Abstract
Background
A growing number of patients continue to receive total knee replacement (TKR) surgery. Nevertheless, such surgeries result in moderate to severe postoperative pain and difficulty in managing it. Musical interventions are regarded as a type of multimodal analgesia, achieving beneficial results in other clinical treatments. This study aims to evaluate the effect of musical interventions in improving short-term pain outcomes following TKR in order to determine a more reasonable and standard way of delivering musical intervention.
Methods
A systematic search was conducted to identify available and relevant randomized controlled trials (RCTs) regarding musical interventions compared against non-musical interventions in patients treated with TKR in Embase, MEDLINE, Cochrane Library, Web of Science, CNKI, and Wanfang Med Online up to 8 January 2020. The authors independently assessed study eligibility and risk of bias and collected the outcomes of interest to analyze. The statistical analysis was conducted using the Review Manager (RevMan) version 5.30 software.
Results
Eight RCTs comprised of 555 patients satisfied the inclusion criteria and were enrolled in the present study. The results showed no significant difference between the music and control groups in pain of the visual analog scale (VAS), during postoperative recovery room, back to the ward after surgery; anxiety degree of VAS; heart rate; respiratory rate; oxygen saturation; blood pressure, systolic blood pressure, and diastolic blood pressure. Nevertheless, significant differences were observed between the two groups in average increase in continuous passive motion (CPM) angles and LF/HF ratio (one kind index of heart rate variability).
Conclusions
Musical interventions fail to demonstrate an obvious effect in improving short-term pain outcomes following TKR. A reasonable standardization of musical interventions, including musical type, outcome measures used, outcomes measured, duration, timing and headphones or players, may improve pain outcomes with certain advantages and should be further explored after TKR.
Keywords: Total knee replacement, TKR, TKA, Knee surgery, Music interventions, Music therapy, Pain, Meta-analysis, Systematic-review
Introduction
Total knee replacement has achieved good therapeutic effects in easing pain and improving functional outcomes for patients with rheumatoid arthritis or knee osteoarthritis [1, 2]. Approximately 100, 000 TKR operations are performed each year in the UK [3]. The number of TKR surgeries has been estimated to reach over 3.45 million by 2030 and increase by more than 670% by 2030 in the USA [4, 5]. Nevertheless, one study demonstrated that patients treated with TKR have been suffering from disproportionate pain, with 30% having moderate pain and 60% having severe pain [6]. Due to inadequate pain management following TKR, the procedure can lead to adverse outcomes such as severe anxiety, delayed convalescence, trouble with rest and sleep, reduced patient satisfaction, prolonged hospital stay, and heavier burden on healthcare [7–10]. It is a key focus of research, therefore, to improve patient satisfaction, optimize treatment, and reduce post-operation pain of TKR.
Chronic pain after TKR is caused by multiple factors such as psychological, biological, mechanical, surgical, and other factors [11–14]. Conventional studies have mainly focused on aspects of mechanical and biological using pharmacological interventions and physiotherapy [15, 16]. However, adverse drug reactions are important factors needing consideration like vomiting, nausea, dysarteriotony, urinary retention, and respiratory depression [17]. Non-pharmaceutical interventions have been regarded as simple, valuable, and low-cost supplementary methods in managing pain [18]. In the past two decades, a growing level of awareness regarding the hidden effects of music and other non-pharmacological strategies to improve postoperative results was present for interventions during the preoperative, perioperative, or postoperative periods [19, 20].
Musical therapies are natural interventions embodying multiple aspects like physical, emotional, psychological, spiritual recovery, and social. The proposed interventions have little side effects and high performance-cost ratio strategies that are easy to use and apply [21]. Music can stimulate the brain’s α waves, triggers relaxation and decreases muscular tension. It also stimulates the limbic system, leading to the release of endorphins, a type of neurotransmitter that causes a sense of well-being in humans [22]. Moreover, it can efficiently slow down the transmission of pain signals through the act of listening, alleviating the sense of pain [23], and reducing the dosage of paregoric post-surgery [24]. Listening to music stimulates the parasympathetic nervous system, restraining the action of the sympathetic nervous system, and reaching a target efficacy in easing anxiety [25, 26].
In practical clinic applications, nevertheless, incompatible consequences for musical interventions were present during the perioperative period, where various studies demonstrated pain relief [27–30] while others reported no significant changes [31]. Meanwhile, a number of studies carried out musical interventions solely within the operating room [30], while others applied them in post-anesthesia care units [32].
To the best of our knowledge, previous systematic reviews regarding psychological interventions in improving outcomes following TKR included musical therapy, hypnosis, guided imagery, and other different types of psychological interventions [33]. Due to its high heterogeneity, attaining a firm conclusion about the effectiveness of musical interventions in those treated with TKR is difficult. Furthermore, another meta-analysis and systematic review reported the effect of musical therapy on pain following orthopedic surgery, where musical interventions were found to relieve pain [34]. The study included a series of surgical operations when assessing the utility of listening to music after TKR, including the position of the knee, hip, shoulder, spine, and others. In similar circumstances, this study discussed improving outcomes for patients after TKR or THR [35]. The results are unconvincing because of the distinct prognosis and indications of two different surgical procedures.
Until now, no meta-analysis and systematic reviews have reported the effectiveness of musical interventions in patients who just received TKR. Due to the high incidence of pain following TKR, it may be of particular benefit to manage pain via musical interventions during the perioperative period. Therefore, a meta-analysis and systematic review was conducted to evaluate the effect of musical interventions in improving short-term pain outcomes after total knee replacement in order to ascertain a more reasonable and standard way of delivering musical interventions.
Materials and methods
Search strategies
This study was conformed to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [36]. Comprehensive literature searches were conducted in Embase, MEDLINE, Cochrane Library, Web of Science, CNKI, and Wanfang Med Online databases for RCTs published from the earliest available records to 8 January 2020 using the following keywords and their combinations: total knee replacement, TKR, total knee arthroplasty, TKA, music, audio, music therapy, and music interventions. Both MeSH and Emtree headings were combined and were supplied with free text to enhance their sensitivity; however, they were also manually retrieved references from related research to ensure the inclusion of other studies. There were no language restrictions for searching.
Inclusion and exclusion criteria
Studies were selected in the present research if they matched the following PICOS (population, intervention, comparator, outcome, study design) criteria: (I) Population, patients had received TKR; (II) Intervention, patients received musical interventions (music medicine or music therapy) intra-operatively, pre-operatively, or postoperatively; (III) Comparator, patients received an active treatment or control treatment (e.g., placebo, standard care, or no treatment); (IV) Outcomes such as assessment of pain severity during perioperative period, degree of anxiety, range of motion of the knee, physiological data including oxygen saturation, blood pressure, heart rate, heart rate variability, and respiratory rate; (V) Study design, RCTs.
The following conditions were considered exclusion criteria: revision knee arthroplasty; articles involving bilateral TKR; non-randomized trials; review articles; quasi-randomized trials; and articles with insufficient outcome data. The data were submitted to a third author for any divarication.
Primary and secondary outcomes
This study only gathered statistical outcomes during the perioperative period. The primary outcomes included pain severity, while secondary outcomes included degree of anxiety, average increase in CPM angles, and physiological parameters including oxygen saturation, blood pressure, heart rate, LF/HF (heart rate variability) and respiratory rate.
Data extraction
Final variables extracted included year of intervention, first author, country of origin, intervention time (perioperative, pre-operative, intra-operative, post-operative, or their combinations), type of music selection, music tracks, methodological characteristics, intervention details, participant characteristics, and measured outcomes. Two researchers independently extracted the data mentioned above. Discrepancies were discussed and resolved by additional authors. The corresponding authors of the primary studies were contacted to ensure that the integrated information was available. If there were multiple comparisons, only the interest data and information reported were extracted from the original studies.
Quality assessment and risk of bias
Two authors independently evaluated the methodological quality according to Cochrane Handbook, version 5.1.0, for Systematic Reviews of Interventions (http://handbook.cochrane.org/). There were seven items to be included: (a) selection bias, random sequence generation; (b) selection bias, allocation concealment; (c) performance bias, blinding of the participants and personnel; (d) detection bias, blinding of outcome assessments; (e) reporting bias, selective reporting; (f) attrition bias, incomplete outcome data; (g) other biases. The entire methodological quality of each study in our review was measured as “yes” (low risk of bias), “unclear” (unclear risk of bias), or “no” (high risk of bias) and was used to obtain the risk of the bias graph and bias summary via Review Manager 5 (RevMan 5, version 5.30 Cochrane Collaboration, Oxford, UK). Any divided opinions were solved through team consensus.
Statistical analysis
Review Manager 5 (RevMan 5) software (version 5.30, Cochrane Collaboration, Oxford, UK) was adopted for the statistical analysis in the present meta-analysis, where P value < 0.05 was considered to be statistically significant. Dichotomous outcomes were shown by risk difference (RD) and 95% confidence intervals (CIs). Continuous outcomes were shown by mean differences (MDs) and 95% CI, which was used for evaluation based on the P value and I2 value by the standard χ2 test. When the I2 < 50% or χ2 test > 0.1, manifesting significant heterogeneity, the fixed-effects model was adopted in the meta-analysis. Otherwise, the random-effects model was used. Sensitivity analysis was performed, if possible, to ascertain the origins of any heterogeneity.
Results
Study selection and characteristics of the selected studies
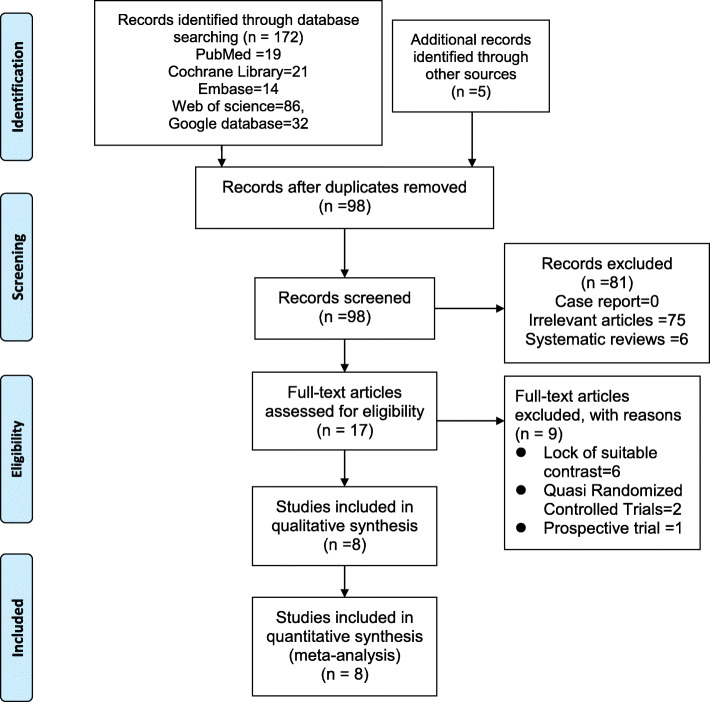
In total, 172 studies were initially identified via electronic databases. Among the excluded articles, participators of three studies [37, 38] had both TKR and THA, and data in a particular study [39] had published in their anterior article [40]. Therefore, feasible data was unable to be acquired [41, 42]. After assessing the titles or abstracts, and after screening the full-texts of related studies, 8 RCTs satisfied the inclusion criteria [40, 43–49]. The present literature search was expounded by the PRISMA flow diagram (Fig. 1). All included articles were published between 2008 and 2019, and 555 participants were included in the analysis. The sample sizes of each study ranged from 32 to 117. The general characteristics of RCTs included in the meta-analysis are shown in Table 1, and the study clinic intervention protocol of RCTs included in the meta-analysis are put forward in Table 2.
Fig. 1.
The PRISMA flow diagram detailing our literature search
Table 1.
General characteristics of RCTs included in the meta-analysis
| Studies | Year | Country | Type | Date of study | Sample size | Gender | Mean age | Timing of intervention | Primary results of statistics | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Music | Control | Music(F/M) | Control (F/M) | Music(M ± D) | Control(M ± D) | |||||||||
| Allred et al. [37] | 2010 | USA | RCT | In 2007 | 28 | 28 | 14 | 14 | 17 | 11 | 64.3 ±9.6 | 63.5 ± 9.6 | Post-op |
I. Pain: VAS and MPQ-SF II. Anxiety: VAS III. Physiologic data |
| Chen et al. [38] | 2015 | Taiwan | RCT | Not reported | 30 | 30 | 20 | 10 | 25 | 5 | 69.86 ± 7.56b | 69.86 ± 7.56b | Pre-op and post-op |
I. Pain: VAS II. Physiological data III. Total amount of opioids used |
| Finlay et al. [39] | 2016 | UK | RCT | Not reported | 72a | 17 | NS | NS | NS | NS | 68.07 ± 8.03b | 68.07 ± 8.03b | Pre-op and post-op |
I. Pain: VRS/NRS II. Salivary cortisol concentrations III. Mood states: TMD |
| Hooks et al. [40] | 2014 | USA | RCT | September 2013 to November 2013 | 30 | 30 | NS | NS | NS | NS | 66.84 ± 66b | 66.84 ± 66b | Post-op |
I. Pain: NRS II. Physiological data III. Amount of opioids IV. LOS |
| Hsu et al. [41] | 2015 | Taiwan | RCT | November 2013 to April 2014 | 49 | 42 | 34 | 15 | 33 | 9 | 73.9 ± 7.5 | 71.33 ± 8.45 | Post-op |
I. Anxiety: VAS II. Physiological Parameters III. CPM angles 4.ROM |
| Leonard et al. [42] | 2019 | USA | RCT | Not reported | 16 | 16 | 11 | 5 | 12 | 4 | 67.9(45–87)c | 67.6(53–80)c | Post-op | I. Pain: NRS |
| Simcock et al. [43] | 2008 | USA | RCT | Junr 2006 to March 2007 | 60 | 57 | 37 | 23 | 33 | 24 | 31.3 ± 5.8 | 29.6 ± 6.1 | Intra-op | I. Satisfaction scores II. Pain: VAS |
| You et al. [44] | 2019 | China | RCT | June 2018 to June 2018 | 25 | 25 | NS | NS | NS | NS | 65.2 ± 3.6b | 65.2 ± 3.6b | Post-op |
I. Physiological Parameters II. CPM angles III. ROM |
NS not stated, RCT randomized controlled trial, F/M female/male, M ± D means ± standard deviation, Post-op = postoperative, pre-op preoperative, Intra-op intraoperative, VAS visual analog scale, NRS numerical rating scale, MPQ-SF McGill pain questionnaire short-form, TMD total mood disturbance, LOS length of stay, CPM continuous passive motion, PPI present pain intensity, PRI pain rating intensity, ROM range of motion
a Containing four experimental groups
bThe age of music group and control group
cAge range
Table 2.
Clinic intervention protocol of RCTs included in the meta-analysis
| Studies | Intervention details | Intervention and comparison | Type of music | Follow-up assessments | Intervention treatment | Control treatment |
|---|---|---|---|---|---|---|
| Allred et al. | Music via headphones | Music vs. quiet rest period | Easy listening | D1:T1 = 20 min before first PT session; T2 = just before PT; T3 = immediately after PT, T4 = 20 min after PT; T5 = 6 hours after intervention. | Listening to CD of easy listening music on headphones 20 min before first ambulation and for 20 min rest period after ambulation. Music had no lyrics, 60–80 beats/min. | 20 min quiet rest period |
| Chen et al. | Music via broadcast speakers | Music vs. standard care | Soothing piano and violin |
I. 10 min while the investigator prepared the study equipment at rest. II. In the surgical room in the morning. III. In the postoperative recovery area after the surgery. IV. Sending back to the ward One hour later. |
Soothing piano and Chinese violin music played on a CD player through broadcast speakers. Played for 30 min in the preoperative ward, 30 min in the surgical room waiting area and 1 h in postoperative recovery. | Usual care |
| Finlay et al. | Music via headphones | Music vs. quiet bed rest | Varying degrees of harmonicity and rhythmicity | Pre-operative assessment at pre-admissions 2 weeks. All assessment measures were completed (D1–3) each day post-surgery. PCA usage was monitored pre-intervention in the immediate 24 h post-operatively (D0). | Four music-listening groups with four music types. Being visited daily and completing pre- and post-test at the same time each day, once per day for 3 days after surgery | Wearing noise canceling headphones with no input |
| Hooks et al. | Music via headphones | Music vs. quiet bed rest | Soft rock, jazz, Easy listening, R&B, Classical, Bluegrass, Country, Gospel, Pop, Nature sound | The patients were monitored in the morning between the times of 10:00 AM to 12:00 PM, early afternoon between 2:00 PM to 5:00 PM and evening between 7:30 PM to 9:30 PM on the first day after surgery. | The patients were asked not to alter the music player at any time. Before each session with the patients, I checked with the nurse and physical therapist to make sure the 30-min session would not interfere with the patient’s care plan. | wearing the ear buds for 30 min without music and the individual patient room door closed |
| Hsu et al. | Music via headphones | Music vs. standard care | Relaxing slow tempo, low tone, and soft melody | Receiving CPM rehabilitation twice daily (10 AM and 4 PM) on the first and second day following surgery | Listening to music from 10 min before receiving CPM until the end of the session (25 min in total) on the first and second day following surgery | Only to rest in bed 10 min before CPM. |
| Leonard et al | Music via music therapist | Music vs. standard care | Rock, Country, Traditional, Pop, Pop, Jazz, Bossa Nova | Baseline (1 min after flexion assessment), after each 2 min intervention period (two periods). | Music therapy during bicycling pedaling exercise postoperatively. Live music was played by a music therapist during PT supported pedaling exercise for 2 min, then pedaling alone with no music. Music included singing with paced guitar accompaniment and at a moderate/fast tempo. | Pedaling exercise with no music. |
| Simcock et al. | Music via headphones | Music vs. placebo | Patient’s choice what they like | Baseline, 3 h, 6 h, and 24 h after surgery procedure | Patient selection music during surgery by wearing headphones. | White noise control on headphones. |
| You et al. | Music via headphones | Music vs. quiet rest period | Soothing music | Preoperative , the first day and the second day after surgery during CPM | Starting CPM and listening to music until the end of the first 10 min during surgery by wearing headphones. | Usual care |
D postoperative day, PT physical therapy, CPM continuous passive motion
Quality assessment and risk of bias
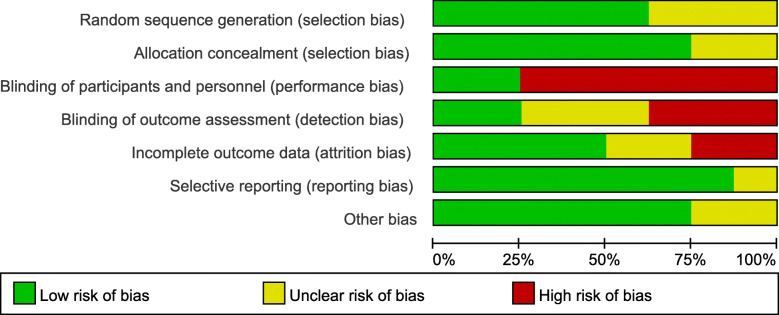
The present study was evaluated according to the Cochrane Handbook for Systematic Reviews of Interventions in terms of the methodological quality of all included RCTs. Five RCTs [43–45, 47, 48] mentioned the sequence generation (randomization scheme performed) fairly well, and six trials mentioned allocation concealment [40, 43–45, 47, 48]. In the remaining articles, this information was indistinct or absent [46, 49]. Blinding of personnel and participants was mentioned in two trials [46, 49], but was not performed in six trials [40, 43, 44, 46–48]. In regard to outcome assessors, two trials were blinded [44, 48], though three trials were unclear [40, 43, 49]. Blinding was not performed in the other three studies [45–47]. Furthermore, no other apparent bias was found in each included study. All included RCTs were considered to be low risk for attrition bias and furnished complete data. The detailed risks of bias for the eligible studies are shown in Figs. 2 and 3.
Fig. 2.
The risk of bias summary of the included studies. (+ represents yes; – represents no; ? represents not clear)
Fig. 3.
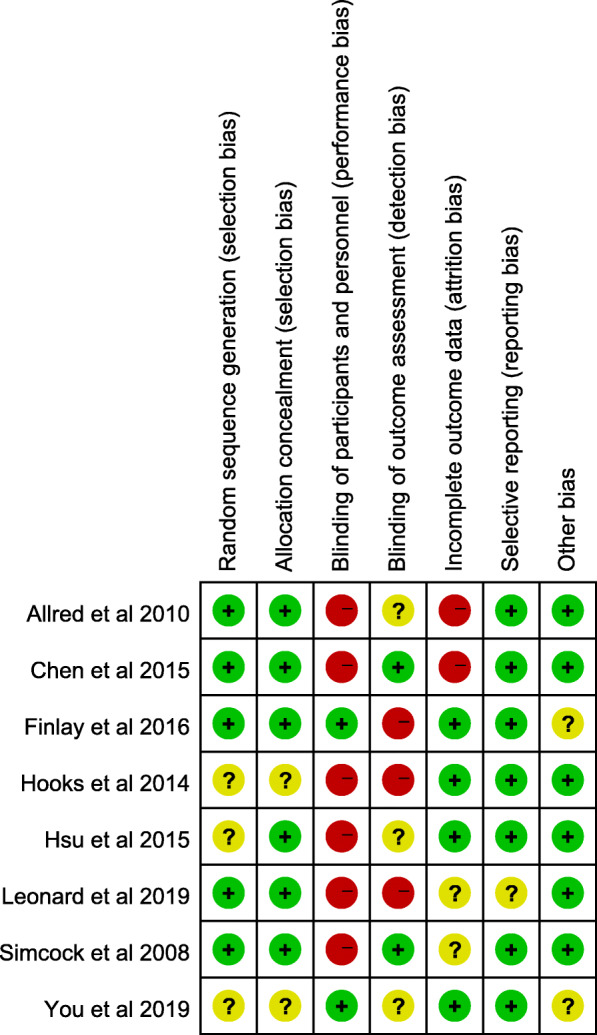
The risk of bias graph of the included studies.
Primary outcomes
Meta-analysis of pain severity
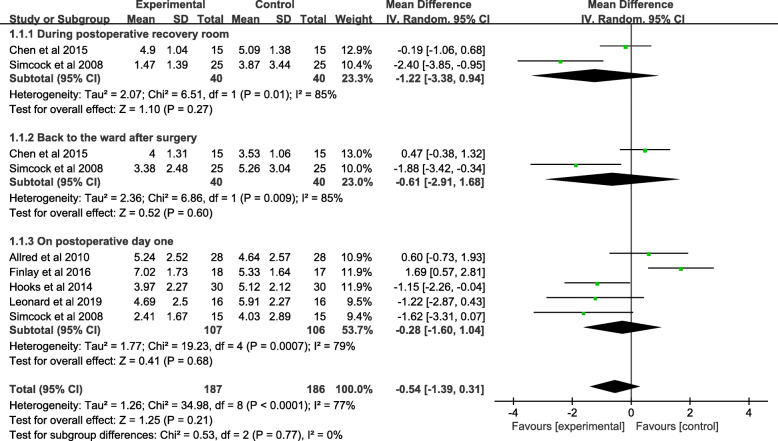
A total of 373 patients reported pain severity in 6 studies. Two studies assessing 80 knees involved pain of VAS in the postoperative recovery room. Moreover, no significant difference was evident between the music and control groups (MD = − 1.22; 95% CI; − 3.38 to 0.94; P = 0.27). Only 2 studies (80 patients) reported pain of VAS back to the ward after surgery, where no significant difference was found between the music and control groups (MD = − 0.61; 95% CI; − 2.91 to 1.68; P = 0.60). Additionally, 5 studies (213 patients) stated related pain in the VAS score on the postoperative day (POD) 1. The pooled data showed no significant difference between the two groups (MD = − 0.28; 95% CI; − 1.60 to 1.04; P = 0.68). In terms of the high heterogeneity of the three subgroups following, during postoperative recovery (χ2 = 6.51; df = 1; P = 0.01; I2 = 85%); back to the ward (χ2 = 6.86; df = 1; P = 0.009; I2 = 85%), POD1 (χ2 = 19.23; df = 2; P = 0.0007; I2 = 79%), a random-effects model was used (Fig. 4 and Table 3).
Fig. 4.
A forest plot diagram showing the pain severity
Table 3.
Clinical results of meta-analysis
| Clinical results | Studies | Number of participants | Incidence | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Music | Control | P | MD | 95% CI | Heterogeneity P (I2) | Model | ||
| Pain severity | |||||||||
| During PRR | 2 | 80 | 40 | 40 | 0.27 | − 1.22 | − 3.38 to 0.94 | 0.01(85%) | Random |
| Back to the ward after surgery | 2 | 80 | 40 | 40 | 0.60 | − 0.61 | − 2.91 to 1.68 | 0.009(85%) | Random |
| On POD 1 | 5 | 213 | 107 | 106 | 0.68 | − 0.28 | − 1.60 to 1.04 | 0.0007(79%) | Random |
| Anxiety degree | |||||||||
| Before PT on POD 1 | 2 | 147 | 77 | 70 | 0.87 | − 0.18 | − 2.35 to 1.99 | 0.004 (88%) | Random |
| After PT on POD 1 | 2 | 147 | 77 | 70 | 0.20 | − 1.49 | − 3.78 to 0.79 | 0.001(91%) | Random |
| Average increase in CPM angles | |||||||||
| On POD 1 | 2 | 141 | 74 | 67 | 0.0008 | 8.90 | 3.72 to 14.08 | 0.01(84%) | Random |
| On POD 2 | 2 | 141 | 74 | 67 | < 0.00001 | 4.24 | 2.15 to 6.32 | 0.13(56%) | Random |
| Heart rate | |||||||||
| Before PT on POD 1 | 2 | 147 | 77 | 70 | 0.54 | 1.23 | − 2.66 to 5.13 | 0.49(0%) | Fixed |
| After PT on POD 1 | 3 | 207 | 107 | 100 | 0.97 | 0.31 | − 3.53 to 3.65 | 0.31(16%) | Fixed |
| Blood pressure | |||||||||
| Systolic blood pressure | 2 | 90 | 45 | 45 | 0.52 | − 2.76 | − 11.10 to 5.58 | 0.46(0%) | Fixed |
| Diastolic blood pressure | 2 | 90 | 45 | 45 | 0.38 | − 1.80 | − 5.78 to 2.19 | 0.83(0%) | Random |
| Respiratory rate | 2 | 116 | 58 | 58 | 0.56 | 0.14 | − 0.33 to 0.61 | 0.93(0%) | Fixed |
| Oxygen saturation | 2 | 116 | 58 | 58 | 0.22 | − 0.51 | − 1.32 to 0.31 | 0.50(0%) | Fixed |
| LF/HF ratio | |||||||||
| Before PT on POD 1 | 2 | 141 | 74 | 67 | < 0.00001 | − 1.00 | − 1.23 to − 0.78 | 0.96(0%) | |
| After PT on POD 1 | 2 | 141 | 74 | 67 | < 0.00001 | − 1.40 | − 1.50 to − 1.30 | 0.98(0%) | Fixed |
| Before PT on POD 2 | 2 | 141 | 74 | 67 | < 0.00001 | − 0.90 | − 0.98 to − 0.82 | 0.95(0%) | Fixed |
| After PT on POD 2 | 2 | 141 | 74 | 67 | < 0.00001 | − 1.60 | − 1.71 to − 1.49 | 1.00(0%) | Fixed |
PRR postoperative recovery room, MD mean difference, CI confidence interval, FPM fast-paced music, POD postoperative day, CPM continuous passive motion, LF/HF one kind index of heart rate variability
Secondary outcomes
Meta-analysis of anxiety degree
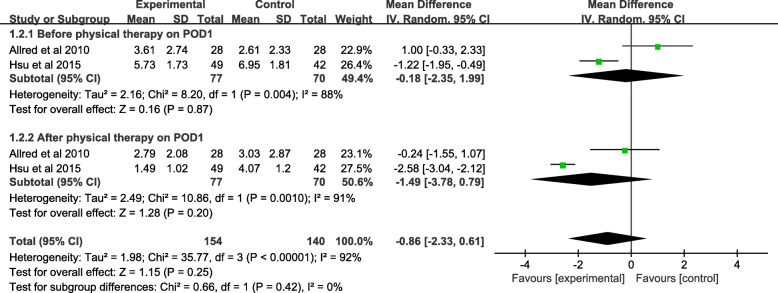
Only 2 studies (147 patients) reported the anxiety degree of VAS scores before PT on POD1. No significant difference was found between the two groups (MD = − 0.18; 95% CI; − 2.35 to 1.99; P = 0.87). The anxiety degree of VAS scores after PT on POD1 was reported in tow of the included studies, and a total of 147 patients were involved in the meta-analysis. The pooled data showed no significant difference between the music and control groups (MD = − 1.49; 95% CI; − 3.78 to 0.79; P = 0.20). Finding the high heterogeneity in before PT (χ2 = 8.20; df = 1; P = 0.004; I2 = 88%) and after PT (χ2 = 10.86; df = 1; P = 0.001; I2 = 91%), a random-effects model was adopted (Fig. 5 and Table 3).
Fig. 5.
A forest plot diagram showing the anxiety degree
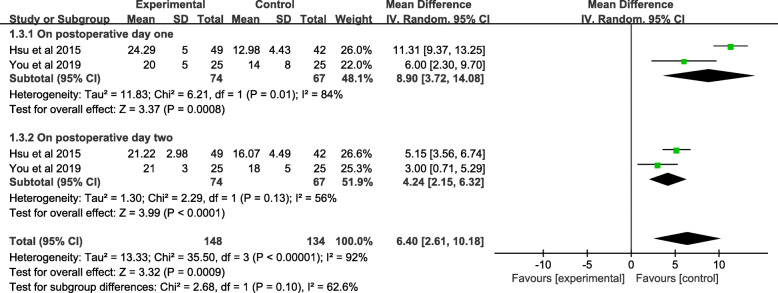
Meta-analysis of the average increase in CPM angles
A total of 141 patients reported an average increase in CPM angles in tow studies on POD1. There were significant differences between the music and control groups (MD = 8.90; 95% CI; 3.72 to 14.08; P = 0.0008). Two studies assessing 141 knees involved an average increase in CPM angles POD2, and a significant difference was observed between the included studies (MD = 4.24, 95% CI 215 to 6.32, P < 0.00001). In view of the high heterogeneity in the tow subgroups, POD1 (χ2 = 6.21; df = 1; P= 0.01; I2 = 84%) and POD2 (χ2 = 3.99; df = 1; P = 0.13; I2 = 56%), a random-effects model was utilized (Fig. 6 and Table 3).
Fig. 6.
A forest plot diagram showing the average increase in CPM angles
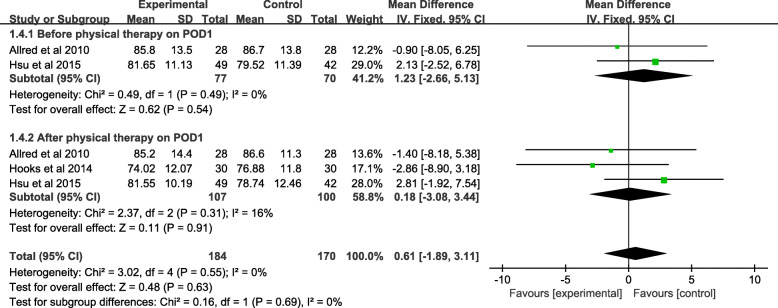
Meta-analysis of heart rate
Heart rate before PT on postoperative day (POD) 1 was reported in two studies, where a total of 147 patients was involved in the present research. The pooled data showed no significant difference between the two methods of interventions (MD = − 1.23, 95% CI − 2.66 to 5.13, P = 0.54). Three trails (207 patients) reported the heart rate after PT on postoperative day (POD) 1. The pooled data showed no significant difference (MD = − 0.06, 95% CI − 3.53 to 3.65, P = 0.97) between the two methods of interventions. Due to the important heterogeneity in heart rate before PT on POD 1 (χ2 = 0.49; df = 1; P = 0.49; I2 = 0%) and heart rate after PT on POD 1 (χ2 = 2.37; df = 2; P = 0.31; I2 = 16%), a fixed-effects model was applied (Fig. 7 and Table 3).
Fig. 7.
A forest plot diagram showing the heart rate
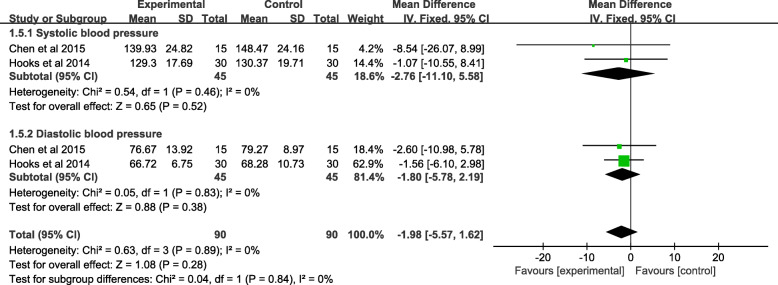
Meta-analysis of blood pressure
Two studies comprised of 90 patients reported systolic blood pressure, showing no statistical significance between the music and control groups (MD = − 2.76, 95% CI − 11.10 to 5.58, P = 0.52). The data of diastolic blood pressure was reported by two trails (147 patients). No significant difference was found between the two groups (MD = − 1.80, 95% CI − 5.78 to 2.19, P = 0.38). A random-effects model was used due to significant heterogeneity, systolic blood pressure (χ2 = 0.54; df = 1; P = 0.46; I2 = 0%), and diastolic blood pressure (χ2 = 0.05; df = 2; P = 1; I2 = 0%), which was found in the data of blood pressure (Fig. 8 and Table 3).
Fig. 8.
A forest plot diagram showing the blood pressure
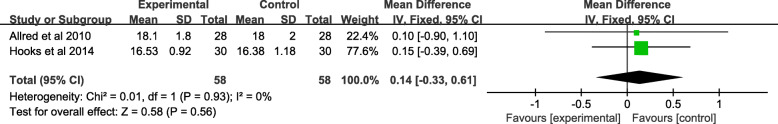
Meta-analysis of respiratory rate
Only 2 studies (116 patients) reported the respiratory rate after PT on POD1. No significant difference was found between the two groups (MD = 0.14; 95% CI − 0.33 to 0.61; P = 0.56). A fixed-effects model was used as significant heterogeneity was found in the data of respiratory rate (χ2 = 0.01; df = 1; P = 0.93; I2 = 0%) (Fig. 9 and Table 3).
Fig. 9.
A forest plot diagram showing the respiratory rate
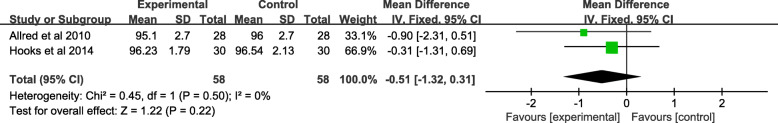
Meta-analysis of oxygen saturation
Oxygen saturation was reported in two studies, where a total of 116 knees were involved in the meta-analysis. There was no significant difference between the music and control groups (MD = − 0.51; 95% CI − 1.32 to 0.31; P = 0.22). In view of low heterogeneity (χ2 = 0.45; df = 1; P = 0.50; I2 = 0%), a fixed-effects model was applied (Fig 10 and Table 3).
Fig. 10.
A forest plot diagram showing the oxygen saturation
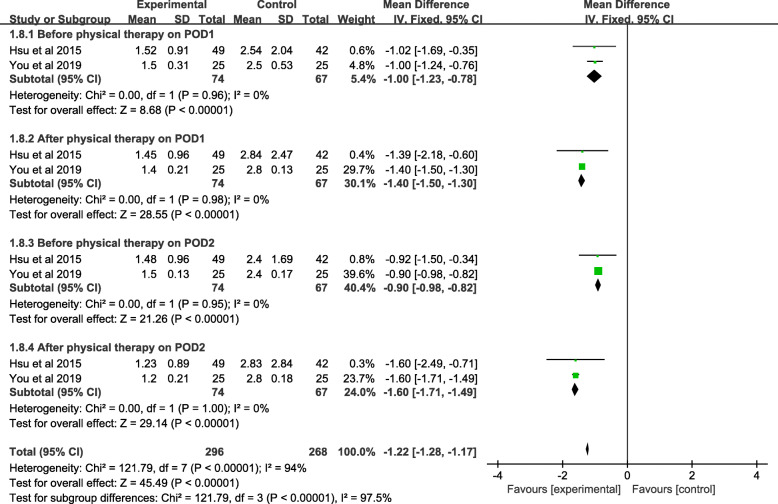
Meta-analysis of LF/HF ratio
Two studies (141 patients) reported the LF/HF ratio before PT on POD 1, and a significant difference was shown between the included studies (MD = − 1.00, 95% CI − 1.23 to − 0.78, P < 0.001). Two studies with 141 patients reported the LF/HF after PT on POD1, demonstrating a statistical significance between the music and control groups (MD = − 1.40, 95% CI − 1.50 to − 0.30, P < 0.001). Data pertaining to LF/HF before PT on POD 2 was reported by two trials of 141 patients. A significant difference was found between the two groups (MD = − 0.90, 95% CI − 0.98 to − 0.82, P < 0.001). Data regarding the LF/HF after PT on POD 2 was reported in two of the included studies, where a total of 141 patients were involved in the meta-analysis. The pooled data showed a significant difference between the music and control groups (MD = − 1.60; 95% CI − 1.71 to − 1.49; P < 0.001). Low heterogeneity of the four subgroups was observed, where POD1: before PT(χ2 = 0.00; df = 1; P = 0.98; I2 = 0%), POD1: after PT(χ2 = 0.00; df = 1; P = 0.98; I2 = 0%), POD2: after PT(χ2 = 0.00; df = 1; P = 0.95; I2 = 0%), POD2: before PT(χ2 = 0.00; df = 1; P = 1.00; I2 = 0%), a fixed-effects model was used (Fig. 11 and Table 3).
Fig. 11.
A forest plot diagram showing the LF/HF ratio
Subgroup analysis of others
A subgroup analyses were conducted to assess the effects of music via headphones as well as fast-paced music between the two groups (Table 4). The outcomes indicated that patients in the music groups had no significant difference in respiratory rate, heart rate, pain severity, oxygen saturation, and blood pressure compared to the control groups with or without music via headphones and fast-paced music.
Table 4.
Results subgroup analysis of others
| Clinical results | Studies | Number of participants | Incidence | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Music | Control | P | MD | 95% CI | Heterogeneity P (I2) | Model | ||
| Respiratory rate | |||||||||
| Headphones | 2 | 116 | 58 | 58 | 0.76 | 0.06 | − 0.35 to 0.48 | 0.80(0%) | Fixed |
| Non-headphones | 1 | 30 | 15 | 15 | 0.22 | 0.14 | − 0.88 to 1.17 | NS | NS |
| Including FPM | 1 | 60 | 30 | 30 | 0.58 | 0.15 | − 0.39 to 0.69 | NS | NS |
| Not including FPM | 2 | 86 | 43 | 43 | 0.98 | − 0.01 | − 0.52 to 0.51 | 0.62(0%) | Fixed |
| Heart rate | |||||||||
| Headphones | 3 | 207 | 107 | 100 | 0.74 | 0.34 | − 1.68 to 2.37 | 0.79(0%) | Fixed |
| Non-headphones | 1 | 30 | 15 | 15 | 1.00 | − 0.02 | − 6.36 to 6.33 | NS | NS |
| Including FPM | 1 | 60 | 30 | 30 | 0.35 | − 2.86 | − 8.90 to 3.18 | NS | NS |
| Not including FPM | 3 | 187 | 92 | 95 | 0.52 | 0.67 | − 1.37 to 2.71 | 0.95(0%) | Fixed |
| Pain severity | |||||||||
| Headphones | 4 | 182 | 91 | 91 | 0.28 | − 0.74 | − 2.09 to 0.60 | < 0.00001(83%) | Random |
| Non-headphones | 2 | 62 | 31 | 31 | 0.96 | − 0.02 | − 0.59 to 0.56 | 0.18(42%) | Fixed |
| Including FPM | 4 | 157 | 79 | 78 | 0.12 | − 1.05 | − 2.37 to 0.28 | < 0.00001(82%) | Random |
| Not including FPM | 2 | 86 | 43 | 43 | 0.42 | 0.23 | − 0.33 to 0.78 | 0.48(0%) | Fixed |
| Oxygen saturation | |||||||||
| Including FPM | 1 | 60 | 30 | 30 | 0.54 | − 0.31 | − 1.31 to 0.69 | NS | NS |
| Not including FPM | 1 | 56 | 28 | 28 | 0.21 | − 0.90 | − 0.90 to 0.51 | NS | NS |
| Blood pressure | |||||||||
| Headphones | 1 | 60 | 30 | 30 | 0.48 | − 1.47 | − 5.56 to 2.26 | NS | NS |
| Non-headphones | 1 | 30 | 15 | 15 | 0.34 | − 3.71 | 11.27 to 3.86 | NS | NS |
MD mean difference, CI confidence interval, FPM fast-paced music, NS not state
Discussion
Recently, an increasing number of patients received TKR [50]; however, pain management remains unsatisfactory following surgery [51]. Epidural analgesia, patient-controlled analgesia (PCA), and other medications serve as conventional methods in controlling pain [52–54], which may be associated with side effects. Multimodal analgesia implements at least two separate modalities of analgesia [55], and non-pharmacologic approaches are one aspect of multimodal therapy [56]. Music may be regarded to be very effective in terms of non-pharmacological pain management strategies [57]; however, its efficacy is known in relation to patients treated with TKR. This study is the first systematic review and meta-analysis evaluating the efficiency of musical interventions on patients treated with TKR, which attempted to determine a more reasonable and standard implementation of musical interventions.
Pain severity
In the present meta-analysis, no significant difference was observed for VAS scores during the postoperative recovery room, back to the ward after surgery, and postoperative day 1 between the music and control groups. The corresponding result is at variance with previous outcomes. First, researchers have previously shown the positive effects of musical interventions in different aspects of treatment such as cesarean section, intestinal, gynecologic, and nasal care [58–61]. Orthopedic surgeries are frequently associated with different outcomes in other types of surgery. Due to copious amounts of bone destruction and soft tissue injury, orthopedic surgery is generally associated with insufferable post-surgical pain [62]. Second, one study found that musical interventions performed immediately after TKR obviously alleviated pain over time [43] and mentioned that such interventions resulted in reduced opioid dosages and incidence of adverse reactions. The best efforts were made in collecting data long after having TKR as this may make a difference to a certain degree but failed due to the limited number of RCTs. Third, musical interventions could, in theory, shift one’s attention [63, 64], make people relax [65], and increase one’s sense of well-being [22]. We consider the main reason why it is different from us is the increased pain due to functional exercise in order to attain better knee flexion angles, which is a key result indicator of TKR surgery [66]. This study did not exclude the possibility of being influenced by subjective factors as the VAS score is a subjective scale. In addition, the heterogeneity of musical interventions should be noted as it also leads to divergence.
Anxiety degree
Previous studies have reported postoperative decreased anxiety with intraoperative music use in orthopedic surgery [67]. Due to limited studies, the present meta-analysis only collected data regarding before and after physical therapy with postoperative music use on POD 1. The results of the combined analysis showed that the music and control groups had no significant difference in anxiety degree after TKR. This outcome is similar to that of Allred and his colleagues [43], though another study found positive outcomes [40], which may be explained by the timing of the musical interventions. In Allred’s study, they rendered their music before and after initial physical therapy. However, Hsu and his colleagues provided music in three moments: before, during and after physical therapy. Therefore, we assume whether increasing the frequency of music may be associated with a positive efficiency. A similar assumption was supported in a previous systematic review [34], but varying surgical procedures may result in unreliable evidence. As correlation studies are limited in TKR surgery, this study failed to obtain an accurate answer. In addition, it is worth noting that a sense of stress can excite or stimulate a patient’s sympathetic nervous system, facilitating anxiety [68].
The average increase in CPM angles
The average increase in CPM angles was the secondary outcome assessed in this meta-analysis. Accordingly, significant differences were noted in the first and second days following surgery between the two groups. Many researchers posited that postoperative knee flexion angle is one of the main prognostic indexes of TKR surgery [69–72], and treatment of CPM was current clinical common practice [73, 74]. To this effect, CPM was reported to increase the voluntary knee joint ROM angle by an average of 4.3° in a short period [70]. As CPM treatment stretches surgical wounds, patients suffered from severe pain during this process. Therefore, certain patients were unsuccessful in complying with daily CPM rehabilitation. As the feeling of fear caused their muscles to tighten, the effectiveness of CPM was impacted. Patients who are relaxed during rehabilitation would improve the effectiveness of the treatment [75]. Music is known to be an art that promotes relaxation, which theoretically make sense. However, more RCTs are needed to confirm the degree of relaxation.
Physiologic parameters
Thus far, adopting musical treatment in clinical practice remains ambiguous. In order to generate further discussion, physiological parameters serve as an important component in accessing interventions. This study collected multiple physiologic parameters including oxygen saturation, blood pressure, heart rate, LF/HF ratio, and respiratory rate, though only LF/HF showed statistical significance. Similar results were reported by another study, where they found a lack of statistical difference among diastolic blood pressure, systolic blood pressure, and heart rate in participants in a rest group (n = 20) as well as a musical intervention group (n = 50) [76]. LF was used to describe the sympathetic activity and was of positive relevance with anxiety, however, HF indicated parasympathetic activity [77]. Furthermore, the LF/HF ratio evaluated the quantity of sympathetic balance to some extent [78], as well as a type of evaluation index concerning heart rate variability [79]. Low LF/HF ratio values indicate strong parasympathetic activity, whereas high values show strong sympathetic activity. Studies in other fields of surgery demonstrated similar ratios as this study [39, 78]. Other holistic studies reported that musical interventions decreased physiological stress parameters and perioperative stress hormones. These results were not supported by powerful evidence [61, 80]. Nevertheless, another article considered only sparse evidence regarding the effectiveness of music in blood pressure, heart rate, and respiratory rate during the preoperative, postoperative, or intraoperative periods [20]. Surgery may influence the cardiovascular system by stimulating the sympathetic nervous system like in elevated blood pressure, heart rate, and oxygen saturation [81]. Additional research in this regard could provide the relevant data in these fields.
Subgroup analysis of others
During data processing, various modes of musical interventions were identified, which led to high heterogeneity in the systematic review. Consequently, subgroup analyses were performed to assess the effects of music via headphones and fast-paced music between the two groups in order to determine a more reasonable and standard way of musical intervention. Due to the limited number of studies, this study failed to obtain a definite conclusion. More than one study demonstrated large discrepancies in the studied intervention type, outcome measures used, outcomes measured, duration, timing of intervention participants, and choices of music [82, 83]. Participants with headphones in the control group reported that headphones relieved anxiety by shielding background noise in the postoperative recovery room [84]. In addition, headphones promoted privacy, avoiding external noise, reducing noise-related mental fatigue, and more [22, 85, 86]. The music preferences of patients were a key factor when opting for musical intervention. This involved a patient-centered practice by allowing patients to choose the type of rhythm, which may achieve better results [87]. Interestingly, a previous study found that melodies were preferred to rhythms as melodies could alter the activity level of the adrenergic system [88]. Due to this study’s small sample size, the results should be interpreted with caution as additional related studies are undertaken.
Limitations
This research is the first meta-analysis and systematic review that appraises the effectiveness of musical interventions for TKR patients. However, various limitations were present in this study. Due to heterogeneity in the intensity, duration, type of music, and type of the interventions, few probabilities in acquiring abundant data exist in this study, which increased the difficulty in generalizing the findings for this population. In addition, high-quality studies may have been overlooked. Moreover, the conclusions may have been affected as some of the included studies had noticeable methodological shortcomings. Additionally, the studies in the present meta-analysis had unclear or high risk-of-bias ratings, which may cause the conclusion to lack persuasiveness. However, despite these limitations, a comprehensive review was given to estimate the effect of musical interventions in improving short-term pain outcomes following TKR, while determining meaningful methodological instructions for future studies.
Conclusion
Musical interventions fail to demonstrate an obvious effect in improving short-term pain outcomes following TKR. This review also repeatedly emphasizes the need for additional evidence in exploring the standardization of musical interventions (including musical type, outcome measures used, outcomes measured, duration, timing, and headphones or players) in improving pain outcomes after TKR, paving the way for future studies. The number and quality of the included studies were limited; consequently, studies with properly randomized techniques and larger sample sizes are anticipated.
Acknowledgements
We are very grateful for many helpful comments by an anonymous reviewer on an earlier version of this manuscript.
Patient and public involvement
No patient involved
Declarations
The first author is responsible for misconduct in the research and writing process. The original images, data (including computer database) records and samples involved in the paper have been saved, Shared and destroyed in accordance with relevant regulations and can accept verification.
Abbreviations
- CI
Confidence interval
- CPM
Continuous passive motion
- LOS
Length of stay
- LF/HF
Low-frequency/high-frequency ratio
- MD
Mean difference
- NS
Not stated
- Intra-op
Intraoperative
- POD
Postoperative day
- Pre-op
Preoperative
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PT
Physical therapy
- Post-op
Postoperative
- RCTs
Randomized controlled trials
- RD
Risk difference
- RevMan
Review Manager
- ROM
Range of motion
- TKA
Total knee arthroplasty
- TKR
Total knee replacement
- VAS
Visual analog scale
Authors’ contributions
RGY, YGZ, and EYF performed study design. FTL, ZLL, LQL, LLX, HYW, YTH, CLW, and WLW participated in literature search and data extraction. RGY, EYF, and YGZ were in charge of quality assessment and statistical analysis. RGY was responsible for manuscript review. All authors read and approved the final manuscript.
Funding
There is no funding for this article.
Availability of data and materials
We state that all data generated during the present study are included in this article.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rongguo Yu, Email: 876309664@qq.com.
Youguang Zhuo, Email: 871287899@qq.com.
Eryou Feng, Email: 19105008682@163.com.
Wulian Wang, Email: 859529732@163.com.
Wentao Lin, Email: taoTao123@qq.com.
Feitai Lin, Email: 15926183719@qq.com.
Zhanglai Li, Email: quinnliu95@163.com.
Liqiong Lin, Email: 859529732@qq.com.
Lili Xiao, Email: 987946771@qq.com.
Haiyang Wang, Email: 18254118970@163.com.
Yuting Huang, Email: 1333985916@qq.com.
Chunlin Wu, Email: chun@qq.com.
Yiyuan Zhang, Email: rongsteer@163.com.
References
- 1.Grant AE, Schwenk ES, Torjman MC, Hillesheim R, Chen AF. Postoperative analgesia in patients undergoing primary or revision knee arthroplasty with adductor canal block. Anesthesiology and pain medicine. 2017;7(3):e46695. doi: 10.5812/aapm.46695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tang Y, Tang X, Wei QH, Zhang H. Intrathecal morphine versus femoral nerve block for pain control after total knee arthroplasty: a meta-analysis. J Orthop Surg Res. 2017;12:8. doi: 10.1186/s13018-017-0510-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vasarhelyi EM, Petis SM. Use of national joint registries to evaluate a new knee arthroplasty design. J Arthroplast. 2020;35(2):413–416. doi: 10.1016/j.arth.2019.09.018. [DOI] [PubMed] [Google Scholar]
- 4.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. Jama. 2012;308(12):1227–1236. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi: 10.2106/00004623-200704000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Singelyn FJ, Deyaert M, Joris D, Pendeville E, Gouverneur JM. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg. 1998;87(1):88–92. doi: 10.1097/00000539-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Kehlet H, Dahl JB. Anaesthesia, surgery, and challenges in postoperative recovery. Lancet (London, England) 2003;362(9399):1921–1928. doi: 10.1016/S0140-6736(03)14966-5. [DOI] [PubMed] [Google Scholar]
- 8.Essving P, Axelsson K, Aberg E, Spannar H, Gupta A, Lundin A. Local infiltration analgesia versus intrathecal morphine for postoperative pain management after total knee arthroplasty: a randomized controlled trial. Anesth Analg. 2011;113(4):926–933. doi: 10.1213/ANE.0b013e3182288deb. [DOI] [PubMed] [Google Scholar]
- 9.Dihle A, Helseth S, Kongsgaard UE, Paul SM, Miaskowski C. Using the American Pain Society's patient outcome questionnaire to evaluate the quality of postoperative pain management in a sample of Norwegian patients. The journal of pain : official journal of the American Pain Society. 2006;7(4):272–280. doi: 10.1016/j.jpain.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Sinatra RS, Torres J, Bustos AM. Pain management after major orthopaedic surgery: current strategies and new concepts. The Journal of the American Academy of Orthopaedic Surgeons. 2002;10(2):117–129. doi: 10.5435/00124635-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Vissers MM, Bussmann JB, Verhaar JA, Busschbach JJ, Bierma-Zeinstra SM, Reijman M. Psychological factors affecting the outcome of total hip and knee arthroplasty: a systematic review. Semin Arthritis Rheum. 2012;41(4):576–588. doi: 10.1016/j.semarthrit.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 12.Pinto PR, McIntyre T, Ferrero R, Almeida A, Araujo-Soares V. Risk factors for moderate and severe persistent pain in patients undergoing total knee and hip arthroplasty: a prospective predictive study. PLoS One. 2013;8(9):e73917. doi: 10.1371/journal.pone.0073917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lindberg MF, Miaskowski C, RustoEn T, Rosseland LA, Cooper BA, Lerdal A. Factors that can predict pain with walking, 12 months after total knee arthroplasty. Acta Orthop. 2016;87(6):600–606. doi: 10.1080/17453674.2016.1237440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katz J, Seltzer Z. Transition from acute to chronic postsurgical pain: risk factors and protective factors. Expert Rev Neurother. 2009;9(5):723–744. doi: 10.1586/ern.09.20. [DOI] [PubMed] [Google Scholar]
- 15.Li B, Wen Y, Liu D, Tian L. The effect of knee position on blood loss and range of motion following total knee arthroplasty. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2012;20(3):594–599. doi: 10.1007/s00167-011-1628-4. [DOI] [PubMed] [Google Scholar]
- 16.Napier RJ, Bennett D, McConway J, Wilson R, Sykes AM, Doran E, O'Brien S, Beverland DE. The influence of immediate knee flexion on blood loss and other parameters following total knee replacement. The bone & joint journal. 2014;96-b(2):201–209. doi: 10.1302/0301-620X.96B2.32787. [DOI] [PubMed] [Google Scholar]
- 17.Moucha CS, Weiser MC, Levin EJ. Current Strategies in Anesthesia and Analgesia for Total Knee Arthroplasty. The Journal of the American Academy of Orthopaedic Surgeons. 2016;24(2):60–73. doi: 10.5435/JAAOS-D-14-00259. [DOI] [PubMed] [Google Scholar]
- 18.Hyman RB, Feldman HR, Harris RB, Levin RF, Malloy GB. The effects of relaxation training on clinical symptoms: a meta-analysis. Nurs Res. 1989;38(4):216–220. doi: 10.1097/00006199-198907000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Abraha I, Rimland JM, Trotta F, Pierini V, Cruz-Jentoft A, Soiza R, O'Mahony D, Cherubini A. Non-pharmacological interventions to prevent or treat delirium in older patients: clinical practice recommendations the SENATOR-ONTOP Series. J Nutr Health Aging. 2016;20(9):927–936. doi: 10.1007/s12603-016-0719-9. [DOI] [PubMed] [Google Scholar]
- 20.Nilsson U. The anxiety- and pain-reducing effects of music interventions: a systematic review. AORN J. 2008;87(4):780–807. doi: 10.1016/j.aorn.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 21.Cole LC, LoBiondo-Wood G. Music as an adjuvant therapy in control of pain and symptoms in hospitalized adults: a systematic review. Pain management nursing : official journal of the American Society of Pain Management Nurses. 2014;15(1):406–425. doi: 10.1016/j.pmn.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 22.McCaffrey R, Locsin RC. Music listening as a nursing intervention: a symphony of practice. Holist Nurs Pract. 2002;16(3):70–77. doi: 10.1097/00004650-200204000-00012. [DOI] [PubMed] [Google Scholar]
- 23.Nilsson U. The anxiety-and pain-reducing effects of music interventions: a systematic review. AORN J. 2008;87(4):780–807. doi: 10.1016/j.aorn.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 24.Tam WW, Wong EL, Twinn SF. Effect of music on procedure time and sedation during colonoscopy: a meta-analysis. World J Gastroenterol. 2008;14(34):5336–5343. doi: 10.3748/wjg.14.5336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jeong GS, Kim MH. Effect of music therapy on anxiety, blood pressure, heart rate and glucose levels of patients undergoing surgery during spinal anesthesia. Journal of Korean Academy of Fundamentals of Nursing. 2015;22(1):25–34. doi: 10.7739/jkafn.2015.22.1.25. [DOI] [Google Scholar]
- 26.Kuhlmann AY, Etnel JR, Roos-Hesselink JW, Jeekel J, Bogers AJ, Takkenberg JJ. Systematic review and meta-analysis of music interventions in hypertension treatment: a quest for answers. BMC Cardiovasc Disord. 2016;16:69. doi: 10.1186/s12872-016-0244-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Good M, Stanton-Hicks M, Grass JA, Cranston Anderson G, Choi C, Schoolmeesters LJ, Salman A. Relief of postoperative pain with jaw relaxation, music and their combination. Pain. 1999;81(1-2):163–172. doi: 10.1016/S0304-3959(99)00002-0. [DOI] [PubMed] [Google Scholar]
- 28.Heiser RM, Chiles K, Fudge M, Gray SE. The use of music during the immediate postoperative recovery period. AORN J. 1997;65(4):777–785. doi: 10.1016/S0001-2092(06)62999-2. [DOI] [PubMed] [Google Scholar]
- 29.Hekmat HM, Hertel JB. Pain attenuating effects of preferred versus non-preferred music interventions. Psychol Music. 1993;21(2):163–173. doi: 10.1177/030573569302100205. [DOI] [Google Scholar]
- 30.Koch ME, Kain ZN, Ayoub C, Rosenbaum SH. The sedative and analgesic sparing effect of music. Anesthesiology. 1998;89(2):300–306. doi: 10.1097/00000542-199808000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Ikonomidou E, Rehnstrom A, Naesh O. Effect of music on vital signs and postoperative pain. AORN J. 2004;80(2):269–274. doi: 10.1016/S0001-2092(06)60564-4. [DOI] [PubMed] [Google Scholar]
- 32.Shertzer KE, Keck JF. Music and the PACU environment. Journal of perianesthesia nursing : official journal of the American Society of PeriAnesthesia Nurses. 2001;16(2):90–102. doi: 10.1053/jpan.2001.22594. [DOI] [PubMed] [Google Scholar]
- 33.Whale K, Wylde V, Beswick A, Rathbone J, Vedhara K, Gooberman-Hill R. Effectiveness and reporting standards of psychological interventions for improving short-term and long-term pain outcomes after total knee replacement: a systematic review. BMJ Open. 2019;9(12):e029742. doi: 10.1136/bmjopen-2019-029742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lin CL, Hwang SL, Jiang P, Hsiung NH. Effect of Music Therapy on Pain After Orthopedic Surgery—A Systematic Review and Meta-Analysis. Pain Practice. 2019. [DOI] [PubMed]
- 35.Sibanda A, Carnes D, Visentin D, Cleary M. A systematic review of the use of music interventions to improve outcomes for patients undergoing hip or knee surgery. J Adv Nurs. 2019;75(3):502–516. doi: 10.1111/jan.13860. [DOI] [PubMed] [Google Scholar]
- 36.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cetinkaya F. Effect of Listening to Music on Postoperative Cognitive Function in Older Adults After Hip or Knee Surgery: A Randomized Controlled Trial. Journal of perianesthesia nursing : official journal of the American Society of PeriAnesthesia Nurses. 2019;34(5):919–928. doi: 10.1016/j.jopan.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 38.Antall GF, Kresevic D. The use of guided imagery to manage pain in an elderly orthopaedic population. Orthop Nurs. 2004;23(5):335–340. doi: 10.1097/00006416-200409000-00012. [DOI] [PubMed] [Google Scholar]
- 39.Hsu CC, Chen SR, Lee PH, Lin PC. The effect of music listening on pain, heart rate variability, and range of motion in older adults after total knee replacement. Clin Nurs Res. 2019;28(5):529–547. doi: 10.1177/1054773817749108. [DOI] [PubMed] [Google Scholar]
- 40.Hsu CC, Chen WM, Chen SR, Tseng YT, Lin PC. Effectiveness of music listening in patients with total knee replacement during CPM rehabilitation. Biological research for nursing. 2016;18(1):68–75. doi: 10.1177/1099800415572147. [DOI] [PubMed] [Google Scholar]
- 41.Kang JG, Lee JJ, Kim DM, Kim JA, Kim CS, Hahm TS, Lee BD. Blocking noise but not music lowers bispectral index scores during sedation in noisy operating rooms. J Clin Anesth. 2008;20(1):12–16. doi: 10.1016/j.jclinane.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 42.Keshmiri A, Wolf T, Wiech O, Benditz A, Grifka J, Springorum H. Einfluss der intraoperativen Schallprotektion auf postoperative Schmerzen. Schmerz. 2014;28(1):82–89. doi: 10.1007/s00482-013-1368-0. [DOI] [PubMed] [Google Scholar]
- 43.Allred KD, Byers JF, Sole ML. The effect of music on postoperative pain and anxiety. Pain management nursing : official journal of the American Society of Pain Management Nurses. 2010;11(1):15–25. doi: 10.1016/j.pmn.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 44.Chen HJ, Chen TY, Huang CY, Hsieh YM, Lai HL. Effects of music on psychophysiological responses and opioid dosage in patients undergoing total knee replacement surgery. Japan journal of nursing science : JJNS. 2015;12(4):309–319. doi: 10.1111/jjns.12070. [DOI] [PubMed] [Google Scholar]
- 45.Finlay KA, Wilson JA, Gaston P, Al-Dujaili EA, Power I. Post-operative pain management through audio-analgesia: Investigating musical constructs. Psychol Music. 2016;44(3):493–513. doi: 10.1177/0305735615577247. [DOI] [Google Scholar]
- 46.Hooks HE. Effects of music intervention on the patient’s perception of pain after knee replacement surgery. 2014. [Google Scholar]
- 47.Leonard H. Live music therapy during rehabilitation after total knee arthroplasty: a randomized controlled trial. J Music Ther. 2019;56(1):61–89. doi: 10.1093/jmt/thy022. [DOI] [PubMed] [Google Scholar]
- 48.Simcock XC, Yoon RS, Chalmers P, Geller JA, Kiernan HA, Macaulay W. Intraoperative music reduces perceived pain after total knee arthroplasty: a blinded, prospective, randomized, placebo-controlled clinical trial. The journal of knee surgery. 2008;21(4):275–278. doi: 10.1055/s-0030-1247831. [DOI] [PubMed] [Google Scholar]
- 49.Linna Y, Yuan L, Lingyun Z, Yan S: Effect of music therapy on CPM accepted in early stages after operation by patients with total knee arthroplasty, vol. 16; 2019.
- 50.Zeng C, Lane NE, Hunter D, Wei J, Choi H, McAlindon T, Li H, Lu N, Lei G, Zhang Y. Intra-articular corticosteroids and the risk of knee osteoarthritis progression: results from the Osteoarthritis Initiative. Osteoarthr Cartil. 2019;27(6):855–862. doi: 10.1016/j.joca.2019.01.007. [DOI] [PubMed] [Google Scholar]
- 51.Puolakka PA, Rorarius MG, Roviola M, Puolakka TJ, Nordhausen K, Lindgren L. Persistent pain following knee arthroplasty. Eur J Anaesthesiol. 2010;27(5):455–460. doi: 10.1097/EJA.0b013e328335b31c. [DOI] [PubMed] [Google Scholar]
- 52.Gomez-Cardero P, Rodriguez-Merchan EC. Postoperative analgesia in TKA: ropivacaine continuous intraarticular infusion. Clin Orthop Relat Res. 2010;468(5):1242–1247. doi: 10.1007/s11999-009-1202-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kazak Bengisun Z, Aysu Salviz E, Darcin K, Suer H, Ates Y. Intraarticular levobupivacaine or bupivacaine administration decreases pain scores and provides a better recovery after total knee arthroplasty. J Anesth. 2010;24(5):694–699. doi: 10.1007/s00540-010-0970-x. [DOI] [PubMed] [Google Scholar]
- 54.Safa B, Gollish J, Haslam L, McCartney CJ. Comparing the effects of single shot sciatic nerve block versus posterior capsule local anesthetic infiltration on analgesia and functional outcome after total knee arthroplasty: a prospective, randomized, double-blinded, controlled trial. J Arthroplast. 2014;29(6):1149–1153. doi: 10.1016/j.arth.2013.11.020. [DOI] [PubMed] [Google Scholar]
- 55.Elmallah RK, Cherian JJ, Pierce TP, Jauregui JJ, Harwin SF, Mont MA. New and common perioperative pain management techniques in total knee arthroplasty. The journal of knee surgery. 2016;29(2):169–178. doi: 10.1055/s-0035-1549027. [DOI] [PubMed] [Google Scholar]
- 56.Ekman EF, Koman LA. Acute pain following musculoskeletal injuries and orthopaedic surgery: mechanisms and management. Instr Course Lect. 2005;54:21–33. [PubMed] [Google Scholar]
- 57.Cepeda MS, Carr DB, Lau J, Alvarez H. WITHDRAWN: Music for pain relief. The Cochrane database of systematic reviews. 2013;10:Cd004843. doi: 10.1002/14651858.CD004843.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ebneshahidi A, Mohseni M. The effect of patient-selected music on early postoperative pain, anxiety, and hemodynamic profile in cesarean section surgery. Journal of alternative and complementary medicine (New York, NY) 2008;14(7):827–831. doi: 10.1089/acm.2007.0752. [DOI] [PubMed] [Google Scholar]
- 59.Good M, Anderson GC, Ahn S, Cong X, Stanton-Hicks M. Relaxation and music reduce pain following intestinal surgery. Res Nurs Health. 2005;28(3):240–251. doi: 10.1002/nur.20076. [DOI] [PubMed] [Google Scholar]
- 60.Hook L, Songwathana P, Petpichetchian W. Music therapy with female surgical patients: effect on anxiety and pain. Pacific Rim International Journal of Nursing Research. 2008;12(4):259–271. [Google Scholar]
- 61.Tse MM, Chan MF, Benzie IF. The effect of music therapy on postoperative pain, heart rate, systolic blood pressures and analgesic use following nasal surgery. Journal of pain & palliative care pharmacotherapy. 2005;19(3):21–29. doi: 10.1080/J354v19n03_05. [DOI] [PubMed] [Google Scholar]
- 62.Zhang XL, Cheng T, Zeng BF. Experts’ consensus on minimally invasive surgery for total joint arthroplasty. Orthop Surg. 2011;3(3):147–151. doi: 10.1111/j.1757-7861.2011.00134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Melzack R. Pain and the neuromatrix in the brain. J Dent Educ. 2001;65(12):1378–1382. doi: 10.1002/j.0022-0337.2001.65.12.tb03497.x. [DOI] [PubMed] [Google Scholar]
- 64.Melzack R, Wall PD. Pain mechanisms: a new theory. Science (New York, NY) 1965;150(3699):971–979. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- 65.Smith JC, Joyce CA. Mozart versus new age music: relaxation states, stress, and ABC relaxation theory. J Music Ther. 2004;41(3):215–224. doi: 10.1093/jmt/41.3.215. [DOI] [PubMed] [Google Scholar]
- 66.Argenson JN, Parratte S, Ashour A, Komistek RD, Scuderi GR. Patient-reported outcome correlates with knee function after a single-design mobile-bearing TKA. Clin Orthop Relat Res. 2008;466(11):2669–2676. doi: 10.1007/s11999-008-0418-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Eisenman A, Cohen B. Music therapy for patients undergoing regional anesthesia. AORN J. 1995;62(6):947–950. doi: 10.1016/S0001-2092(06)63563-1. [DOI] [PubMed] [Google Scholar]
- 68.Chanda ML, Levitin DJ. The neurochemistry of music. Trends Cogn Sci. 2013;17(4):179–193. doi: 10.1016/j.tics.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 69.Denis M, Moffet H, Caron F, Ouellet D, Paquet J, Nolet L. Effectiveness of continuous passive motion and conventional physical therapy after total knee arthroplasty: a randomized clinical trial. Phys Ther. 2006;86(2):174–185. doi: 10.1093/ptj/86.2.174. [DOI] [PubMed] [Google Scholar]
- 70.Glassner PJ, Slover JD, Bosco JA, 3rd, Zuckerman JD. Blood, bugs, and motion - what do we really know in regard to total joint arthroplasty? Bulletin of the NYU hospital for joint diseases. 2011;69(1):73–80. [PubMed] [Google Scholar]
- 71.Lenssen TA, van Steyn MJ, Crijns YH, Waltje EM, Roox GM, Geesink RJ, van den Brandt PA, De Bie RA. Effectiveness of prolonged use of continuous passive motion (CPM), as an adjunct to physiotherapy, after total knee arthroplasty. BMC Musculoskelet Disord. 2008;9:60. doi: 10.1186/1471-2474-9-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lucas B. Total hip and total knee replacement: postoperative nursing management. British journal of nursing (Mark Allen Publishing) 2008;17(22):1410–1414. doi: 10.12968/bjon.2008.17.22.31866. [DOI] [PubMed] [Google Scholar]
- 73.Brosseau L, Milne S, Wells G, Tugwell P, Robinson V, Casimiro L, Pelland L, Noel MJ, Davis J, Drouin H. Efficacy of continuous passive motion following total knee arthroplasty: a metaanalysis. J Rheumatol. 2004;31(11):2251–2264. [PubMed] [Google Scholar]
- 74.Harvey LA, Brosseau L, Herbert RD. Continuous passive motion following total knee arthroplasty in people with arthritis. The Cochrane database of systematic reviews. 2010;3:Cd004260. doi: 10.1002/14651858.CD004260.pub2. [DOI] [PubMed] [Google Scholar]
- 75.Wright WL. Management of mild-to-moderate osteoarthritis: effective intervention by the nurse practitioner. J Nurse Pract. 2008;4(1):25–34. doi: 10.1016/j.nurpra.2007.09.014. [DOI] [Google Scholar]
- 76.Sendelbach SE, Halm MA, Doran KA, Miller EH, Gaillard P. Effects of music therapy on physiological and psychological outcomes for patients undergoing cardiac surgery. J Cardiovasc Nurs. 2006;21(3):194–200. doi: 10.1097/00005082-200605000-00007. [DOI] [PubMed] [Google Scholar]
- 77.Tang S, Lo L, Yen M, Tsai W. The relationship between anxiety and heart rate variability in patients receiving cardiac catheterization. Journal of Evidence-Based Nursing. 2006;2:53–62. [Google Scholar]
- 78.Peng SM, Koo M, Yu ZR. Effects of music and essential oil inhalation on cardiac autonomic balance in healthy individuals. Journal of alternative and complementary medicine (New York, NY) 2009;15(1):53–57. doi: 10.1089/acm.2008.0243. [DOI] [PubMed] [Google Scholar]
- 79.Chen G, Kuo C, Lo H. Heart rate variablility. Journal of Emergency and Critical Care Medicine. 2000;11(2):47–58. [Google Scholar]
- 80.Nilsson U, Unosson M, Rawal N. Stress reduction and analgesia in patients exposed to calming music postoperatively: a randomized controlled trial. Eur J Anaesthesiol. 2005;22(2):96–102. doi: 10.1017/S0265021505000189. [DOI] [PubMed] [Google Scholar]
- 81.Pasero C, Paice JA, McCaffery M. Basic mechanisms underlying the causes and effects of pain. Pain: clinical manual. 1999:15–34.
- 82.Bradt J, Dileo C, Shim M. Music interventions for preoperative anxiety. The Cochrane database of systematic reviews. 2013;6:Cd006908. doi: 10.1002/14651858.CD006908.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yinger OS, Gooding LF. A systematic review of music-based interventions for procedural support. J Music Ther. 2015;52(1):1–77. doi: 10.1093/jmt/thv004. [DOI] [PubMed] [Google Scholar]
- 84.Lee OK, Chung YF, Chan MF, Chan WM. Music and its effect on the physiological responses and anxiety levels of patients receiving mechanical ventilation: a pilot study. J Clin Nurs. 2005;14(5):609–620. doi: 10.1111/j.1365-2702.2004.01103.x. [DOI] [PubMed] [Google Scholar]
- 85.Evans D. The effectiveness of music as an intervention for hospital patients: a systematic review. J Adv Nurs. 2002;37(1):8–18. doi: 10.1046/j.1365-2648.2002.02052.x. [DOI] [PubMed] [Google Scholar]
- 86.MacDonald RA, Mitchell LA, Dillon T, Serpell MG, Davies JB, Ashley EA. An empirical investigation of the anxiolytic and pain reducing effects of music. Psychol Music. 2003;31(2):187–203. doi: 10.1177/0305735603031002294. [DOI] [Google Scholar]
- 87.Daveson BA. Music therapy and childhood cancer: Goals, methods, patient choice and control during diagnosis, intensive treatment, transplant and palliative care. Music Ther Perspect. 2001;19(2):114–120. doi: 10.1093/mtp/19.2.114. [DOI] [Google Scholar]
- 88.Yamamoto T, Ohkuwa T, Itoh H, Kitoh M, Terasawa J, Tsuda T, Kitagawa S, Sato Y. Effects of pre-exercise listening to slow and fast rhythm music on supramaximal cycle performance and selected metabolic variables. Arch Physiol Biochem. 2003;111(3):211–214. doi: 10.1076/apab.111.3.211.23464. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
We state that all data generated during the present study are included in this article.