Abstract
We present the case of a young adult with stroke and very mild coronavirus disease 2019 (COVID-19). Results of hematologic work-up suggest SARS-CoV-2-induced endotheliitis. No concurrent etiology for stroke was detected. This case illustrates the possibility of stroke in healthy SARS-CoV-2-infected patients without hyperinflammatory state or excessive systemic coagulation activation.
Keywords: Coagulopathy, endothelial dysfunction, endotheliitis, SARS-CoV-2, stroke
We describe a previously healthy 24-year-old man who presented with a 1-day history of left-sided paresthesia, arm weakness and hemiataxia, homonymous hemianopsia and gait instability (National Institutes of Health Stroke Scale (NIHSS) 4). Twenty-four hours earlier he had noted a fever (temperature 38.5°C), nausea and right-sided headache but denied any respiratory symptoms. He was not receiving any medication and denied any illicit drug use.
At presentation, the patient was in good general condition; vital signs were normal. Chest radiograph was unremarkable; C-reactive protein was 13 mg/L (reference, <8 mg/L). Cerebral imaging (computed tomography and magnetic resonance imaging) showed ischaemic stroke in the territory of the right posterior cerebral artery with persisting thrombus (P1/2 segment) (Fig. 1). Cerebrospinal fluid (CSF) showed slightly elevated proteins of 0.59 g/L (reference, 0.15–0.45 g/L); cell count and glucose and lactate levels were normal. PCR of nasopharyngeal swab and stool samples was performed and was positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2); PCR testing of blood and CSF samples remained negative.
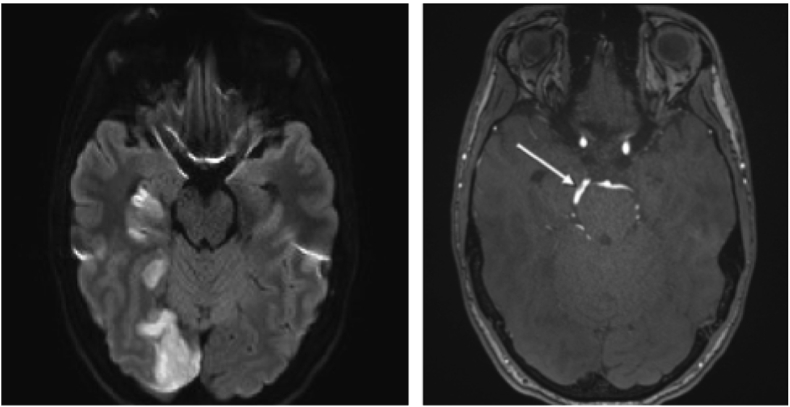
Fig. 1.
(Left) Diffusion-weighted magnetic resonance imaging scan of right hemispheric thalamus, hippocampus and occipital ischaemia. (Right) Time-of-flight magnetic resonance angiography of right posterior cerebral artery with partially autolyzed rest thrombus.
Investigations for other infectious agents (influenza A/B, syphilis, HIV, hepatitis B/C, varicella, herpes simplex, Borrelia burgdorferi) were negative, except for Mycoplasma pneumoniae–specific IgM and IgG antibodies, which were positive at low levels. An acute M. pneumoniae infection was excluded by negative nasopharyngeal and CSF PCR results, negative antibody-secreting cell (ASC) enzyme–linked immunospot (ELISpot) assay results and by follow-up serology, which did not show significant changes. Blood culture testing and cold agglutinin and autoantibody screening were negative.
Transesophageal echocardiography did not reveal any cardiac thrombus, endocarditis or patent foramen ovale. Long-term electrocardiogram monitoring was unremarkable. Coagulation assessment 3 days after admission revealed markedly elevated factor VIII at 321% (reference, 50–150%) and von Willebrand factor activity at 198% (reference, 65–145%); however, no signs of systemic blood coagulation activation were evident (nonelevated d-dimers and prothrombin fragments), suggesting vascular endothelial dysfunction. Classical hereditary thrombophilia, lupus anticoagulant and antiphospholipid antibodies were excluded later in the course.
The patient was treated with acetylsalicylic acid, enoxaparin and hydroxychloroquine and was discharged to a rehabilitation hospital 14 days after hospital admission. Antibody testing against SARS-CoV-2 at 6 weeks after initial presentation showed positive IgG and negative IgM.
We present the case of a previously healthy young adult with stroke in the context of very mild coronavirus disease 2019 (COVID-19). Extensive assessment did not reveal any other infectious or noninfectious cause. Ischaemic stroke has been reported in association with COVID-19, particularly among the elderly and those with a severe disease course [1,2]. Coagulopathy and vascular endothelial dysfunction have been discussed as complications of COVID-19 [3]. Although not proven, results of haematologic assessment in our patient suggested SARS-CoV-2–induced endotheliitis as the underlying pathomechanism. Indeed, SARS-CoV-2 has been shown to attack angiotensin-converting enzyme 2 receptors in endothelial cells causing endotheliitis, thereby disrupting the integrity of the blood vessel wall [4]. In a report of three COVID-19 patients with mesenteric ischaemia, histopathology identified viral elements and accumulation of inflammatory cells associated with endothelial cells [5].
This case illustrates the possibility of stroke in healthy SARS-CoV-2–infected patients without evidence of a hyperinflammatory state or excessive systemic coagulation activation. We recommend measuring factor VIII and von Willebrand factor levels as sign of endothelial activation in case of COVID-19–associated cryptogenic stroke.
Conflicts of interest
None declared.
References
- 1.Mao L., Jin H., Wang M., Hu Y., Chen S., He Q. Vol. 77. JAMA Neurol; 2020. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. ;77:683–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oxley T.J., Mocco J., Majidi S., Kellner C.P., Shoirah H., Singh P. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020;382 doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang Y., Xiao M., Zhang S., Xia P., Cao W., Jiang W. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med. 2020;382:e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Monteil V., Kwon H., Prado P., Hagelkrüys A., Wimmer R.A., Stahl M. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell. 2020;181:905–913. doi: 10.1016/j.cell.2020.04.004. e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A.S. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]