Abstract
Purpose
To determine the quality of life (QOL) in glaucoma patients undergoing combined cataract and minimally invasive glaucoma surgery from various perspectives ranging from personal, social, occupational life, and economic status.
Settings and Design
A cross-sectional study design at King Fahd Hospital of the University, Khobar, Saudi Arabia.
Methods
Patients undergoing phacoemulsification in conjunction with various forms of minimally invasive glaucoma surgery (MIGS) for each patient, including either Kahook Dual Blade (KDB) goniotomy, iStent, iStent inject and gonioscopy-assisted transluminal trabeculotomy (GATT), were included in the study between 2018 and 2019. Data were collected through a self-administered questionnaire based on the Visual Function Questionnaire (VFQ-25) for the 25-item National Eye Institute.
Results
The study included 93 eyes of 78 patients (40 males and 38 females) who had MIGS: 50 KDB, 13 iStent, 23 iStent inject, and 7 GATT. An overall reduction in the number of anti-glaucoma medications (p<0.001) was statistically significant. In the study, 36.6% of patients had a better social life, but 85.2% had no change in occupational life. Eventually, 86% were satisfied with the operation’s outcome, and 79% confirmed that the overall quality of life improved after the procedure.
Conclusion
Evaluating QOL is a crucial component of glaucoma treatment. More research is needed on MIGS and their relationship to QOL. In the future, MIGS may provide the desired outcomes in controlling glaucoma and improving the QOL.
Keywords: glaucoma, quality of life, goniotomy, Kahook Dual Blade, iStent, iStent inject, gonio-assisted transluminal trabeculotomy, combined phacoemulsification, MIGS, Schlemm’s canal
Introduction
Quality of life (QOL) reflects the general well-being of the individual and their ability to pursue life to its fullest.1 A better understanding of patients’ quality of life, ranging from psychological, social, and economic status, can improve patient–physician interaction, enhance adherence to treatment and optimize long-term prognosis. However, visually impaired people are at higher risk for accidents, social withdrawal, and depression.2 Glaucoma and cataract have a significant impact on the QOL of patients, mainly due to reduced visual function and corresponding activity restriction.3 Intraocular pressure (IOP) has proved to be the only modifiable risk factor for the progression of glaucoma.4 In addition to the classical glaucoma management, cataract extraction may help to lower the IOP independently.
Nevertheless, with good eye drop adherence, medical treatment is effective in minimizing the intraocular pressure. Although there are numerous challenges, such as the complexity of instruction and application of glaucoma medication, ocular symptoms, and cost-effectiveness may predispose to poor adherence.5 Glaucoma incisional surgery is a gold standard with great success in reducing intraocular pressure, but there are still many vision risks such as endophthalmitis or choroidal hemorrhage.6 In 2018, the Primary Tube Versus Trabeculectomy (PTVT) study found 1% of the group with drainage devices and 7% of the trabeculectomy group had serious complications leading to vision loss or reoperation.7
The minimally invasive glaucoma surgery (MIGS) era was introduced to minimize the IOP and reliance on topical medications with rapid visual recovery as a safer and least traumatic procedure for those with mild to moderate glaucoma and help them early in the disease.8 It is usually combined with cataract extraction surgery, using ab interno, micro-incisional, and conjunctiva-sparing approach. Since a visually significant cataract has been found to influence QOL, it will eventually lead to an improvement in QOL, along with MIGS.9 Unfortunately, the literature lacks evidence for the effect of glaucoma treatment on the quality of life. Most clinical trials focus on treatment success instead of patient satisfaction.10
This study’s objective is to assess the quality of life of patients undergoing combined cataract and MIGS from a different perspective (personal, social, occupational and economic status) and to express the impact of MIGS on the quality of life of patients with a safer and less invasive approach.
Methodology
Participants
A cross-sectional study was conducted in a total of 78 patients undergoing combined cataract and minimally invasive glaucoma surgery with various forms of MIGS for each patient, including either Kahook Dual Blade (KDB; New World Medical, Rancho Cucamonga, CA, USA) goniotomy, first-generation iStent (Glaukos Corporation, San Clemente, CA, USA), iStent inject (Glaukos Corporation, San Clemente, CA, USA) and gonioscopy-assisted transluminal trabeculotomy (GATT) between 2018 and 2019. All patients received regular follow-up for 18 months post-op. We have excluded any patient who has undergone any other ophthalmological surgery rather than MIGS and cataract extraction. The surgery was performed by one surgeon (A.H.). Patients have been reached at the ophthalmology clinic at King Fahd Hospital of the University in Khobar, Saudi Arabia.
QOL Questionnaire
A self-administered questionnaire based on the 25-item National Eye Institute Visual Function Questionnaire (NEI-VFQ-25) was designed to assess the impact of minimally invasive glaucoma surgery with cataract extraction on the quality of life. We assessed the benefit of the surgery on how many eye drops have been decreased, the side effect that results from the use of anti-glaucoma eye drop including redness, itching, and pain. We also assessed the level of dependability of others, number of ER visits and follow-up after the procedure and the progression of glaucoma subjectively by asking about the condition of vision and overall satisfaction of surgery.
Ethical Considerations
Patients’ anonymity was assured by using numbers rather than names for analysis only. All the participants were informed about the purpose of the study and a written consent was obtained from the patients before participation with the Helsinki Declaration. No incentives or rewards were given to the participant. This study was approved by the Institutional Review Board of the Imam Abdulrahman Bin Faisal University.
Statistical Analysis
The patient’s responses have been classified to a scale of 0–100 points and higher scores reflect better functioning and well-being. The composite score was determined as the mean of all questionnaire scales per case. The normality of the data has been checked by Kolmogorov–Smirnov Test. Preoperative and postoperative anti-glaucoma medications were compared with the McNemar–Bowker Test. The scores of the four surgeries per questionnaire scale were compared with the Kruskal Walli Test. The scores of two surgeries were compared with Mann–Whitney U-Test. The percentages were determined using a Chi-square test.
The difference in questionnaire scale scores equal to or greater than 10 points was considered clinically significant. A p-value of less than 0.05 was considered to be statistically significant. Statistical analysis was carried out by the Social Sciences Statistical Package (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.).
Results
The study included 93 eyes of 78 patients (40 males and 38 females) who underwent MIGS: 50 KDB, 13 first-generation iStent, 23 iStent inject and 7 GATT.
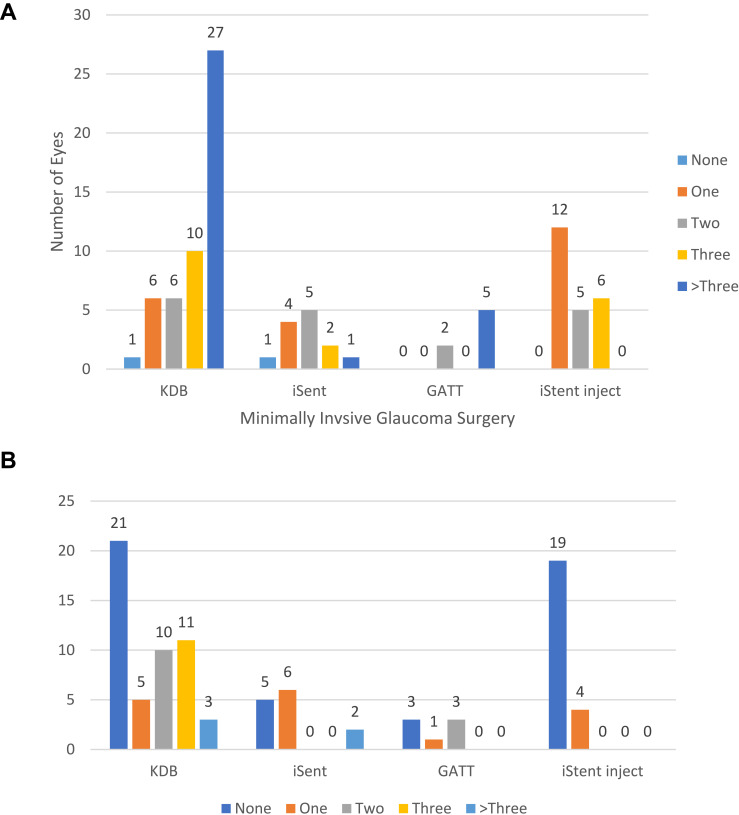
Approximately a similar number of males and females participated in the study. About 75.7% (59) of the patients were over 60 years of age. Approximately 85% (79) of the eyes had open-angle glaucoma (OAG). There was a statistically significant overall reduction in the number of anti-glaucoma medications (p<0.001). Figure 1A and B shows the preoperative and postoperative number of anti-glaucoma medications per surgery. The demographics and all characteristics are shown in Table 1.
Figure 1.
(A) Preoperative number of anti-glaucoma medications. (B) Postoperative number of anti-glaucoma medications.
Table 1.
Demographics and Clinical Characteristics of Glaucoma Patients Underwent Minimally Invasive Glaucoma Surgery
| Parameters | MIGS | KDB | iStent | GATT | iStent Inject | |
|---|---|---|---|---|---|---|
| Eyes (n) | 93 | 50 | 13 | 7 | 23 | |
| Age (years) | ||||||
| 20 to 40 | 2.6% (2) | |||||
| 41 to 60 | 21.8% (17) | |||||
| 61 to 70 | 44.9% (35) | |||||
| >70 | 30.8% (24) | |||||
| Gender | ||||||
| Male %(n) | 51.3(40) | |||||
| Female %(n) | 48.7(38) | |||||
| Diagnosis | ||||||
| POAG | 71.0% (66) | 54.0% (27) | 92.3% (12) | 100.0% (7) | 87.0% (20) | |
| SOAG | 14.0% (13) | 18.0% (9) | 7.7% (1) | 0% (0) | 13.0% (3) | |
| PACG | 10.8% (10) | 20.0% (10) | 0% (0) | 0% (0) | 0% (0) | |
| NTG | 1.1% (1) | 2.0% (1) | 0% (0) | 0% (0) | 0% (0) | |
| PXF | 3.2% (3) | 6.0% (3) | 0% (0) | 0% (0) | 0% (0) | |
| Preoperative AGM | ||||||
| 0 | 2.2% (2) | 2.0% (1) | 7.7% (1) | 0% (0) | 0% (0) | |
| 1 | 23.7% (22) | 12.0% (6) | 30.8% (4) | 0% (0) | 52.2% (12) | |
| 2 | 19.4% (18) | 12.0% (6) | 38.5% (5) | 28.6% (2) | 21.7% (5) | |
| 3 | 19.4% (18) | 20.0% (10) | 15.4% (2) | 0% (0) | 26.1% (6) | |
| >3 | 35.5% (33) | 54.0% (27) | 7.7% (1) | 71.4% (5) | 0% (0) | |
| Postoperative AGM | ||||||
| 0 | 51.6% (48) | 42.0% (21) | 38.5% (5) | 42.9% (3) | 82.6% (19) | |
| 1 | 17.2% (16) | 10.0% (5) | 46.2% (6) | 14.3% (1) | 17.4% (4) | |
| 2 | 14.0% (13) | 20.0% (10) | 0% (0) | 42.9% (3) | 0% (0) | |
| 3 | 11.8% (11) | 22.0% (11) | 0% (0) | 0% (0) | 0% (0) | |
| >3 | 5.4% (5) | 6.0% (3) | 15.4% (2) | 0% (0) | 0% (0) |
Abbreviations: MIGS, minimally invasive glaucoma surgery; KDB, Kahook Dual Blade; GATT, gonioscopy-assisted transluminal trabeculotomy; POAG, primary open-angle glaucoma; SOAG, secondary open-angle glaucoma; PACG, primary angle-closure glaucoma; NTG, normal-tension glaucoma; PXF, pseudoexfoliation glaucoma; AGM, anti-glaucoma medication.
Table 2 summarizes the percentages of the scale of the questionnaire in patients who underwent minimally invasive glaucoma surgery from different perspectives. From a personal perspective, 83.9% reported vision improvement. However, in terms of redness, itching, and pain, most patients reported that it was not there before surgery, but 40.9% reported a statistically significant improvement in redness after surgery (p<0.03). Also, 68.2% said that their sleep did not change. Moreover, since most of the participants were over 60 years of age, the majority of them were retired and therefore their occupational life did not change by 85.2%. On the other hand, after surgery, 36.6% had a better social life. In addition, 78.5% of patients were self-reliant for eye drops, and this did not change after surgery, which is statistically significant (p < 0.02). Finally, 86% were satisfied with the results of the surgery and 79% reported that the overall quality of life after the procedure improved.
Table 2.
Percent of Levels of Questionnaire Scale in Patients Underwent Minimally Invasive Glaucoma Surgery
| Questionnaire Scale | Level | MIGS (n=93) |
KDB (n=50) |
iStent (n=13) |
GATT (n=7) |
iStent Inject (n=23) |
P-value* |
|---|---|---|---|---|---|---|---|
| Vision | |||||||
| Better | 83.9% (78) | 78.0% (39) | 76.9% (10) | 85.7% (6) | 100% (23) | 0.277 | |
| No Change | 8.6% (8) | 12.0% (6) | 15.4% (2) | 0% (0) | 0% (0) | ||
| Worse | 7.5% (7) | 10.0% (5) | 7.7% (1) | 14.3% (1) | 0% (0) | ||
| Redness | |||||||
| Better | 40.9% (38) | 42.0% (21) | 30.8% (4) | 0% (0) | 56.5% (13) | 0.033 | |
| No change | 11.8% (11) | 14.0% (7) | 0% (0) | 0% (0) | 17.4% (4) | ||
| Worse | 3.2% (3) | 4.0% (2) | 0% (0) | 14.3% (1) | 0% (0) | ||
| No redness before | 44.1% (41) | 40.0% (20) | 69.2% (9) | 85.7% (6) | 26.1% (6) | ||
| Itching | |||||||
| Better | 25.8% (24) | 20.0% (10) | 30.8% (4) | 0% (0) | 43.5% (10) | 0.189 | |
| No change | 16.1% (15) | 20.0% (10) | 7.7% (1) | 0% (0) | 17.4% (4) | ||
| Worse | 10.8% (10) | 10.0% (5) | 7.7% (1) | 14.3% (1) | 13.0% (3) | ||
| No itching before | 47.3% (44) | 50.0% (25) | 53.8% (7) | 85.7% (6) | 26.1% (6) | ||
| Pain | |||||||
| Better | 35.5% (33) | 36.0% (18) | 53.8% (7) | 14.3% (1) | 30.4% (7) | 0.052 | |
| No change | 9.7% (9) | 4.0% (2) | 7.7% (1) | 0% (0) | 26.1% (6) | ||
| Worse | 8.6% (8) | 10.0% (5) | 0% (0) | 28.6% (2) | 4.3% (1) | ||
| No pain before | 46.2% (43) | 50.0% (25) | 38.5% (5) | 57.1% (4) | 39.1% (9) | ||
| Occupational life | |||||||
| Better | 14.8% (13) | 16.3% (8) | 7.7% (1) | 0% (0) | 21.1% (4) | 0.490 | |
| No change | 85.2% (75) | 83.7% (41) | 92.3% (12) | 100% (7) | 78.9% (15) | ||
| Worse | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | ||
| Social life | |||||||
| Better | 36.6% (30) | 35.6% (16) | 38.5% (5) | 0% (0) | 52.9% (9) | 0.209 | |
| No change | 59.8% (49) | 60.0% (27) | 61.5% (8) | 85.7% (6) | 47.1% (8) | ||
| Worse | 3.7% (3) | 4.4% (2) | 0% (0) | 14.3% (1) | 0% (0) | ||
| Economic status | |||||||
| Better | 1.1% (1) | 2.0% (1) | 0% (0) | 0% (0) | 0% (0) | 0.853 | |
| No change | 98.9% (86) | 98.0% (48) | 100% (13) | 100% (7) | 100% (18) | ||
| Worse | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | ||
| Sleep | |||||||
| Better | 27.1% (23) | 26.5% (13) | 30.8% (4) | 0% (0) | 33.3% (6) | 0.489 | |
| No change | 68.2% (58) | 65.3% (32) | 69.2% (9) | 100% (5) | 66.7% (12) | ||
| Worse | 4.7% (4) | 8.2% (4) | 0% (0) | 0% (0) | 0% (0) | ||
| Hospital followup | |||||||
| Decreased | 55.9% (52) | 60.0% (30) | 61.5% (8) | 85.7% (6) | 34.8% (8) | 0.255 | |
| No change | 40.9% (38) | 36.0% (18) | 38.5% (5) | 14.3% (1) | 60.9% (14) | ||
| Increased | 3.2% (3) | 4.0% (2) | 0% (0) | 0% (0) | 4.3% (1) | ||
| ER visits | |||||||
| Decreased | 31.2% (29) | 36.0% (18) | 23.1% (3) | 57.1% (4) | 17.4% (4) | 0.399 | |
| No change | 67.7% (63) | 62.0% (31) | 76.9% (10) | 42.9% (3) | 82.6% (19) | ||
| Increased | 1.1% (1) | 2.0% (1) | 0% (0) | 0% (0) | 0% (0) | ||
| Dependency | |||||||
| Decreased | 12.9% (12) | 24.0% (12) | 0% (0) | 0% (0) | 0% (0) | 0.029 | |
| No change | 78.5% (73) | 66.0% (33) | 100% (13) | 85.7% (6) | 91.3% (21) | ||
| Increased | 8.6% (8) | 10.0% (5) | 0% (0) | 14.3% (1) | 8.7% (2) | ||
| Satisfaction | |||||||
| Satisfied | 86.0% (80) | 80.0% (40) | 84.6% (11) | 85.7% (6) | 100% (23) | 0.232 | |
| No difference | 5.4% (5) | 10.0% (5) | 0% (0) | 0% (0) | 0% (0) | ||
| Unsatisfied | 8.6% (8) | 10.0% (5) | 15.4% (2) | 14.3% (1) | 0% (0) | ||
| Overall QOL | |||||||
| Improved | 79.6% (74) | 74.0% (37) | 69.2% | 85.7% (6) | 95.7% (22) | 0.109 | |
| Same as before | 14.0% (13) | 16.0% (8) | 30.8% (4) | 0% (0) | 4.3% (1) | ||
| Worse | 6.5% (6) | 10.0% (5) | 0% (0) | 14.3% (1) | 0% (0) |
Note: *Chi-square test was performed.
Abbreviations: MIGS, minimally invasive glaucoma surgery; KDB, Kahook Dual Blade; GATT, gonioscopy-assisted transluminal trabeculotomy; POAG, primary open-angle glaucoma; SOAG, secondary open-angle glaucoma; PACG, primary angle-closure glaucoma; NTG, normal-tension glaucoma; PXF, pseudoexfoliation glaucoma.
The mean and standard deviation of scores by questionnaire scale per procedure is shown in Table 3. The positive Spearman rho Correlation between age and MIGS composite score was neither clinically important nor statistically significant (r=0.109, p=0.338). There was no statistically significant difference between gender in the composite score (p=0.863) There was a statistically significant difference between the redness in the questionnaire scale (p=0.010), itching (p=0.019) and the composite score (p=0.021). The redness and itching scales were better for the iStent inject group and worse for the GATT group. There was no statistically significant difference between the four study groups in the rest of the questionnaire scales (P>0.05). In the pain scale, however, there was a clinically important difference of 36.3 points between the iStent group and the GATT group. On the occupational life scale, the iStent group differed by 10.5 points from the GATT group. In social life, there was a clinically important difference of 33.6 points between the iStent inject group and the GATT group. There was no clinically important difference in economic status between surgeries. In the sleep scale, iStent inject was 16.7 points higher than GATT. The GATT group differed by 14.9 points from the KDB in the hospital follow-up scale. The GATT group differed by 19.9 points from the iStent inject group in the ER visit scale. In the satisfaction scale, iStent inject differed by 15.4 points from the iStent group. There was no clinically important difference between surgeries in the overall QOL scale. The composite score was the highest in the iStent inject group and the lowest in the GATT group. The composite scores of the KDB and iStent inject groups were statistically different (p=0.030). In addition, the iStent group and the iStent inject showed a statistical difference in the composite score (p=0.050). There was no statistically significant difference in the composite score between the KDB group and the iStent group (p=0.666).
Table 3.
Questionnaire Scores in Patients Underwent Minimally Invasive Glaucoma Surgery
| Questionnaire Scale | MIGS (n=93) |
KDB (n=50) |
iStent (n=13) |
GATT (n=7) |
iStent Inject (n=23) |
P-value |
|---|---|---|---|---|---|---|
| Vision | 88.2±28.9 | 84.0±32.6 | 84.6±31.5 | 85.7±37.8 | 100.0±0 | 0.113 |
| Redness | 47.6±46.5 | 50.0±46.0 | 30.8±48.0 | 3.6±9.4 | 65.2±43.8 | 0.010 |
| Itching | 36.6±41.6 | 32.5±39.2 | 36.5±46.3 | 3.6±9.4 | 55.4±43.3 | 0.019 |
| Pain | 42.5±45.4 | 40.5±46.5 | 57.7±49.4 | 21.4±36.6 | 44.6±42.6 | 0.489 |
| Occupational life | 57.4±17.8 | 58.2±18.7 | 53.8±13.9 | 50.0±0 | 60.5±20.9 | 0.495 |
| Social life | 66.5±27.3 | 65.6±27.8 | 69.2±25.3 | 42.9±18.9 | 76.5±25.7 | 0.062 |
| Economic status | 50.6±5.4 | 51.0±7.1 | 50.0±0 | 50.0±0 | 50.0±0 | 0.855 |
| Sleep | 61.2±26.0 | 59.2±28.3 | 64.4±24.0 | 50.0±0 | 66.7±24.3 | 0.510 |
| Hospital follow-up | 76.3±28.2 | 78.0±28.9 | 80.8±25.3 | 92.9±18.9 | 65.2±27.9 | 0.073 |
| ER visits | 65.1±24.2 | 67.0±26.0 | 61.5±21.9 | 78.6±26.7 | 58.7±19.4 | 0.202 |
| Dependency | 52.2±23.2 | 57.0±28.6 | 50.0±0 | 42.9±18.9 | 45.7±14.4 | 0.142 |
| Satisfaction | 88.7±29.6 | 85.0±32.3 | 84.6±37.6 | 85.7±37.8 | 100.0±0 | 0.167 |
| Overall QOL | 86.6±28.7 | 82.0±33.1 | 84.6±24.0 | 85.7±37.8 | 97.8±10.4 | 0.146 |
| Composite Score | 69.4±13.0 | 69.0±13.3 | 67.5±13.5 | 57.5±13.9 | 75.9±7.8 | 0.021 |
Abbreviations: MIGS, minimally invasive glaucoma surgery; KDB, Kahook Dual Blade; GATT, gonioscopy-assisted transluminal trabeculotomy; POAG, primary open-angle glaucoma; SOAG, secondary open-angle glaucoma; PACG, primary angle-closure glaucoma; NTG, normal-tension glaucoma; PXF, pseudoexfoliation glaucoma.
Discussion
Quality of life is considered to be one of the major and important factors in the health and well-being of patients. Compared to other progressive disorders, glaucoma had fewer publications on quality of life.10 In fact, maintaining the quality of life of patients with glaucoma is one of the primary objectives of treatment for this neurodegenerative progressive disease. In our study, we used a questionnaire based on the 25-item National Eye Institute Visual Function Questionnaire (NEI-VFQ-25) that is well established to assess QOL in relation to visual functions,11 to determine the overall QOL and the level of satisfaction from surgical outcome of glaucoma patient who underwent minimal invasive glaucoma surgery with cataract extraction.
Glaucoma needs lifelong treatment and, like many other chronic diseases, it has a low adherence rate which results in disease progression; on the other hand, glaucoma treatment is well known for its local and systemic side effects and can improve patient QOL by reducing them.12 However, a cross-sectional study on 360 participants was conducted in 2018 to determine the proportion of adherence to topical glaucoma medications that showed 61.4% adherence to their glaucoma medications, but although more than half of the participants were adherents, it is still not good enough.13 Studies have consistently shown that greater adherence is correlated with simpler medication regimens. Pahlitzsch et al found a significant reduction in glaucoma eye drops following MIGS.14 Besides the favorable risk profile of MIGS, it had a moderate efficacy in decreasing the IOP.12 In our study, there was a statistically significant overall reduction in the number of anti-glaucoma medications (p<0.001) following MIGS. In addition, 40.9% reported an improvement in redness after surgery, which could be linked to a reduction in the number of glaucoma medications and was statistically significant (p < 0.03). The changes in visual acuity have a great effect on the QOL, but NEI VFQ depends only on the VA to determine the vision status and that could be preserved in glaucoma patients as their visual deficiencies start from the visual field.15 As assessed by VF testing recent study showed that glaucoma even at an early stage has a significant effect on QOL of patients and that could decrease in accordance with glaucoma severity.16 Nevertheless, our study shows that 83.9% of patients had better vision after the combined procedure, which was not statistically significant (p=0.27). It may be due to the impact of cataract extraction or the optic nerve status, as most patients had mild to moderate glaucoma. Another advantage of MIGS strategies is a reduced risk of a large refractive surprise compared to conventional filtering operations and faster visual rehabilitation.17 Sieck et al concluded that there were no difference found between the refractive outcomes of glaucoma patients with or without KDB.18 Also, in 2020 a study result that iStent inject does not risk refractive outcomes and can be paired with cataract procedure safely.19
In addition, most patients reported that there were no changes in their occupational, social and economic status following MIGS (85.2%, 59.8% and 98.8%) respectively. Since most of patients were over 60 years of age and retired, this may explain why their occupational life did not change and their economic status was not affected by changes in increased or decreased number of eye drops, as our institution provides free eye drops to all patients. However, about 31.2% of patients report a decrease in the frequency of emergency room visits due to eye complaints. The KDB and GATT groups appear to have more regular follow-up in the clinic as a result of post-op hyphema in the early postoperative period, which gradually decreased to a comparable extent with the other subgroups. It may affect the QOL by initially raising the number of eye drops with stress on compliance and indirectly through close clinic follow-ups and prolonged recovery time. Also, most patients were independent when applying eye drops and this will also improve QOL.
Finally, 86% were satisfied with the result of the surgery and 79% confirmed subjectively the improvement of the overall quality of life following the surgery. In addition, the study had a limitation in evaluating the visual function using the NEI VFQ by using only the visual acuity in deciding glaucoma progression, other modalities such as visual field and optical coherence tomography (OCT) for the optic nerve should be used.
Conclusion
QOL is one of the important aspects of the management plan for each disease and should be kept in mind when dealing with patients, particularly those with a progressive disease pattern. We believed that the treatment of mild to moderate glaucoma in patients with MIGS would improve QOL from different perspectives and reduce the number of eye drops needed and, in turn, reduce its side effects. In addition, MIGS considered a safe and feasible surgical intervention that could replace other invasive procedures. Eventually, quality of life plays a key role in the life of a patient and should be safeguarded by providing all possible options.
Acknowledgment
The authors thankfully acknowledge Dr. Hatlan Mohammed Alhatlan for his contributions to our study’s data collection.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Elliott DB, Pesudovs K, Mallinson T. Vision-related quality of life. Optom Vis Sci. 2007;84:656–658. doi: 10.1097/OPX.0b013e31814db01e [DOI] [PubMed] [Google Scholar]
- 2.Ribeiro MVMR, Hasten-Reiter HN, Ribeiro EAN, Jucá MJ, Barbosa FT, de Sousa-rodrigues CF. Association between visual impairment and depression in the elderly: a systematic review. Arq Bras Oftalmol. 2015;78:197–201. doi: 10.5935/0004-2749.20150051 [DOI] [PubMed] [Google Scholar]
- 3.Goldberg I, Clement CI, Chiang TH, et al. Assessing quality of life in patients with glaucoma using the glaucoma quality of life-15 (GQL-15) questionnaire. J Glaucoma. 2009;18(1):6–12. doi: 10.1097/IJG.0b013e3181752c83 [DOI] [PubMed] [Google Scholar]
- 4.Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M. Reduction of intraocular pressure and glaucoma progression: results from the early manifest glaucoma trial. Arch Ophthalmol. 2002;120(10):1268–1279. doi: 10.1001/archopht.120.10.1268 [DOI] [PubMed] [Google Scholar]
- 5.Joseph A, Pasquale LR. Attributes associated with adherence to glaucoma medical therapy and its effects on glaucoma outcomes: an evidence-based review and potential strategies to improve adherence. Semin Ophthalmol. 2017;32(1):86–90. doi: 10.1080/08820538.2016.1228406 [DOI] [PubMed] [Google Scholar]
- 6.Gedde SJ, Schiffman JC, Feuer WJ, Herndon LW, Brandt JD, Budenz DL. Treatment outcomes in the tube versus trabeculectomy (TVT) study after five years of follow-up. Am J Ophthalmol. 2012;153(5):789–803. doi: 10.1016/j.ajo.2011.10.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gedde SJ, Feuer WJ, Shi W, et al. Treatment outcomes in the primary tube versus trabeculectomy study after 1 year of follow-up. Ophthalmology. 2018;125(5):650–663. doi: 10.1016/j.ophtha.2018.02.003 [DOI] [PubMed] [Google Scholar]
- 8.Francis BA, Singh K, Lin SC, et al. Novel glaucoma procedures: a report by the American Academy of ophthalmology. Ophthalmology. 2011;118(7):1466–1480. doi: 10.1016/j.ophtha.2011.03.028 [DOI] [PubMed] [Google Scholar]
- 9.Skalicky SE, Martin KR, Fenwick E, Crowston JG, Goldberg I, McCluskey P. Cataract and quality of life in patients with glaucoma. Clin Exp Ophthalmol. 2015;43(4):335–341. doi: 10.1111/ceo.12454 [DOI] [PubMed] [Google Scholar]
- 10.Waisbourd M, Parker S, Ekici F, et al. A prospective, longitudinal, observational cohort study examining how glaucoma affects quality of life and visually-related function over 4 years: design and methodology Glaucoma. BMC Ophthalmol. 2015;15(1):91. doi: 10.1186/s12886-015-0088-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119(7):1050–1058. doi: 10.1001/archopht.119.7.1050 [DOI] [PubMed] [Google Scholar]
- 12.M-G F, T-H M. Influence of cost of care and adherence in glaucoma management: an update. J Ophthalmol. 2020;2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anbesse DH, Yibekal BT, Assefa NL. Adherence to topical glaucoma medications and associated factors in Gondar University Hospital Tertiary Eye Care Center, northwest Ethiopia. Eur J Ophthalmol. 2019;29(2):189–195. doi: 10.1177/1120672118772517 [DOI] [PubMed] [Google Scholar]
- 14.Pahlitzsch M, Klamann MKJ, Pahlitzsch ML, Gonnermann J, Torun N, Bertelmann E. Is there a change in the quality of life comparing the micro-invasive glaucoma surgery (MIGS) and the filtration technique trabeculectomy in glaucoma patients? Graefe’s Arch Clin Exp Ophthalmol. 2017;255(2):351–357. doi: 10.1007/s00417-016-3550-4 [DOI] [PubMed] [Google Scholar]
- 15.Kotecha A, Feuer WJ, Barton K, Gedde SJ. Quality of life in the tube versus trabeculectomy study. Am J Ophthalmol. 2017;176:228–235. doi: 10.1016/j.ajo.2017.01.019 [DOI] [PubMed] [Google Scholar]
- 16.Azoulay-Sebban L, Zhao Z, Zenouda A, et al. Correlations between subjective evaluation of quality of life, visual field loss and performance in simulated activities of daily living in glaucoma patients. J Glaucoma. 2020. doi: 10.1097/IJG.0000000000001597 [DOI] [PubMed] [Google Scholar]
- 17.Luebke J, Boehringer D, Neuburger M, et al. Refractive and visual outcomes after combined cataract and trabectome surgery: a report on the possible influences of combining cataract and trabectome surgery on refractive and visual outcomes. Graefe’s Arch Clin Exp Ophthalmol. 2015;253(3):419–423. doi: 10.1007/s00417-014-2881-2 [DOI] [PubMed] [Google Scholar]
- 18.Sieck EG, Capitena Young CE, Epstein RS, et al. Refractive outcomes among glaucoma patients undergoing phacoemulsification cataract extraction with and without Kahook Dual Blade goniotomy. Eye Vis. 2019;6(1):28. doi: 10.1186/s40662-019-0153-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ioannidis AS, Töteberg-Harms M, Hamann T, Hodge C. Refractive outcomes after trabecular micro-bypass stents (Istent inject) with cataract extraction in open-angle glaucoma. Clin Ophthalmol. 2020;14:517–524. doi: 10.2147/OPTH.S239103 [DOI] [PMC free article] [PubMed] [Google Scholar]