Abstract
Social distancing measures have been used to contain the COVID-19 pandemic; nevertheless, it causes unintended greater time at home and consequently a reduction in general physical activity and an increase in sedentary time, which is harmful to older people. A decrease in daily physical activities and an increase in sedentary time culminates in an impactful skeletal muscle disuse period and reduction in neuromuscular abilities related to functional capacity. Home-based resistance training is a strategy to mitigate physical inactivity and improve or retain muscle function and functional performance. Therefore, it is an urgent time to encourage older people to perform resistance exercises at home to avoid a harmful functional decline and promote physical health.
Keywords: Social isolation, Skeletal muscle disuse, Neuromuscular impairment, Functional capacity, Home-based exercise, Elderly
Highlights
-
•
Skeletal muscle disuse is related to reduction in neuromuscular abilities associated to functional capacity in older people;
-
•
COVID-19 pandemic promotes unintended physical inactivity and increased sedentary time;
-
•
Home-based resistance training is effective to improve or retain muscle and functional performance in older people;
-
•
It is an urgent time to encourage older people to perform resistance exercises at home to promote physical health.
1. COVID-19 pandemic, physical inactivity, neuromuscular and functional impairments in older people
The novel coronavirus (COVID-19) global pandemic has negatively impacted the population's health and the worldwide economy (Andersen et al., 2020). In August 2020, 216 countries have reported the disease, with more than 20 million reported cases and more than 750,000 deaths (World Health Organization, 2020a). Environmental contamination is the COVID-19 transmission route (Ong et al., 2020). For this reason, social distancing measures have been recommended to slow the virus transmission and to align the medical care capacity to the number of cases (World Health Organization, 2020b, World Health Organization, 2020c). These measures have directly impacted older people as the case-fatality rates dramatically increase with age, approximately 8% to 13% in individuals between the ages of 70 and 79 years and 15% to 20% in individuals with 80 years or older (Onder et al., 2020). In the United States, 8 out of 10 COVID-19-related deaths have occurred in adults aged 65 years or older (Centers for Disease Control and Prevention, 2020).
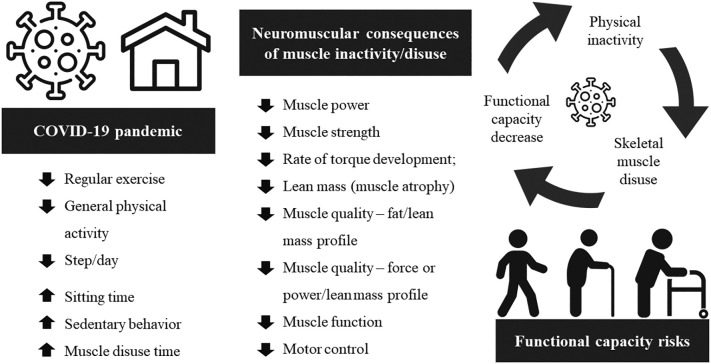
Social distancing measures are essential strategies used to contain the COVID-19 spread (World Health Organization, 2020b, World Health Organization, 2020c). Nevertheless, it has unintended negative consequences in increasing the population's time at home and, thus, general physical inactivity and sedentary behavior. Recently, Schuch et al. (2020) showed that the time spent on moderate to vigorous physical activity decreased by 60% in young adults, while sedentary time increased by 42% in the current pandemic. Also, López-Sánchez et al. (2020) showed a decrease in moderate and vigorous physical activity in men and women with chronic conditions during the COVID-19 quarantine. It is observed that both incidental and planned physical activity have decreased in all people with social distancing; however, physical inactivity has harmful consequences in older adults (Cunningham et al., 2020). As shown in Fig. 1 , isolation at home due to social distancing measures can promote an unintended reduction of daily physical activities outside the home (e.g. work, market, leisure activities, walking) and increase the sedentary time (e.g. sitting and lying) (López-Sánchez et al., 2020; Schuch et al., 2020). This scenario culminates in an impactful skeletal muscle disuse period, inducing a reduction of critical neuromuscular abilities (Bamman et al., 1998; Kortebein et al., 2008, Kortebein et al., 2007; Paddon-Jones et al., 2004; Pagano et al., 2018), which are related to the loss of intrinsic capacity and functional ability in older people (Byrne et al., 2016; Misic et al., 2007; Wilhelm et al., 2014). Thus, counterattack the skeletal muscle disuse is essential in this period of unintended decreased physical activity due to social distancing measures.
Fig. 1.
COVID-19 pandemic and physical inactivity consequences, neuromuscular and functional impairments in older people.
Skeletal muscle disuse periods (e.g. bed rest, sitting time) have been linked not only to lower-limb neuromuscular impairments such as loss of strength, power output, muscle mass, and quality but also to functional capacity decline (Kortebein et al., 2008, Kortebein et al., 2007; Paddon-Jones et al., 2004; Pagano et al., 2018). Moreover, even a decrease in the number of daily steps (i.e. a reduction in overall low intensity aerobic physical activity) impacts the levels of muscle strength in older individuals (Reidy et al., 2018). In addition, sarcopenic older people, as well as those with lower strength levels and higher sitting time, are at greater risk for premature mortality (Kim et al., 2014; León-Muñoz et al., 2013; Li et al., 2018). Likewise, gait and sit-to-stand ability are functional outcomes strongly associated with all-cause mortality, especially in the oldest old (Landi et al., 2010; Studenski, 2011). Moreover, a recent study by Esain et al. (2019) showed that three months of no physical exercise led to a decline in physical function, mental health and quality of life in physically active older people. Such adverse consequences may be even greater in older individuals who are sedentary or in poor health conditions. Thus, to combat skeletal muscle disuse is essential in the COVID-19 pandemic period.
2. Home-based resistance training as a strategy to avoid a harmful functional decline and promote physical health
Considering the impact of physical inactivity on overall health and functionality, strategies to mitigate the unintended negative consequences of the increased sedentary behavior are necessary. In this scenario, resistance exercise emerges as an effective modality, especially to the lower limbs, as it suffers abrupt loss and impairments with few weeks of inactivity (Fragala et al., 2019). Importantly, neuromuscular adaptations (e.g. muscle strength and power improvements) occur mainly with resistance exercise compared to aerobic exercise (Izquierdo et al., 2005; Villareal et al., 2017). Due to social distancing measures and measures to control access to gyms, home-based resistance training (HBRT) is a fundamental strategy to mitigate physical inactivity in the older population (e.g. workers, physically active, inactive, healthy, frail or chronic disease).
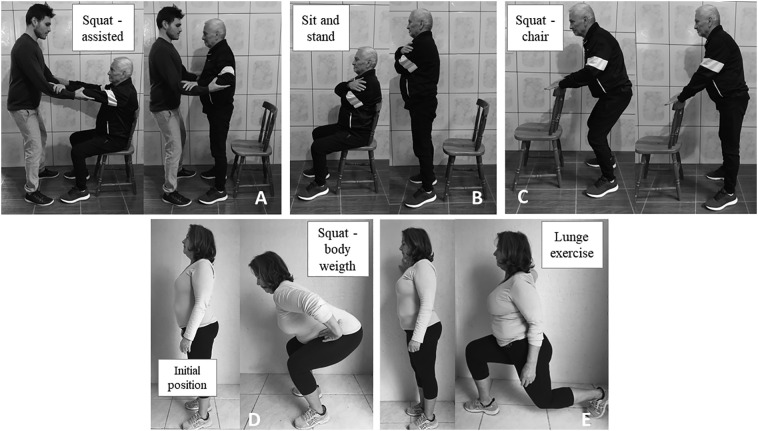
Previous literature has reported gains in muscle strength and functional capacity in older people using HBRT modality (Hill et al., 2015; Kis et al., 2019; Mikesky et al., 1994; Thiebaud et al., 2014). Also, a recent meta-analysis conducted by Kis et al. (2019) showed that even minimally supervised HBRT can be a safe, effective and low-cost exercise option to increase lower body muscle strength in older individuals with a variety of health conditions. HBRT can be designed using exercises that simulate daily physical activities like sit and stand up and step up, as well as climbing stairs when it is possible. It is important to note that HBRT can be performed with little material resources (i.e. chair, elastic and sticks), and accessible exercises (e.g. squat, hip flexion and calf-raise in a standing position) can be adapted to the current individuals' physical condition (Fig. 2, Fig. 3, Fig. 4 ).
Fig. 2.
Accessible lower-limb home-based resistance exercises. We emphasize the need to adjust the exercise according to individual physical capacity. Possible progression of the squat exercise is exhibited from A to E, from the simplest to most difficult execution performance.
Fig. 3.
Accessible lower-limb home-based resistance exercises. Possible progression of the calf-rise exercise is exhibited in panels A (chair) and 3B (wall).
Fig. 4.
Accessible lower-limb home-based resistance exercises. Possible hip-flexion exercise.
Based on strong evidence provided by the resistance exercise research area, older individuals should progress from 1 to 3 sets per exercise and 8 to 12 repetitions should be performed (Chodzko-Zajko et al., 2009; Fragala et al., 2019). The use of perceived exertion is an effective alternative to control exercise intensity. For older individuals on a scale from 0 to 10, moderate and vigorous intensity are represented by 5–6 and 7–8, respectively (Chodzko-Zajko et al., 2009). Two to three training sessions per week should be performed, and, whenever possible, three or more training sessions should be preferred (Chodzko-Zajko et al., 2009; Fragala et al., 2019; Thiebaud et al., 2014). Resistance exercise is also essential for individuals with fragility (Cadore et al., 2019, Cadore et al., 2013; Fragala et al., 2019). Frailty is characterized by the cumulative decline in several physiological systems that leads to a state of vulnerability, having as common indicators the presence of unintended weight loss, self-reported exhaustion, low energy expenditure per week, slow gait speed and weakness (Clegg et al., 2013). In frail older individuals, previous recommendations can be adapted. Due to their constant fatigue sensation and low physical activity levels, it might be necessary to use light or more tolerable intensities and lower number of repetitions and sets per exercise, making the exercise sessions more suitable for them (Fragala et al., 2019).
Another alternative of performing HBRT is the use of muscle power exercise, which is mainly characterized by performing the concentric phase of the movement as fast as possible (Byrne et al., 2016; Fragala et al., 2019; Radaelli et al., 2019, Radaelli et al., 2018). For example, in the exercise of sitting and getting up from the chair, the individual should be encouraged to stand from the chair (ascending/concentric phase) at the highest possible velocity (<1 s if possible), while the descending/eccentric phase (sitting) is performed in 2–3 s. Muscle power training is an effective and safe strategy to increase muscle strength and hypertrophy adaptations, as well as greater benefits in muscle power and functional capacity (Fragala et al., 2019; Radaelli et al., 2019, Radaelli et al., 2018; Ramírez-Campillo et al., 2014). Also, high-velocity training at home has also been shown to be effective for neuromuscular (e.g. muscle strength and power) and functional improvements (e.g. stair climb time, walking speed) (Fukumoto et al., 2017, Fukumoto et al., 2014; Mair et al., 2019; Orange et al., 2020). Similar to the traditional resistance training, muscle power training can be conducted with 1 to 3 sets per exercise (Fragala et al., 2019; Radaelli et al., 2019, Radaelli et al., 2018). However, light to moderate intensity (≤60% of maximum) should be used (Byrne et al., 2016; Fragala et al., 2019; Radaelli et al., 2019, Radaelli et al., 2018), as it provides greater muscle power production during the exercise (Strand et al., 2019). In addition, a lower number of repetitions per set and longer rest interval are indicated, as it provides less reduction in performance during the subsequent sets (Latella et al., 2019; Tufano et al., 2016). Likewise traditional resistance exercise, high-velocity exercise is important for frail individuals and should be used if possible (Fragala et al., 2019). In addition, for people with systemic arterial hypertension and cardiovascular disease, which are common in older people (Benjamin et al., 2019; Mills et al., 2016), muscle power training should be prioritized. This type of training is characterized by the use of light to moderate intensity loads, submaximal sets and repetitions and higher interval rest between sets (Byrne et al., 2016; Radaelli et al., 2019, Radaelli et al., 2018; Strand et al., 2019) which induces lower blood pressure responses. Differently, traditional resistance training is characterized by the use of moderate to high intensity, greater repetitions per set, lower rest set interval and maximum efforts (i.e. muscle concentric failure), which induces greater blood pressure responses (Gjøvaag et al., 2016; Haslam et al., 1988; Lamotte et al., 2010; MacDougall et al., 1985).
Recently, other models of muscle power training including the cluster design and resistance elastic-assisted or overspeed exercise have been recommended. In the cluster design, a traditional set (i.e. continuous repetitions) is organized with rest intervals between repetitions (Latella et al., 2019; Ramirez-Campillo et al., 2018; Tufano et al., 2017). For example, a continuous set of 8 repetitions can be divided into 8 (or less) blocks of 1 (or more) repetition with an interval of 30–45 s after each repetition (Latella et al., 2019; Ramirez-Campillo et al., 2018; Tufano et al., 2017). Cluster training has shown greater preservation of muscle power levels during exercise (Latella et al., 2019; Tufano et al., 2016) and also positive adaptations on functional capacity and quality of life in older individuals, which may be superior to traditional muscle power training (Ramirez-Campillo et al., 2018). In addition, as this training design can also provide a lower cardiovascular response during exercise (Iglesias-Soler et al., 2015; Ribeiro-Torres et al., 2020), it also appears as an option for the older people with cardiovascular risk factors or hypertensive response to exercise. When the resistance elastic-assisted or overspeed exercise format is performed, an elastic is positioned for implementing a greater velocity during the concentric phase of the movement (Tufano, 2019; Tufano et al., 2020; Vetrovsky et al., 2020). As an example, an individual who does a bodyweight squat or jump would position a resistance elastic band at a high point and hold it during the movement; in the eccentric/downward phase of the movement, the elastic stretches, and in the concentric/upward phase, the elastic is shortened, providing an increased velocity of the movement beyond the voluntary capacity, causing an overspeed (supramaximal execution) during the concentric phase. The use of overspeed exercise has recently been suggested for the older individuals, showing benefits in the neuromuscular parameters and lower perceived exertion in this population (Tufano, 2019; Tufano et al., 2020; Vetrovsky et al., 2020).
Because poor mobility and risk of falls are hallmarks of frailty, multicomponent training, including resistance training, gait and balance exercises should be applied (Cadore et al., 2019). Home-based multicomponent training, including traditional resistance or high-velocity exercise, is effective to induce neuromuscular and functional improvements in healthy and frail older people (Bohrer et al., 2019; Garcia et al., 2020). The complementary program should include exercises as walking with changes in pace and direction, stepping practice, stair climbing, stationary cycling, tandem foot standing, multidirectional weight lifts, heel-toe walking, line walking, standing on one leg, and weight transfers (from one leg to the other) (Cadore et al., 2019, Cadore et al., 2013).
It is important to consider the existing relationship between motivation, intensity and supervision influence the overall strength improvements in HBRT (Thiebaud et al., 2014). Also, attention should also be given to provide clear exercise instructions and control progression according to the individual's physical capacity. Telehealth can be used with the older population and promote physical exercise during the COVID-19 pandemic (Denay et al., 2020; Verduzco-Gutierrez et al., 2020). The use of technology can be useful to instruct, monitor and control HBRT through digital devices (Denay et al., 2020; Jay et al., 2014; Verduzco-Gutierrez et al., 2020; Yoshiko et al., 2018). Fig. 2, Fig. 3, Fig. 4 show examples of lower-limb exercises that are easy to reproduce at home and can be adapted according to the individual's current condition. The exercises selected involve muscle groups (e.g. quadriceps femoris) with higher age-related loss (Abe et al., 2014; Janssen et al., 2000; Lynch et al., 1999), which are associated to functional capacity in older individuals (Akima et al., 2020; Byrne et al., 2016; Misic et al., 2007; Suzuki et al., 2001; Wilhelm et al., 2014). Moreover, a sequence of progression of squat exercise is shown in Fig. 2A to E starting from the simplest way to more challenging ways to perform it. Finally, it is essential to consider patient compliance to both exercise and the proposed training prescription.
3. Conclusion
In summary, it is an urgent time for older people to practice both resistance/strength and power training at home to mitigate the harmful functional decline and to promote physical health in this population. Finally, the definitive end of the pandemic remains uncertain; therefore, strategies that help to avoid physical inactivity and promote physical health in older people are needed. In this scenario, HBRT should be encouraged as it is an alternative modality of exercise to promote and maintain physical health during this period.
Acknowledgments
Acknowledgments
The authors would like to thank CNPq (Conselho Nacional de Desenvolvimento Científico e Tecnológico) and CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior) for their financial support. The authors are also grateful to those involved in the exercise examples. All photos were taken with permission.
Author's contribution
All authors have made substantial contributions to conception, drafting and revising the manuscript critically for relevant intellectual content. All authors approved the final version and agreed to be accountable for all aspects of the manuscript.
Declaration of competing interest
The authors declare no conflict of interest.
Section Editor: Emanuele Marzetti
References
- Abe T., Thiebaud R.S., Loenneke J.P., Loftin M., Fukunaga T. Prevalence of site-specific thigh sarcopenia in Japanese men and women. Age (Omaha) 2014;36:417–426. doi: 10.1007/s11357-013-9539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akima H., Yoshiko A., Ogawa M., Maeda H., Tomita A., Ando R., Tanaka N.I. Quadriceps echo intensity can be an index of muscle size regardless of age in 65 or more years old. Exp. Gerontol. 2020;138:111015. doi: 10.1016/j.exger.2020.111015. [DOI] [PubMed] [Google Scholar]
- Andersen K.G., Rambaut A., Lipkin W.I., Holmes E.C., Garry R.F. The proximal origin of SARS-CoV-2. Nat. Med. 2020;26:450–452. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bamman M.M., Clarke M.S.F., Feeback D.L., Talmadge R.J., Stevens B.R., Lieberman S.A., Greenisen M.C. Impact of resistance exercise during bed rest on skeletal muscle sarcopenia and myosin isoform distribution. J. Appl. Physiol. 1998;84:157–163. doi: 10.1152/jappl.1998.84.1.157. [DOI] [PubMed] [Google Scholar]
- Benjamin E.J., Muntner P., Alonso A., Bittencourt M.S., Callaway C.W., Carson A.P., Chamberlain A.M., Chang A.R., Cheng S., Das S.R., Delling F.N., Djousse L., Elkind M.S.V., Ferguson J.F., Fornage M., Jordan L.C., Khan S.S., Kissela B.M., Knutson K.L., Kwan T.W., Lackland D.T., Lewis T.T., Lichtman J.H., Longenecker C.T., Loop M.S., Lutsey P.L., Martin S.S., Matsushita K., Moran A.E., Mussolino M.E., O’Flaherty M., Pandey A., Perak A.M., Rosamond W.D., Roth G.A., Sampson U.K.A., Satou G.M., Schroeder E.B., Shah S.H., Spartano N.L., Stokes A., Tirschwell D.L., Tsao C.W., Turakhia M.P., VanWagner L.B., Wilkins J.T., Wong S.S., Virani S.S. Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- Bohrer R.C.D., Pereira G., Beck J.K., Lodovico A., Rodacki A.L.F. Multicomponent training program with high-speed movement execution of ankle muscles reduces risk of falls in older adults. Rejuvenation Res. 2019;22:43–50. doi: 10.1089/rej.2018.2063. [DOI] [PubMed] [Google Scholar]
- Byrne C., Faure C., Keene D.J., Lamb S.E. Ageing, muscle power and physical function: a systematic review and implications for pragmatic training interventions. Sport. Med. 2016;46:1311–1332. doi: 10.1007/s40279-016-0489-x. [DOI] [PubMed] [Google Scholar]
- Cadore E.L., Rodríguez-Mañas L., Sinclair A., Izquierdo M. Effects of different exercise interventions on risk of falls, gait ability, and balance in physically frail older adults: a systematic review. Rejuvenation Res. 2013;16:105–114. doi: 10.1089/rej.2012.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadore E.L., Sáez de Asteasu M.L., Izquierdo M. Multicomponent exercise and the hallmarks of frailty: considerations on cognitive impairment and acute hospitalization. Exp. Gerontol. 2019;122:10–14. doi: 10.1016/j.exger.2019.04.007. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Centers for Disease Control and Prevention [WWW document] 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html URL.
- Chodzko-Zajko W.J., Proctor D.N., Fiatarone Singh M.A., Minson C.T., Nigg C.R., Salem G.J., Skinner J.S. Exercise and physical activity for older adults. Med. Sci. Sport. Exerc. 2009;41:1510–1530. doi: 10.1249/MSS.0b013e3181a0c95c. [DOI] [PubMed] [Google Scholar]
- Clegg A., Young J., Iliffe S., Rikkert M.O., Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–762. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham C., O’ Sullivan R., Caserotti P., Tully M.A. Consequences of physical inactivity in older adults: a systematic review of reviews and meta-analyses. Scand. J. Med. Sci. Sports. 2020;30:816–827. doi: 10.1111/sms.13616. [DOI] [PubMed] [Google Scholar]
- Denay K.L., Breslow R.G., Turner M.N., Nieman D.C., Roberts W.O., Best T.M. ACSM call to action statement: COVID-19 considerations for sports and physical activity. Curr. Sports Med. Rep. 2020;19:326–328. doi: 10.1249/JSR.0000000000000739. [DOI] [PubMed] [Google Scholar]
- Esain I., Gil S.M., Bidaurrazaga-Letona I., Rodriguez-Larrad A. Effects of 3 months of detraining on functional fitness and quality of life in older adults who regularly exercise. Aging Clin. Exp. Res. 2019;31:503–510. doi: 10.1007/s40520-018-0990-1. [DOI] [PubMed] [Google Scholar]
- Fragala M.S., Cadore E.L., Dorgo S., Izquierdo M., Kraemer W.J., Peterson M.D., Ryan E.D. Resistance training for older adults: position statement from the National Strength and Conditioning Association. J. Strength Cond. Res. 2019;33:2019–2052. doi: 10.1519/JSC.0000000000003230. [DOI] [PubMed] [Google Scholar]
- Fukumoto Y., Tateuchi H., Ikezoe T., Tsukagoshi R., Akiyama H., So K., Kuroda Y., Ichihashi N. Effects of high-velocity resistance training on muscle function, muscle properties, and physical performance in individuals with hip osteoarthritis: a randomized controlled trial. Clin. Rehabil. 2014;28:48–58. doi: 10.1177/0269215513492161. [DOI] [PubMed] [Google Scholar]
- Fukumoto Y., Tateuchi H., Tsukagoshi R., Okita Y., Akiyama H., So K., Kuroda Y., Ichihashi N. Effects of high- and low-velocity resistance training on gait kinematics and kinetics in individuals with hip osteoarthritis. Am. J. Phys. Med. Rehabil. 2017;96:417–423. doi: 10.1097/PHM.0000000000000640. [DOI] [PubMed] [Google Scholar]
- Garcia R.N.S. de A., Costa S.N., Garcia E.D.S. de A., Bento P.C.B. Does home-based exercise improve the physical function of prefrail older women? Rejuvenation Res. 2020;55 doi: 10.1089/rej.2019.2292. rej.2019.2292. [DOI] [PubMed] [Google Scholar]
- Gjøvaag T.F., Mirtaheri P., Simon K., Berdal G., Tuchel I., Westlie T., Bruusgaard K.A., Nilsson B.B., Hisdal J. Hemodynamic responses to resistance exercise in patients with coronary artery disease. Med. Sci. Sport. Exerc. 2016;48:581–588. doi: 10.1249/MSS.0000000000000811. [DOI] [PubMed] [Google Scholar]
- Haslam D., McCartney N., McKelvie R., MacDougall J. Direct measurements of arterial blood pressure during formal weightlifting in cardiac patients. J. Cardiopulm. Rehabil. Prev. 1988;8:213–225. [Google Scholar]
- Hill K.D., Hunter S.W., Batchelor F.A., Cavalheri V., Burton E. Individualized home-based exercise programs for older people to reduce falls and improve physical performance: a systematic review and meta-analysis. Maturitas. 2015;82:72–84. doi: 10.1016/j.maturitas.2015.04.005. [DOI] [PubMed] [Google Scholar]
- Iglesias-Soler E., Boullosa D.A., Carballeira E., Sánchez-Otero T., Mayo X., Castro-Gacio X., Dopico X. Effect of set configuration on hemodynamics and cardiac autonomic modulation after high-intensity squat exercise. Clin. Physiol. Funct. Imaging. 2015;35:250–257. doi: 10.1111/cpf.12158. [DOI] [PubMed] [Google Scholar]
- Izquierdo M., Häkkinen K., Ibáñez J., Kraemer W.J., Gorostiaga E.M. Effects of combined resistance and cardiovascular training on strength, power, muscle cross-sectional area, and endurance markers in middle-aged men. Eur. J. Appl. Physiol. 2005;94:70–75. doi: 10.1007/s00421-004-1280-5. [DOI] [PubMed] [Google Scholar]
- Janssen I., Heymsfield S.B., Wang Z., Ross R. Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr. J. Appl. Physiol. 2000;89:81–88. doi: 10.1152/jappl.2000.89.1.81. [DOI] [PubMed] [Google Scholar]
- Jay K., Schraefel m.c., Brandt M., Andersen L.L. Effect of video-based versus personalized instruction on errors during elastic tubing exercises for musculoskeletal pain: a randomized controlled trial. Biomed. Res. Int. 2014;2014:1–7. doi: 10.1155/2014/790937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J.H., Lim S., Choi S.H., Kim K.M., Yoon J.W., Kim K.W., Lim J.-Y., Park K.S., Jang H.C., Kritchevsky S. Sarcopenia: an independent predictor of mortality in community-dwelling older Korean men. Journals Gerontol. Ser. A. 2014;69:1244–1252. doi: 10.1093/gerona/glu050. [DOI] [PubMed] [Google Scholar]
- Kis O., Buch A., Stern N., Moran D.S. Minimally supervised home-based resistance training and muscle function in older adults: a meta-analysis. Arch. Gerontol. Geriatr. 2019;84:103909. doi: 10.1016/j.archger.2019.103909. [DOI] [PubMed] [Google Scholar]
- Kortebein P., Ferrando A., Lombeida J., Wolfe R., Evans W.J. Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA. 2007;297:1769. doi: 10.1001/jama.297.16.1772-b. [DOI] [PubMed] [Google Scholar]
- Kortebein P., Symons T.B., Ferrando A., Paddon-Jones D., Ronsen O., Protas E., Conger S., Lombeida J., Wolfe R., Evans W.J. Functional impact of 10 days of bed rest in healthy older adults. Journals Gerontol. Ser. A Biol. Sci. Med. Sci. 2008;63:1076–1081. doi: 10.1093/gerona/63.10.1076. [DOI] [PubMed] [Google Scholar]
- Lamotte M., Fleury F., Pirard M., Jamon A., Borne P. van de. Acute cardiovascular response to resistance training during cardiac rehabilitation: effect of repetition speed and rest periods. Eur. J. Cardiovasc. Prev. Rehabil. 2010;17:329–336. doi: 10.1097/HJR.0b013e328332efdd. [DOI] [PubMed] [Google Scholar]
- Landi F., Liperoti R., Russo A., Capoluongo E., Barillaro C., Pahor M., Bernabei R., Onder G. Disability, more than multimorbidity, was predictive of mortality among older persons aged 80 years and older. J. Clin. Epidemiol. 2010;63:752–759. doi: 10.1016/j.jclinepi.2009.09.007. [DOI] [PubMed] [Google Scholar]
- Latella C., Teo W.-P., Drinkwater E.J., Kendall K., Haff G.G. The acute neuromuscular responses to cluster set resistance training: a systematic review and meta-analysis. Sport. Med. 2019;49:1861–1877. doi: 10.1007/s40279-019-01172-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- León-Muñoz L.M., Martínez-Gómez D., Balboa-Castillo T., López-García E., Guallar-Castillón P., Rodríguez-Artalejo F. Continued sedentariness, change in sitting time, and mortality in older adults. Med. Sci. Sport. Exerc. 2013;45:1501–1507. doi: 10.1249/MSS.0b013e3182897e87. [DOI] [PubMed] [Google Scholar]
- Li R., Xia J., Zhang X., Gathirua-Mwangi W.G., Guo J., Li Y., Mckenzie S., Song Y. Associations of muscle mass and strength with all-cause mortality among us older adults. Med. Sci. Sport. Exerc. 2018;50:458–467. doi: 10.1249/MSS.0000000000001448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-Sánchez G.F., López-Bueno R., Gil-Salmerón A., Zauder R., Skalska M., Jastrzębska J., Jastrzębski Z., Schuch F.B., Grabovac I., Tully M.A., Smith L. Comparison of physical activity levels in Spanish adults with chronic conditions before and during COVID-19 quarantine. Eur. J. Pub. Health. 2020;30:484–491. doi: 10.1093/eurpub/ckaa159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch N.A., Metter E.J., Lindle R.S., Fozard J.L., Tobin J.D., Roy T.A., Fleg J.L., Hurley B.F. Muscle quality. I. Age-associated differences between arm and leg muscle groups. J. Appl. Physiol. 1999;86:188–194. doi: 10.1152/jappl.1999.86.1.188. [DOI] [PubMed] [Google Scholar]
- MacDougall J.D., Tuxen D., Sale D.G., Moroz J.R., Sutton J.R. Arterial blood pressure response to heavy resistance exercise. J. Appl. Physiol. 1985;58:785–790. doi: 10.1152/jappl.1985.58.3.785. [DOI] [PubMed] [Google Scholar]
- Mair J.L., De Vito G., Boreham C.A. Low volume, home-based weighted step exercise training can improve lower limb muscle power and functional ability in community-dwelling older women. J. Clin. Med. 2019;8:41. doi: 10.3390/jcm8010041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikesky A.E., Topp R., Wigglesworth J.K., Harsha D.M., Edwards J.E. Efficacy of a home-based training program for older adults using elastic tubing. Eur. J. Appl. Physiol. Occup. Physiol. 1994;69:316–320. doi: 10.1007/BF00392037. [DOI] [PubMed] [Google Scholar]
- Mills K.T., Bundy J.D., Kelly T.N., Reed J.E., Kearney P.M., Reynolds K., Chen J., He J. Global disparities of hypertension prevalence and control. Circulation. 2016;134:441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misic M.M., Rosengren K.S., Woods J.A., Evans E.M. Muscle quality, aerobic fitness and fat mass predict lower-extremity physical function in community-dwelling older adults. Gerontology. 2007;53:260–266. doi: 10.1159/000101826. [DOI] [PubMed] [Google Scholar]
- Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323:1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- Ong S.W.X., Tan Y.K., Chia P.Y., Lee T.H., Ng O.T., Wong M.S.Y., Marimuthu K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) from a symptomatic patient. JAMA. 2020;323:1610. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orange S.T., Marshall P., Madden L.A., Vince R.V. Effect of home-based resistance training performed with or without a high-speed component in adults with severe obesity. Transl. Sport. Med. 2020;3:34–45. doi: 10.1002/tsm2.115. [DOI] [Google Scholar]
- Paddon-Jones D., Sheffield-Moore M., Urban R.J., Sanford A.P., Aarsland A., Wolfe R.R., Ferrando A.A. Essential amino acid and carbohydrate supplementation ameliorates muscle protein loss in humans during 28 days bedrest. J. Clin. Endocrinol. Metab. 2004;89:4351–4358. doi: 10.1210/jc.2003-032159. [DOI] [PubMed] [Google Scholar]
- Pagano A.F., Brioche T., Arc-Chagnaud C., Demangel R., Chopard A., Py G. Short-term disuse promotes fatty acid infiltration into skeletal muscle. J. Cachexia. Sarcopenia Muscle. 2018;9:335–347. doi: 10.1002/jcsm.12259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radaelli R., Brusco C.M., Lopez P., Rech A., Machado C.L.F., Grazioli R., Müller D.C., Cadore E.L., Pinto R.S. Higher muscle power training volume is not determinant for the magnitude of neuromuscular improvements in elderly women. Exp. Gerontol. 2018;110:15–22. doi: 10.1016/j.exger.2018.04.015. [DOI] [PubMed] [Google Scholar]
- Radaelli R., Brusco C.M., Lopez P., Rech A., Machado C.L.F., Grazioli R., Müller D.C., Tufano J.J., Cadore E.L., Pinto R.S. Muscle quality and functionality in older women improve similarly with muscle power training using one or three sets. Exp. Gerontol. 2019;128:110745. doi: 10.1016/j.exger.2019.110745. [DOI] [PubMed] [Google Scholar]
- Ramírez-Campillo R., Castillo A., de la Fuente C.I., Campos-Jara C., Andrade D.C., Álvarez C., Martínez C., Castro-Sepúlveda M., Pereira A., Marques M.C., Izquierdo M. High-speed resistance training is more effective than low-speed resistance training to increase functional capacity and muscle performance in older women. Exp. Gerontol. 2014;58:51–57. doi: 10.1016/j.exger.2014.07.001. [DOI] [PubMed] [Google Scholar]
- Ramirez-Campillo R., Alvarez C., Garcìa-Hermoso A., Celis-Morales C., Ramirez-Velez R., Gentil P., Izquierdo M. High-speed resistance training in elderly women: effects of cluster training sets on functional performance and quality of life. Exp. Gerontol. 2018;110:216–222. doi: 10.1016/j.exger.2018.06.014. [DOI] [PubMed] [Google Scholar]
- Reidy P.T., McKenzie A.I., Mahmassani Z., Morrow V.R., Yonemura N.M., Hopkins P.N., Marcus R.L., Rondina M.T., Lin Y.K., Drummond M.J. Skeletal muscle ceramides and relationship with insulin sensitivity after 2 weeks of simulated sedentary behaviour and recovery in healthy older adults. J. Physiol. 2018;596:5217–5236. doi: 10.1113/JP276798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro-Torres O., de Sousa A.F.M., Iglesias-Soler E., Fontes-Villalba M., Zouhal H., Carré F., Foster C., Boullosa D. Lower cardiovascular stress during resistance training performed with inter-repetition rests in elderly coronary patients. Medicina (B. Aires) 2020;56:264. doi: 10.3390/medicina56060264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuch F., Bulzing R., Meyer J., Lopez-Sanchez G., Grabovac I., Willeit P., Vancampfort D., Caperchione C., Sadarangani K., Werneck A., Ward P., Tully M., Smith L. vol. 51. 2020. Moderate to Vigorous Physical Activity and Sedentary Behavior Change in Self-Isolating Adults during the COVID-19 Pandemic in Brazil: A Cross-Sectional Survey Exploring Correlates. medRxiv. 2020.07.15.20154559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strand K.L., Lucchi L., Copo T.G., Cherup N.P., Signorile J.F. Optimal loads for power in older men and women using plate-loaded resistance machines. Exp. Gerontol. 2019;124:110638. doi: 10.1016/j.exger.2019.110638. [DOI] [PubMed] [Google Scholar]
- Studenski S. Gait speed and survival in older adults. JAMA. 2011;305:50. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki T., Bean J.F., Fielding R.A. Muscle power of the ankle flexors predicts functional performance in community-dwelling older women. J. Am. Geriatr. Soc. 2001;49:1161–1167. doi: 10.1046/j.1532-5415.2001.49232.x. [DOI] [PubMed] [Google Scholar]
- Thiebaud R.S., Funk M.D., Abe T. Home-based resistance training for older adults: a systematic review. Geriatr Gerontol Int. 2014;14:750–757. doi: 10.1111/ggi.12326. [DOI] [PubMed] [Google Scholar]
- Tufano J.J. Assisted jumping: a possible method of incorporating high-velocity exercise in older populations. Med. Hypotheses. 2019;126:131–134. doi: 10.1016/j.mehy.2019.03.028. [DOI] [PubMed] [Google Scholar]
- Tufano J.J., Conlon J.A., Nimphius S., Brown L.E., Seitz L.B., Williamson B.D., Haff G.G. Maintenance of velocity and power with cluster sets during high-volume back squats. Int. J. Sports Physiol. Perform. 2016;11:885–892. doi: 10.1123/ijspp.2015-0602. [DOI] [PubMed] [Google Scholar]
- Tufano J.J., Brown L.E., Haff G.G. Theoretical and practical aspects of different cluster set structures. J. Strength Cond. Res. 2017;31:848–867. doi: 10.1519/JSC.0000000000001581. [DOI] [PubMed] [Google Scholar]
- Tufano J.J., Vetrovsky T., Stastny P., Steffl M., Malecek J., Omcirk D. Assisted jumping in healthy older adults: optimizing high-velocity training prescription. J. Strength Cond. Res. Publish Ah. 2020:1–6. doi: 10.1519/JSC.0000000000003661. [DOI] [PubMed] [Google Scholar]
- Verduzco-Gutierrez M., Bean A.C., Tenforde A.S., Tapia R.N., Silver J.K. How to conduct an outpatient telemedicine rehabilitation or prehabilitation visit. PM&R. 2020;12:714–720. doi: 10.1002/pmrj.12380. [DOI] [PubMed] [Google Scholar]
- Vetrovsky T., Omcirk D., Malecek J., Stastny P., Stef M., Tufano J.J. 2020. Overspeed Stimulus Provided by Assisted Jumping Encourages Rapid Increases in Strength and Power Performance of Older Adults. [DOI] [PubMed] [Google Scholar]
- Villareal D.T., Aguirre L., Gurney A.B., Waters D.L., Sinacore D.R., Colombo E., Armamento-Villareal R., Qualls C. Aerobic or resistance exercise, or both, in dieting obese older adults. N. Engl. J. Med. 2017;376:1943–1955. doi: 10.1056/NEJMoa1616338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilhelm E.N., Rech A., Minozzo F., Radaelli R., Botton C.E., Pinto R.S. Relationship between quadriceps femoris echo intensity, muscle power, and functional capacity of older men. Age (Omaha) 2014;36:9625. doi: 10.1007/s11357-014-9625-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization World Health Organization. WHO coronavirus disease (COVID-19) dashboard [WWW document] 2020. https://covid19.who.int/ URL.
- World Health Organization World Health Organization. COVID-19 strategy update [WWW document] 2020. https://www.who.int/publications/i/item/covid-19-strategy-update---14-april-2020 URL.
- World Health Organization Policy brief: the impact of COVID-19 on older persons [WWW document] 2020. https://www.paho.org/en/documents/policy-brief-impact-covid-19-older-persons URL.
- Yoshiko A., Tomita A., Ando R., Ogawa M., Kondo S., Saito A., Tanaka N.I., Koike T., Oshida Y., Akima H. Effects of 10-week walking and walking with home-based resistance training on muscle quality, muscle size, and physical functional tests in healthy older individuals. Eur. Rev. Aging Phys. Act. 2018;15:13. doi: 10.1186/s11556-018-0201-2. [DOI] [PMC free article] [PubMed] [Google Scholar]