Abstract
Introduction
Medical students extend their preparatory learning on entering the clinical work environment, by joining their clinical team as peripheral participants and start to care for “real” patients. This learning is situated, experiential, varied, mainly unstructured, highly dependent on clinical opportunities (affordances), and students’ motivation to learn (learner agency). Students ideally contribute to workplace activities, which allow their practical skills, confidence and professional identity to evolve. This study sought to investigate senior students’ perspectives in their early stages of workplace learning, by using social learning theory as a framework. The focus is on team integration, practical skills performance, professional development and their evolving professional identity.
Methods
Between 2015 and 2018, we conducted five focus groups, with a total of 36 volunteers, out of a possible 200 (18% Stage 3 (Year 3)) medical students. Each focus group session was audio recorded and transcribed verbatim. Participants were de-identified, and framework analysis used the theoretical frameworks of communities of practice, and workplace affordances to gain insight into their work-place learning experience during the first two months of their clinical rotation.
Results
Thirty-six students out of 200 (18%) attended focus groups over a four-year period. The results are presented using the theoretical frameworks of community of practice and workplace affordances and presented as themes of: meaning, “learning as experience”, practice, “learning as doing” community, “learning as belonging”, and identity, “learning as becoming”.
Discussion
Participants reported many positive examples of workplace learning while dealing directly with patients. Students were also exposed to ethical dilemmas and unexpected risks in the workplace. These included lack of site orientation, unsupportive teams, lack of supervision, and students’ inability to initiate agency, all of which contributed to their workplace uncertainty. Performing manageable tasks for their team provided a role in their community of practice, strengthening their identity as evolving doctors. Exposure to both positive and negative role models allowed students to reflect on ethical issues, further extending their own professional identities.
Summary
Participants were quick to observe and report workplace dynamics as they were exposed to the positive and negative aspects of the hidden curriculum. This allowed them to reflect on patient safety, and ethical concerns promoting the development of their professional identity.
Keywords: third-year medicine, workplace learning, professional identity, role modelling, communities of practice
Background
In the senior years, medical students transition to the clinical learning environment, whereby they join their clinical team, and engage in experiential work-based learning.1 Here students learn “real medicine,” as they develop socially and professionally with others who share the profession. There has been a considerable body of evidence to suggest that this transition is challenging, stressful and a huge learning opportunity. It is in this environment that their professional identity further develops by exposure to “real” medical situations, where they witness ethical dilemmas,2 and the professional and/or unprofessional behaviours of other clinicians.
Theoretical Framework
This type of learning is known as workplace learning, situated learning,3 or situated cognition,4 and is an entry into what Lave and Wenger (1991) have described as a “community of practice”,3 Here, common interests are shared, members socialise and engage in collective learning in the context in which it is applied.
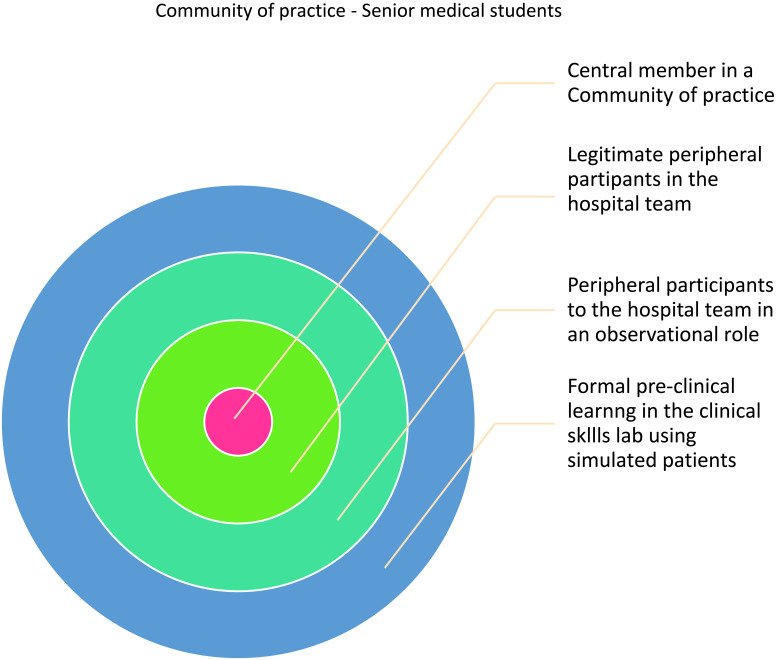
Students commence work as newcomers to their community of practice as “peripheral participants”;3 and by performing tasks appropriate for their level of training, students become more engaged within their workplace community. Their contribution allows them to become “legitimate peripheral participants” in the profession.3 This learning forms an upward trajectory over the duration of students’ training as they move towards a more central role, and become a full professional within their community of practice.3 This is illustrated in Figure 1.
Figure 1.
The evolution of senior medical students in this study in their journey to becoming central members to their community of practice.3
To allow learning to occur in the work environment, students require opportunities that enable learning. Billet describes these opportunities as workplace affordances,5 which are closely aligned with communities of practice. Such affordances include clinicians seeking tasks for students which are within their level of educational development6 and will not pose any risk to patient safety. Along with affordances, students require the motivation and determination to initiate their learning, which Billet refers to as learner agency.7 Learning is ideally performed utilising “deliberate practice”,8 whereby supervision is provided by an experienced clinician and feedback is given.9 Although this feedback is invaluable in influencing students’ learning outcomes, it can be overlooked or omitted due to supervisor time constraints.10
There is an array of educational frameworks to explain medical students learning patterns,11 and their experience of transferring their ‘preparatory’ or basic science knowledge to real-life, clinical application. In this study, we chose Lave and Wenger’s (1991) communities of practice theory3 to examine student integration into their team, and Billet’s (2009) workplace affordances12 to investigate situations that permit student workplace engagement. Both theoretical frameworks help to describe the early learning experiences of senior medical students, through their reports on early encounters in the clinical workplace.
Lave and Wenger (1991) focused on the interaction between new learners, experts, and the evolution of the professional identity of newcomers, by emphasising the social nature of learning. This was characterised by three key elements: Joint enterprise; refers to people who share a domain of interest, are engaged and working together toward a common goal. Mutual engagement; describes the interaction between individuals, including joint activities that leads to the creation of shared meaning on issues, or problems. Shared repertoire; refers to the common resources, including tools and conversations that members use to negotiate meaning, and facilitate learning within the group.
Wenger (1998) revised the above three key elements of a community of practice and indicated that four inter-connected elements are necessary to make a community of practice work:
1. Meaning: Members' experience expands to gain a shared meaning.
2. Practice: In medicine, practice consists of clinical care, educational practices, research, and a perspective that will sustain mutual engagement.
3. Community: Refers to learning as “belonging” to the community such as joint enterprise.
4. Identity: Members experience how learning changes who they are.13
Context
The participants in this study were Year 3, medical students enrolled in a 4-year graduate entry degree in the Sydney Medical Program (SMP), at the University of Sydney School of Medicine, Australia. During years 1 and 2, students attended their “parent” hospital at Central Clinical School (CCS) Royal Prince Alfred Hospital (RPAH), one day per week. Over those two years, their contact with “real” patients was limited to tutor supervised Clinical examination and Communication Skills tutorials on the wards, plus Procedural skills tutorials, utilising simulated models, or standardized patients, in the Clinical Skills Laboratory.
Despite this limited contact with “real” patients during the first year of medical school, it is compulsory for students to engage in reflective writing tasks. This is termed “Personal and Professional Development” (PPD),14 and provides the opportunity for them to explore ethical and professional components from their own clinical observations.
Immediately prior to commencing Year 3, all RPAH medical students attend an intensive orientation program consisting of an overview of Stage 3 (ie, Years 3 and 4) at a faculty orientation, and a two-day orientation at their home Clinical School (RPAH). The latter included the revision of core procedural skills; cardiopulmonary resuscitation; revision of cannulation; scrubbing/gowning/gloving; suturing; venepuncture; plus an introduction to writing in the patients’ case notes.
Students meet with their supervisors on a weekly basis to complete a protocol of scheduled tasks over the duration of their attachment. In addition, all Stage 3 students attend a weekly bedside teaching session, and additional structured teaching, including student-led presentations.
Methods
Developing of Study Instruments
Focus group questions were developed in collaboration with the co-author (C M), and two intern clinicians. The focus group questions asked about; students’ experience in working as part of the hospital team; encounters with clinician role models; observation of clinical professionalism; experience of interactions with patients; and opportunities to perform procedural skills under supervision. Focus group questions are in Appendix 1.
Sampling and Recruitment
Between 2015 and 2018, a convenience sample of Year 3 students at Central Clinical School Royal Prince Alfred Hospital (total n=200) was selected. All students were invited by e-mail to participate in focus groups regarding their first two 8-week rotations in the clinical work environment.
Data Collection and Analysis
After obtaining signed consent, five focus groups were conducted by the first author (SMcK). (Two in 2015 and one in subsequent years). Participants’ confidentiality was protected by the use of pseudonyms to conceal their identity.
Focus Groups
Focus groups were audio recorded, transcribed verbatim and thematically analysed15 by SMcK and AB, using framework analysis to code the date set within the conceptual frameworks of community of practice,13 workplace affordances.12
Ethical Considerations
Ethics approval was obtained from The University of Sydney Human Research Ethics Committee. Approval number 2024/182.
Results
Thirty-six students out of 200 (18%) attended focus groups over a four-year period. The results are presented using the theoretic frameworks of community of practice13 and Billet’s workplace affordances.12
The themes are summarised in Tables 1 and 2; Themes of: Meaning “learning as experience,” Practice “learning as doing,” Community “learning as belonging”, and Identity “learning as becoming” (Table 1). The themes of “workplace affordances”, (referring to situations that allow student learning), are presented in Table 2, under “clinical affordances,” “student agency” and “risks”.7
Table 1.
Participants’ Responses Relating to Wenger’s Summarised Conceptual Framework for a Social Theory of Learning “Communities of Practice”
| Theme 1: Responses relating to Meaning: “Learning as experience” | |
| Sample of Student Comments | |
|
The beginning of the workplace learning experience. Overall participants were enthusiastic to be in the clinical work environment. Examining patients and doing the work of “the doctor” not only provided a valuable learning experience; such autonomy further extended their professional identity. |
“I like being able to examine and take a history from people without six watching opposite me, I have been waiting for it for years.” “I felt that it is ‘proper medicine’ for the first time in years.” |
| Some participants saw third year as a new beginning: This “re-learning” is involved in the transition from pre-clinical learning to the workplace, and is a sharp contrast to the structured pre-clinical preparatory experience of the controlled simulated setting of the Clinical Skills Laboratory. | “It is like being in first year again” – “it is so different to being on the wards every day for a week and “a little unpleasant for me as it was just so different.” “Yeah me too, I felt like a fish out of water, felt useless just for my first week then it improved.” |
|
Inter-disciplinary observation Participants observed and reported the value of observing other health professionals at work; they expressed surprise in witnessing, that our members of the team provide “extended care,” through discharge planning, and witnessing an exchange of knowledge shared through mutual collaboration. |
“There is, “Extended care” ….not just being concerned about fixing the patient up and sending them home.” The other members of the team, the social workers, or the Occupational therapist (OT) …. so that when you send them home you know that they are in the best possible condition. They are extremely concerned about the patients’ home situation. |
| Theme 2: Responses relating to Practice: “Learning as doing” | |
| Sample of student comments | |
| Participants felt they were of great value to the team by writing in the case notes it was not only a good learning experience, as students performed small tasks for their team they moved from the role of “novice observer” and “peripheral participant” to that of legitimate participant to their team as seen in Figure 1. | Writing in the notes was the best learning experience for me because you learn what the team needs to do every day - although it was a daunting experience at the time. “I have a lot to do with written notes,” “I wrote in the patients notes, having to listen at the same time.” “I found that I was running walking and writing, it was fine because the intern would always help me.” |
| The introduction of electronic medical record (EMR2) allowed students to type patient document prior to a senior clinician signing off. | “EMR2 is much more comfortable – they let me do the typing.” |
| “One of the positive things is that you can see a patient when they come in and build a relationship until they leave.” | |
| Theme 3: Responses relating to Community: “Learning as belonging” | |
| Supporting student learning | Sample of student comments |
|
Clear directives Clear established frameworks of direction, which included guidelines, expectations and responsibilities, were provided to students during induction to specialised units. |
“With emergency we had an introduction session first.” “We were given guidelines and work responsibilities.” |
|
Active support Participants learned skills were extended by workplace clinicians who facilitated workplace learning by offering their support. |
“Once the second intern started, it really helped me out. They said, I will teach you how to take bloods and then supervise you.” “The more staff the higher level of support.” “Since the change- over, there are just oodles of people.” |
| Theme 4: Responses relating to Identity: “Learning as becoming” | |
| Role models - identity formation | Sample of student comments |
| Respondents witnessed positive clinician- patient interactions, which exhibited examples of positive role modelling in clinical empathy. This observation indicates that clinical decisions were made in a humane manner and rather than their previous experience in a simulated setting, empathy was conveyed in a real life situation, therefore, providing the students with a deep learning experience as direct witnesses to positive role modelling. Dealing effectively with a combative patient in a professional calm manner- is example of unconditional professionalism and positive role modelling. |
“I have had many situations whereby I have seen fantastic clinician skills” “A clinician spoke to a family about minimal intervention about end of life; The patient was suffering from aspiration pneumonia and the clinician was very clear with the family regarding what he thought was the most humane thing to do.” There was a combative patient who said, ‘I do not think much of doctors’ and the doctor just sat and diffused the situation by sitting and listening- he just let the person run out of steam. -It may have taken ten minutes. |
| Although new to the clinical area, participants exhibited astuteness in identifying unprofessional behaviours. This is surely and extension of their own professional development and an extension of their pre-clinical training, as in the clinical setting they are witnessing the reality of previously learned behavioural skills. | “I saw a doctors and a resident talking at the end of the bed about the patients” cancer- Eventually the patient interrupted – “I thought you said; Cancer!” Then the consult said, “we were going through the differentials and mentioned ‘cancer’.” |
Table 2.
Participants responses relating to Billet’s Workplace Affordances in Participants’ Experiences in Situated Learning: Clinical Affordances
| Sample of Student Comments | |
|---|---|
|
Facilitated learning The intern facilitated learning by seeking practical skills for the student to perform. |
Funnily enough, I got to do a lot, as the new intern gave me the cannulation as he was not good at it. He was from a different medical school – he did not want to try. |
|
Contrasting levels of support In contrast, curricular familiarity was no guarantee of pedagogic support. |
Both of my interns had been ex Sydney University students, the first one was amazing and excellent, the best teacher that I have had, the second one just doing his own thing. If you wanted to get him to help you would have needed to twist his arm. |
|
Hidden risks in the workplace Developing a sense of patient safety, workplace safety and professionalism instilled in the pre-clinical student years. However, without a clear description of workplace expectations, new third year students were subjected an ethical dilemma between risking their own safety, or the patients’ safety. It Is difficult for students to respond to supervisor behaviour that falls short of standards. |
“There was an expectation that I would, ‘just have a crack at it’, (cannulation) it did not help me with learning. It just stressed me out.” ‘I went with one of the other students’, the supervisor said; “just go do a cannula.” “I remember going to patient once and they were in recovery -they were psychotic - grabbed by arm and the team was laughing at me -the patient had scabies”. |
|
Mean teams Participants were in a vulnerable situation by their medical team whose challenging behaviour excluded students from fully integrating into their team. Furthermore, it was hard for students to be agentic in rectifying the situation, as they were dependent upon these clinicians for their end of rotation reports. Workplace affordances Participant comments highlight the intractable obstacles of workplace learning. Workplace affordances made it impossible to for students to engage with the hospital team or to have any form of supervision. The agentic student may have compensated by considering alternative ways of learning in the workplace, such as taking a patient history or engaging with the inter professional team. |
“I was doing 10–12 hour days for the first few weeks and I was expected to be there - told point blank.” “I was expected to be there the whole time – then they would take a two-hour coffee break.” “We were told you do not leave until everyone else goes then you are dismissed.” “Working for long hours, and being excluded from coffee breaks.” “Change over ‘A tricky time to start.’ We had two teams going through as we were in the middle of the changeover.” “They were super super, busy the best thing that they could have done was to say we are really busy and we will put you on a new team.” |
|
Student agency Participants report optimising their learning experience, by electing to engage in their work place to enhance their own learning. They had an understanding of passive learning and the limited value of non- active engagement in the workplace. |
“My name is X and I am here to learn”-it made them take notice of me ….I got to scrub in and they were explaining aspects of the operation to me. “Standing in the corner in an operating theatre has limited value.” |
Discussion
This study sought to investigate senior students’ perspective on their early experiences in workplace learning using the theoretical frameworks of communities of practice and workplace affordances. Interestingly, students did not explicitly discuss issues such as personal stress, and “the steep learning curve,” strong reoccurring themes in similar studies.16 Their reports focused on positive and negative clinician role models, their interaction with the patients and their teaching ability, as they further formulated their own professional identity. They were quick to identify ethical dilemmas, although as students they were powerless to take the initiative to modify such behaviours.
Theme of Meaning: “Learning as experience”
Participants reported many positive examples of enthusiasm in participating in workplace learning and being in a situation that enhanced their professional identities. This included performing the role of the doctor, by independently examining and taking patient histories. One reported witnessing optimum patient care by observing the activities of the inter-professional team. This learning experience highlights the value of exposure to inter-professional teamwork, to gain an understanding of the role of others in the healthcare team,12 and suggests the need for this to be added to future curricular implementation.
Theme of Practice: “Learning as doing”
Although at first daunting, participants found workplace learning to be the best learning experience, as they “learn by doing” in everyday work activities. Evidence suggests that actively engaging in learning promotes a greater depth of understanding, and increased knowledge retention, as well as further development of their own professional identity. For example, entrustment in performing the professional procedure of cannulation (See Table 1). This concept of entrustment was first proposed by Ten Cate (2005) as Entrustable Professional Activities, (EPAs),17 to describe trainees who have the knowledge and skills to perform a particular procedure under varied levels of supervision. This enabled some study participants to assist their team and become legitimate peripheral participants in their community of practice.
Theme of Community: “Learning as belonging”
Participants who had a formal introduction to the learning environment reported better team integration, and a stronger framework for learning. In contrast, the absence of an induction left some respondents feeling unwanted, unwelcome, and ignored.
These findings are consistent with the studies of Boor (2008), in that the clinical learning climate “affects undergraduate medical students’ behaviour, satisfaction and success.”18 In accordance with Gordon (2000), “learners need adequate briefing prior to moving into new clinical experiences”,19 and “leaders should make the rotation supportive for their students”.20,21
Theme of Identity: “Learning as becoming ”
By exposure to positive and negative role models, participants were able to identify with the kind of doctor that they would like to become. Positive role models demonstrated good teaching skills, knowledge, communication skills and patient-centred skills. These findings are in line with Ginsberg et al (2011) who found that through witnessing professional decision making, students developed their own professional judgment. Clearly, this is “not something that can be learned in a lecture”.2 This highlights that professional ethos has been developing not just in clerkship, but also in the preparatory years. Cruess et al assert that:
A physician’s identity is a representation of self, achieved in stages over time during which the characteristics, values, and norms of the medical profession are internalized, resulting in an individual thinking, acting, and feeling like a physician.22
Affordances
Some clinicians offered workplace affordances, such as permitting participants to write in the case notes and perform rudimentary procedural skills – thus allowing them to experience a sense of autonomy from day one. This contribution to the team allowed students to be legitimate participants in their community of practice. Furthermore, students enhanced their learning experience by contributing to workplace goals through participatory practice.12 One participant reported optimising their contributions to their team by being agentic and announcing that “they were there to learn”; therefore, rather than remain a passive observer, they facilitated active workplace involvement (Table 2). Whilst a challenge, agentic, participatory practice of this kind was reported as effective,12 and obviously, this self-regulated learning can help prepare students for lifelong learning.23
The Risks of Learning in a Community of Practice
Lave and Wenger (1991) acknowledged that there are risks involved in learning in a “community of practice,”3 as the learning community can be weak, or learning situations can be tied to organisational or power inequalities,24 Furthermore, the clinical work environment is “real,” highly complex, and varied, as students interact with an array of clinicians and patients to engage in first-hand clinical experiences. This informal learning is a sharp contrast to students’ structured preparatory experience of learning basic procedural and communication skills in the controlled simulated setting of the Clinical Skills Laboratory.25 Outside of the formal university curriculum students learn in an informal manner, Haffery and Franks describe this as the “hidden curriculum”,26 which has positive and negative aspects. Participants were unprepared for the negative aspects of the “hidden curriculum.” For example, workplace risks involving “mean teams”, and clinician lapses in professionalism that could compromise both patients and students’ physical and emotional safety. Others reported being coerced into performing tasks beyond their level of experience, and conflicting with learned values from their formal curriculum26. That is, performing invasive procedures on patients without adequate supervision. This has been described by Vygotsky (1990) as, beyond the “Zone of proximal commencing development.”27 There were also unexpected hidden risks for students in the workplace. For example, the teams' amusement regarding a student’s exposure to an infectious patient. Also, team constraints, resulting in missed opportunities to perform skills – such as the team completing procedural skills work to avoid the student slowing them down; and students lack of agency to initiate situations that would enhance their learning.7
What This Study Adds
This study highlights the curricular need for future learners to have an understanding of their novice role, the roles of others, and “hidden risks” when entering the workplace as peripheral participants. Having an awareness of workplace affordances and being agentic, promoted engagement into their team as students moved towards becoming legitimate participants.
Orientation sessions, worksite inductions, and an awareness of their responsibility to the team assist students in attaining their workplace goals. Dealing with “real patients”, ethical dilemmas, positive and negative role models all contribute to the development of professional identity, and of achieving their ultimate goal of becoming a competent doctor.
Limitations
The sample size was smaller than intended as students had other, unforeseen obligations to remain in the clinical area. Consequently, this study may not reflect the opinions of all Year 3 students.
Conclusion
By using the theoretical frameworks communities of practice and workplace affordances, we found that participants reported enthusiasm and a sense of autonomy in workplace learning. They became legitimate peripheral participants to their community of practice by performing appropriate tasks for their team. Workplace affordances can facilitate, or hinder students’ progress. Those who were agentic were able to express their motivation and effectively join the team, thus avoiding the risk of being ignored. Students were exposed to unexpected hidden risks in the workplace, such as lack of site induction; unsupportive teams; ethical dilemmas; risks to patient safety; and lack of adequate supervision. Role models, both positive and negative, allowed participants to reflect on the further development of their own professional identity, and explore the traits of the kind of doctor they aspire to be.
Future Research
Further research in this important area of learning is needed. Future similar studies in other medical schools (both nationally and internationally), utilising larger sample sizes should further clarify many of the issues raised by our study.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Dornan T, Bundy C. What can experience add to early medical education? Consensus survey. BMJ. 2004;329:834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ginsburg S, Lingard L. ‘Is that normal?’Pre‐clerkship students’ approaches to professional dilemmas. Med Educ. 2011;45(4):362–371. doi: 10.1111/j.1365-2923.2010.03903.x [DOI] [PubMed] [Google Scholar]
- 3.Lave J. Situated Learning: Legitimate Peripheral Participation. Cambridge [England]: Cambridge University Press; 1991. [Google Scholar]
- 4.Wilson AL. The promise of situated cognition. New Dir Adult Cont Educ. 1993;1993(57):71–79. doi: 10.1002/ace.36719935709 [DOI] [Google Scholar]
- 5.Billett S. Toward a workplace pedagogy: guidance, participation, and engagement. Adult Educ Q. 2002;53(1):27–43. doi: 10.1177/074171302237202 [DOI] [Google Scholar]
- 6.Valsiner J. Culture and Human Development: An Introduction. London UK: Sage; 2000. [Google Scholar]
- 7.Billett S Developing agentic professionals through practice-based pedagogies. Final Report for Australian Learning and Teaching Council (ALTC) Associate Fellowship. Strawberry Hills, NSW: ALTC; 2009. [Google Scholar]
- 8.Ericsson K. Deliberate practice and acquisition of expert performance: a general overview. Acad Emerg Med. 2008;15:988–994. doi: 10.1111/j.1553-2712.2008.00227.x [DOI] [PubMed] [Google Scholar]
- 9.Kilminster S, Jolly B. Effective supervision in clinical practice settings: a literature review. Med Educ. 2000;34(10):827–840. doi: 10.1046/j.1365-2923.2000.00758.x [DOI] [PubMed] [Google Scholar]
- 10.Irby DM. Teaching and learning in ambulatory care settings: a thematic review of the literature. Acad Med. 1995;70(10):898–931. doi: 10.1097/00001888-199510000-00014 [DOI] [PubMed] [Google Scholar]
- 11.Taylor DCM, Hamdy H. Adult learning theories: implications for learning and teaching in medical education: AMEE Guide No. 83. Med Teach. 2013;35(11):e1561–e1572. doi: 10.3109/0142159X.2013.828153 [DOI] [PubMed] [Google Scholar]
- 12.Billett S. Workplace participatory practices: conceptualising workplaces as learning environments. J Workplace Learn. 2004;16(6):312–324. doi: 10.1108/13665620410550295 [DOI] [Google Scholar]
- 13.Wenger E. Communities of Practice: Learning, Meaning, and Identity. Cambridge, U.K.: Cambridge University Press; 1998. [Google Scholar]
- 14.Gordon J. Assessing students’ personal and professional development using portfolios and interviews. Med Educ. 2003;37(4):335–340. doi: 10.1046/j.1365-2923.2003.01475.x [DOI] [PubMed] [Google Scholar]
- 15.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 16.Atherley A, Dolmans D, Hu W, Hegazi I, Alexander S, Teunissen PW. Beyond the struggles: a scoping review on the transition to undergraduate clinical training. Med Educ. 2019;53(6):559–570. doi: 10.1111/medu.13883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ten Cate O. Entrustability of professional activities and competency-based training. Med Educ. 2005;39(12):1176–1177. doi: 10.1111/j.1365-2929.2005.02341.x [DOI] [PubMed] [Google Scholar]
- 18.Boor K, Scheele F, Van Der Vleuten CPM, Teunissen PW, Den Breejen EME, Scherpbier AJJA. How undergraduate clinical learning climates differ: a multi-method case study. Med Educ. 2008;42(10):1029–1036. doi: 10.1111/j.1365-2923.2008.03149.x [DOI] [PubMed] [Google Scholar]
- 19.Gordon J, Hazlett C, Ten Cate O, et al. Strategic planning in medical education: enhancing the learning environment for students in clinical settings. Med Educ. 2000;34(10):841–850. doi: 10.1046/j.1365-2923.2000.00759.x [DOI] [PubMed] [Google Scholar]
- 20.Dornan T, Tan N, Boshuizen H, et al. How and what do medical students learn in clerkships? Experience based learning (ExBL). Adv Health Sci Educ. 2014;19(5):721–749. doi: 10.1007/s10459-014-9501-0 [DOI] [PubMed] [Google Scholar]
- 21.Jenny B, C TS, Geoff M. Novice students navigating the clinical environment in an early medical clerkship. Med Educ. 2017;51(10):1014–1024. doi: 10.1111/medu.13357 [DOI] [PubMed] [Google Scholar]
- 22.Cruess RL, Cruess SR, Boudreau JD, Snell L, Steinert Y. Reframing medical education to support professional identity formation. Acad Med. 2014;89(11):1446–1451. doi: 10.1097/ACM.0000000000000427 [DOI] [PubMed] [Google Scholar]
- 23.White CB. Smoothing out transitions: how pedagogy influences medical students’ achievement of self-regulated learning goals. Adv Health Sci Educ. 2007;12(3):279–297. doi: 10.1007/s10459-006-9000-z [DOI] [PubMed] [Google Scholar]
- 24.Collin K, Sintonen T, Paloniemi S, Auvinen T. Work, power and learning in a risk filled occupation. Manag Learn. 2011;42(3):301–318. doi: 10.1177/1350507610394411 [DOI] [Google Scholar]
- 25.Remmen R, Scherpbier A, Van Der Vleuten C, et al. Effectiveness of basic clinical skills training programmes: a cross‐sectional comparison of four medical schools. Med Educ. 2001;35(2):121–128. doi: 10.1046/j.1365-2923.2001.00835.x [DOI] [PubMed] [Google Scholar]
- 26.Hafferty FW, Hafler JP. The hidden curriculum, structural disconnects, and the socialization of new professionals In: Hafler JP, editor. Extraordinary Learning in the Workplace. Dordrecht: Springer Netherlands; 2011:17–35. [Google Scholar]
- 27.Vygotsky LS. Mind in Society: The Development of Higher Psychological Processes. Harvard University Press; 1980. [Google Scholar]