when cases were considered futile. The data available within OSCHAR precluded us from a direct comparison with a pre-COVID period. Finally, it is possible that with a larger sample the negative trend in survival at discharge would have been significant.
Role of the funding source
This work was supported by the Spanish Resuscitation Council. The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Statement authors’ contribution
- Study design: F. Rosell, J I Ruiz, X Jiménez, J A Iglesias, A Echarri.
- Literature search: F. Rosell, J I Ruiz, X Jiménez, J A Iglesias, J M Navalpotro, A Daponte.
- Tables and Figures: E Knox, P Fernández.
- Data collection and quality control: D Alonso, A Forner, M García-Ochoa, N López, B Mainar, X Jiménez, J A Iglesias, J M Navalpotro, S Batres, M I Ceniceros, F A Guirao, J A Cortés, B Fernández, J I Ruiz.
- Data analysis: E Knox, A Daponte, I Mateo, P Fernández.
- Data interpretation: E Knox, A Daponte, I Mateo, P Fernández, F Rosell, J I Ruiz.
- Writing: F Rosell, A Daponte, E Knox, I Mateo, J I Ruiz, P Fernández.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.resuscitation.2020.09.037.
Contributor Information
On behalf of OHSCAR investigators:
Francisco José Mellado Vergel, Sonia Royo, Bernardo Aguilo, Elvira Prieto Cuervo, Juan Jose Garcia Lindez, Marta Sansegundo Campo, Ignacio del Campo Arenal, Carmen del Pozo Pérez, Margarita Baez del Pozo, Marta de la Cruz Martínez, Angels Mora Vives, Francisco José Carmona Jiménez, Silvia Solà Muñoz, Xavier Escalada Roig, Carmen Escriche, María Remedios Belmonte Gómez, Antonio José Fernández Barril, Juan Ramírez Márquez, Gabina Pérez López, Pedro Dacal Pérez, Antonio Rodríguez Rivera, Elena Pastor González, María luz Sabin Gómez, Carmen Camacho Leis, Francisco Alfonso Peinado Vallejo, Alfredo Carrillo Moya, Yago Muñecas Cuesta, Belén Muñoz Isabel, Manuel José González León, Juan Ignacio Les González, Antonia Sáez Jiménez, José Muñoz Pastor, María Teresa López Pérez, Maitane Tainta Laspalas, Cristian Fernández Barreras, Mª Mar Vaqueriza Iturriza, Mario Jiménez Mercado, Blanca Alberro Aranzasti, Cristian Fernández Barreras, Amelie Le Gall, María Lourdes Bragado-Blas, and Basilio Teja-Ruiz
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.WHO . 2020. Rapid Assessment of Service Delivery for NCDs During the COVID-19 Pandemic.https://www.who.int/news-room/detail/01-06-2020-covid-19-significantly-impacts-health-services-for-noncommunicable-diseases (Accessed 29 July 2020) [Google Scholar]
- 2.Rosenbaum L. The untold toll—the pandemic’s effects on patients without Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMms2009984. published April 17. [DOI] [PubMed] [Google Scholar]
- 3.Solomon M., Mc Nulty E.J., Rana J., et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020 doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 4.Baldi E., Sechi G.M., Primi R., et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020 doi: 10.1056/NEJMc2010418. published online April 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marijon E., Karam N., Jost D., et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study [published online ahead of print, 2020 May 27] Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baldi E., Sechi G.M., Mare C., et al. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lai P.H., Lancet E.A., Weiden M.D., et al. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol. doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed]
- 8.Johns Hopkins University and Medicine. COVID-19 map. Johns Hopkins Coronavirus Resource Centre. https://coronavirus.jhu.edu/map.html (Accessed 11 June 2020).
- 9.Spanish Ministry of Health. Update 92: Coronavirus Disease (COVID-19-19). https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCovChina/documentos/Actualizacion_92_COVID-19-19.pdf. (Accessed 15 May 2020).
- 10.Daily Mortality Surveillance System (MoMo). Instituto de Salud Carlos III, Ministerio de Ciencia e Innovación, España. Available at: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/MoMo/Documents/informesMoMo2020/MoMo_Situacion%20a%203%20de%20mayo_CNE.pdf. (Accessed 15 May 2020).
- 11.Medeiros Figueiredo A., Daponte-Codina A., Moreira Marculino Figueiredo D.C., Toledo Vianna R.P., Costa de Lima K., Gil-García E. Factores asociados a la incidencia y la mortalidad por COVID-19 en las comunidades autónomas [Factors associated with the incidence and mortality from COVID-19 in the regions of Spain] [published online ahead of print, 2020 May30] Gac Sanit. 2020 doi: 10.1016/j.gaceta.2020.05.004. S0213-9111(20)3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spanish Ministry of Health. Update 30: Coronavirus Disease (COVID-19-19. https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCovChina/documentos/Actualizacion_92_COVID-19-19.pdf. (Accessed 15 May 2020).
- 13.Rosell-Ortiz F., Escalada-Roig X., Fernández Del Valle P., et al. Out-of-hospital cardiac arrest (OHCA) attended by mobile emergency teams with a physician on board. Results of the Spanish OHCA Registry (OSHCAR) Resuscitation. 2017;113:90–95. doi: 10.1016/j.resuscitation.2017.01.029. [DOI] [PubMed] [Google Scholar]
- 14.Perkins G.D., Jacobs I.G., Nadkarni V.M., et al. Cardiac arrest and cardiopulmonary resuscitation outcomes reports: update of the utstein resuscitation registry templates for out-of-hospital cardiac arrest. A statement of healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, Inter-American Heart Foundation, Resuscitation Council of Sothern Africa, Resuscitation Council of Asia); and the American heart association emergency cardiovascular care committee and the council on cardiopulmonary, critical care, perioperative and resuscitation. Resuscitation. 2015;96:328–340. doi: 10.1016/j.resuscitation.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 15.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gräsner J.T., Lefering R., Koster R.W., et al. EuReCa ONE-27 Nations, ONE Europe, ONE Registry. A prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188–195. doi: 10.1016/j.resuscitation.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 17.Gräsner J.T., Wnent J., Herlitz J., et al. Survival after out-of-hospital cardiac arrest in Europe - Results of the EuReCa TWO study. Resuscitation. 2020;148:218–226. doi: 10.1016/j.resuscitation.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 18.El‐Boghdadly K., Wong D.J.N., Owen R., et al. Risks to healthcare workers following tracheal intubation of patients with COVID-19: a prospective international multicentre cohort study Anesthesia First published: 09 June 2020 10.1111/anae.15170. [DOI] [PMC free article] [PubMed]
- 19.European Resuscitation Council. European resuscitation council COVID-19 guidelines. Resuscitation [Internet]. 2020 [cited 2020 June 29]; 23:255–258. Available from: https://erc.edu/sites/5714e77d5e615861f00f7d18/content_entry5ea884fa4c84867335e4d1ff/5ea885f34c84867335e4d20e/files/ERC_covid19_pages.pdf?1588257310%0D.
- 20.Edelson D.P., Topjian A.A. On behalf of the American Heart Association ECC Interim COVID Guidance Authors. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19 from the emergency cardiovascular care committee and get with the guidelines-resuscitation adult and pediatric task forces of the American Heart Association. Circulation. 2020;141:e933–e943. doi: 10.1161/CIRCULATIONAHA.120.047463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weisfeldt M.L., Everson-Stewart S., Sitlani C., et al. Ventricular tachyarrhythmias after cardiac arrest in public versus at home. N Engl J Med. 2011;364:313–321. doi: 10.1056/NEJMoa1010663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sondergaard K.B., Wissenberg M., Gerds T.A., et al. Bystander cardiopulmonary resuscitation and long-termoutcomes in out-of-hospital cardiac arrest according to location of arrest. Eur Heart J. 2019;40:309–318. doi: 10.1093/eurheartj/ehy687. [DOI] [PubMed] [Google Scholar]
- 23.Strömsöe A., Leif Svensson L., Axelsson ÅB., et al. Improved outcome in Sweden after out-of-hospital cardiac arrest and possible association with improvements in every link in the chain of survival. Eur Heart J. 2015;36:863–871. doi: 10.1093/eurheartj/ehu240. [DOI] [PubMed] [Google Scholar]
- 24.Schneiderman L.J. Defining medical futility and improving medical care. J Bioeth Inq. 2011;8:123–131. doi: 10.1007/s11673-011-9293-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garcia S., Albaghdadi M.S., Meraj P.M., et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perkins G.D., Couper K. COVID-19: Long-Term Effects on the Community Response to Cardiac Arrest? Published Online May 27, 2020 10.1016/S2468-2667(20)30134-1. [DOI] [PMC free article] [PubMed]
- 27.Blewer A.L., Wah Ho A.F., Shahidah N., et al. Impact of bystander-focused public health interventions on cardiopulmonary resuscitation and survival: a cohort study. Lancet Public Health. 2020;5:e428–e436. doi: 10.1016/S2468-2667(20)30140-7. [DOI] [PubMed] [Google Scholar]
- 28.De Rosa S., Spaccarotella C., Basso C., et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kansagra A.P., Goyal M.S., Hamilton S., Albers G.W. Collateral effect of Covid-19 on stroke evaluation in the United States. N Engl J Med. 2020;383:400–401. doi: 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rudilosso S., Laredo C., Vera V., et al. Acute stroke care is at risk in the era of COVID-19: experience at a comprehensive stroke center in Barcelona. Stroke. 2020;51:1991–1995. doi: 10.1161/STROKEAHA.120.030329. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.