Abstract
Various organizations and societies around the globe have issued guidelines in response to the coronavirus disease (COVID-19) and virus (SARS-CoV-2). In this paper, heating, ventilating, and air-conditioning-related guidelines or documents in several major countries and regions have been reviewed and compared, including those issued by the American Society of Heating Refrigerating and Air-Conditioning Engineers, the Federation of European Heating, Ventilation, and Air Conditioning Associations, the Society of Heating, Air-Conditioning and Sanitary Engineers of Japan, Architectural Society of China, and the Chinese Institute of Refrigeration. Most terms and suggestions in these guidelines are consistent with each other, although there are some conflicting details, reflecting the underlying uncertainty surrounding the transmission mechanism and characteristics of COVID-19 in buildings. All guidelines emphasize the importance of ventilation, but the specific ventilation rate that can eliminate the risk of transmission of airborne particulate matter has not been established. The most important countermeasure, commonly agreed countermeasures, the conflicting content from different guidelines, and further work have been summarized in this paper.
Keywords: SARS-CoV-2, COVID-19, HVAC, Guidance
Nomenclature
- ASHRAE
the American Society of Heating, Refrigeration, and Air-Conditioning Engineers
- AHU
Air handling unit
- CDC
Centers for Disease Control and Prevention
- CIBSE
The Chartered Institution of Building Services Engineers
- COVID-19
Coronavirus Disease 2019
- DCV
demand control ventilation
- ECDC
European Centre for Disease Prevention and Control
- FGI
the Facilities Guidelines Institute
- HEPA(HEPA filter)
high-efficiency particulate air(high-efficiency particulate absorbing)
- HVAC
Heating, ventilation and air-conditioning
- MERV
minimum efficiency reporting value
- REHVA
the Federation of European of Heating, Ventilation, and Air-Conditioning Associations
- RLT
the German Association of Indoor Ventilation Technologies
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- SHASE
the Society of Heating, Air-Conditioning and Sanitary Engineering in Japan
- UV
ultraviolet
- UV-C
the ultraviolet with the wavelengths from 200 to 280 nm
- UVGI
ultraviolet germicidal irradiation
1. Introduction
1.1. The role of the HVAC system in the transmission of COVID-19
The coronavirus disease (i.e. COVID-19) started affecting the world at the beginning of 2020. According to a pre-print study of 318 outbreaks involving 1245 confirmed COVID-19 cases in 120 prefectural cities of China, all outbreaks occurred in indoor spaces except one involving only 2 cases, which implicates sharing indoor space is a major SARS-CoV-2 infection risk [1]. The duty of HVAC system is to maintain a healthy and comfortable indoor environment. However, poor ventilation in indoor spaces is associated with increased transmission of respiratory infections [2]. The bad use of ventilation systems is non-negligible factors in SARS-CoV-2 transmission [3]. A COVID-19 outbreak in a restaurant without windows is reported to be associated with the bad use of air conditioning [4]. In this outbreak, persons around tables nearby the infector's table were still infected while the distances between them and the infector were all greater than 1 m. The author implicates the transmission of respiratory droplets carrying SARS-CoV-2 was prompted by the airflow generated by the air-conditioning. Studies have shown that SARS-CoV-2 was detected in the air [5]. And in the outbreak of the Diamond Princess cruise ship, a study indicates except the main route for transmission(person to person), other routes such as aerosol transmission via central air supply or drainage system should not be neglected [6]. According to WHO, Airborne transmission (i.e. the spread of an infectious agent caused by the dissemination of droplet nuclei that remains infectious when suspended in air over long distances and time.) of SARS-CoV-2 can occur during the medical procedure that generates aerosols [7]. It is also possible that SARS-CoV-2 can be transmitted by air in other situations. So, dilution ventilation, correct direction of airflow, pressure differential, etc. offered by the well-maintained HVAC system could effectively mitigate the risk of SARS-CoV-2 transmission. ASHRAE even stated two statements officially opposing the advice not to run residential or commercial HVAC systems [8].
1.2. HVAC-related guidelines or documents associated with COVID-19
Since the HVAC system plays such an important role in the transmission of SARS-CoV-2, how best to operate heating, ventilating, and air-conditioning (i.e. HVAC) systems has become an urgent problem for the HVAC industry. Till June 2020, HVAC-related institutions such as the Architectural Society of China, the Chinese Association of Refrigeration, the American Society of Heating, Refrigeration, and Air-Conditioning Engineers (i.e. ASHRAE), the Federation of European of Heating, Ventilation, and Air-conditioning Associations (REHVA), and the Society of Heating, Air-Conditioning and Sanitary Engineering in Japan (i.e. SHASE) have all issued documents in response to COVID-19. On January 20, 2020, China's National Health Commission included the new pneumonia, COVID-19, as a Class B infectious disease, the prevention and control measures were for a Class A infectious disease, and the new pneumonia was treated according to the “Health and Quarantine Law of the People's Republic of China.” [9] The Architectural Society of China has given corresponding guidelines for hospitals, office buildings, residential buildings, hotels used for temporary isolation, and public buildings that were transformed into temporary hospitals [10]. The State Council of China issued “Guidelines for The Operation and Management of Air-Conditioning and Ventilation Systems in Office and Public Buildings during the COVID-19 Epidemic.” [11] The Chinese Association of Refrigeration also issued “Recommendations for the Safe Use of Air-Conditioning (Heating) Systems in Response to the COVID-19 Epidemic.” [12] ASHRAE issued a position document on airborne infectious diseases on February 5, 2020. With the growing severity of the epidemic in the United States, the operation and maintenance guidelines for buildings were published on the ASHRAE website on March 24, 2020 [13]. On April 14, 2020, ASHRAE updated its position document on airborne infectious diseases [14]. On April 20, 2020, the ASHRAE website released two statements on the relationship between air-conditioning systems and the spread of COVID-19 viruses [8]. And on May 7, 2020, ASHRAE released “ASHRAE Offers COVID-19 Building Readiness/Reopening Guidance” [15]. REHVA released a document on air-conditioning system guidelines for COVID-19 on March 17, 2020, and updated it on April 3 [16], and REHVA proposed that it would continue to update the document if necessary. The Chartered Institution of Building Services Engineers (i.e. CIBSE) and the German Association of Indoor Ventilation Technologies (i.e. RLT), also issued suggestions on their official websites [[16], [17], [18]]. On March 30, 2020, Japan's Society of Heating, Air-Conditioning and Sanitary Engineers of Japan (SHASE) published “Q & A on Ventilation in the Control of SARS-CoV-2 Infection.” [19] On April 8, 2020, SHASE issued “Operation of Air-Conditioning Equipment and Other Facilities as SARS-CoV-2 Infectious Disease Control.” [20] The guidance documents from HVAC-related institutions provide suggestions and references for the management of air-conditioning and ventilation systems during the outbreak. This paper compares and analyzes guidelines regarding the transmission mechanism of SARS-CoV-2 and the countermeasures that need to be taken with respect to HVAC systems.
2. SARS-CoV-2 transmission mechanism
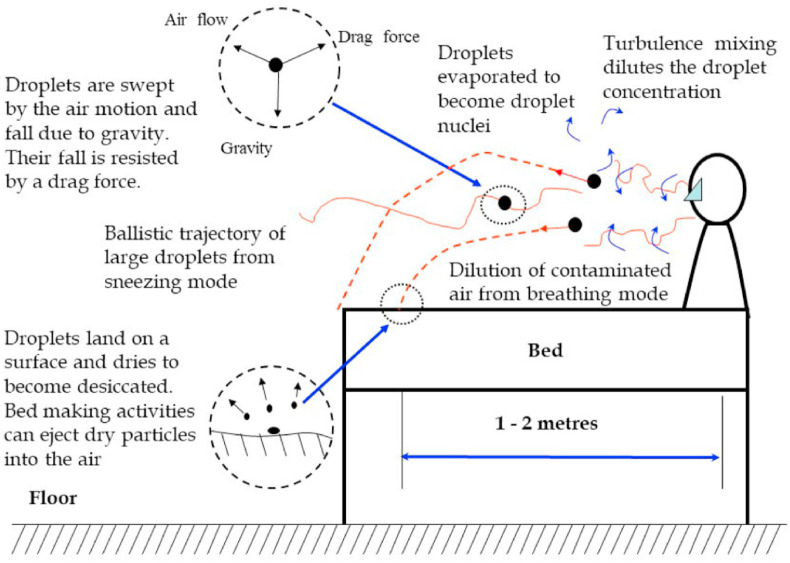
A respiratory infection can be transmitted through direct contact with surfaces contaminated by respiratory droplets, by inhaling airborne respiratory droplets, or by fecal-oral transmission. According to World Health Organization's (i.e. WHO) latest technical briefing [5], the two primary transmission routes are inhaling airborne droplets that contain viruses and contact. Up to now, there is no scientific evidence to support fecal-oral route transmission for SARS-CoV-2, but some evidence has shown that the SARS-CoV-2 virus may lead to intestinal infection and could be present in patients' feces. In specific situations, this can trigger airborne transmission, such as with SARS (e.g. Amoy Gardens [21]). ASHRAE explains the inhalation route of transmission (e.g., see Fig. 1 ): diseases have been found to have higher transmission rates when susceptible individuals are close to an infected individual (about 1–2 m). Such close contact permits droplet spray exposure and maximizes inhalation exposure to small particles and inspirable droplets. It takes only 2 s for droplets to evaporate and become more dry and smaller particles. The size of coronavirus particle ranges from 80 to 160 nm [22]. In general, a virus can survive for 3 h in the air and up to 2–3 days on indoor surfaces unless regular disinfection is implemented [23]. Studies have shown that SARS-CoV-2 is detected in the air [5]. Before a definitive conclusion can be made at as to whether SARS-CoV-2 can be transmitted by air, the HVAC system should be operated with caution. Droplets <1 μm have a high probability of transmission through ventilation ducts, since these smaller diameter droplets can remain suspended for long periods of time. In the United States, most air-conditioning systems are all-air systems, and an infection in one room is more likely to infect an entire floor, or even an entire building. There have been no reports so far of COVID-19 disease acquired because of spreading through the HVAC system.
Fig. 1.
Theoretical aerobiology of transmission of droplets and small airborne particles produced by an infected patient with an acute infection (from ASHRAE) [14].
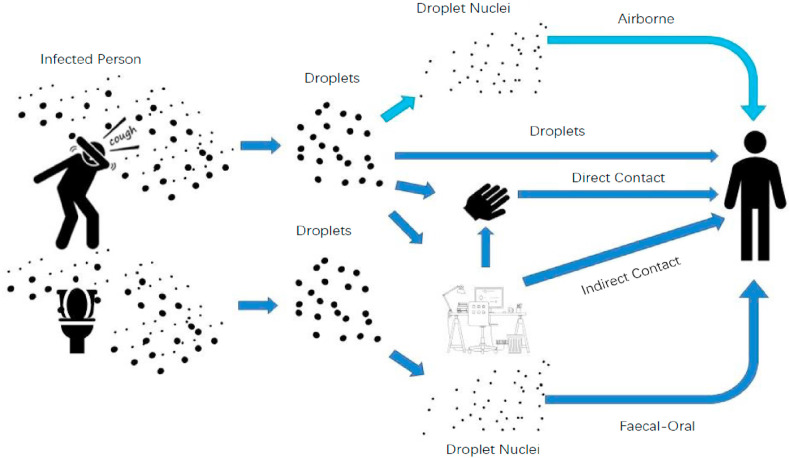
The main transmission routes of SARS-CoV-2 in a building, as established by REHVA, are shown in Fig. 2 . Dark blue arrows represent transmissions recognized by WHO, and REHVA and WHO have increasingly been paying more attention to fecal-oral transmission, because SARS-CoV-2 viruses have been detected in stool samples [24,25]. A light blue color shows transmission by inhalation of airborne droplets, which is known as a route from SARS-CoV-1 and other flu viruses. Current understanding of inhalation transmission of SARS-CoV-2 is that it is more probable when certain conditions are met (i.e., crowded indoor environments, with longer exposure times and minimal fresh air ventilation to dilute concentrations of airborne droplets).
Fig. 2.
Exposure mechanisms of SARS-CoV-2, SARS-CoV-1 and other flu viruses in buildings (from REHVA [16]).
Given that we do not yet fully understand SARS-CoV-2, REHVA proposes to adopt the principle of ALARA (As Low as Reasonably Achievable), especially in “hot spot” areas; this is in addition to the standard hygiene measures recommended by WHO.
SHASE's views on the transmission of the virus are similar to those of ASHRAE and REHVA. A study comparing SARS-CoV-2 with SARS-CoV-1, mentioned in the SHASE guide, shows that the survival characteristics of SARS-CoV-2 and SARS-CoV-1 are similar, and there is evidence that SARS-CoV-1 can be transmitted through air [26].
Overall, the views on SARS-CoV-2's transmission routes are consistent. Airborne transmission of SARS-CoV-2 is possible, according to the experience with previous similar viruses (e.g., SARS-CoV-1). Suggestions on the operation and maintenance of HVAC systems are given in the form of guidelines in almost all countries, to help reduce the spread of SARS-CoV-2.
3. Countermeasures using HVAC systems
HVAC engineers should propose solutions based on available information to ensure safe and healthy buildings. Since national guidelines mainly apply to public buildings (e.g. office buildings and commercial buildings) other than hospitals and health centers, the countermeasures for HVAC systems suggested in this paper primarily focus on public buildings.
3.1. Countermeasures suggested by ASHRAE
ASHRAE issued two statements on April 20, 2020 [8], officially opposing the advice not to run residential or commercial HVAC systems. Statement 1 pertains to airborne transmission of SARS-CoV-2/COVID-19. Studies show that inhalation transmission of airborne SARS-CoV-2 is sufficient likely; hence, airborne exposure to the virus should be controlled. Appropriate operation of HVAC systems can reduce airborne exposure. Statement 2 pertains to operating HVAC systems in such a way as to reduce SARS-CoV-2 exposure. Ventilation and filtration can reduce the airborne concentration of virus, and thus they can reduce the risk of airborne transmission. Moreover, people should not suffer from thermal stress in an unconditioned space by disabling the HVAC system. HVAC filters help to reduce virus transmission.
Guidelines for building operations during the COVID-19 pandemic were published in the ASHRAE Journal newsletter on March 24, 2020. Further, ASHRAE updated the “ASHRAE Position Document on Infectious Aerosols” on April 14, 2020. On May 7, 2020, ASHRAE released “ASHRAE Offers COVID-19 Building Readiness/Reopening Guidance” to mitigate potential health risks during reopening of buildings closed during the COVID-19 pandemic [27].
ASHRAE's guidance for building operations during the COVID-19 pandemic argues that HVAC systems play a minor role in infectious disease transmission, and the SARS-CoV-2 viruses spread primarily through droplets and contact in non-medical buildings. Maintaining social distance (1–2 m), surface cleaning and disinfection, handwashing, and other strategies of good hygiene are far more important than the strategies related to the HVAC system. The following actions related to HVAC systems are also recommended once the above basic measures are taken [13]:
-
1)
Increase the amount of outdoor air in ventilation systems, and open the minimum outdoor air dampers, as high as 100% if possible. Disable demand-controlled ventilation (i.e. DCV).
-
2)
Improve the level of the central air filter as much as possible, at least to the grade of MERV-13, and seal the edges of the filter to limit bypass. The minimum efficiency reporting value (i.e. MERV) for an air cleaner is based on three composite average particulate size efficiency from tests at the manufacturer's specified airflow rate (according to ASHRAE 52.2). The droplets <5 (droplet nuclei or aerosols) in diameter can be suspended in air over long distances and time. They are of great danger to help the transmission of SARS-CoV-2 [7]. The MERV-13 air cleaner can effectively mitigate the transmission of infectious aerosols, the efficiency of which is greater than 90% for particulates ranging 3.0–10.0 .
-
3)
Keep the system running longer hours; if possible, keep the system running for 24 h a day, 7 days a week (7/24).
-
4)
Portable room air cleaners with HEPA filters are recommended.
-
5)
Ultraviolet germicidal irradiation (i.e. UVGI) is also recommended, particularly in some high-risk spaces such as waiting rooms, prisons, and shelters. Shielding is needed to protect occupants from radiation.
According to ASHRAE Position Document on Infectious Aerosols [14], varying approaches should be adopted according to the facility type. For healthcare facilities, there are standards in ventilation design to mitigate airborne transmission of infectious diseases (ASHRAE 2013, 2017a, 2019a; FGI 2010). For other types of buildings, general ventilation and air quality requirements are given by ASHRAE in ANSI/ASHRAE Standards 62.1–2019, ANSI/ASHRAE Standards 62.2–2019 and ANSI/ASHRAE/ASHE Standard 170–2017.
The strategies recommended by the ASHRAE position document mainly include dilution and extraction ventilation, pressurization, airflow distribution and optimization, mechanical filtration, UVGI, and humidity control.
3.1.1. Ventilation and air-cleaning strategies
Ventilation with effective airflow patterns is the most important infectious disease control strategy [28], by diluting the indoor air around the source and removing the infectious agents. Many buildings are completely or partially naturally ventilated. These strategies are associated with both risks and benefits. On the one hand, the airflow rate and quality of outdoor air in those buildings are variable and unpredictable, resulting in different air distribution patterns, thus greatly reducing the ability to actively manage risk in these buildings. On the other hand, the rational use of natural ventilation can reduce the risk of infectious aerosols.
Pressure differentials between zones in the building should be controlled so that air flows from safe areas to unsafe areas, from personal use areas to public areas, such as from anterooms to airborne infection isolation rooms (i.e. AIIRs). HEPA filters are recommended. HEPA filters in centralized air-conditioning systems can reduce the risk of cross-infection due to the supply of recirculated air in areas sharing the same central HVAC system. HEPA filters in a single room can significantly reduce the concentration of infectious aerosol as long as they are appropriately sized and have sufficient particulate removal efficiencies.
ASHRAE argues that the entire ultraviolet (i.e. UV) spectrum can kill or inactivate microorganisms, while UV-C (ultraviolet with the wavelengths from 200 to 280 nm) provides the best effect, with 265 nm being the optimum wavelength. It does not penetrate deeply into human tissues but can penetrate the outermost layers of the eyes and skin, with the eyes being the most vulnerable. Therefore, when UVGI lamps are used, shielding is required to protect the eyes and skin. The US Centers for Disease Control and Prevention (i.e. CDC) also agrees that UVGI can help reduce the risk of virus transmission [29]. It is recommended to adopt personalized-air-supply and local-exhaust or all-fresh-air operation, and to set HEPA filters or UVGI in the occupant's breathing zone.
3.1.2. Temperature and humidity
The research carried out by Derby and Taylor et al. suggests that controlling the relative humidity reduces the transmission of certain airborne infectious organisms [30,31],including some strains of influenza viruses. Mousavi et al. reported that the most unfavorable survival condition for microorganisms is a relative humidity between 40% and 60% [32]. Studies have shown that a relative humidity below 40% can increase infections associating with three factors [32]. First, the droplets evaporate and become droplet nuclei quickly in a dry environment. Those small virus particles remain suspended in air and can travel great distances. Second, many viruses and bacteria have increased viability in dry conditions [33,34]. Finally, mucus membrane barriers and other components of the human immune system will be impaired when the ambient relative humidity falls below 40% [35]. Temperature and humidity can influence the stability of SARS-CoV-2. A study shows the virus is highly stable at 4 °C, but sensitive to heat [36]. Therefore, controlling the temperature and humidity is beneficial for controlling airborne transmission of the virus. The temperature and relative humidity setpoint in a building should be carefully considered on a case-by-case basis.
ASHRAE requires that all buildings strictly implement the latest published standards and guidelines. ASHRAE also suggests that the design and construction team, including HVAC designers, should engage in an integrated design process to consider the appropriate infection control strategies in the early stages of design, especially buildings with a higher risk of transmission.
Recommendations in building readiness and reopening guidance offered by ASHRAE mainly include the followings [27]:
-
1)
Create the strategic plan prior to opening a building, including measures to make occupants feel safer, ensuring supply chain for critical items such as filters and communication plans for building support and safety measures for occupants.
-
2)
Operate HVAC related devices including exhaust fan and outside air damper to provide flushing 2 h before and post occupancies.
-
3)
Keep the system running on minimum outdoor air when the building is unoccupied.
-
4)
Run garage exhaust 2 h before occupancy.
More specific recommendations for reopening buildings are outlined in the frequently asked questions section of ASHRAE's COVID-19 Resources webpage [37].
3.2. Countermeasures suggested by REHVA
REHVA updated the COVID-19 guidance document on April 3 with seven revisions and additions, including the virus transmission mechanism, ventilation equipment operation, virus viability in different temperature and humidity conditions, and operation of heat recovery equipment, and summarized 14 practical measures for building services operation [16]. The recommendation from REHVA can be summarized in the following aspects.
3.2.1. Outdoor air and ventilation strategies
The key to mitigate the airborne transmission of SARS-CoV-2 in buildings is secure ventilation of spaces with outdoor air. REHVA recommends supplying as much outdoor air as reasonably possible. Ensure the amount of fresh air supplied per person by maintaining or increasing social distancing (minimum physical distance 2–3 m between persons).
The windows should be opened regularly even in mechanically ventilated buildings. It is recommended to open windows for about 15 min before occupation of the room, especially a room that was occupied by others beforehand.
3.2.2. The operation of HVAC systems
During the outbreak, HVAC system shouldn't be operated as usual. It is recommended to run ventilation at the nominal speed for at least 2 h before the building usage time and at a lower speed 2 h after the building usage time. In DCV systems, the CO2 setpoint is suggested to be changed to 400 ppm, ensuring ventilation system operation at the nominal speed. It is not recommended to turn ventilation off at night and during weekends; instead, the system should be kept running at a lower speed. In buildings that have been vacated due to the outbreak, such as office buildings and schools, it is also not recommended to turn the ventilation system off, but to keep the system running continuously at a lower speed, so that the virus in the building can be removed from the building with limited energy penalties. For the toilet ventilation system, it is recommended to keep running for 24 h a day, 7 days a week to avoid the fecal-oral transmission route.
As for the operation of terminal devices, air handling units with recirculation are recommended to switch to 100% outdoor air, even some equipped with return air filters, as virus particles in return ducts can re-enter a building even when centralized air handling units are equipped with recirculation filters. The return air filters usually do not meet HEPA standards and are usually unable to filter virus particles effectively. The fan coils should be turned off or operated continuously. The fan coils working with circulation should be turned off to avoid resuspension of virus particles in the room. If it is impossible to turn the fan coils off, it is recommended to operate the fans continuously to prevent resuspension of viruses that were deposited on the filter when fans are turned on again.
3.2.3. Temperature and humidity setpoint
It is not recommended to change the heating, cooling, and relative humidity setpoints. Chin et al. found that SARS-CoV-2 is highly stable for 14 days at 4 °C. To inactivate the virus, 37 °C for one day and 56 °C for 30 min were needed [36]. The high viability of SARS-CoV-2 has been tested by van Doremalen et al. at a typical indoor temperature of 21–23 °C and a relative humidity of 65% [23]. It appears that the viability of SARS-CoV-2 will not be reduced significantly in moderate humidity (40–60%), according to the studies. However, the nasal chambers and mucous membranes of human beings are more sensitive to infections at a very low relative humidity range of 10–20% [38]. However, the indoor relative humidity in the forthcoming climatic conditions in Europe will be higher than 30% without humidification. Most importantly, humidification is not a method for reducing the viability of SARS-CoV-2.
3.2.4. Filters and air cleaning
REHVA believes that filters in central outdoor air and extract air have low efficiency and can filter only large particulate matter, but the filters should be replaced and maintained as usual according to the maintenance schedule, to prevent filter blocking, which would reduce the supply airflow rate. For air cleaning, REHVA considers cleaning with HEPA filters to be effective, but the airflow through air cleaners is often limited (due to noise and fan size). Hence, it is recommended to locate the air-cleaning device close to the breathing zone. Special UV cleaning equipment installed for the supply air or room air treatment is also effective.
3.2.5. Heat recovery equipment
For heat recovery equipment, it is recommended to inspect the devices including setting the pressure difference measurement to make sure that leakages are under control. The leakage rate of properly operating rotary heat exchangers is in the range 1–2%. For existing systems, heat exchangers with leakage below 5% are acceptable. This can be compensated by increasing the amount of outdoor air ventilation. However, if return air fans have been mounted in those systems, the pressure of the exhaust air may be higher than the supply air side. The leakage rate will then increase to 20% or so, which is not acceptable. Because the air leakage rate has nothing to do with the rotation speed of the rotor, there is no need to switch the rotors off. As the leakage rate is higher at a low airflow rate, it is suggested to operate with an increased ventilation rate.
3.2.6. Other strategies
To be on the safe side, REHVA recommends to wear masks, gloves‚ and other respiratory protection when regular filter replacement and maintenance work is being performed.
To maintain the proper pressure differential, REHVA recommends not to open windows in toilets. According to the experience in Hong Kong (Amoy Garden), during the SARS 2002–2003 outbreak [21], the virus spreads through open connected sewage pipes; therefore, it is important to avoid dried-out water seals in floors and other sanitary devices by adding water regularly (every 3 weeks depending on the weather). And REHVA recommends to close the lid when flushing toilets.
Besides, REHVA release two system specific guidance documents on fan coils operation in case recirculation can't be avoided and on measures to minimize air-leakages across rotary heat exchangers.
As members of REHVA, CIBSE and RLT have supported the recommendations in the REHVA guidance. CIBSE stressed the importance of ventilation and outdoor air. But in-duct UV-C devices are not recommended by CIBSE unless it is used to decontaminate air that is recirculated. Devices that emit ozone or other potentially hazardous by-products are also not recommended in occupied spaces [16,18]. RLT believes the SARS-CoV-2 will not spread through HVAC systems. On the contrary, HVAC systems help dilution of the possible viral load in a building. The importance of proper operation of HVAC systems and maintenance of pressure differentials between different zones are stressed by RLT [17].
3.3. Countermeasures suggested by SHASE
The SHASE's recommendations regarding operation of air-conditioning equipment and other facilities as SARS-CoV-2 infectious disease control are as follows.
3.3.1. Outdoor air and ventilation strategies
SHASE recommends to open the outer window regularly to increase outdoor air even if the ventilation systems are on, while ensuring thermal comfort and no draft, because 95% of the indoor air will be replaced when the outdoor air is three times the room volume.
For houses and small buildings, the ventilation systems should be kept on and supply as much outdoor air as possible. For centralized air-conditioning mainly in large buildings, as a general principle, it is recommended to increase the opening of the outdoor air damper and exhaust air damper to as high as 100% if possible. If the airflow is inverter controlled, the current value of both supply fan inverter and exhaust fans inverter should be raised, and the automatic control of the outdoor air should be removed.
3.3.2. The operation of HVAC systems
It is recommended to lower the CO2 setpoint. It is also recommended to increase the running time of air-conditioning equipment, running it continuously for 24 h if possible.
The exhaust system of the toilet should be kept running continuously. In addition, to ensure negative pressure in the toilet, the toilet window should be kept closed.
3.3.3. Temperature and humidity setpoint
According to WHO, the SARS-CoV-2 virus can infect any community, not only in dry and cold areas, but also in hot and humid areas such as Guangxi Zhuang Autonomous Region and Singapore [39]. However, in a low-temperature environment, the drying of the oral mucous membrane in humans decreases its defensive efficacy; therefore, in addition to ensuring the necessary amount of ventilation (30 m3/h per person), the temperature should be controlled between 17 and 28 °C, and the relative humidity should be controlled between 40 and 70%.
3.3.4. Filters and air cleaning
For a system with 100% outdoor air, the filter can be operated as usual. For return air operation, it is recommended to check the differential pressure of the filter more often and replace the filter sooner than usual.
As for air cleaner, not all air cleaners can filter out the virus, and the purification efficiency is also related to the volume of air. The air cleaner should be selected considering the volume of the target space. Air cleaners are effective as auxiliary devices. However, the effect of ventilation on reducing the concentration of viruses is more significant.
3.3.5. Heat recovery equipment
For the static total heat exchanger, the risk of virus leakage through the heat exchanger is small, as low as approximately 5%. Therefore, it can be operated in heat exchange mode. The manual recommends operating it with a large effective ventilation volume. When buildings use a merged drainage system to handle drainage, it is also recommended to install a check valve for the airflow in the drainpipe of the indoor unit.
For the rotary type, if a purge sector is set and the pressure balance is proper (return air pressure < supply air pressure), the risk of virus entry is acceptable. Therefore, it is recommended to operate with a large effective ventilation volume, while checking/adjusting the operation status as necessary.
3.3.6. Other strategies
The toilet lid should be closed while flushing the toilet. The integrity of the water seal should be checked regularly.
3.4. Countermeasures by China
Several institutions and societies in China have issued recommendations for the usage of air-conditioning during the COVID-19 pandemic, and the various recommendations from different Chinese institutions are basically the same. It is considered that increasing the outdoor air rate is one of the most effective means of preventing virus from transmitting through air. Specific recommendations for non-medical buildings are mainly as follows.
3.4.1. Ventilation strategies
The recommendations differ depending on the conditions prevailing in the rooms. For rooms with openable exterior windows, such windows should be opened as much as possible. For rooms without exterior windows and exhaust ventilation, two-way energy-saving ventilation machines should be installed to meet the need for ventilation. For rooms with a centralized outdoor air system and floor-centralized exhaust system, it is recommended that the doors remain open (or blinds can be set up in the door). Alternatively, a mechanical exhaust fan can be set up on the partition wall to ensure that the total exhaust volume of the floor-centralized exhaust system is not less than 70% of the design outdoor air volume. For rooms with a centralized outdoor air system but without a floor-centralized exhaust system, addition of a mechanical exhaust system is a reasonable option; or with the consent of the fire department, a fire anti-smoke exhaust system could be used as a centralized exhaust system.
When ventilation is insufficient, the exhaust system should be turned on or a portable room air cleaner with a HEPA filter should be added. Air-conditioning and mechanical ventilation systems should be turned on in advance and closed later.
3.4.2. Outdoor air and the operation of HVAC systems
The amount of outdoor air in the air-conditioning system is recommended to be increased as much as possible. For a centralized air-conditioning system, if the system is shared by multiple areas, the system should be operated with 100% outdoor air. If recirculated air is necessary, the ratio of outdoor air should be greater than 40%, and the system must be equipped with a return air filter (at least F7 grade, a level of filters raising by the European Committee for Standardization at EN779, the efficiency of which is greater than 65% for particles range 1.0–10.0 ) [12]. The quality of outdoor air should be ensured in the fan coil with the outdoor air system. Rooms without an outdoor air system and openable outside window should be discontinued. If “suspected cases” are found in the building, all the convective terminals (fan coils, etc.) should be shut down. In the operation of the air-conditioning system, the air supply temperature in heating mode is recommended to be increased, and in cooling mode, it is recommended to be decreased [40].
3.4.3. Filters and air cleaning
The filter in the HVAC system should be cleaned and replaced as usual. For office buildings, “chemical disinfection” should not be used in air-conditioned rooms and air-conditioning plant rooms. UV devices should not be installed in the air-conditioning system. During working hours, the indoor air cleaner should be operated.
3.4.4. Heat recovery equipment
Indirect heat exchangers and other heat exchangers that are not associated with the risk of mixing outdoor air and exhaust air can operate as usual. Rotary heat exchangers are not recommended to be used [40].
3.4.5. Pressure differentials between zones
The dining room should be separated from the kitchen, and the pressure in the kitchen should be slightly higher than that in the other areas. To maintain the positive pressure in the kitchen, the pressurized ventilator should be turned on while the kitchen exhaust fume fan runs. The exhaust systems of the toilets, sewage rooms, etc., are recommended to operate continuously to maintain negative pressure [40].
3.4.6. Other strategies
For the maintaining of the HVAC system, regular inspection and cleaning of the system should be carried out. The position of the outdoor air vents should be checked to ensure the quality of the outdoor air, to avoid outdoor air and exhaust air short circuit.
For the water system, it is recommended to check whether the water seals of each drainage, wastewater, medium water, and condensate system, and of the drainage apparatus, are effective. Keep the uplift ventilation pipe in the sewage system unobstructed, and set up silver ions, the photocatalytic oxidation sterilizer, and other equipment in the supply water pipe to ensure the safety of the water system.
4. Comparison and discussion
Airborne route and bad use of ventilation systems are non-negligible factors in SARS-CoV-2 transmission [3]. Various HVAC-related organizations and societies around the globe have issued guidelines in response to the coronavirus disease (COVID-19). But so far, the understanding of the transmission route and the characteristic of SARS-CoV-2 is incomplete, those guidelines are constantly being updated. Reviewing and comparing the countermeasures from different guidelines are of great benefit for guidelines updating. It also helps to implement reasonable countermeasures, rapidly respond to the outbreak and carry out further studies related to SARS-CoV-2.
The main countermeasures to mitigate the risk of the indoor transmission of SARS-CoV-2 issued by different guidelines are shown by Table A.1 in appendix A.
Guidelines or documents released in different countries exhibit commonalities regarding the transmission mechanism of COVID-19 in buildings. Air-conditioning and ventilation systems could minimize the airborne transmission of viruses. In regard to the operation of the HVAC system, the specific content in the guidelines varies slightly.
4.1. Operation of HVAC systems
As for the operation of the HVAC system, all the guidelines or documents mentioned above emphasize the importance of increasing the outdoor air ratio and ventilation. They all agree that the ventilation system should operate before the room is occupied, and that it should operate for as long as possible. People should open windows as much as possible for ventilation. Moreover, REHVA suggests that the setpoint of CO2 concentration should be decreased to 400 PPM, and SHASE also suggests that the CO2 concentration setpoint should be decreased. However, there is no agreement as to how much ventilation can effectively reduce the risk of infection.
Various suggestions have been made about the operation of different types of air-conditioning systems. For all-air systems, all suggest fully outdoor air operations, if possible. For fan coils with a dedicated outdoor air system, REHVA suggests that the return airflow should be stopped to avoid resuspension from the virus due to convection, while the Chinese guidelines suggest stopping all convection equipment, including fan coils, when suspected patients are in the room. ASHRAE also recommends increasing the filter level in the air-conditioning system to MERV-13. Other guidelines suggest that the filters used in the normal operation and maintenance of air-conditioning systems should be sufficient, and no pipe cleaning is required.
4.2. Operation of air cleaners
For room air cleaners, HEPA filters are effective for controlling the spread of viruses. Both REHVA and SHASE guidelines mention that most air cleaners recirculate a limited amount of air. ASHRAE and REHVA both believe that ultraviolet radiation can effectively inactivate viruses. ASHRAE suggests that ultraviolet sterilization irradiation equipment be used in all buildings, while REHVA believes that it is more appropriate to use it in medical buildings. The Architectural Society of China states that it is not appropriate to install UV lamps in air-conditioning and ventilation systems for office buildings without a firm basis or supporting medical opinion.
4.3. Pressure differentials of areas
All guidelines agree that the principle is to ensure airflow from areas with high cleanliness to areas with low cleanliness. All the guidelines state that the exhaust system should be kept running and that the outer windows should be closed to ensure negative pressure in the toilet. The Chinese guidelines also mention that a slight positive pressure should be maintained in the kitchen.
4.4. Operation of heat recovery devices
For heat recovery devices, the guidelines in the updated REHVA guide are consistent with those of SHASE. Both agree that if the return air pressure is lower than the supply air pressure, the mixing amount of return air caused by the heat exchanger is acceptable, and that increasing the supply air volume can further reduce the mixing amount. The current guidelines issued by China state that heat recovery devices except indirect heat exchangers should be closed and bypassed.
4.5. Temperature and humidity setpoint
For indoor temperature and humidity setpoints, the ASHRAE recommendations depend on the prevailing situation and building conditions. According to REHVA, it is not necessary to adjust the temperature and humidity setpoints in spring. SHASE recommends that the temperature setpoint should be between 17 and 28 °C, and that the relative humidity setpoint should be between 40 and 70%. However, the Chinese guidelines only recommend that the air-conditioning system should increase the supply air temperature during the heating season and reduce the supply air temperature during the cooling season.
In all guidelines mentioned above, all guidelines emphasize the importance of ventilation which can effectively decrease the concentration of droplets containing virus. Both natural ventilation and mechanical ventilation should be enhanced as much as possible. However, the specific ventilation rate that can eliminate the risk of transmission of airborne particulate matter is still unclear. The latest review on ventilation rates for minimizing infectious disease risk reports effects on health were seen for a wide range of outdoor ventilation rates from 6 to 40 L/s/person [41]. UV lamps and HEPA filters are also beneficial to decrease the virus concentration. It will take some time for the UV lamps to inactivate the virus, thus it is not recommended by China to install UV lamps to the duct. The air that air cleaner can handle is limited. It can be located close to the breathing zone as an auxiliary countermeasure. And to avoid resuspension of virus and transmission of SARS-CoV-2 by HVAC system, the recirculation sector is recommended to be switched off if possible.
It is controversial whether to change the setpoint of temperature and relative humidity in the air-conditioning system. To inactivate the virus, 37 °C for one day and 56 °C for 30 min were needed [36]. It is obviously impossible for people to stay in such a high-temperature environment for a long time. So, there is no need to change the temperature setpoint. As for relative humidity, the viability of SARS-CoV-2 will not decrease when the relative humidity is 40–60% [32]. However, studies have shown that relative humidity below 40% can increase infections [32].(elaborate in section 3.2.3). Thus, it is plausible that humidification is needed when the relative humidity is lower than 40%.
5. Conclusion and further work
5.1. Conclusion
This paper reviews and compares the countermeasures related to HVAC system to mitigate the transmission of SARS-CoV-2 in the building issued by different societies in several major countries and regions. HVAC system with proper operation could mitigate the transmission of SARS-CoV-2 in the building effectively. Those countermeasures mainly include the amount of outdoor air, the operation of the whole HVAC systems and different terminal devices (e.g. AHU), filters and air cleaning, the temperature and humidity setpoints of air conditioning, operation of heat recovery equipment. The conclusions are drawn as follow:
-
1)
Ventilation with sufficient outdoor air and effective airflow patterns is the most important strategy to mitigate the risk of transmission of SARS-CoV-2.
-
2)
The main commonly agreed countermeasures from different guidelines are listed as follow:
For outdoor air, it is recommended to supply as much outdoor air as possible. Open the outdoor air damper as high as 100% if possible.
For the operation of HVAC system, it is recommended that the running time of HVAC system should be increased. REHVA and ASHRAE both recommend open HVAC related devices 2 h before and after occupancies.
For air cleaning strategy, portable room air cleaners are recommended. It is crucial to maintain the filter regularly.
For air conditioning devices (e.g. AHU), disable the recirculation sector if possible.
It is also recommended to keep negative pressure in toilets and check the water seals regularly.
-
3)
The following countermeasures vary from different guidelines:
For the temperature and humidity setpoint of the air-conditioning system, the guideline issued by REHVA suggests there is no need to change it in the forthcoming climatic conditions in Europe while SHASE recommends to control the temperature between 17 and 28 °C and control the relative humidity between 40 and 70%.
For the operation of heat recovery equipment, if the leakage rate and pressure differential are reasonable, it can be operated in a particular mode while guidelines issued by China recommend all rotary heat exchangers should not be installed in the HVAC system.
5.2. Further work
It can be observed that most suggestions in these guidelines are roughly consistent with one another, except for a few conflicting details, which reflects the underlying uncertainty regarding the transmission of SARS-CoV-2.
-
1)
Further studies are needed to determine whether and in what condition SARS-CoV-2 can be spread by air and HVAC system in buildings.
-
2)
The specific ventilation rate that can eliminate the risk of transmission of airborne particulate matter remains to be studied.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
This work was supported by National Science & Technology Pillar Program during the thirteenth Five-year Plan Period (2017YFB0903404). We thank ChuXuan Feng (TianYi High) and Evonne Xu (Campolindo High) for translating documents and evaluating infection risk in their study environments.
Appendix A.
Table A.1 comparison of the main strategies
| ASHRAE | REHVA | SHASE | Related Society of China | |
|---|---|---|---|---|
| Outdoor air |
|
|
|
|
| Operation of HVAC systems |
|
|
|
|
| Temperature and humidity setpoint |
|
|
|
|
| Pressure differential |
|
|
|
|
| Filters equipped in the HVAC system |
|
|
|
|
| Air cleaning |
|
|
|
|
| Heat recovery equipment |
|
|
|
|
| Others |
|
|
|
|
References
- 1.Qian Hua. Indoor transmission of SARS-CoV-2. https://www.medrxiv.org/content/10.1101/2020.04.04.20053058v1 April 07, 2020. Accessed September 18 2020. [DOI] [PubMed]
- 2.ECDC Heating, ventilation and air-conditioning systems in the context of COVID-19 2020. https://www.ecdc.europa.eu/sites/default/files/documents/Ventilation-in-the-context-of-COVID-19.pdf Accessed September, 19 2020.
- 3.Correia G. Airborne route and bad use of ventilation systems as non-negligible factors in SARS-CoV-2 transmission, Med. Hypotheses. 2020;141:5. doi: 10.1016/j.mehy.2020.109781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu J.Y. COVID-19 outbreak associated with air conditioning in restaurant, guangzhou, China. Emerg. Infect. Dis. 2020;26(7):1628–1631. doi: 10.3201/eid2607.200764. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO . 2020. Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations.https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations Accessed May, 9 2020. [Google Scholar]
- 6.Zhang S. Estimation of the reproductive number of novel coronavirus (COVID-19) and the probable outbreak size on the Diamond Princess cruise ship: a data-driven analysis. Int. J. Infect. Dis. 2020;93:201–204. doi: 10.1016/j.ijid.2020.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO Transmission of SARS-CoV-2: implications for infection prevention precautions. 2020. https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions Accessed September, 19 2020.
- 8.ASHRAE . 2020. ASHRAE Issues Statements on Relationship between COVID-19 and HVAC in Buildings.https://www.ashrae.org/about/news/2020/ashrae-issues-statements-on-relationship-between-covid-19-and-hvac-in-buildings Accessed May, 9 2020. [Google Scholar]
- 9.Xinhuanet, China Has Released Information on COVID-19 and Promoted International Cooperation on Epidemic Prevention and Control. 2020. http://www.nhc.gov.cn/wjw/xwdt/202004/ef0708c0e01f452492dbf6c418ef41a0.shtml Accessed May, 9 2020. [Google Scholar]
- 10.The Architectural Society of China . 2020. All Kinds of Guidance.http://www.chinaasc.org/news/kangjiyiqing/geleizhinan/list_311_1.html Accessed May, 9 2020. [Google Scholar]
- 11.The State Council of China . 2020. Guidelines for the Operation and Management of Air-Conditioning and Ventilation Systems in Office and Public Buildings during the New Pneumonia Epidemic.http://www.gov.cn/xinwen/2020-02/13/content_5478015.htm Accessed May, 9 2020. [Google Scholar]
- 12.The Chinese Association Of Refrigeration . 2020. Recommendations for the Safe Use of Air-Conditioning (Heating) Systems in Response to the COVID-19 Epidemic.http://www.car.org.cn/index.php?s=/articles_1348.html Accessed May, 9 2020. [Google Scholar]
- 13.Schoen Lawrence J. 2020. Guidance for Building Operations during the COVID-19 Pandemic.https://www.ashrae.org/news/ashraejournal/guidance-for-building-operations-during-the-covid-19-pandemic Accessed May, 9 2020. [Google Scholar]
- 14.ASHRAE . 2020. ASHRAE Position Document on Infectious Aerosols.https://www.ashrae.org/file%20library/about/position%20documents/pd_infectiousaerosols_2020 Accessed May, 9 2020. [Google Scholar]
- 15.ASHRAE . 2020. ASHRAE Offers COVID-19 Building Readiness/Reopening Guidance.https://www.ashrae.org/about/news/2020/ashrae-offers-covid-19-building-readiness-reopening-guidance Accessed May, 9 2020. [Google Scholar]
- 16.REHVA . 2020. REHVA COVID-19 Guidance Document.https://www.rehva.eu/fileadmin/user_upload/REHVA_COVID-19_guidance_document_ver2_20200403_1.pdf Accessed May, 9 2020. [Google Scholar]
- 17.RLT Pressemeldung. 2020. Betrieb von Lüftungs- und Klimaanlagen während der COVID-19-Pandemie.https://www.rlt-geraete.de/joomla/index.php/ct-menu-item-9/pressemeldungen Accessed May, 9 2020. [Google Scholar]
- 18.CIBSE . 2020. CORONAVIRUS COVID-19 AND HVAC SYSTEMS.http://www.cibse.org/coronavirus-(covid-19)/coronavirus-covid-19-and-hvac-systems Accessed May, 9 2020. [Google Scholar]
- 19.SHASE Q. 2020. A on Ventilation in the Control of SARS-CoV-2 Infection.http://www.shasej.org/recommendation/shase_COVID_ventilizationQ&A.pdf Accessed May, 9 2020. [Google Scholar]
- 20.SHASE Operation of air-conditioning equipment and other facilities as SARS-CoV-2 infectious disease control 2020. http://www.shasej.org/recommendation/Operation_of_air-conditioning_equipment_and_other_facilities20200407.pdf Accessed May, 9 2020.
- 21.Lee Shiu Hung. The SARS epidemic in Hong Kong: what lessons have we learned? J. R. Soc. Med. 2003;96(8):374. doi: 10.1258/jrsm.96.8.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Monto A.S. Medical reviews. Coronaviruses. Yale J. Biol. Med. 1974;47(4) 51-234. [PMC free article] [PubMed] [Google Scholar]
- 23.van Doremalen N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang Wei. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg. Microb. Infect. 2020;9(1):386–389. doi: 10.1080/22221751.2020.1729071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guan Wei-Jie. Clinical characteristics of 2019 novel coronavirus infection in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ignatius T.S. Yu. Evidence of airborne transmission of the severe acute respiratory syndrome virus. N. Engl. J. Med. 2004;350(17):1731–1739. doi: 10.1056/NEJMoa032867. [DOI] [PubMed] [Google Scholar]
- 27.ASHRAE . 2020. ASHRAE Offers COVID-19 Building Readiness/Reopening Guidance.https://www.ashrae.org/about/news/2020/ashrae-offers-covid-19-building-readiness-reopening-guidance Accessed June, 28 2020. [Google Scholar]
- 28.Morawska L. How can airborne transmission of COVID-19 indoors be minimised? Environ. Int. 2020;142:7. doi: 10.1016/j.envint.2020.105832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.CDC Environmental control for tuberculosis: basic upper-room ultraviolet germicidal irradiation guidelines for healthcare settings. 2009. www.cdc.gov/niosh/docs/2009-105/pdfs/2009-105.pdf Accessed May, 9 2020.
- 30.Derby M.M. Update of the scientific evidence for specifying lower limit relative humidity levels for comfort, health, and indoor environmental quality in occupied spaces (RP-1630) Sci. Technol. Built Environ. 2017;23(1):30–45. [Google Scholar]
- 31.Taylor S., Tasi M. Low indoor-air humidity in an assisted living facility is correlated with increased patient illness and cognitive decline. Indoor Air. 2018:1–8. [Google Scholar]
- 32.Mousavi Ehsan. Academic research to support facility guidelines Institute & ANSI/ASHRAE/ASHE standard 170. 2019. https://www.ashrae.org/file%20library/technical%20resources/covid-19/ashrae-d-co-rp3.pdf Accessed May, 9 2020.
- 33.Stone W. Microbes at surface-air interfaces: the metabolic harnessing of relative humidity, surface hygroscopicity, and oligotrophy for resilience. Front. Microbiol. 2016;7:1563. doi: 10.3389/fmicb.2016.01563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marcus C. de Goffau. Bacterial pleomorphism and competition in a relative humidity gradient. Environ. Microbiol. 2009;11(4):809–822. doi: 10.1111/j.1462-2920.2008.01802.x. [DOI] [PubMed] [Google Scholar]
- 35.Kudo Eriko. Low ambient humidity impairs barrier function and innate resistance against influenza infection. Proc. Natl. Acad. Sci. U. S. A. 2019;116(22):10905–10910. doi: 10.1073/pnas.1902840116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chin Alex W.H. Stability of SARS-CoV-2 in different environmental conditions. The Lancet. Microbe. 2020;1(1) doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.ASHRAE Frequently asked questions (FAQ) 2020. https://www.ashrae.org/technical-resources/frequently-asked-questions-faq Accessed May, 9 2020.
- 38.Salah B. Nasal mucociliary transport IN healthy-subjects IS slower when breathing dry air. Eur. Respir. J. 1988;1(9):852–855. [PubMed] [Google Scholar]
- 39.WHO . 2020. Coronavirus Disease (COVID-19) Advice for the Public: Mythbusters.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters Accessed May, 9 2020. [Google Scholar]
- 40.The Architectural Society of China . 2020. Guidance for Office Building Operations during the COVID-19 Pandemic.http://www.chinaasc.org/news/127036.html Accessed May, 9 2020. [Google Scholar]
- 41.Carrer Paolo. What does the scientific literature tell us about the ventilation-health relationship in public and residential buildings? Build. Environ. 2015;94:273–286. [Google Scholar]