ABSTRACT
Mongolia had an epidemic of measles in 2015–2016, even though more than 90% of the population have been vaccinated since 1997. This study aimed to examine the associations between unvaccinated proportion and measles incidence according to aimag. Mongolia has 21 provinces (aimag) with Ulaanbaatar as the capital city. Vaccination coverage between 1991 and 2014 and measles incidence according to aimag were obtained from the National Center for Communicable Diseases of Mongolia database. Accumulated unvaccinated proportion (AUP) among those aged 1 to 24 years in 2015 was estimated from the unvaccinated at the 1st dose of 1991 to 2014. From 1991 to 2014, unvaccinated proportion among those aged 1 to 24 years in the whole country has been reducing from 28.0% in 1991 to 1.8% in 2014. The AUP in 2015 varied from 2.7% (Selenge) to 21.8% (Govisumber). The incidence was remarkably higher in only two aimags with a large density of the unvaccinated aged 1 to 24 years (Ulaanbaatar and Darkhan-Uul) than in the other aimags. The incidence had no significant correlation with the AUP, although the correlation between the incidence and the density of unvaccinated aged 1 to 24 years was significant when the two aimags were included. In conclusion, the AUP between 2.7% and 21.8% had no correlation with the incidence according to aimags in Mongolia measles epidemic 2015–2016.
Key Words: measles, aimag, the accumulated unvaccinated proportion, Mongolia
INTRODUCTION
Measles may be potentially eliminable because “1) humans are the sole pathogen reservoir, 2) accurate diagnostic tests exist, and 3) an effective, practical intervention is available at a reasonable cost.”1 Annual incidence rate of measles had globally decreased by 75% from 146 to 36 per million population during 2000–2015. The annual death rate had also decreased by 79% from 651,600 to 134,200 during the corresponding period.2 However, measles outbreaks were recently reported in North America,3,4 South America,5 Europe,6,7 Africa,8 and Asia.9-11
Immunity against measles is acquired by infection and usually lasts throughout life,12 and the vaccination against measles is also effective.13 The World Health Organization (WHO) recommended a two-dose vaccination with a very high (>95%) coverage; the first dose during the first year of life and the second dose at preschool age depending on the country-specific factors.14 In many countries, measles vaccine is included in the country’s immunization program and is freely available to all.
In Mongolia, the incidence of measles was 125 per 10,000 population during 1960–1972. Expanded Program on Immunization (EPI) was introduced to Mongolia in 1962,15 but the measles vaccine was included in the EPI in 1973 with a one-dose measles-containing vaccine (MCV1). The two-dose vaccine (MCV2) was introduced in 1989 for children aged 8 months and children aged 1 year and 2 months.16 MCV2 was replaced in 2009 with a measles-mumps-rubella (MMR) vaccine, which was administered to children aged 9 months and 2 years. After the introduction of MCV2, measles cases decreased gradually during 1990–2002. However, three measles outbreaks were reported in 1992, 1995 and 2000–2002.17 Since no case was reported in Mongolia since 2011, the WHO Regional Office for the Western Pacific certified measles elimination in 2014.18 In March 2015, a measles case was reported in Ulaanbaatar city, followed by a large outbreak involving 53,737 cases during 2015–2016.19 The majority affected by measles outbreak were 1 to 24 years old; 14,813 (63.2%) cases in 2015 and 15,361 (50.8%) cases in 2016.20 It was stated that only 6.5% of all measles cases had vaccination history.20
According to WHO position paper 2017, the risk of measles outbreaks is determined by the rate of accumulation of susceptible people in the population. WHO suggests that programs should use available good quality data on population immunity (i.e. vaccination coverage, surveillance, serological studies) to monitor the accumulation of susceptible people and conduct follow-up campaigns in order to prevent an outbreak of measles. This approach has been found to be programmatically useful in preventing large outbreaks. Additionally, WHO advises to take a more extensive assessment of the accumulation of susceptible persons and undertake it at the subnational level in case of countries close to measles elimination.21
Several studies such as those on risk factors for measles virus infection among adults,19 epidemiological characteristics and trends of nationwide measles outbreak in Mongolia,17,20 Measles and Rubella Seroprevalence Survey Mongolia 2017,22 health system strengthening and measles elimination,23 healthcare associated measles after nationwide outbreak,24 and infant measles deaths during nationwide measles outbreak,25 were conducted on the measles outbreak 2015–2016 in Mongolia. However, there was no similar study conducted to analyze the association between accumulated unvaccinated proportion and measles outbreak 2015–2016 in Mongolia.
This study aimed to estimate the proportion of the unvaccinated among those aged less than 25 years in 2015 according to aimag based on the measles vaccine coverage in 1991–2014. Furthermore, the associations between the accumulated unvaccinated proportion (AUP) in 2015 and the incidence of measles in the epidemic in 2015–2016 were examined.
MATERIALS AND METHODS
Data sources
Mongolia has 22 provinces (aimags) including Ulaanbaatar, the capital that contained 46% of Mongolia’s population in 2015 (Fig. 1). The data of vaccination coverage during 1991–2014 and measles incidence according to aimag were obtained from the National Center for Communicable Diseases and Center for Health Development of Mongolia database. Although MCV2 started before 1991, the vaccination coverage of the second dose during 1991–2008 was not available because it was not registered in each aimag.
Fig. 1.
Map of Mongolia showing 22 provinces named aimag, including Ulaanbaatar
AUP among those aged 1 to 24 years in 2015 according to aimag was estimated using the data on the first dose of vaccination during 1991–2014 as follows; 1) summation of target children (STC) during 1991–2014, 2) summation of vaccinated children (SVC) during 1991–2014, and 3) calculation of (STC-SVC)/STC. The value was regarded as AUP among those aged 1 to 24 years in 2015.
Statistical analysis
The associations between the estimated AUP and incidence of measles in the epidemic during 2015–2016 were examined with Pearson’s correlation coefficients. P values less than 0.05 were considered statistically significant. The analyses were performed using the SPSS version 24.
Ethical considerations
The study protocol was approved by the Bio Medical Science Ethical Inspection Committee of Ministry of Health, Mongolia (Ref. no: 01/2017). The permission to use official statistical data of measles reported cases from the national surveillance database was obtained from the National Center for Communicable Diseases, Ministry of Health, Mongolia (Ref. no:50/2018). Anonymous data were used for the analysis.
RESULTS
Proportion of the unvaccinated
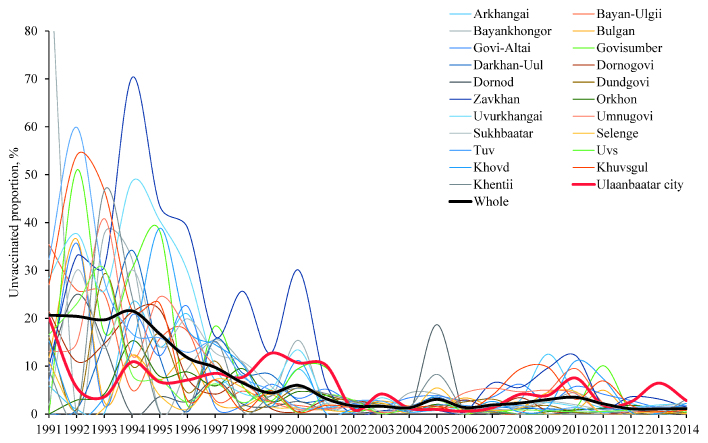
The proportions of the unvaccinated subjects of Mongolian mandatory measles vaccination scheduled at 9th month during 1991–2014 are shown according to aimag in Fig. 2 and Supplementary Table 1. Since Govisumber, Darkhan-Uul and Orkhon aimags were newly established in 1992, there were no data for the unvaccinated proportion for those aimags in 1991. Before 1992, Govisumber was a part of Dornogovi aimag, and Darkhan-Uul and Orkhon were cities in Selenge and Bulgan aimags, respectively. Data on Bayankhongor aimag in 1991 was not adopted by the government because of the unreliableness.
Fig. 2.
Trends in the unvaccinated proportion in the first dose of measles vaccine by aimag in Mongolia from 1991 to 2014
As shown in Fig. 2, the unvaccinated proportion of the first dose was relatively high in Bayan-Ulgii (35.4%), Tuv (32.3%), Uvurkhangai (28.4%), Khuvsgul (27.0%), and Dornogovi (21.4%) aimags, while it was low in Sukhbaatar (1.9%), Arkhangai (5.9%), and Govi-Altai (6.9%). The first dose of unvaccinated proportion of children throughout Mongolia was reduced by nearly 15 times from 28.0% in 1991 to 1.8% in 2014. In Ulaanbaatar, the unvaccinated proportion was reduced by 7 times from 20.1% in 1991 to 2.8 % in 2014. The reduction was achieved around 2002 (98.4%), although the unvaccinated proportion was slightly increased in some aimags after 2002.
The AUP among those aged 1 to 24 years in 2015 is shown in Table 1. Govisumber with the smallest target children (7,912 children) had the highest AUP (21.8%), followed by Bayankhongor (20.3%) and Zavkhan (18.6%) aimags. The AUP was low in Selenge (2.7%), Orkhon (3.6%), and Dornod (4.4%) aimags. The AUP in whole country was 8.7%.
Table 1.
Accumulated unvaccinated proportion (AUP) among those aged 1 to 24 years in 2015
| Summation of target children | Summation of vaccinated children | AUP | Measles cases among 1 to 24 years in 2015–16 | Cases / 1,000 target children | Incidence for all population per 1,000* | Population density per 1 km2 in 2015 | |
| Arkhangai | 50,730 | 47,914 | 5.6% | 479 | 9.4 | 11.9 | 1.7 |
| Bayan-Ulgii | 64,184 | 59,302 | 7.6% | 358 | 5.6 | 6.8 | 2.2 |
| Bayankhongor | 51,315 | 40,877 | 20.3% | 409 | 8.0 | 12.7 | 0.7 |
| Bulgan | 27,399 | 25,863 | 5.6% | 145 | 5.3 | 4.6 | 1.2 |
| Govi-Altai | 33,856 | 31,317 | 7.5% | 474 | 14.0 | 12.0 | 0.4 |
| Govisumber | 7,912 | 6,188 | 21.8% | 110 | 13.9 | 11.3 | 3.0 |
| Darkhan-Uul | 44,066 | 39,656 | 10.0% | 1,421 | 32.2 | 24.1 | 30.6 |
| Dornogovi | 26,575 | 25,180 | 5.2% | 492 | 18.5 | 18.6 | 0.6 |
| Dornod | 38,253 | 36,558 | 4.4% | 230 | 6.0 | 5.7 | 0.6 |
| Dundgovi | 24,971 | 23,486 | 5.9% | 225 | 9.0 | 10.7 | 0.6 |
| Zavkhan | 44,201 | 35,970 | 18.6% | 117 | 2.6 | 3.4 | 0.8 |
| Orkhon | 37,286 | 35,936 | 3.6% | 468 | 12.6 | 10.4 | 125.9 |
| Uvurkhangai | 60,604 | 53,067 | 12.4% | 745 | 12.3 | 14.4 | 1.8 |
| Umnugovi | 27,008 | 25,035 | 7.3% | 328 | 12.1 | 13.2 | 0.4 |
| Sukhbaatar | 28,930 | 26,736 | 7.6% | 283 | 9.8 | 9.0 | 0.7 |
| Selenge | 44,513 | 43,320 | 2.7% | 668 | 15.0 | 12.3 | 2.6 |
| Tuv | 40,138 | 35,368 | 11.9% | 452 | 11.3 | 9.6 | 1.2 |
| Uvs | 55,093 | 51,782 | 6.0% | 312 | 5.7 | 8.6 | 1.2 |
| Khovd | 52,180 | 48,741 | 6.6% | 445 | 8.5 | 10.6 | 1.1 |
| Khuvsgul | 63,537 | 56,428 | 11.2% | 363 | 5.7 | 8.0 | 1.3 |
| Khentii | 37,242 | 35,285 | 5.3% | 492 | 13.2 | 13.9 | 0.9 |
| Ulaanbaatar | 418,460 | 396,556 | 5.2% | 21,148 | 50.5 | 26.3 | 297.1 |
| Total | 1,278,453 | 1,180,565 | 8.7% | 30,164 | 23.6 | 18.0 | 2.0 |
* Reported in reference 20
Outbreak in 2015–2016 among those aged 1 to 24 years
Among 53,737 measles cases during 2015–2016, 30,164 (56.1%) individuals were reportedly 1 to 24 years old. The city of Ulaanbaatar had the largest number of cases among those aged 1 to 24 years (21,148 cases), followed by Darkhan-Uul (1,421 cases), Uvurkhangai (745 cases), Selenge (668 cases), Dornogovi (492 cases), and Orkhon (468 cases) aimags. Although there was a large population movement from rural area to urban area since 1991, the measles cases were divided by summation of target children during 1991–2014. The figure was high in both Ulaanbaatar (50.5 per 1,000) and Darkhan-Uul (32.2 per 1,000). For reference, the incidence of measles among all population reported by Orsoo et al (2019)20 and population density in 2015 are listed in Table 1. Ulaanbaatar, Darkhan-Uul, and Orkhon aimag were the most populated areas.
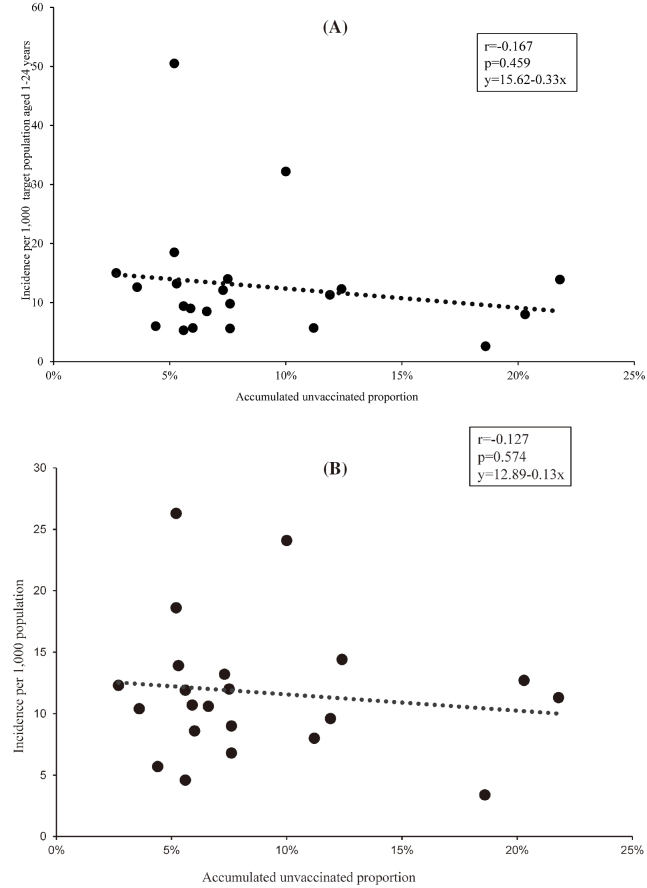
Correlations between AUP among those aged 1 to 24 years in 2015 and measles incidence in 2015–2016
Fig. 3 demonstrated the correlations between the AUP and measles incidence during outbreak 2015–2016. There were no significant correlations between the AUP and measles incidence in 2015–2016 in both among those aged 1 to 24 years (r=–0.167 and p=0.459 in Fig. 3 (A)) and whole population (r=–0.127 and p=0.574 in Fig. 3 (B)). Although the AUP was relatively low in Ulaanbaatar (5.2%) and Darkhan-Uul (10.0%), the incidence of measles was higher in Ulaanbaatar (50.5 and 26.3 per 1,000, respectively) and Darkhan-Uul (32.2 and 24.1 per 1,000, respectively). Similarly, the incidence among children aged 1 to 4 years, age group effectively protected by recent vaccination, had no correlation with the AUP (r=0.077 and p=0.733).
Fig. 3.
Correlations between accumulated unvaccinated proportion among those aged 1 to 24 years in 2015 and measles incidence per 1,000 population in 2015–2016 according to aimag: (A) Incidence among those aged 1 to 24 years, (B) Incidence among the whole population.
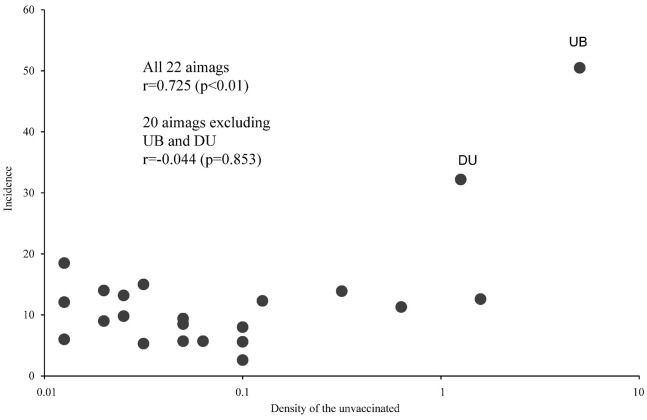
Fig. 4 shows the correlation between the unvaccinated density per 1 km2 of those aged 1 to 24 years in a logarithmic scale and the incidence among those aged 1 to 24 years. The correlation was significant when all 22 aimags were included (r=0.725, p<0.01), while there was no correlation when Ulaanbatar and Darkhan-Uul were removed (r=–0.044, p=0.853).
Fig. 4.
Correlation between density of the unvaccinated aged 1 to 24 years per 1 km2 and measles incidence per 1,000 population among those aged 1 to 24 years; UB: Ulaanbaatar, DU: Darkhan-Uul
DISCUSSION
This is the first report in English on the trends in measles vaccination coverage between 1991–2014 according to aimag collected by Mongolian government. The method to estimate the AUP is simple, but it has been rarely applied for the actual epidemic.
Measles outbreak might be explained by the accumulation of susceptible person and/or their low immunity status. The increase in the susceptible individuals can lead to a measles outbreak, highlighting the importance of a herd immunity.20 The trends in the measles vaccination coverage showed that the unvaccinated proportion among the target population was relatively large before 2001, although some aimags had a slightly large unvaccinated proportion possibly due to poor supply of measles vaccine, disruption of vaccine cold chain, absence of registered children moving to another aimag, etc. It indicated that the proportion of children sensitive to measles were high among those aged 15 years or older. However, our examination suggested that the incidence might not be influenced by the range of 2.7% to 21.8% of the AUP among those aged 1 to 24 years.
Although vaccination policies differed slightly among Western Pacific and Asian countries, most of the countries adopted the MCV1 and MCV2 policy including Republic of Korea, Malaysia, Japan, Australia, Singapore and Mongolia. Vaccination coverage estimates were reported to be high in these countries and near to 100% in neighboring countries such as China and Russia as well. Yet, these countries experienced challenging outbreaks with successful vaccination coverage system.26-29
A total of 1,180,565 (92.3%) children were vaccinated and 97,888 (7.3%) were unvaccinated among 1,278,453 target children during 1991–2014. In order to reduce the unvaccinated children, periodic nationwide measles supplemental immunization activities (SIAs) were implemented 5 times in 1994, 1996, 2000, 2007 and 2012 for the target age groups.19 The vaccination was administered to 162,751 (74.6%) children of 218,034 target children in 1994, 541,441 (97.5%) of 554,968 target children in 1996, 353,389 (96.1%) of 674,38 target children in 2000, 133,648 (96.9%) of 137,790 target children in 2007, and 522,429 (96.1%) of 560,592 target children in 2012. SIAs should be applied based on precise information from monitoring the susceptible people to prevent an outbreak of measles.21 Information on the seropositivity against measles among the target children at each SIA was limited.
We assumed that the incidence in each aimag was strongly influenced by the proportion of the unvaccinated. However, the plots in Fig. 3 demonstrated that there was no significant correlation between the AUP and the incidence. There might be two possibilities; 1) the estimated AUP did not reflect the actual proportion of susceptible children due to the problems stated in the following limitations, and 2) the AUP with the range in this study did not influence the incidence according to aimag. Unvaccinated population density of those aged 1 to 24 years had a significant correlation (p<0.01) with measles incidence among those aged 1 to 24 years. If two highly populated aimags (Ulaanbaatar and Darkhan-Uul), the correlation was not observed (r=–0.044, p=0.853). Measles epidemics are more likely to occur in urban areas because of the close contact. Furthermore, it is speculated that a substantial number of the young adult population, who moved to urban areas, might be susceptible to measles due to vaccine failure. These factors may have contributed to a high incidence of measles in Ulaanbaatar and Darkhan-Uul with the relatively low AUP.
There are several limitations in this study. The first was the inaccuracy of the statistical data on the vaccine coverage and measles incidence. Since these were the only available nationwide data, there was no alternative to estimate the coverage and incidence. The second was the movement of people to other areas, mainly from the rural areas to urban areas during 1991–2015. For example, the population in Ulaanbaatar was 600,985 in 1991 and 1,345,500 in 2015, which showed 2.3 times increase in the population of Ulaanbaatar. The population growth was largely caused by immigration to Ulaanbaatar. Even if the target populations were counted correctly in each year, a part of them moved to the other aimags by 2015. It may cause a difference in the AUP among those aged 1 to 24 years. The third was the age range used for the estimation of the unvaccinated proportion. Since the data on the measles vaccine coverage were available from 1991, the oldest was set to be 24 in 2015. The vaccine coverage for those aged 25 years or older in 2015 was not available. The fourth was the vaccination coverage of the second dose during 1991–2008 was not available, because the data on the second dose was not collected according to the health statistical regulation. Finally, the number of SIAs was not taken into account, because the number according to aimag was not available.
CONCLUSIONS
Unvaccinated proportion among those aged 1 to 24 years in the whole country was reduced by 15 times (from 28.0% in 1991 to 1.8% in 2014) during last 25 years. In the range of AUP between 2.7% and 18.5% among those aged 1 to 24 years, the vaccination coverage was not a significant factor for the incidence according to aimag at measles epidemic 2015–2016 in Mongolia. The density of the unvaccinated among those aged 1 to 24 years had a significant correlation with measles incidence 2015–2016, although the correlation disappeared when two highly populated aimags (Ulaanbaatar and Darkhan-Uul aimag) were excluded.
ACKNOWLEDGEMENT
We would like to express gratitude to all the experts for their participation in this study and for their extensive exploration of the competencies. In addition, we would like to thank our colleagues Dr. Dagva Bolorchimeg and Dr. Dorj Narangerel for the technical support for this study.
CONFLICT OF INTEREST
The study was performed as a part of a measles outbreak control investigation and had no specific funding allocated. The authors of this manuscript have no other conflict of interest to disclose.
Supplementary
Supplementary Table 1.
Percentage of the unvaccinated, based on the government records during 1991–2014 among the targeted population in Mongolia.
| 1991 | 1992 | 1993 | 1994 | 1995 | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
| Arkhangai | 5.9 | 1.0 | 0.2 | 23.3 | 14.0 | 20.9 | 7.1 | 8.1 | 1.6 | 9.4 | 1.7 | 2.8 | 2.3 | 1.0 | 3.9 | 1.6 | 1.3 | 2.9 | 12.5 | 4.3 | 1.3 | 2.2 | 0.0 | 0.4 |
| Bayan-Ulgii | 35.4 | 25.9 | 25.1 | 5.0 | 15.7 | 17.3 | 3.0 | 4.8 | 2.5 | 1.8 | 1.2 | 1.5 | 0.4 | 0.7 | 1.2 | 1.3 | 0.3 | 0.2 | 4.6 | 9.5 | 2.3 | 1.2 | 1.4 | 1.3 |
| Bayankhongor | n/a | 0.0 | 37.7 | 32.3 | 0.5 | 9.4 | 15.5 | 10.6 | 3.7 | 15.4 | 1.7 | 2.0 | 0.1 | 4.4 | 4.2 | 1.5 | 1.0 | 1.0 | 2.5 | 4.5 | 1.6 | 0.8 | 1.2 | 1.6 |
| Bulgan | 11.8 | 36.6 | 2.6 | 12.3 | 7.2 | 11.7 | 2.4 | 1.7 | 4.1 | 0.3 | 1.9 | 1.4 | 2.7 | 1.7 | 1.3 | 3.4 | 1.8 | 2.5 | 0.0 | 0.8 | 5.0 | 0.0 | 0.0 | 1.0 |
| Govi-Altai | 6.9 | 35.7 | 1.7 | 20.7 | 12.2 | 22.5 | 1.5 | 1.8 | 6.2 | 3.3 | 5.2 | 2.2 | 1.6 | 3.4 | 3.8 | 2.8 | 3.6 | 6.2 | 2.5 | 5.8 | 4.2 | 2.8 | 1.5 | 1.8 |
| Govisumber | n/a | 50.9 | 17.0 | 30.4 | 38.2 | 1.8 | 18.4 | 5.8 | 2.7 | 9.5 | 9.7 | 1.2 | 1.6 | 1.3 | 1.0 | 0.0 | 0.8 | 0.0 | 0.0 | 1.2 | 10.1 | 0.6 | 0.0 | 0.5 |
| Darkhan-Uul | n/a | 1.0 | 15.2 | 34.2 | 11.9 | 0.5 | 15.7 | 8.5 | 8.3 | 2.8 | 2.9 | 2.3 | 1.7 | 1.6 | 3.5 | 1.2 | 1.5 | 1.2 | 1.1 | 0.8 | 1.1 | 0.8 | 0.6 | 0.3 |
| Dornogovi | 21.4 | 11.0 | 14.7 | 21.3 | 21.8 | 7.5 | 4.2 | 6.9 | 1.2 | 0.5 | 2.9 | 2.9 | 1.9 | 1.5 | 0.9 | 3.0 | 1.2 | 3.4 | 0.7 | 0.3 | 0.0 | 0.5 | 0.5 | 0.0 |
| Dornod | 10.5 | 25.0 | 14.6 | 0.0 | 3.6 | 2.6 | 7.1 | 2.1 | 1.5 | 2.6 | 0.9 | 0.5 | 0.2 | 0.2 | 18.7 | 0.1 | 0.1 | 0.0 | 0.0 | 0.4 | 0.3 | 0.2 | 0.0 | 0.2 |
| Dundgovi | 16.0 | 1.0 | 29.3 | 10.0 | 16.8 | 4.5 | 11.1 | 1.0 | 2.2 | 5.5 | 4.0 | 2.5 | 2.2 | 1.3 | 1.6 | 2.5 | 3.1 | 1.5 | 1.8 | 0.4 | 0.0 | 0.0 | 0.0 | 0.3 |
| Zavkhan | 9.9 | 33.0 | 30.8 | 70.3 | 43.5 | 38.9 | 16.2 | 25.6 | 12.7 | 30.1 | 6.3 | 0.0 | 0.7 | 0.9 | 0.7 | 0.5 | 6.5 | 5.6 | 9.6 | 12.2 | 1.9 | 3.6 | 3.2 | 1.4 |
| Orkhon | n/a | 2.9 | 4.2 | 15.3 | 7.9 | 8.8 | 5.9 | 9.5 | 2.7 | 4.7 | 3.9 | 1.3 | 1.8 | 0.7 | 2.0 | 1.1 | 0.5 | 0.0 | 0.5 | 0.9 | 1.3 | 1.8 | 1.3 | 0.9 |
| Uvurkhangai | 28.4 | 37.7 | 25.7 | 48.6 | 40.4 | 29.8 | 9.8 | 4.3 | 5.0 | 13.4 | 2.6 | 0.3 | 3.4 | 0.9 | 0.7 | 1.4 | 1.3 | 2.1 | 2.4 | 1.6 | 0.3 | 1.4 | 1.9 | 2.2 |
| Umnugovi | 13.1 | 14.8 | 40.8 | 12.2 | 24.5 | 17.6 | 10.0 | 6.5 | 2.6 | 1.0 | 1.0 | 1.5 | 0.2 | 1.7 | 1.2 | 4.4 | 5.4 | 4.7 | 5.0 | 4.3 | 0.0 | 0.5 | 0.3 | 0.9 |
| Sukhbaatar | 1.9 | 30.0 | 13.7 | 30.1 | 14.1 | 19.9 | 12.8 | 10.9 | 5.9 | 0.8 | 2.2 | 2.4 | 0.6 | 0.9 | 1.0 | 0.1 | 2.2 | 1.5 | 2.6 | 2.0 | 0.9 | 0.5 | 1.6 | 2.2 |
| Selenge | 10.9 | 0.0 | 1.3 | 12.3 | 3.9 | 1.0 | 7.2 | 5.5 | 1.6 | 1.3 | 0.8 | 0.6 | 2.3 | 0.3 | 5.5 | 0.6 | 0.7 | 1.3 | 4.5 | 4.7 | 0.0 | 0.2 | 0.5 | 0.1 |
| Tuv | 32.3 | 59.9 | 27.8 | 16.8 | 15.9 | 12.9 | 15.0 | 7.8 | 5.0 | 1.4 | 1.3 | 2.7 | 2.7 | 0.7 | 1.9 | 1.8 | 1.2 | 1.8 | 0.8 | 1.3 | 0.4 | 1.4 | 1.5 | 1.3 |
| Uvs | 16.6 | 23.0 | 30.4 | 8.2 | 7.2 | 2.5 | 6.3 | 2.4 | 5.0 | 0.3 | 3.9 | 2.9 | 0.1 | 1.3 | 2.9 | 0.5 | 0.5 | 0.9 | 0.7 | 0.5 | 0.5 | 0.8 | 1.1 | 0.4 |
| Khovd | 15.3 | 0.0 | 3.4 | 13.9 | 38.8 | 17.8 | 14.5 | 10.3 | 1.6 | 11.2 | 0.2 | 1.1 | 1.8 | 0.4 | 0.9 | 0.4 | 2.6 | 0.4 | 1.4 | 11.1 | 7.4 | 0.4 | 0.1 | 2.2 |
| Khuvsgul | 27.0 | 54.0 | 46.7 | 21.7 | 23.1 | 2.9 | 7.2 | 0.7 | 4.9 | 0.4 | 1.8 | 1.6 | 1.5 | 1.4 | 1.6 | 0.5 | 4.0 | 9.4 | 9.8 | 3.1 | 6.9 | 1.9 | 0.6 | 0.7 |
| Khentii | 8.9 | 0.0 | 46.7 | 24.5 | 0.3 | 1.0 | 15.2 | 0.5 | 3.8 | 5.4 | 4.3 | 2.7 | 1.9 | 1.5 | 8.3 | 0.9 | 0.6 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 3.1 |
| Ulaanbaatar city | 20.1 | 5.6 | 3.6 | 10.9 | 6.7 | 7.1 | 8.5 | 7.7 | 12.7 | 10.7 | 10.2 | 0.9 | 4.2 | 1.2 | 0.9 | 0.6 | 1.3 | 4.1 | 3.9 | 7.5 | 1.9 | 2.6 | 6.5 | 2.8 |
| Whole country | 28.0 | 17.0 | 17.4 | 19.9 | 14.7 | 12.2 | 9.3 | 6.9 | 6.6 | 7.6 | 4.9 | 1.6 | 1.6 | 1.3 | 2.5 | 1.1 | 1.6 | 3.1 | 3.8 | 4.0 | 1.8 | 1.4 | 3.1 | 1.8 |
n/a: no data available
Abbreviations
- AUP
The accumulated unvaccinated proportion
REFERENCES
- 1.Moss WJ, Strebel P. Biological feasibility of measles eradication. J Infect Dis. 2011;204(Suppl 1):47–53. doi: 10.1093/infdis/jir065. [DOI] [PMC free article] [PubMed]
- 2.World Health Organization. Progress towards regional measles elimination-worldwide, 2000–2015. Wkly Epidemiol Rec. 2016;91(45):525–535. [PubMed]
- 3.Hall V, Banerjee E, Kenyon C, et al. Measles outbreak: Minnesota April-May 2017. MMWR Morb Mortal Wkly Rep. 2017;66(27):713–717. [DOI] [PMC free article] [PubMed]
- 4.Thomas S, Hiebert J, Gubbay JB, et al. Measles outbreak with unique virus genotyping, Ontario, Canada, 2015. Emerg Infect Dis. 2017;23(7):1063–1069. doi: 10.3201/eid2307.161145. [DOI] [PMC free article] [PubMed]
- 5.Le NK, Mhaskar R, Hoare I, et al. Reemergence of measles in the Americas: the genotype B3 2011–2012 outbreak in Ecuador. Vaccines (Basel). 2017;5(2):15. doi: 10.3390/vaccines5020015. [DOI] [PMC free article] [PubMed]
- 6.Magurano F, Baggieri M, Filia A, et al. Towards measles elimination in Italy: virological surveillance and genotypes trend (2013–2015). Virus Res. 2017;236:24–29. doi: 10.1016/j.virusres.2017.05.009. [DOI] [PubMed]
- 7.George F, Valente J, Augusto GF, et al. Measles outbreak after 12 years without endemic transmission, Portugal, February to May 2017. Euro Surveill. 2017;22(23). doi: 10.2807/1560-7917. [DOI] [PMC free article] [PubMed]
- 8.Mafigiri R, Nsubuga F, Ario AR. Risk factors for measles death: Kyegegwa District, western Uganda, February-September, 2015. BMC Infect Dis. 2017;17:462. doi: 10.1186/s12879-017-2558-7. [DOI] [PMC free article] [PubMed]
- 9.Inaida S, Matsuno S, Kobune F. Measles elimination and immunisation: national surveillance trends in Japan, 2008–2015. Epidemiol Infect. 2017;145(11):2374–2381. doi: 10.1017/S0950268817001248. [DOI] [PMC free article] [PubMed]
- 10.Gao J, Shen B, Xiong J, Lu Y, Jiang Q. The measles epidemic trend over the past 30 years in a central district in Shanghai, China. PLoS One. 2017;12(6):e0179470. doi: 10.1371/journal.pone.0179470. [DOI] [PMC free article] [PubMed]
- 11.Ma C, Yan S, Su Q, et al. Measles transmission among adults with spread to children during an outbreak: Implications for measles elimination in China, 2014. Vaccine. 2016;34(51):6539–6544. doi: 10.1016/j.vaccine.2016.02.051. [DOI] [PubMed]
- 12.Heymann DL. Control of Communicable Diseases Manual. 18th ed. Washington DC: American Public Health Association; 2004.
- 13.La Torre G, Saulle R, Unim B, et al. The effectiveness of measles-mumps-rubella (MMR) vaccination in the prevention of pediatric hospitalizations for targeted and untargeted infections: a retrospective cohort study. Hum Vaccin Immunother. 2017;3(8):1879–1883. doi: 10.1080/21645515.2017.1330733. [DOI] [PMC free article] [PubMed]
- 14.World Health Organization. Regional Office for Europe. 2003. Strategic Plan for Measles and Congenital Rubella Infection in the European Region of WHO. Copenhagen: WHO Regional Office for Europe. https://apps.who.int/iris/handle/10665/107526. Accessed February 10, 2019.
- 15.WHO Western Pacific Region. Mongolia WHO Expanded Programme on Immunization Prorgamme Review. Manila, Philippines: WHO Western Pacific Region; 2003.
- 16.Expanded programme on immunization (EPI) immunization schedules in the WHO Western Pacific Region, 1995. Wkly Epidemiol Rec. 1996;71(18):133–137. [PubMed]
- 17.Rentsen T, Enkhtuya B, Nymadawa P, et al. Measles outbreak after a post-honeymoon period in Mongolia, 2001. Jpn J Infect Dis. 2007;60(4):198–199. [PubMed]
- 18.World Health Organization Western Pacific Region. Mongolia certified measles free. https://www.who.int/westernpacific/news/detail/08-07-2014-mongolia-certified-measles-free. Accessed March 28, 2019.
- 19.Hagan JE, Takashima Y, Sarankhuu A, et al. Risk factors for measles virus infection among adults during a large outbreak in postelimination era in Mongolia, 2015. J Infect Dis. 2017;216(10):1187–1195. doi: 10.1093/infdis/jix449. [DOI] [PMC free article] [PubMed]
- 20.Orsoo O, Saw YM, Sereenen E, et al. Epidemiological characteristics and trends of a Nationwide measles outbreak in Mongolia, 2015–2016. BMC Public Health. 2019;19(1):201. doi: 10.1186/s12889-019-6511-0. [DOI] [PMC free article] [PubMed]
- 21.World Health Organization. Measles vaccine: WHO position paper. April 2017- recommendations. Vaccine. 2019;37(2):219–222. doi: 10.1016/j.vaccine.2017.07.066. [DOI] [PubMed]
- 22.World Health Organization Representative Office for Mongolia. Ministry of Health. Report Measles and Rubella Seroprevalence Survey Mongolia - 2017. Ulaanbaatar, Mongolia: WHO Representative Office for Mongolia; 2018.
- 23.Hagan JE, Greiner A, Luvsansharav UO, et al. Use of a diagonal approach to health system strengthening and measles elimination after a large nationwide outbreak in Mongolia. Emerg Infect Dis. 2017;23(Suppl 1):S77–S84. doi: 10.3201/eid2313.170594. [DOI] [PMC free article] [PubMed]
- 24.Lake JG, Luvsansharav UO, Hagan JE, et al. Healthcare-associated mesales after a nationwide outbreak in Mongolia. Clin Infect Dis. 2018;67(2):288–290. doi: 10.1093/cid/ciy067. [DOI] [PubMed]
- 25.Lee CT, Hagan JE, Jantsansengee G, et al. Increase in infant measles deaths during a nationwide measles outbreak, Mongolia, 2015–2016. J Infect Dis. 2019;220(11):1771–1779. doi: 10.1093/infdis/jiz140. [DOI] [PMC free article] [PubMed]
- 26.Dominguez A, Torner N, Barrabeig I, et al. Large outbreak of measles in a community with high vaccination coverage: implications for the vaccination schedule. Clin Infect Dis. 2008;47(9):1143–1149. doi: 10.1086/592258. [DOI] [PubMed]
- 27.Sugerman DE, Barskey AE, Delea MG, et al: Measles outbreak in a highly vaccinated population, San Diego, 2008: role of the intentionally undervaccinated. Pediatrics. 2010;125(4):747–755. doi: 10.1542/peds.2009-1653. [DOI] [PubMed]
- 28.Atrasheuskaya A, Kulak M, Neverov A. Measles cases in highly vaccinated population of Novosibirsk, Russia, 2000–2005. Vaccine. 2008;26(17):2111–2118. doi: 10.1016/j.vaccine.2008.02.028. [DOI] [PubMed]
- 29.Yang W, Li J, Shaman J. Characteristic of meales epidemics in China (1951–2004) and implication for elimination: a case study of three key locations. PLoS Comput Biol. 2019;15(2):e1006806. doi: 10.1371/journal.pcbi.1006806. [DOI] [PMC free article] [PubMed]