Abstract
Onchocerciasis is a parasitic infection caused by the filarial nematode Onchocerca volvulus and transmitted through the bites of black flies of the genus Similium that breed in rivers and streams. The impact of mass treatment with ivermectin and supplemented by vector control in some countries has changed the global scene of onchocerciasis. There has been reported progress made in elimination of onchocerciasis in central and southern American countries and in some localities in Africa. The target for elimination in the Americas has been set at 2022 while for 12 countries in Africa this is expected in 2030. This review was conducted to examine the current status of onchocerciasis elimination at the global level and report on progress made. Literature searches were made through PubMed, articles in English or English abstracts, reports and any other relevant articles related to the subject. The global burden of onchocerciasis is progressively reducing and is no longer a public health problem in some regions. However, programs are challenged with a range of issues: cross-border transmission, diagnostic tools, Loa loa co-endemicity, limited workforce in entomology and maintaining enthusiasm among community drug distributors. More concerted effort using appropriate tools is required to overcome the challenges.
Keywords: onchocerciasis, ivermectin, vector control, elimination, progress, challenges
Introduction
Onchocerciasis is a parasitic infection caused by the filarial nematode Onchocerca volvulus and transmitted through the bites of black flies of the genus Similium that breed in rivers and streams.1 In 2019, World Health Organization (WHO) estimated that 217.5 million people globally require mass drug administration with ivermectin.2 More than 99% of all onchocerciasis cases are in sub-saharan Africa, but some small foci also occurred in the Americas and in Yemen.2,3 The infection causes skin lesions, severe itching, eye disease, including visual impairment which can lead to blindness; hence, the common name, ‘river blindness’4
The development of various partnerships to defeat onchocerciasis as a public health problem in Africa can be traced back to the 1940s,5 but a comprehensive plan was not formulated until 1968. By 1972, the international development community was mobilized to fight the disease. Onchocerciasis control on a large scale began in 1974 in West Africa as a regional project under the auspices of the World Bank, Food and Agriculture Organization (FAO), United Nations for Development Progamme (UNDP) and World Health Organisation (WHO), known as the Onchocerciasis Control Program (WHO-OCP). At that time vector control with environmentally safe insecticides was the only available approach.6 The program area covered 1,200,000 km2 to protect 30 million people across 11 countries from river blindness, namely Benin, Burkina Faso, Côte d’Ivoire, Ghana, Guinea-Bissau, Guinea, Mali, Niger, Senegal, Sierra Leone and Togo.6 The estimated total cost of the program was USD 550 million, which was less than 1 USD per year for each protected person.7 The global benefit of the WHO-OCP operations prevented almost 600,000 cases of blindness, protected 18 million children born in the controlled areas from the risk of river blindness, and brought 25 million hectares of land that was infested by black flies under cultivation. WHO-OCP demonstrated the vital role-played by this operation and its socio-economic impact in remote and neglected areas.7 These operations involved international developmental partners and the regional endemic countries with little engagement of the community-level efforts.
Although the WHO-OCP was successful, it was considered expensive and had technical challenges of insecticide resistance and black fly migration across the borders.8 However, following the registration of ivermectin for human use in 1987, its unprecedented donation by Merck & Co. Inc. in 1987, ivermectin become the mainstay for the treatment of onchocerciasis. The discovery, development and use of ivermectin for the treatment of onchocerciasis were the effort of William Campbell of Drew University in Madison, New Jersey, and Satoshi Ōmura of Kitasato University in Tokyo who were recognized with a Nobel Prize in 2015.9
Following the ivermectin donation announcement, by 1990 Ecuador, Guatemala and Mexico had already undertaken field trials in ivermectin distribution. In Guatemala, the program was supported by various partners including the United States Centers for Disease Control and Prevention (CDC).10 During that time, countries like Brazil, Colombia and Venezuela had no active program to distribute ivermectin. However, in 1991 the first regional Inter-American Conference on Onchocerciasis by experts on the disease discussed new opportunities for controlling or eliminating onchocerciasis. The Pan American Health Organization (PAHO) steered the meeting in response to the call on the feasibility of eliminating onchocerciasis using ivermectin in some parts of Africa and the Americas.11 The Onchocerciasis Elimination Program for the Americas (OEPA) was established in 1993 with the goal of eliminating onchocerciasis transmission in the region. Its strategy was six-monthly mass distribution of ivermectin with a target coverage of 85% of the eligible population, although ivermectin has been distributed up to four times per year in some areas.12 According to its regional resolution and strategic plan, elimination of onchocerciasis transmission is anticipated by 2022.13,14 PAHO then developed the first onchocerciasis elimination verification guidelines in 200115 and these formed the basis for the strategy later adopted by most African countries.
The first description of onchocerciasis in the Yemen was from the early 1940s when Petrie and Seal16,17 reported the first onchocerciasis case associated with a type of dermatitis, referred to as “blue skin disease” among people in southern Yemen. The presence of a clinical presentation of dermatitis attributed to onchocerciasis was reported from the north of Yemen, which was called “sowda” by local populations due to the darkened skin appearance.18,19 Onchocerciasis is now known to be endemic in 33 Districts in eight Governorates in the Western Region of Yemen, where it occurs along the wadis that drain westward to the Red Sea.16 It is thought to be absent further east, but this has yet to be confirmed. Despite the incrimination of S. damnosum s.l. as the vector of O. volvulus in Yemen, little is known about its breeding sites, behaviors related to disease transmission, feeding habits and biting rates.20 Prior to the advent of ivermectin in 1987, treatment of onchocerciasis in Yemen was by Diethyl-carbamazine and suramin that were used on an individual basis but were not appropriate for Mass Drug Administration (MDA).21 A national action plan to eliminate the disease was developed in 2010, but social unrest and political instability in the country since 2011 have hampered the full implementation of the road map.22 The first pilot MDA was launched in 2016; this was followed by full MDA in 2018.2
The African Programme for Onchocerciasis Control (APOC) was launched in 1995 with the objective of controlling onchocerciasis as a public health and socio-economic problem in the 19 participating countries in Africa.23 In 1997, it adopted Community-Directed Treatment with Ivermectin (CDTI) as its core strategy and coverage and compliance steadily increased.24 This strategy was important because endemic communities were empowered to determine timing of distribution, select their distributors, agree on mode of distribution and participate in supervision of MDA. In 2009 under the auspices of APOC, an international group of experts convened to review the state-of-the-art of onchocerciasis elimination in Africa with current tools and there resulted a paradigm shift from control to elimination.25 Following this, APOC developed the conceptual and operational framework for onchocerciasis elimination with ivermectin treatment to guide endemic countries in implementing elimination activities.26 APOC closed at the end of 2015. By the time of its closure, more than 25 million people lived in areas where few or no people had microfilariae in their skin27 and onchocerciasis-related blindness in most parts had been controlled. Models suggested that APOC had saved 17.4 million DALYs, at a cost of USD 27/DALY28 and country programs distributed >112 million treatments in the final year of the program.29 In order to maintain and build on the success of APOC, WHO in 2016 established a new structure, the Expanded Special Project for Elimination of Neglected Tropical Diseases (ESPEN), to co-ordinate technical support for activities focused on five neglected tropical diseases in Africa, including onchocerciasis elimination.30 Globally, the onchocerciasis elimination effort being made is improving the general quality of life of the population and achieving Sustainable Development Goals (SDGs).31 However, programs are challenged with a range of issues: cross-border transmission, diagnostic tools, Loa loa co-endemicity, limited workforce in entomology and maintaining enthusiasm among community drug distributors. Development of new tools to tackle these challenges are needed, and this paper will review progress so far made, describes where we are as of 2020 and highlights key challenges associated with onchocerciasis elimination.
Onchocerciasis Elimination Strategies
The basic elimination strategy has been MDA supplemented by vector control in some countries, and the proof of principle that MDA alone can eliminate onchocerciasis in Africa was demonstrated in Mali and Senegal, and the Joint Action Forum of APOC endorsed the results.23 The momentum to steer elimination led to the development of WHO guidelines in 2016 which was a modification of guidelines from PAHO.15,32 Both ESPEN and WHO NTD Department in Geneva continue to support programs in Africa with technical advice. However, ESPEN is not able to provide direct advice on the same scale as APOC partly due to funding constraints and to the move to increase in the responsibility of individual endemic countries to plan their own programs. To fill this gap in technical input, the Ministry of Health of each endemic country establishes its own onchocerciasis elimination expert advisory committee to apply and adjust WHO Guidelines, to recommend best practices, to review progress towards elimination, and to provide technical support.33
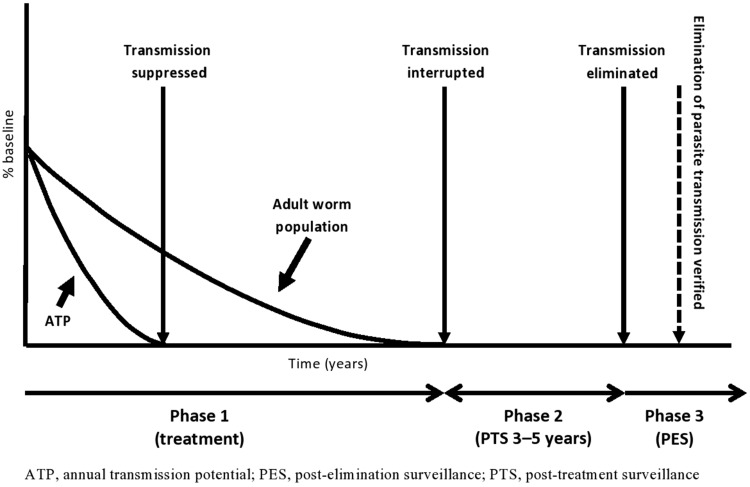
The process leading to elimination starts with mapping of onchocerciasis and instituting MDA with ivermectin (phase 1), followed by monitoring and evaluation. Stopping-MDA surveys use entomological evaluation of black flies and epidemiological assessments of children using serology.32,34 If successful, CDTI is stopped and the onchocerciasis-endemic area moves into Phase 2 (Post-Treatment Surveillance – PTS) for 3–5 years. Entomological surveillance is then used to confirm the elimination of transmission and progression of the endemic area into Phase 3 (Post-Elimination Surveillance – PES), with permanent cessation of treatment. There will be further occasional surveys during phase 3, until regional elimination is declared to ensure that recrudescence or re-establishment of infections do not occur35 (Figure 1).
Figure 1.
Phases in the elimination of human onchocerciasis. Reproduced with permission from World Health Organization. Guidelines for Stopping Mass Drug Administration and Verifying Elimination of Human Onchocerciasis: Criteria and Procedures. Geneva, Switzerland: WHO Press; 2016. Licence: CC BY-NC-SA 3.0 IGO.32
Mapping of Onchocerciasis
During the APOC era mapping for onchocerciasis was by Rapid Epidemiological Mapping of Onchocerciasis (REMO), a tool developed by Ngoumou et al.36 REMO allowed the mapping of most endemic countries according to the prevalence of palpable nodules, categorizing communities as hyper-, meso- and hypo-endemic. During that time ivermectin treatment was prioritized by APOC in areas with nodule prevalence >20% and microfilaria prevalence >40% leaving out the hypo-endemic areas on assumption that the disease was not of public health significance and that transmission was not self-sustaining in such areas and hence it would disappear without intervention, but this was never proven. With the paradigm shift from control to elimination,26 the issue of hypo-endemic zones became of concern and it was demonstrated in Cameroun that self-sustaining transmission can occur in hypoendemic areas.37 This is an important issue for onchocerciasis elimination. The Onchocerciasis Technical Sub-group (OTS) of WHO and ESPEN have developed Onchocerciasis Elimination Mapping (OEM) to guide endemic countries ensure that during the scaling up of MDA to hypo-endemic zones, no onchocerciasis-endemic district is left behind.38,39 All those areas previously excluded from onchocerciasis control because they had been defined as hypo-endemic must now be reassessed to determine the precise area over which onchocerciasis is endemic. Data collected during elimination mapping will feed directly into the ESPEN data portal, in accordance with agreements reached between ESPEN and the relevant Ministries of Health.39 This has been an innovation because maps and underlying datasets for all the five PC-NTDs are made available at both implementation unit and site levels.
Interventions
Mass Drug Administration with Ivermectin
Ivermectin has been the main tool in the fight against onchocerciasis,40 in most programs, it is delivered to communities once a year, usually by CDTI.41 In Africa, the targeted therapeutic coverage for MDA was ≥65% and geographical coverage of 100% of the meso- and hyper-endemic areas.42 However, with the shift from control to elimination, therapeutic coverage target was adjusted from ≥65% to ≥80% so as to meet the criteria for elimination, and 100% geographic coverage in all endemic areas.26
The OEPA adopted ivermectin MDA twice or four times per year, with at least 85% coverage of the eligible population in all endemic communities. The Ministry of Health personnel conducted MDA. All individual foci were subjected to the three phases of elimination43 before a request was made to WHO for verification of elimination across a country.44,45
In Africa, the adoption of an elimination strategy occurred in 2009.26 Shifting the target from control to elimination made countries in Africa to refocus their strategies based on the local epidemiological situation.25 Some countries (Uganda, Nigeria, Ethiopia) changed the treatment regimen from the annual to bi-annual. The decision to change treatment strategy was made by the National Oncocerciasis Elimination Committees (NOEC) of each country.33 In a few exceptional cases, where progress towards elimination has been problematic, further increases in frequency of MDA have been introduced. For example, Ethiopia adopted four times/year ivermectin treatment in part of one focus (Matema) bordering Sudan. Stop MDA evaluation identified a hot spot of ongoing transmission that was the result of low MDA coverage. MDA was stopped throughout most of the foci, except within the hot-spot where it was increased to speed-up elimination and to protect the rest of the foci from reinvasion by the parasite. In 2018, South Sudan introduced bi-annual treatment in Maridi County, Western Equatoria,46 and this decision was made based on the local situation.47
Vector Control
Historical and recent efforts for black fly control have relied on treating breeding sites with larvicides.48,49 When APOC was launched in 1995, one of its objectives was to support vector elimination in geographically isolated areas.6 Two foci supported by APOC in Equatorial Guinea (Bioko focus) and Uganda (Itwara focus) were successful.50,51 In Bioko, S. yahense was eliminated in 2005 by aerial spraying with the organophosphate insecticide temephos (Abate EC200), while in Uganda S. neavei that lives in phoretic association with freshwater crabs, P. aloysisabaudiae, was also eliminated in 2003 by ground larviciding. The experiences of ground larviciding motivated the Uganda program to subsequently eliminate S. neavei from Mt. Elgon, Kashoya-Kitomi and Mpamba-Nkusi foci.49,52,53
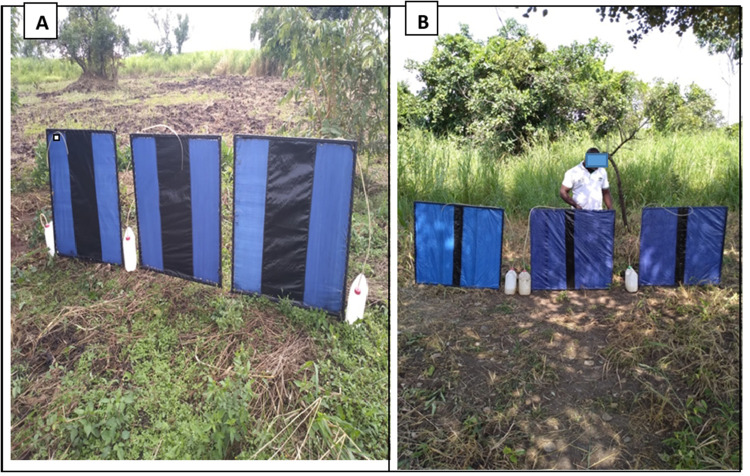
Anti-vector activities in other African countries have been considered in support of CDTI where there were exceptional problems and progress towards elimination has been slow but so far none have been instigated, largely because larviciding is too resource-hungry. However, other sorts of anti-vector approaches are being actively researched. The Esperanza Window Trap (EWT) was originally developed in Mexico to replace human landing collections (HLCs) for monitoring the transmission of O. volvulus in elimination programs.54,55 It consists of a vertical blue and black striped sheet with a sticky surface. The black fly vectors are attracted to the colour pattern, but it is also baited with carbon dioxide (released by yeast fermenting a sugar solution) and dirty socks or trousers (which seem to release unknown chemo-attractants). In Mexico and Guatemala, EWT evaluations were conducted to see if it can reduce biting rates around schools and households in Las Golondrinas and Jose Maria Morelos located in Southern Chiapas. The traps collected epidemiologically significant numbers of Simulium ochraceum s.l.56 Similarly, in Africa, the EWT was evaluated in Burkina Faso against S. damnosum s.l.57 and in Tanzania against S. plumbeum in the Mahenge focus.58 Results were generally good, and in many cases, the EWT catch was more or less equivalent (or better) than HLCs, but the performance was inconsistent between some sites, and this was also found to be the case in small-scale trials in Sierra Leone (Post, unpublished data). The variation has been difficult to explain but may have been related to the vector cytospecies and/or the exact placing of the trap. The most recent and extensive evaluations on EWTs are being undertaken in Madi mid-north focus located in Northern Uganda. The EWT has been optimized during studies along River Ayago in northern Uganda and has resulted in reduction in vector biting rates.59 Adjustments of the size of the black stripe in the middle (Figure 2, Panel B) of the trap was observed to improve the EWT catches significantly compared with the standard trap60(Figure 2, Panel A). EWTs are showing promise as an additional anti-vector strategy in accelerating onchocerciasis elimination in areas with high vector density. Similarly, a modified biconical Challier-Laveissière tsetse fly traps have been shown to perform well as HLCs in some localities, but not others.61 Further development and evaluation of EWT is required before it could replace HLCs.
Figure 2.
Standard black stripe Esperanza Window Trap (A) and the modified narrow black stripe EWT (B).
Notes: Reproduced with permission from Vector Control Division, Ministry of Health Uganda, Slash & Clear Project, 2018.
Another recent development in potential novel vector control is “Slash and Clear”. This involves the removal of vegetation from S. damnosum s.l. breeding sites to reduce the number of larval supports, in the hope that this would have the knock-on effect of reducing the vector biting rates. It had previously been tried in the Democratic Republic of Congo (then Belgian Congo) in 1942–44, South Sudan (then Sudan) in 1983 and Malawi in 1992.62 All these projects showed some reduction in populations of S. damnosum s.l., but they were never followed up until recent and more systematic studies in Uganda which have shown that the approach has great promise. Slash and Clear has been evaluated in Madi mid-north focus in Northern Uganda, and a dramatic reduction in daily vector biting rates was observed.63 This result implies that during the trial, the experimental area was not subject to vector reinvasion and that most of the biting black flies were breeding locally. This inference is supported by the observation of local variation of chromosomal polymorphisms in the vector larvae in the same area (Post, unpublished). It is at the moment unclear the extent to which Slash and Clear might be applied in other geographical situations and other vector cytospecies.
Slash and Clear, and EWTs are available alternative vector control strategies that should be considered to minimize cost of larviciding and mitigate the risk of insecticide resistance.64,65
The dynamics of transmission of O. volvulus indicate that transmission intensity is strongly affected by the rate of host-vector contact,66,67 and reducing vector densities can be an effective method of suppressing transmission.68 However, based on Bayesian data-driven mathematical modeling approach, supplementing annual drug treatments with “Slash and Clear” can significantly accelerate the achievement of onchocerciasis elimination. This intervention is not very sensitive to the timing of implementation, and the impact is evident even if vegetation is cleared only once per year. Therefore, this community-driven technique shows promise as a cost-effective option for achieving and sustaining O. volvulus elimination.69 The strategy is community-driven because of their involvement in planning, implementation, supervision of the slash activities and participating in data collection (human landing catches).
Diagnostic Tools in the Onchocerciasis Elimination Era
There is now a global momentum to eliminate onchocerciasis under the WHO Neglected Tropical Diseases road map,70 and this led to the development of new guidelines by the World Health Organization for verification that transmission has been suppressed and eventually eliminated.32 These guidelines are expected to be revised by WHO in 2020, but it is clear that progress towards onchocerciasis elimination effort would benefit enormously by newer, more sensitive and specific diagnostic tests to verify that transmission of infection has been suppressed or interrupted.71 Elimination programs can use the following:
Serological Test to Detect Exposure to O. volvulus
Currently WHO guidelines have recommended Ov16 ELISA for demonstrating the interruption of transmission of O.volvulus in all elimination programs.32 The serological threshold for stopping MDA is an Ov16 antibody prevalence of <0.1% among children aged 5–9 years (inclusive) who act as sentinels for recent infection. The test being currently used by most countries such as Uganda has a sensitivity of around 40% and there are arguments by experts about whether the current <0.1% threshold is too stringent and an Ov16 threshold of <2% might be sufficient.72 However, this is as yet unproven in the field. The IgG4 response takes time to develop and thus will not immediately reflect recent exposure, yet the current assays have focused on detection of IgG4. There are also test cards that consist of either a single IgG4 rapid test or a combination test utilizing Ov16 and the W. bancrofti antigen Wb123.73,74 The sensitivity of the Ov16 RDT single test is 81.1% and the Ov16 test line of the biplex test is 81.3%.75 The specificity is listed at 99.0% for the single Ov16 RDT test and 100% for the biplex test76. The Ov16 RDT was successfully field tested in Senegal77 and has been extended to a number of other African countries and the results are yet to be published. However, according to recommendations from WHO-OTS, the Ov16 RDT on eluted dry blood spots in the laboratory (ie, not using fresh blood in the field) can be used for mapping and Monitoring & Evaluation (M&E) surveys. There are studies planned to evaluate RDTs effectiveness in Stop-MDA surveys, and the different Ov16 ELISA systems need to be properly compared and evaluated.
Detection of Parasites in Black Flies by Pool-Screening
The vectors of O. volvulus are various species of black flies of the genus Simulium. The successful interruption of transmission of onchocerciasis implies the absence of parasites in vectors as well as people, and is the most sensitive measure of the interruption of transmission.32 Black fly vectors caught by HLCs are not normally tested for infective larvae of O. volvulus by dissection, because of the difficulty in the microscopic separation from Onchocerca species of animal origin (especially O. ochengi). The O-150 PCR DNA amplification assay applied to vector heads is the most widely used assay to detect infective vectors, and this is usually applied to pools of heads of flies to verify elimination of transmission. The current WHO guidelines call for testing sufficient numbers of flies to ensure that the upper bound of the 95% CI of the prevalence of flies carrying infective larvae is less than 0.05% (1/2000). Meeting this criterion requires testing at least 6000 flies from the endemic area, and having all test negative.32,78 Once a focus meets this criterion (along with the Ov-16 criterion), MDA can be suspended in a focus. This is followed by monitoring for 3–5 years and this is called PTS. The O-150 PCR has been widely applied to collect entomological data verifying elimination of transmission in a number of foci, for example, Mexico, Guatemala, one focus in Sudan78,80 and a Sudan-Ethiopia cross-border focus.81 The cost to process a single pool of 100 flies is US$ 6.90 per pool.82 This technique has been successful apart from challenges associated with collecting sufficient vectors and choosing a suitable geographical assessment unit.
An understanding of the seasonality of rivers, vector breeding sites and the numbers of biting flies is essential to collect sufficient number of flies; and vector collection sites must be representative of the whole assessment area. Davies et al83 earlier reported that annual climatic changes, especially well marked wet and dry seasons, have associated biting patterns. In the savannas of West Africa (Sierra Leone) with severe drought seasons the biting of S. damnosum s.l. almost ceases for several months, resuming again with the coming of rains and re-establishment of extensive breeding sites in the rivers; biting is heavily concentrated in the wet season. Seasonality also has influence on vector species composition, competence and transmission patterns. The problem of collecting sufficient numbers of flies using HLCs might be resolved by the recent development of EWT platform demonstrated in Mexico and Uganda55,58.
The choice of assessment unit is problematic and WHO recommends that Transmission Zones (TZs) should be used. TZs are defined as “a geographical area where transmission of Onchocerca volvulus occurs by locally breeding vectors”.32,84 This has worked well in South America12 and Uganda85 where TZs are fairly small and well separated from others. However, this is very problematic in much of Africa because there are often no obvious gaps in the distribution of infections which might indicate TZ boundaries. Most countries either use river basins as surrogates for well-defined TZs, or use administrative areas (often Districts, but States in the case of Nigeria) for convenience, which they then consider in the light of local hydrology86 This stems from lack of knowledge of fly movements and dispersal of parasites. The minimum of 6000 flies to be screened is to give statistical validation,82 but it assumes that the area from which the flies have been drawn is uniform. Therefore, countries are sometimes forced to adopt ad-hoc solutions to this general problem.
Detection of Parasites in Humans
The method of detecting microfilariae in humans has been skin snip microscopy, and this has been recognized as highly specific but poorly sensitive and painful to the affected communities.87,88 To address the problem of sensitivity, skin snip can be replaced with detection of PCR-amplified parasite DNA. Most of these assays target the tandemly repeated sequence in the O. volvulus genome called the O–150 repeat. Real-time PCR and isothermal loop amplification (LAMP) assays have also been developed.89 Currently, the qPCR-O-150 assay was proved to be more appropriate for evaluating skin snips of Ov-16 positive children when deciding when to stop MDA.90 A novel O-5S qPCR assay targeting the O. volvulus O-5S rRNA gene had 100% specificity and proved more sensitive than O-150 qPCR assay.91
There has been further development of infection assays using parasite-specific metabolites that are produced by the female worms, including a neurotransmitter excreted in host urine92 and microRNAs in the peripheral blood.93,94 All these showed promise, but the neurotransmitter detection system was unsuitable for large-scale use and the parasite microRNA may not be present in sufficient concentration for easy detection.95
Progress Towards Elimination
The Legacy of WHO-APOC in Africa
At the inception of APOC in 1995, the population at risk with onchocerciasis in Africa was 120 million, those infected 17 million, 800,000 were visually impaired, 270,000 blind and approximately 6.4 million people with severe skin conditions.96 The objective of APOC was to control onchocerciasis as a public health problem, because at that time it was thought that in an African setting mass treatment with ivermectin was unlikely to achieve elimination. In 2010, the objective was changed to elimination of transmission following the results of studies in Senegal and Mali,97 and in Nigeria1 which indicated that mass treatment with ivermectin might eliminate onchocerciasis in Africa. When APOC closed in 2015, new structures were developed to achieve elimination in the endemic countries, but APOC had already set the scene11 and made progress towards elimination in Africa by sponsoring REMO assessments to map hypo-endemic areas and extension of CDTI. By 2015, the loss of an estimated 19 million disability-adjusted life years (DALYs) had been averted by APOC countries, which represented an 80% reduction in DALY loss due to onchocerciasis in those countries,28 and it has been argued that throughout most of Africa onchocerciasis may have been eliminated as a public health issue.98 Thus, APOC had achieved a remarkable and widespread reduction in lost DALYS and started Africa on the road to elimination. However, in the five years since adopting the objective of elimination, there were only a few endemic countries (Uganda, Sudan) where transmission had been suppressed and MDA stopped, but no foci had entered into Post-Elimination Surveillance by 2015.99 This is not altogether surprising given the time-scale, but APOC had also achieved cost-effective vector elimination in two geographically isolated foci (in Equatorial Guinea and Uganda) and thus eliminated transmission.50,51
Current Status of Onchocerciasis Elimination in Africa
Most of the endemic countries in Africa have adopted an elimination policy and have formed onchocerciasis elimination expert advisory committees as required by the 2016 WHO guidelines.32,33 Elimination of transmission is expected to avert the loss of 4.3–5.6 million DALYs over 2013–2045 when compared with the control mode, and also reduction in the number of community volunteers and health workers.100 In the long-term elimination is the only certain sustainable option, and is cost-effective. The total number of people treated in the region has increased by 6 million to 151.2 million; and at least 15 countries had achieved 100% geographical coverage by 2018.2 In spite of this progress, no country in Africa has yet been verified by WHO as free of the disease, and by 2018 there were still more than 15 million people living in districts in various countries where MDA was required but had not yet been started. It is not surprising that some of the ex-OCP countries are amongst those instigating elimination programs, because some have areas which were not included in OCP operations, for example, the southern part of Ghana (forested), or they received insufficient treatment due to civil unrest (Sierra Leone). However, there have also been some surprising problems of transmission in areas which had been subject to sustained vector control by OCP and should have been cleared of parasites. There has been a recrudescence of transmission in South West Burkina Faso,101 but this was discovered and brought under control by MDA with ivermectin. Similarly, there are also areas of ongoing transmission in Mali, which are also now under MDA. It is not clear whether these recrudescences are the result of transmission of an endemic population of parasites which had survived OCP operations, or a result of immigration of parasites from other non-OCP areas. But what is clear is that the countries have instigated appropriate actions.
In Africa, the Abu Hamed focus in Sudan, which had predominantly the severe form of skin disease sowda or lichenified onchodermatitis, was the first focus in Africa to have successfully completed the entire WHO-recommended process to confirm elimination.79 Furthermore, Sudan and Ethiopia have stopped MDA and progressed to PTS in collaboration with each other in the Metema-Galabat focus which straddles the Ethiopia-Sudan border.80 Uganda has also made remarkable progress since launching its onchocerciasis elimination policy in 2007. Elimination has been based on twice-yearly treatment supplemented by vector control/elimination. By 2019, onchocerciasis had been eliminated from 8 out of the 17 foci in Uganda and over four million people living in these districts are no longer at-risk. This is the largest protected population currently known under WHO elimination guidelines.102 This provides further evidence that elimination of onchocerciasis in Africa is possible,103 and according to the new WHO NTD road map 2021–2030 12 countries are expected to achieve complete elimination by 2030.104
Current Status of Onchocerciasis Elimination in Yemen
Yemen is the second country after Sudan in the WHO Eastern Mediterranean Region (EMRO) which is endemic for onchocerciasis, and there are currently 33 endemic Districts. MDA with ivermectin was conducted from 2001 to 2013 with the objective of eliminating Sowda, but in 2013, the country adopted a national plan to eliminate onchocerciasis.105 In 2016 Yemen piloted an MDA campaign and treated 162,000 people with support from End Fund and Schistosomiasis Control Initiative. There was implementation of MDA in Yemen where 550,131 people were treated with good results (87.5% therapeutic coverage) despite experiencing instability.2 Exclusion and elimination mapping is underway and operational research is planned to develop a treatment plan which takes into account the country’s unique and difficult geography. Progress is surprisingly good in the face of ongoing armed conflict.22 The first meeting of the Yemen Onchocerciasis Expert Committee was held in February 2020.
Current Status of Onchocerciasis Elimination in the Americas
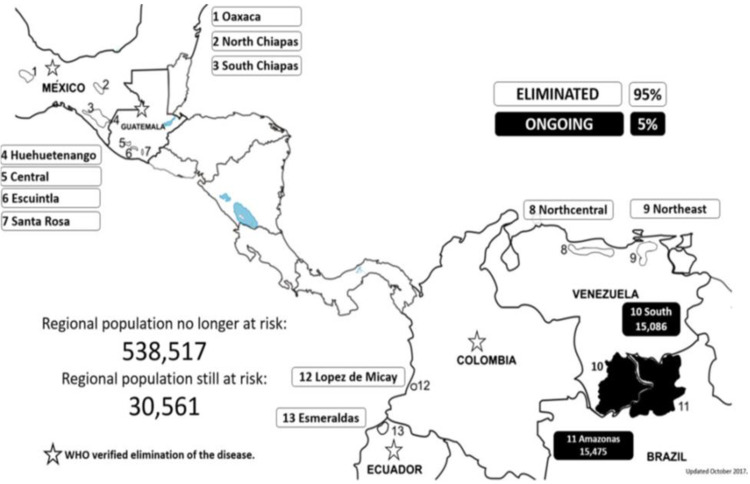
Tremendous progress has been made by OEPA where onchocerciasis transmission has been eliminated in 11 out of the 13 foci, and four out of six endemic countries have been verified as eliminated by WHO12 (Figure 3). The first was Colombia in 2013,106 followed by Ecuador in 2014, Mexico in 2015 and Guatemala in 2017.12 A total of 538,517 people are no longer at risk of onchocerciasis and there has been a 95% reduction in the target population.2,12 However, the program is now grappling with the Yanomami focus where a population of 33,746 by 2018 is still at risk of the disease in the rain forest highlands which form the watershed between the Amazon and Orinoco river basins. The population in this focus is highly mobile and difficult to access requiring collaborative effort from Brazil and Venezuela. The program’s concerted effort has been the use of helicopter/aircraft to reach remote areas, use of 4 times/year ivermectin treatment, training of indigenous health agents, sharing data and information aimed at interrupting transmission of onchocerciasis in this remaining focus.2,12 Progress is extremely good but new endemic communities are still being found (Table 1).
Figure 3.
Distribution of onchocerciasis in the Americas, 2017.
Notes: Reprinted from Sauerbrey M, Lindsay JR, Richards FO Jr. Progress toward elimination of onchocerciasis in the Americas. Int Health. 2018;10:i71–i78, by permission of Oxford University Press.12
Table 1.
Onchocerciasis in the Americas: Population at Risk, No Longer at Risk, Under Post-Treatment Surveillance (PTS), Eligible for Treatment and Transmission Status by Focus in 2017
| Country | Focus | Treatment Approach | Rounds >85% Through 2016 | Number of Communities | Population at Risk | Population No Longer at Risk | Population Eligible for Treatment | Status of Transmission | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Colombia | Lopez de Micay | 2×/year | 20 | 1 | 1366 | Eliminated in 2010 | |||||
| Ecuador | Esmeraldas | 2×/year | 25 | 119 | 25,863 | Eliminated in 2012 | |||||
| Mexico | North Chiapas | 2×/year | 17 | 13 | 7125 | Eliminated in 2010 | |||||
| Oaxaca | 2×/year | 18 | 98 | 44,919 | Eliminated in 2011 | ||||||
| South Chiapas | 2×/year | 25 | 396 | 83,218 | Eliminated in 2014 | ||||||
| 4×/year | 35 | 163 | 34,607 | ||||||||
| Focus total | 559 | 117 825 | |||||||||
| Guatemala | Escuintla | 2×/year | 13 | 117 | 62,590 | Eliminated in 2010 | |||||
| Santa Rosa | 2×/year | 16 | 37 | 12,208 | Eliminated in 2010 | ||||||
| Huehuetenango | 2×/year | 17 | 43 | 30,239 | Eliminated in 2011 | ||||||
| Central | 2×/year | 22 | 321 | 126 430 | Eliminated in 2014 | ||||||
| Venezuela | North central | 2×/year | 17 | 45 | 14,385 | Eliminated in 2013 | |||||
| Northeast | 2×/year | 20 | 330 | 73,212 | Eliminated in 2017 | ||||||
| 4×/year | 9 | 135 | 22,355 | ||||||||
| Focus total | 465 | 95,567 | |||||||||
| South | 2×/year | 16 | 66 | 4248 | 3744 | Ongoing | |||||
| 4×/year | 9 | 236 | 10,838 | 9273 | |||||||
| Focus total | 302 | 15,086 | 13,017 | ||||||||
| Brazil | Amazonas | 2×/year | 26 | 117 | 7209 | 5954 | Ongoing | ||||
| 4×/year | 13 | 122 | 8266 | 6634 | |||||||
| Focus total | 239 | 15,475 | 12,588 | ||||||||
| Regional total | 2359 | 30,561 | 538 517 | 25,605 | |||||||
Notes: Reprinted from Sauerbrey M, Lindsay JR, Richards FO Jr. Progress toward elimination of onchocerciasis in the Americas. Int Health. 2018;10:i71–i78, by permission of Oxford University Press.12
Onchocerciasis Elimination Challenges
Tremendous progress has been made towards the global elimination of onchocerciasis based on the current available data.2 Some potential improvements in approaches and technology have already been discussed above, but there are other challenges that directly threaten elimination effort. These challenges are likely to delay the achievement of elimination as outlined below:
Conflict and Civil Strife
This has affected the implementation of ivermectin MDA activities leading to anticipated delayed achievement of disease elimination. For example, DRC, South Sudan, Central African Republic, Angola and Côte d’Ivoire107,108 have had their annual geographic and therapeutic coverage rates affected. In DRC, inspite of continued fighting in eastern part of the country treatment coverage increased from 2001 to 2012 but they still did not reach the planned target.109 Involvement of relief organizations or armed personnel in MDA are options to be considered.
Loa Loa Co-Endemicity
The biggest obstacles to onchocerciasis elimination in countries where loasis occurs is that the expected treatment threshold required for elimination cannot be achieved due to fear of severe adverse events. Usually, people with high microfilarial loads of Loa loa are those who suffer severe and occasionally fatal encephalopathy reactions.110,111 In DRC, 14 people died in 2004 and this led to the temporary suspension of MDA.67 Improvements in handling these severe adverse events resulted from the implementation of the Rapid Assessment Procedures for Loasis (RAPLOA) mapping tool112 all over APOC countries, the utilization of the loascope113 and the ‘Test and Not Treat’ strategy.114 These new developments are anticipated to increase number of persons who can be safely treated.
Cross-Border Transmission
This has remained a big issue as countries strive to achieve elimination of onchocerciasis and other NTDs.115 Uncoordinated MDA across common borders have created problems in geographical and therapeutic coverages leading to sustained onchocerciasis transmission in a number of countries.116 For example, while Uganda has made great strides in the elimination of onchocerciasis, the last two foci to be eliminated are both cross-border between Uganda and DRC and South Sudan, respectively. Efforts to foster collaboration commenced in 2013, and this has registered some successes such as elimination of onchocerciasis in Bwindi focus through joint efforts of Uganda and DRC but has also met some challenges including language, logistics and insecurity to allow expedited joint implementation.117 Other collaborations in Africa like the Mano River Union are expected to provide good structures for Neglected Tropical Diseases collaboration.115 International collaborations to eliminate onchocerciasis in cross-border foci need to be given due attention.
Diagnostic Tools for Elimination
As most programs transition from control to verification of elimination, one of their main challenges is how their diagnostic needs will change. Verifying suppression and interruption of transmission in the context of the current WHO guidelines32 is important for programs. A good diagnostic test should be able to prove that infection no longer exists. In the absence of a highly specific test, most positive results are likely to be false positives, and the positive predictive value of the test will be very low. To minimize the number of false-positive results the number of people sampled can be increased to compensate for decreases in sensitivity.118 There are still outstanding issues on what type of serological Ov16 ELISA country elimination programs should adopt for decision-making. However, WHO-OTS has been providing guidance and encouraging further evaluations of diagnostic kits.34
Entomological Workforce
One of the criteria for verification of onchocerciasis elimination and stop MDA involves entomological assessment.32 This extends further to PTS that involves collection of flies and processing them by poolscreening; and the role of an entomologist or entomological technicians are vital. Most programs have inadequate or no entomological workforce to guide such important program activities. WHO-OTS recommended programs to address gaps in entomological staffing.34 The WHO Vector Control response 2017 also guides countries to build vector control capacity to enhance faster progress towards elimination.31
Motivation of Community Volunteers
Elimination can only be achieved when the program can attain not less than 80% treatment coverage; and the role of community drug distributors (CDDs) are critical. Maintaining the motivation and willingness of these CDDs is vital for programs. Low motivation and high attrition rates of CDDs have been reported in many countries.116 Lack of incentive has been identified as one of the causes and CDDs are also overloaded in other NTD interventions.119 Governments should take full ownership of their national elimination programs by allocating and mobilizing adequate resources for the intended goal.
Conclusion
Great strides have been made globally in the elimination of onchocerciasis. In Africa, although no country has been verified free of onchocerciasis, progress has been made to eliminate the disease in some limited localities with optimism that the continent will be able to achieve complete elimination in 12 countries by 2030. In the Americas, elimination of all onchocerciasis foci has been achieved, except a single focus (Yanomami) along the border of Brazil and Venezuela. Yemen has made some progress in elimination despite the civil strife. The global outlook in onchocerciasis elimination is promising; however, the need to address key challenges remains a priority to programs.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Rory Post reports personal fees from Sightsavers, The Carter Center, and The End Fund, outside the submitted work. The authors report no other potential conflicts of interest for this work.
References
- 1.Tekle AH, Elhassan E, Isiyaku S, et al. Impact of long-term treatment of onchocerciasis with ivermectin in Kaduna State, Nigeria: first evidence of the potential for elimination in the operational area of the African program for onchocerciasis control. Parasit Vectors. 2012;5:28. doi: 10.1186/1756-3305-5-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Progress report on the elimination of human onchocerciasis, 2018–2019. Wkly Epid Rec. 2019;94:513–524. [Google Scholar]
- 3.Mahdy MAK, Abdul-Ghani R, Abdulrahman TAA, et al. Onchocerca volvulus infection in Tihama region-west of Yemen: continuing transmission in ivermectin-targeted endemic foci and unveiled endemicity in districts with previously unknown status. PLoS Negl Trop Dis. 2018;12:1–16. doi: 10.1371/journal.pntd.0006329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Onchocerciasis and its control. report of a WHO expert committee on onchocerciasis control. World Health Organ Tech Rep Ser. 1995;852:1–104. [PubMed] [Google Scholar]
- 5.Bump JB, Benton B, Seketeli A et al. West Africa: river blindness- success in scaling up and lessons learned. scaling up poverty reduction: A Global Learning Process and Conference Shanghai, May 25–27, 2004. [Google Scholar]
- 6.Seketeli A. APOC at mid-point: so far so good. Ann Trop Med Parasitol. 2002;96(Suppl 1):S3–S4. doi: 10.1179/atm.2002.96.supplement1.001 [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization (WHO). Onchocerciasis control program in West Africa (OCP); 2018. Available from: http://www.who.int/apoc/onchocerciasis/ocp/en/(accessed on. Accessed May2, 2020.
- 8.Kurtak D, Meyer R, Ocran MH, et al. Management of insecticide resistance in control of the Simulium damnosum complex by the Onchocerciasis Control Program, West Africa: potential use of negative correlation between organophosphate resistance and pyrethroid susceptibility. Med Veterinary Entomol. 1987;1(2):137–146. doi: 10.1111/j.1365-2915.1987.tb00334.x [DOI] [PubMed] [Google Scholar]
- 9.Stokstad E, Vogel G. Neglected tropical diseases get the limelight in Stockholm. Science. 2015;350:144–145. doi: 10.1126/science.350.6257.144 [DOI] [PubMed] [Google Scholar]
- 10.Blanks J, Richards F, Beltrán F, et al. The Onchocerciasis Elimination Program for the Americas: a history of partnership. Rev Panam Salud Publica/Pan Am J Public Health. 1998;3(6):367–374. doi: 10.1590/S1020-49891998000600002 [DOI] [PubMed] [Google Scholar]
- 11.Dadzie Y, Neira M, Hopkins D. Final report of the Conference on the eradicability of Onchocerciasis. Filaria Jour. 2003;2(1):2. doi: 10.1186/1475-2883-2-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sauerbrey M, Lindsay JR, Richards FO Jr. Progress toward elimination of onchocerciasis in the Americas. Int Health. 2018;10:i71–i78.doi: 10.1093/inthealth/ihx039. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. Progress report on the elimination of human onchocerciasis, 2015–2016. Wkly Epid Rec. 2016;43:505–514. [Google Scholar]
- 14.Pan American Health Organization. Resolution CD49.R19. Elimination of neglected diseases and other poverty-related infections. PAHO, Regional office for the Americas, 2009. [Google Scholar]
- 15.World Health Organization. Certification of Elimination of Human Onchocerciasis: Criteria and Procedures. Geneva: WHO; 2001. [Google Scholar]
- 16.Büttner DW, von Laer G, Mannweiler E, Büttner M. Clinical, parasitological and serological studies on onchocerciasis in the Yemen Arab Republic. Tropenmed Parasitol. 1982;33:201–212. [PubMed] [Google Scholar]
- 17.Petrie PWR, Seal KS. Blue Skin Disease: A Medical Survey of the Western Aden Protectorate 1939–1940. London: Colonial Office; 1943. [Google Scholar]
- 18.Gasparini G. “Sowda”: a new disease or an unpublished type of onchocerciasis? Arch Ital Sci Med Trop Parasitol. 1962;43:635–646. [PubMed] [Google Scholar]
- 19.Omar MS, Franz M, Büttner DW. Some observations on onchocerciasis including sowda in the Yemen, Arab Republic. Tropenmed Parasitol. 1979;30:113–119. [PubMed] [Google Scholar]
- 20.Garms R, Kerner M. Anthropophily of Simulium damnosum s.l. and its role as a vector of human onchocerciasis in the Yemen, Arab Republic. Tropenmed Parasitol. 1982;33:175–180. [PubMed] [Google Scholar]
- 21.World Health Organization. WHO expert committee on onchocerciasis. Third report. World Health Organ. Tech Rep Ser. 1987;752:1–167. [PubMed] [Google Scholar]
- 22.World Health Organization. Sustaining the drive to overcome the global impact of neglected tropical diseases—second WHO report on neglected tropical diseases. Geneva:WHO; 2013. WHO/HTM/NTD/2013.1 Avialable from http://www.who.int/iris/bitstream/10665/77950/1/9789241564540 eng.pdf. Accessed May05 2020. [Google Scholar]
- 23.Fobi G, Yameogo L, Noma M, et al. Managing the fight against onchocerciasis in Africa: APOC Experience. PLoS Negl Trop Dis. 2015;9:e0003542. doi: 10.1371/journal.pntd.0003542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amazigo U. “The African Program for Onchocerciasis Control (APOC).”. Ann Trop Med Parasitol. 2008;102(Suppl 1):19–22. doi: 10.1179/136485908X337436 [DOI] [PubMed] [Google Scholar]
- 25.Hopkins AD. From ‘control to elimination’: A strategic change to win the end game. Int Health. 2015;7:304–305. doi: 10.1093/inthealth/ihv056 [DOI] [PubMed] [Google Scholar]
- 26.African Program for Onchocerciasis Control/World Health Organization. Conceptual and operational framework of onchocerciasis elimination with ivermectin treatment. World Health Organization/African Program for Onchocerciasis Control, 2010. WHO/APOC/MG/10.1, JAF 16.6 II. [Google Scholar]
- 27.Tekle AH, et al. Progress Towards Onchocerciasis Elimination in the Participating Countries of the African Programme for Onchocerciasis Control: epidemiological Evaluation Results. Infectious Diseases of Poverty. 2016;5(1):66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coffeng LE, et al. African programme for onchocerciasis control 1995-2015: model-estimated health impact and cost. PLoS Negl Trop Dis. 2013;7(1):e2032. doi: 10.1371/journal.pntd.0002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization.Progress report on the elimination of human onchocerciasis, 2015–2016. Wkly Epid Rec. 2016;91:505–514. [PubMed] [Google Scholar]
- 30.Hopkins AD. Neglected tropical diseases in Africa: A new paradigm. Int Health. 2016;8:i28–i33. doi: 10.1093/inthealth/ihv077 [DOI] [PubMed] [Google Scholar]
- 31.Fourth WHO Report on Neglected Tropical Diseases. Integrating Neglected Tropical Diseases into Global Health and Development. Geneva, Switzerland: WHO Press; 2017. [Google Scholar]
- 32.World Health Organization. Guidelines for Stopping Mass Drug Administration and Verifying Elimination of Human Onchocerciasis: Criteria and Procedures. Geneva, Switzerland: WHO Press; 2016. [PubMed] [Google Scholar]
- 33.Griswold E, Unnasch T, Eberhard M, et al. The role of national committees in eliminating onchocerciasis. Int Health. 2018;10:i60–i70. doi:doi: 10.1093/inthealth/ihx048. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization. Report of the Second Meeting of the WHO Onchocerciasis Technical Advisory Subgroup. Geneva, Switzerland: WHO Press; 2018. [Google Scholar]
- 35.Program Coordinating Committee and OEPA Staff. Guide to detecting a potential recrudescence of onchocerciasis during the post-treatment surveillance period: the American paradigm. Res Rep Trop Med. 2012;3:21–33. doi: 10.2147/RRTM.S30482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ngoumou P, Walsh JF, et al. A rapid mapping technique for the prevalence and distribution of onchocerciasis: a Cameroon case study. Ann Trop Med Parasitol. 1994;88:463–474. doi: 10.1080/00034983.1994.11812893 [DOI] [PubMed] [Google Scholar]
- 37.Katabarwa MN, Eyamba A, Chouaibou M, et al. Does onchocerciasis transmission take place in hypoendemic areas? A study in North Region of Cameroon. J Trop Int Hlth. 2010;15:645–652. doi: 10.1111/j.1365-3156.2010.02501.x [DOI] [PubMed] [Google Scholar]
- 38.World Health Organization. Report of the First Meeting of the WHO Onchocerciasis Technical Advisory Subgroup. Geneva, Switzerland: WHO Press; 2017. [Google Scholar]
- 39.World Health Organization. Africa region, the expanded special project for elimination of neglected tropical diseases (ESPEN): annual report-reaching everywhere towards 2020. WHO, Regional Office for Africa, 2018. [Google Scholar]
- 40.Thylefors B, Alleman MM, et al. “Operational lessons from 20 years of the mectizan donation program for the control of onchocerciasis. Trop Med Int Health. 2008;13(5):689–696. doi: 10.1111/j.1365-3156.2008.02049.x [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization. Preventive chemotherapy in human helminths. Coordinated use of anthelminthic drugs in control interventions In A Manual for Health Professionals and Programme Managers. 2006. [Google Scholar]
- 42.WHO Report. Strategies for Ivermectin Distribution Through Primary Health Care. Document WHO/PBL/91.24 Geneva: WHO;1991. [Google Scholar]
- 43.Pan American Health Organization. Resolution CD35.R14 Available from: https://iris.paho.org/bitstream/handle/10665.2/1551/CD35.R14en.pdf?sequence=1&isAllowed=y. Accessed May05 2020.
- 44.Progress towards eliminating onchocerciasis in the WHO Region of the Americas: verification of elimination of transmission in Guatemala. Wkly Epidemiol Rec. 2016;91(43):501–505. [PubMed] [Google Scholar]
- 45.Pan American Health Organization. Resolution CD55.R9 Plan of action for the elimination of neglected infectious diseases and post-elimination actions 2016–2022. PAHO, Regional Office for the Americas, 2016. [Google Scholar]
- 46.Abd-Elfarag G, Logora MY, Carter JY, et al. The effect of bi-annual community-directed treatment with ivermectin on the incidence of epilepsy in onchocerciasis endemic villages in South Sudan: a study protocol. Infect Dis Poverty. 2018;7:112. doi: 10.1186/s40249-018-0496-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Colebunders R, Stolk WA, Siewe Fodjo JN, et al. Elimination of onchocerciasis in Africa by 2025: an ambitious target requires ambitious interventions. Infect Dis Poverty. 2019;8:83. doi: 10.1186/s40249-019-0593-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hougard JM, Poudiougo P, Guillet P, et al. Criteria for the selection of larvicides by the onchocerciasis control program in West Africa. Ann Trop Med Parasitol. 1993;87(5):435±42. doi: 10.1080/00034983.1993.11812793 [DOI] [PubMed] [Google Scholar]
- 49.Lakwo TL, Garms R, Wamani J, et al. Interruption of the transmission of Onchocerca volvulus in the Kashoya-Kitomi focus, Western Uganda by long-term ivermectin treatment and elimination of the vector Simulium neavei by larviciding. Acta Trop. 2017;167:128–136. doi: 10.1016/j.actatropica.2016.12.029 [DOI] [PubMed] [Google Scholar]
- 50.Traoré S, Wilson MD, Sima A, et al. The elimination of the onchocerciasis vector from the island of Bioko as a result of larviciding by the WHO African Program for Onchocerciasis Control. Acta Trop. 2009;111:211–218. doi: 10.1016/j.actatropica.2009.03.007 [DOI] [PubMed] [Google Scholar]
- 51.Garms R, Lakwo TL, Ndyomugyenyi R, et al. The elimination of the vector Simulium neavei from the Itwara onchocerciasis focus in Uganda by ground larviciding. Acta Trop. 2009;111:203–210. doi: 10.1016/j.actatropica.2009.04.001 [DOI] [PubMed] [Google Scholar]
- 52.Katabarwa MN, Lakwo TL, Habomugisha P, et al. Transmission of Onchocerca volvulus by Simulium neavei in Mount Elgon focus of Eastern Uganda has been interrupted. Am Jour Trop Med Hyg. 2014;90:1159–1166. doi: 10.4269/ajtmh.13-0501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lakwo TL, Garms R, Tukahebwa E, et al. Successful interruption of the transmission of Onchocerca volvulus in Mpamba-Nkusi focus, Kibaale district, Mid-Western Uganda. E Afr Med Jour. 2015;72:1–7. [Google Scholar]
- 54.Rodriguez-Perez MA, Adeleke MA, Burkett-Cadena ND, et al. Development of a novel trap for the collection of black flies of the Simulium ochraceum complex. PLoS One. 2013;8:e76814. doi: 10.1371/journal.pone.0076814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rodriguez-Perez MA, Adeleke MA, Rodriguez-Luna IC, et al. Evaluation of a community- based trapping program to collect Simulium ochraceum sensu lato for verification of onchocerciasis elimination. PLoS Negl Trop Dis. 2014;8:e3249. doi: 10.1371/journal.pntd.0003249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rodriguez-Perez MA, Garza-Herna JA, Salinas-Carmona MC, et al. The esperanza window trap reduces the human biting rate of Simulium ochraceum s.l. in formerly onchocerciasis endemic foci in Southern Mexico. PLoS Negl Trop Dis. 2017;11(7):e0005686. doi: 10.1371/journal.pntd.0005686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Toé LD, Koala L, Burkett-Cadena ND, et al. Optimization of the Esperanza window trap for the collection of the African onchocerciasis vector Simulium damnosum sensu lato. Acta Trop. 2014;137:39–43. doi: 10.1016/j.actatropica.2014.04.029 [DOI] [PubMed] [Google Scholar]
- 58.Hendy A, Sluydts V, Tushar T, et al. Esperanza Window Traps for the collection of anthropophilic blackflies (Diptera: simuliidae) in Uganda and Tanzania. PLoS Negl Trop Dis. 2017;11(6):e0005688. doi: 10.1371/journal.pntd.0005688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Loum D, Cozart D, Lakwo TL, et al. Optimization and evaluation of the Esperanza Window Trap to reduce biting rates of Simulium damnosum sensu lato in Northern Uganda. PLoS Negl Trop Dis. 2019;13(7):e0007558. doi: 10.1371/journal.pntd.0007558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Loum D, Katholi CR, Lakwo T, et al. Evaluation of community-directed operation of black fly traps for entomological surveillance of Onchocerca volvulus transmission in the Madi-Mid North focus of onchocerciasis in Northern Uganda. Am J Trop Med Hyg. 2017;97(4):1235–1242. doi: 10.4269/ajtmh.17-0244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cheke RA, Garms R. Trials of attractants to enhance biconical trap catches of Simulium yahense and S. Sanctipauli s l Trop Med Parasit. 1987;38:62–63. [Google Scholar]
- 62.Davies JB. Sixty years of onchocerciasis control: a chronological summary with comments on eradication, reinvasion and insecticide resistance. Annu, Rev Entomol. 1994;39:23–45. doi: 10.1146/annurev.en.39.010194.000323 [DOI] [PubMed] [Google Scholar]
- 63.Benjamin GJ, Loum D, Lakwo TL, et al. Community-directed vector control to supplement mass drug distribution for onchocerciasis elimination in the Madi mid-North focus of Northern Uganda. PloS Negl Trop Dis. 2018;12(8):e0006702. doi: 10.1371/journal.pntd.0006702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Boussinesq M, Fobi G, Kuesel AC. Alternative treatment strategies to accelerate elimination of onchocerciasis. Int Hlth. 2018;10:i40–i48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gould F, Brown ZS, Kuzma J. Wicked evolution: can we address the sociobiological dilemma of pesticide resistance? Science. 2018;360(6390):728±32. doi: 10.1126/science.aar3780 [DOI] [PubMed] [Google Scholar]
- 66.Duerr HP, Raddatz G, Eichner M. Control of onchocerciasis in Africa: threshold shifts, breakpoints and rules for elimination. Int J Parasitol. 2011;41(5):581±9. doi: 10.1016/j.ijpara.2010.12.009 [DOI] [PubMed] [Google Scholar]
- 67.Stolk WA, Walker M, Coffeng LE, et al. Required duration of mass ivermectin treatment for onchocerciasis elimination in Africa: a comparative modelling analysis. Parasit Vect. 2015. 8 552. doi: 10.1186/s13071-015-1159-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Basanez MG, Walker M, Turner HC, et al. River blindness: mathematical models for control and elimination. Adv Parasitol. 2016;94:247±341. [DOI] [PubMed] [Google Scholar]
- 69.Smith ME, Bilal S, Lakwo TL, et al. Accelerating river blindness elimination by supplementing MDA with a vegetation “slash and clear” vector control strategy: a data-driven modeling analysis. Sci Rep. 2019;9:15274. doi: 10.1038/s41598-019-51835-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ending the neglect to attain the sustainable development goals a road map for neglected tropical diseases. 2021–2030.Geneva:World Health Organization. [Google Scholar]
- 71.Murdoch ME. Onchodermatitis: where are we now? Trop Med Infect Dis. 2018;3:94. doi:doi: 10.3390/tropicalmed3030094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gass KM. Rethinking the serological threshold for onchocerciasis elimination. PLoS Negl Trop Dis. 2018;12:e0006249. doi: 10.1371/journal.pntd.0006249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Weil GJ, Steel C, Liftis F, et al. A rapid-format antibody card test for diagnosis of onchocerciasis. J Infect Dis. 2000;182(6):1796–1799. doi: 10.1086/317629 [DOI] [PubMed] [Google Scholar]
- 74.Golden A, Steel C, Yokobe L, et al. Extended result reading window in lateral flow tests detecting exposure to Onchocerca volvulus: a new technology to improve epidemiological surveillance tools. PLoS One. 2013;8(7):e69231. doi: 10.1371/journal.pone.0069231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Steel C, Golden A, Stevens E, et al. Rapid point-of-contact tool for mapping and integrated surveillance of Wuchereria bancrofti and Onchocerca volvulus infection. Clin Vaccine Immunol. 2015;22(8):896–901. doi: 10.1128/CVI.00227-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dieye Y, Storey HL, Barrett KL, et al. Feasibility of utilizing the SD BIOLINE Onchocerciasis IgG4 rapid test in onchocerciasis surveillance in Senegal. PLoS Negl Trop Dis. 2017;11:e0005884. doi: 10.1371/journal.pntd.0005884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Basanez MG, Rodriguez-Perez MA, Reyes-Villanueva F, et al. Determination of sample sizes for the estimation of Onchocerca volvulus (Filarioidea: onchocercidae) infection rates in biting populations of Simulium ochraceum s.l. (Diptera: simuliidae) and its application to ivermectin control programs. J Med Entomol. 1998;35(5):745–757. doi: 10.1093/jmedent/35.5.745 [DOI] [PubMed] [Google Scholar]
- 78.Rodriguez-Perez MA, Fernandez-Santos NA, Orozco-Algarra ME, et al. Elimination of onchocerciasis from Mexico. PLoS Negl Trop Dis. 2015;9(7):e0003922. doi: 10.1371/journal.pntd.0003922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Richards F Jr, Rizzo N, Diaz Espinoza CE, et al. One hundred years after its discovery in Guatemala by Rodolfo Robles, Onchocerca volvulus transmission has been eliminated from the central endemic zone. Am J Trop Med Hyg. 2015;93(6):1295–1304. doi: 10.4269/ajtmh.15-0364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zarroug IM, Hashim K, ElMubark WA, et al. The first confirmed elimination of an onchocerciasis focus in Africa: abu Hamed, Sudan. Am J Trop Med Hyg. 2016;27:1037–1040. doi: 10.4269/ajtmh.16-0274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Katabarwa MN, Zarroug IMA, Negussu N, et al. The Galabat-Metema cross-border onchocerciasis focus: the first coordinated interruption of onchocerciasis transmission in Africa. PLoS Negl Trop Dis. 2020;14(2):e0007830. doi: 10.1371/journal.pntd.0007830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Unnasch TR, Golden A, Cama V, et al. Diagnostics for onchocerciasis in the era of elimination. Int Health. 2018;10:i20–i26. doi: 10.1093/inthealth/ihx047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Davies JB, Beech-Garwood PA, Thomson MC, et al. Onchocerciasis Transmission levels and Simulium damnosum complex biting activity at riverside and ricefield sites in Sierra Leone. Med Vet Entomol. 1988;2:357–369. doi: 10.1111/j.1365-2915.1988.tb00209.x [DOI] [PubMed] [Google Scholar]
- 84.Walsh JF, Garms R, Lakwo TL. Planning of focal vector Eradication in Onchocerciasis foci in Uganda. Tropical Disease Research/World Health Organization,1996. Report to UNDP/World Bank/WHO, Allotment No. GL/RES/TDR/045/FA/96/B. [Google Scholar]
- 85.Shannon MN, Kuesel AC, Crawford AE, et al. Genomic epidemiology in filarial nematodes: transforming the basis for elimination program decisions. Front Genet. 2019;10:1282. doi: 10.3389/fgene.2019.01282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Anon. Report of the 38th session of the Technical Consultative Committee (TCC). Ouagadougou:WHO; 2014. DIR/COORD/APOC/REP/TCC38 Available from: http://www.who.int/apoc/about/structure/tcc/TCC32_Final_Master_26_08_11.pdf?ua=1. Accessed January10, 2020. [Google Scholar]
- 87.Centers for Disease Control and Prevention, Global health, division of parasitic diseases. (2014) parasites: onchocerciasis (also known as river blindness). Available from: https://www.cdc.gov/parasites/onchocerciasis/health professionals/index.html. Accessed April30, 2020.
- 88.Eberhard ML, Cupp EW, Katholi CR, et al. Skin snips have no role in programmatic evaluations for onchocerciasis elimination: a reply to Bottomley et al. Parasites Vectors. 2017;10:154. doi: 10.1186/s13071-017-2090-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Thiele EA, Cama VA, Lakwo TL, et al. Detection of onchocerca volvulus in skin snips by microscopy and real-time polymerase chain reaction: implications for monitoring and evaluation activities. Am J Trop Med Hyg. 2016;94:906–911. doi: 10.4269/ajtmh.15-0695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Prince-Guerra JL, Cama VA, Wilson N, et al. Comparison of PCR methods for Onchocerca volvulus detection in skin snip biopsies from the Tshopo Province, Democratic Republic of the Congo. Am J Trop Med Hyg. 2018;98:1427–1434. doi: 10.4269/ajtmh.17-0809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mekonnen SA, Beissner M, Saar M, et al. O-5S quantitative real-time PCR: A new diagnostic tool for laboratory confirmation of human onchocerciasis. Parasites Vectors. 2017;10:451. doi: 10.1186/s13071-017-2382-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Globisch D, Moreno AY, Hixon MS, et al. Onchocerca volvulus-neurotransmitter tyramine is a biomarker for river blindness. Proc Natl Acad Sci USA. 2013;110:4218–4223. doi: 10.1073/pnas.1221969110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Quintana JF, Makepeace BL, Babayan SA, et al. Extracellular Onchocerca-derived small RNAs in host nodules and blood. Parasites Vectors. 2015;8:1–11. doi: 10.1186/s13071-015-0656-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lagatie O, Batsa-Debrah L, Debrah A, et al. Plasma-derived parasitic microRNAs have insufficient concentrations to be used as diagnostic biomarker for detection of Onchocerca volvulus infection or treatment monitoring using LNA-based RT-qPCR. Parasitol Res. 2017;116:1013–1022. doi: 10.1007/s00436-017-5382-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gonzalez-Moa MJ, Dorst BV, Lagatie O, et al. Proof-of-concept rapid diagnostic test for onchocerciasis: exploring peptide biomarkers and the use of gold nanoshells as reporter nanoparticles. ACS Inf Dis. 2018;4:912–917. doi: 10.1021/acsinfecdis.8b00031 [DOI] [PubMed] [Google Scholar]
- 96.River Blindness. The beginning of the end. Working together to eliminate onchocerciasis. NGDO Advocacy Paper. 2018. [Google Scholar]
- 97.Diawara L, Traore MO, Badji A, et al. Feasibility of onchocerciasis elimination with ivermectin treatment in endemic foci in Africa: first evidence from studies in Mali and Senegal. PLoS Negl Trop Dis. 2009;3:e497. doi: 10.1371/journal.pntd.0000497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tekle AH, Zouré HGM, Noma M, et al. Progress towards onchocerciasis elimination in the participating countries of the African program for onchocerciasis control: epidemiological evaluation results. Infectious Diseases of Poverty. 2016;5:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Joni L, Sodahlon YK. Onchocerciasis: the beginning of the end. Int Health. 2018;10:i1–i2. doi: 10.1093/inthealth/ihx070 [DOI] [PubMed] [Google Scholar]
- 100.Kim YE, Stolk WA, Tanner M, et al. Modelling the health and economic impacts of the elimination of river blindness (onchocerciasis) in Africa. BMJ Global Health. 2017;2:e000158. doi: 10.1136/bmjgh-2016-000158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Koala L, Nikiema A, Post RJ, et al. Recrudescence of onchocerciasis in the Comoé valley in Southwest Burkina Faso. Acta Trop. 2017;166:96–105. doi: 10.1016/j.actatropica.2016.11.003 [DOI] [PubMed] [Google Scholar]
- 102.Aceng JR.Uganda Leads the Fight in Africa in Successful Elimination of River Blindness/Onchocerciasis. The New Vision, Uganda: August15, 2019. [Google Scholar]
- 103.Katabarwa MN, Lakwo TL, Habomugisha P, et al. After 70 years of fighting an age-old scourge, onchocerciasis in Uganda, the end is in sight. Int Health. 2018;10:i79–i88. doi: 10.1093/inthealth/ihx044 [DOI] [PubMed] [Google Scholar]
- 104.World Health Organization. Ending the neglect to attain the sustainable development goals: a road map for neglected tropical diseases 2021–2030. Available from: https://creativecommons.org/licenses/by-nc-sa/3.0/igo. Accessed June26, 2020.
- 105.Vos T, Barber RM, Bell B, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systemic analysis for the global burden of disease study 2013. Lancet. 2015;386:743–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Nicholls RS, Duque S, Olaya LA, et al. Elimination of onchocerciasis from Colombia: first proof of concept of river blindness elimination in the world. Parasites Vectors. 2018;11:237. doi: 10.1186/s13071-018-2821-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hotez PJ, Kamath A. Neglected tropical diseases in sub-Saharan Africa: review of their prevalence, distribution, and disease burden. PLoS Negl Trop Dis. 2009;3(8):e412. doi: 10.1371/journal.pntd.0000412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bush S, Ngorok J. Elimination of onchocerciasis; Ten-year strategic fast tracking plan in Sightsavers supported countries 2011–2021. West Sussex: Sight savers; 2011. Available from: http://www.sightsavers.org/wp-content/uploads/2017/11/19377_0303_SS-Oncho-Report-Lowres.pdf. Accessed April16, 2020. [Google Scholar]
- 109.Makenga-Bof JC, Maketa V, Bakajika DK, et al. Onchocerciasis control in the Democratic Republic of Congo (DRC): challenges in a post-war environment. Trop Med Int Health. 2015;20:48–62. doi: 10.1111/tmi.12397 [DOI] [PubMed] [Google Scholar]
- 110.Gardon J, Gardon-Wendel N, Demanga-Ngangue KJ, et al. Serious reactions after mass treatment of onchocerciasis with ivermectin in an area endemic for Loa loa infection. Lancet. 1997;350:18–2210. doi: 10.1016/S0140-6736(96)11094-1 [DOI] [PubMed] [Google Scholar]
- 111.Boussinesq M, Gardon J, Gardon-Wendel N, et al. Clinical picture, epidemiology and outcome of Loa-associated serious adverse events related to mass ivermectin treatment of onchocerciasis in Cameroon. Filaria J. 2003;2((Suppl. 1)):. doi: 10.1186/1475-2883-2-S1-S4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zouré HGM, Wanji S, Noma M, et al. The geographic distribution of Loa loa in Africa: results of large-scale implementation of the Rapid Assessment Procedure for Loiasis (RAPLOA). PLoS Negl Trop Dis. 2011:5 e1210.10.1371/journal.pntd.0001210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Emukah E, Rakers LJ, Kahansim B, et al. Southern Nigeria Loa loa blood microfilaria density is very low even in areas with high prevalence of loiasis: results of a survey using the new loascope technology. Am J Trop Med Hyg. 2018;99(1):116–123. doi: 10.4269/ajtmh.18-0163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kamgno J, Pion SD, Chesnais CB, et al. A test-and-not-treat strategy for onchocerciasis in Loa loa-endemic areas. N Engl J Med. 2017;377(21):2044–2052. doi: 10.1056/NEJMoa1705026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Gustavsen K, Sodahlon Y, Bush S. Cross-border collaboration for neglected tropical disease efforts—Lessons learned from onchocerciasis control and elimination in the Mano River Union (West Africa). Glob Health. 2016;12(1):44. doi: 10.1186/s12992-016-0185-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Gebrezgabiher G, Mekonnen Z, Yewhalaw D, et al. Reaching the last mile: main challenges relating to and recommendations to accelerate onchocerciasis elimination in Africa. Infectious Diseases of Poverty. 2019;8:60. doi: 10.1186/s40249-019-0567-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lakwo TL, Ukety T, Bakajika D, et al. Cross border collaboration in onchocerciasis elimination in Uganda: progress, challenges and opportunities from 2008 to 2013. Glob Health. 2018;14(1):16. doi: 10.1186/s12992-018-0333-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Johnson WO, Su CL, Gardner IA, et al. Sample size calculations for surveys to substantiate freedom of populations from infectious agents. Biometrics. 2004;60(1):165–171. doi: 10.1111/j.0006-341X.2004.00143.x [DOI] [PubMed] [Google Scholar]
- 119.Mathauer I, Imhoff I. Health worker motivation in Africa: the role of non-financial incentives and human resource management tools. Hum Resour Health. 2006;4(1):24. doi: 10.1186/1478-4491-4-24 [DOI] [PMC free article] [PubMed] [Google Scholar]