1. Background
The current ongoing pandemic of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2; COVID-19) is increasing worldwide and in India [1]. The most symptoms are cough, shortness of breath, and fever [2]. Gastrointestinal manifestations of COVID-19 are increasingly being recognized; diarrhea being most common. Here we report a case of acute pancreatitis in a patient positive for COVID-19.
2. Case report
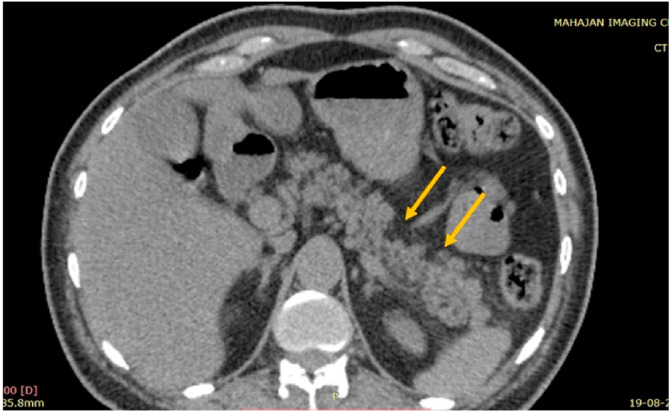
A 63-year-old man with a known case of T2DM on metformin (500 mg twice daily) was referred to our hospital with complaints of fever, shortness of breath and dry cough since 4 days. A SARS COV-2 Real time polymerase chain reaction (RT-PCR) done at a local hospital 2 days back was negative and he was subsequently admitted there with oxygen saturation 80% at room air and was put on oxygen. Upon noticing no improvement in his condition, the family decided to shift him to a tertiary COVID care center. During admission in our hospital he was tested positive for SARS COV-2 by RT-PCR. There was no history of alcohol intake, hypertriglyceridemia or cholelithiasis. He did not have icterus and chest examination revealed bilateral basal crepitations. His SpO2 was 92% on 2 L of nasal oxygen. His investigations on admission were; hemoglobin, 12.8g/dL, white blood cell count, 9000/microL, fasting blood glucose: 289mg/dl, HbA1C, 9%, Interleukin-6, 3.10pg/ml (normal ≤4.40 pg/mL), C-reactive protein, 38.9mg/L (normal <10 mg/L) and normal renal functions. During hospitalization he was given intravenous antibiotics, remdesvir, anticoagulant, and corticosteroids. Hyperglycemia was managed by high doses of insulin. He was discharged and was apparently well for 2 days then he developed drowsiness due to hypoglycemia. During this second admission, his urine culture showed Klebsiella Pneumonia for which he was started on antibiotics. A non-contrast computerized tomography scan of abdomen revealed bulky pancreatic tail with focal areas of necrosis in body and tail of pancreas involving less than 30% of pancreatic parenchyma (Fig. 1 ). His biochemistry was as follows; amylase 58U/L(normal 25–115U/L), lipase 412 U/L (normal 73–160 U/L), serum calcium7.3mg/dL (normal 8.5–10.1 mg/dL), and serum albumin 2.4g/dL (normal 3.5–7.2g/dL). His modified Glasgow Pancreatitis Severity Score was 5 (score >3 suggests severe pancreatitis). He was managed conservatively for his pancreatitis. He was discharged in a fair clinical condition.
Fig. 1.
Transverse section of non-contrast enhanced computerized tomography of abdomen showing bulky pancreatic tail with area of necrosis in body and tail of pancreas (marked by yellow arrows) involving less than 30% of pancreatic parenchyma. Small amount of fluid collection extending along the left anterior and lateroconal fascia is also visible. There was no internal pancreatic calcification.
3. Discussion
There are many etiological factors for acute pancreatitis which include gallstones, alcohol abuse, hypertriglyceridemia, hypercalcemia, infectious diseases etc. [3]. Previous studies have shown that acute inflammation in the pancreas may also be due to various viruses like human immunodeficiency virus, mumps, measles, cytomegalovirus, coxsackievirus B, influenza A (H1N1), epstein barr virus, and hepatitis B, A, E viruses [4]. COVID19 related acute pancreatitis is beginning to gain research attention.
In absence of any known etiology of pancreatitis, radiological findings of necrosis of pancreatic body and tail (Fig. 1), increased serum lipase along with COVID-19 infection confirms the relationship between acute pancreatitis and COVID-19 in our case. Only one other case of acute pancreatitis due to COVID19 has been reported from India [5]. Worldwide, COVID19 related pancreatitis has been reported in a total of 22 patients.
A case-series of 52 COVID-19 patients from China showed that 17% of patients had pancreatic injury as defined by any abnormalities in amylase/lipase. Interestingly these patients did not have any clinical symptom suggestive of pancreatitis similar to our patient [6]. Hadi et al. [7] reported acute pancreatitis in 2 out 3 COVID-19 affected family members from Denmark. In these cases, associated complications of COVID-19 like respiratory distress and acute kidney injury were severe. In another publication, pancreatitis as a complication of COVID-19 was reported in a 59-year-old female with fever, sore throat, and cough. Her comparative CT findings showed marked increase in size of pancreas which was previously atrophied [8]. In a case reported from India a 29-year-old male with fever, abdomen pain, and respiratory distress was diagnosed with COVID-19 and also had acute pancreatitis confirmed on biochemical and radiological investigations [5].
Entry of COVID-19 in human cells is mediated by angiotensin-converting enzyme-2 (ACE-2) receptor on the host cells. These receptors are highly expressed in the human pancreatic islets [9]. Although exact pathogenesis is unknown, pancreatic injury in COVID19 could occur due to the direct cytopathogenic effect of SARS-CoV-2 or by cytokine storm induced cell injury.
Pancreatitis induced by COVID-19 induced is rare, and more data are required. In any case of pancreatitis during this epidemic, common causes of acute pancreatitis must be ruled out before diagnosis of COVID19 induced pancreatitis is made.
Declaration of competing interest
The authors declare ‘no conflict of interest’ regarding this particular article.
Acknowledgement
The authors would like to acknowledge pulmonologist team of Fortis Flt. Lt. Rajan Dhall Hospital, Vasantkunj: Dr. J.C.Suri, Dr. Ayush Gupta, Dr. Abhijeet Singh, and Dr. Nikhil Bante.
References
- 1.Caballero A.E., Ceriello A., Misra A. COVID-19 in people living with diabetes: an international consensus. J Diabet Complicat. 2020;34(9):107671. doi: 10.1016/j.jdiacomp.2020.107671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta R., Ghosh A., Singh A.K., Misra A. Clinical considerations for patients with diabetes in times of COVID-19 epidemic. Diabetes Metab Syndr. 2020;14(3):211–212. doi: 10.1016/j.dsx.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Banks P.A., Conwell D.L., Toskes P.P. The management of acute and chronic pancreatitis. Gastroenterol Hepatol (N Y). 2010 Feb;6(2 Suppl 3):1–16. [PMC free article] [PubMed] [Google Scholar]
- 4.Rawla P., Bandaru S.S., Vellipuram A.R. Review of infectious etiology of acute pancreatitis. Gastronterol Res. 2017;10(3):153–158. doi: 10.14740/gr858w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nikhil Kumar Patnaik R., Gogia A., Kakar A. Acute pancreatic injury induced by COVID-19. IDCases. 2020 doi: 10.1016/j.idcr.2020.e00959. [published online ahead of print, 2020 Sep 10] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang F., Wang H., Fan J. Pancreatic injury patterns in patients with COVID-19 pneumonia. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.03.055. Epub Ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hadi A., Werge M., Kristiansen K.T. Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: case report on three family members. Pancreatology. 2020;20(4):665–667. doi: 10.1016/j.pan.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anand E.R., Major C., Pickering O., Nelson M. Acute pancreatitis in a COVID-19 patient. Br J Surg. 2020;107(7) doi: 10.1002/bjs.11657. 10.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu F., Long X., Zhang B., Zhang W., Chen X., Zhang Z. ACE2 Expression in Pancreas May Cause Pancreatic Damage After SARS-CoV-2 Infection. Clin Gastroenterol Hepatol. 2020;18(9):2128–2130. doi: 10.1016/j.cgh.2020.04.040. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]