Abstract
Objective:
The aim of this study was to evaluate if small group teaching in Radiology impacted Anatomy scores in the summative end of year examination.
Methods:
Small group teaching in Radiology was incorporated into Anatomy of year one medical students during the academic years 2016/17 and 2017/18. Examination outcome for 2 years before and 1 year after the study period were compared.
Question papers for end of year summative examinations were retrieved; questions relating to Anatomy were identified and anonymised scores for students were obtained.
Results:
Student numbers ranged 238 to 290/year. Mean Anatomy scores ranged 62–74%, this compared with mean total exam score of 62–65%. No significant difference in Anatomy and Total examination scores for 2015, 2016 and 2019. Mean (SD) Anatomy scores were significantly higher than the Total examination scores for the study period of 2017 and 2018 [68.97 (17.32) vs 63.12 (11.51) and 73.77 (17.85) vs 64.99 (10.31) (p < 0.001)]. Combined Anatomy scores 2017 and 2018 were significantly higher than 2015 and 2016, difference of 5.50 (95% C.I. 3.31–7.70; p < 0.001).
Conclusion:
This is the first study to objectively demonstrate Radiology small group teaching significantly improved Anatomy scores for medical students in the summative end of year examination.
Advances in knowledge:
No evidence in the literature that Radiology teaching improves examination outcomes for medical students.
This is the first study to directly link Radiology teaching with improved Anatomy examination result.
Small group teaching in Radiology is a feasible way to teach Anatomy.
Introduction
Undergraduate medical curricula have undergone significant evolution in the last 20 years with many Medical Schools moved from the “traditional” pre-clinical basic science/clinical medicine model towards an integrated, clinically oriented, problem-based learning (PBL) one. As a result, formal Anatomy teaching and dissection have often been left out. Medical Schools perform a careful balancing act, in an ever evolving and crowded undergraduate medical curriculum, to decide which new subject / material is added or indeed removed from the student’s time table. Radiology has been espoused as a valuable tool to teach anatomy since 1927.1 Professor RJ Scothorne, Professor of Anatomy Medical School, Newcastle upon Tyne and Regius Professor of Anatomy, University of Glasgow said “I am sure that it is better to teach (radiology) in an integrated fashion, as the student deals with the various organs, rather than as a block of “radiological anatomy” at the end of the anatomy course as used to be done in some schools.”2(1970).
A recent extensive review of almost 100 years of literature on the role of radiology in medical student education has demonstrated 100 fold increase in publications since 1950s3. However, most articles were expository in nature. Less than 3% were truly experimental, with small student numbers, diverse topics and generally of poor quality. None demonstrated a direct correlation between radiology teachings with student summative assessment result.
About 8 years ago, our institution moved from an almost entirely PBL-based curriculum to one using integrated teaching. Formal anatomy teaching was reintroduced into the curriculum together with Radiology to bridge the gap between the basic science and clinical medicine.
Objective
The aim of this retrospective study was to evaluate if small group teaching in Radiology impacted medical students’ Anatomy scores at the end of year summative examination.
Methods
Institutional Board Review approval was waived by our institution, as this work was considered part of normal practice for evaluation of teaching and learning.
Anatomy in the curriculum
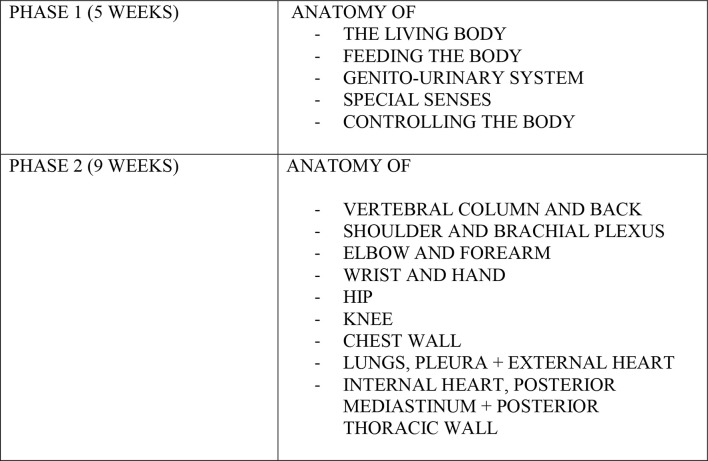
Our institution follows an integrated, “spiral” curriculum as recommended by the General Medical Council – where subject material is revisited at different stages of the curriculum with increasing depth and clinical focus. Anatomy is taught to medical students in the first 2 years of medical school – comprising lectures and laboratory work. In the first year, there is a 5 week “Introduction to Anatomy” (Phase 1), followed by 6 weeks of “Anatomy of the Limbs and Back” and 3 weeks of “Anatomy of the Cardiovascular and Respiratory Systems” (Phase 2). Anatomy laboratory work in Phase 2 comprises of 90 min “wet” cadaveric dissection and 90 min “dry” examination of ready prepared prosection specimen. These laboratory sessions are repeated three times to accommodate the large cohort of students (Figure 1).
Figure 1.
Anatomy curriculum for first year medical students.
Radiology in the curriculum
Radiology was introduced as a vertical theme in our institution in 2010 – spanning all 5 years of undergraduate medical curriculum.
Radiology was initially only involved in Phase 1 of Anatomy teaching(Table 1). During the academic years 2016/17 and 2017/18, Radiology was incorporated as an additional component into the existing “dry” laboratory segments of Phase 2 on a trial basis, and not as part of a research project. This comprised an overview 10 min didactic lecture of the Radiologic Anatomy relevant to that week’s subject, followed by rotating small student groups visiting the Radiology “station.” At the Radiology station, small groups of students (approximately 6) were shown radiologic images of common clinical scenarios pertaining to that week’s region of interest – presented in a quiz format. These interactive Radiology sessions were led by a Consultant Radiologist (Attending) with the assistance of a Radiology Registrar (Resident). There was no change to the timing allocated nor the number of dry prosection specimens that was presented to the students. Total overall time dedicated to Anatomy teaching was unchanged.
Table 1.
Radiologic Anatomy teaching for first year medical students
| Phase 1 (5 weeks) | Phase 2 (9 weeks) |
| 2014/15 & 2015/16 Introduction Radiologic Anatomy: - Small Rotating Groups shown normal radiologic images to demonstrate that week’s anatomy being studied (15 min) - Didactic / Show-and-Tell Style - 12 h Tutor time per week - 15 min Student time per week |
2014/15 & 2015/16 No Radiology Input 90 min “dry lab” – a handful of prosected specimen placed in the lab for studentself directed learning 90 min “wet lab” – cadaveric dissection |
| 2016/17 & 2017/18 Introduction Radiologic Anatomy: - Small Rotating Groups shown normal radiologic images to demonstrate that week’s anatomy being studied (15 min) - Didactic / Show-and-Tell Style - 12 h Tutor time per week - 15 min Student time per week |
2016/17 & 2017/18 90 min “dry lab” – a handful of prosected specimen placed in the lab for student self directed learning - Short introductory lecture of normal anatomy using radiologic Images to 1/6th year group (20 min) x 6 - Radiology “Station” - Short Quiz onclinically relevant radiologic images of common pathology involving that week’s anatomy being studied. (20 min) - Small rotating groups of 4–6 students visit the station - 12 h Tutor time per week - 40 min Student time per week 90 min “wet lab” – cadaveric dissection |
| 2018/19 Introduction Radiologic Anatomy: - Small Rotating Groups shown normal radiologic images to demonstrate that week’s anatomy being studied (15 min) - Didactic / Show-and-Tell Style - 12 h Tutor time per week - 15 min Student time per week |
2018/19 - No Radiology Input - No “dry lab” 180 min “wet lab” - cadaveric dissection handful of prosected specimen scattered around the dissection lab for self directed learning. |
In 2018/19, the “dry” lab component, where small group Radiologic anatomy was taught, was discontinued in favour of 3 h of “wet” cadaveric dissection only. This decision was taken by the Anatomy Department who collectively felt students would benefit from more anatomy teaching through cadaveric dissection.
Examination
First year students sit a summative end of year examination – comprising two papers covering all the subjects taught throughout that year in basic and system based biomedical science, as well as vocational studies and general practice. Paper 1 comprised of short answer questions (SAQ); Paper 2 comprised of SAQ, as well as multiple choice questions (MCQ). In 2018/19, the examination format changed slightly – with MCQs included in both papers. Anatomy was equally represented in both SAQ and MCQ at around a fifth of weighted score. However, as multiple subjects were frequently examined within one stem SAQ, it was not possible to extract the anatomy component from the tabulated score for that question. Therefore for the purpose of this study, only Anatomy MCQ scores were considered.
Question papers for end of year 1 summative examinations were retrieved for academic years 2015–2019. This 5 year period was chosen to reflect the baseline 2 years before the increased Radiology input; the 2 years with increased Radiology input; and the year after increased Radiology was discontinued. The questions relating to Anatomy were identified. Anonymised scores for students in each year were retrospectively obtained. The mean Anatomy as well as the total exam scores were calculated for each exam cycle.
Statistical methods
Exam scores (whole exam and anatomy only) were modelled using a year and exam as predictors. This was done using a general linear model in Minitab (v. 18) at a 5% significance level. An interaction between exam and year was included. Post-hoc comparisons were done using a Bonferroni correction factor to adjust for multiple comparisons. To control for variability in student scores between the years, Anatomy MCQ scores were charted against the Total examination scores (MCQ + SAQ) for each year. In addition, Total examination and Anatomy scores were compared taking 2015 as a baseline.
Results
The total number of students per year ranged from 238 to 290. Mean Anatomy MCQ scores ranged from 62 to 74% while median Anatomy MCQ score was between 62 and 75%. This compared with mean Total examination score of between 62 and 65% and median total exam score of 63–66% (See Tables 2 and 3). The number of questions in Anatomy averaged 21.67% (65 out of a possible 300) of the total MCQ over the 5 years studied. Each correctly answered MCQ scored one point. Total examination – MCQ and SAQ – score possible during the 5 year period was 1140 points.
Table 2.
Anatomy exam scores over time: statistics
| Variable | Year | N | Mean | StDev | Median | Interquartile range |
|---|---|---|---|---|---|---|
| Score | 2015 | 238 | 65.85 | 18.57 | 71.43 | 57.14–85.71 |
| 2016 | 241 | 65.89 | 15.87 | 70.00 | 60.00–80.00 | |
| 2017 | 250 | 68.97 | 17.32 | 75.00 | 58.33–83.33 | |
| 2018 | 251 | 73.77 | 17.85 | 75.00 | 58.33–91.67 | |
| 2019 | 290 | 62.23 | 14.06 | 62.50 | 54.17–75.00 |
Table 3.
Total exam scores over time: statistics
| Variable | Year | N | Mean | StDev | Median | Interquartile range |
|---|---|---|---|---|---|---|
| Score | 2015 | 238 | 64.97 | 9.20 | 65.33 | 59.08–71.74 |
| 2016 | 241 | 65.68 | 9.57 | 65.65 | 60.65–72.61 | |
| 2017 | 250 | 63.12 | 11.51 | 64.63 | 55.63–71.18 | |
| 2018 | 251 | 64.99 | 10.31 | 65.87 | 58.70–71.96 | |
| 2019 | 290 | 62.53 | 12.49 | 63.13 | 54.97–71.46 |
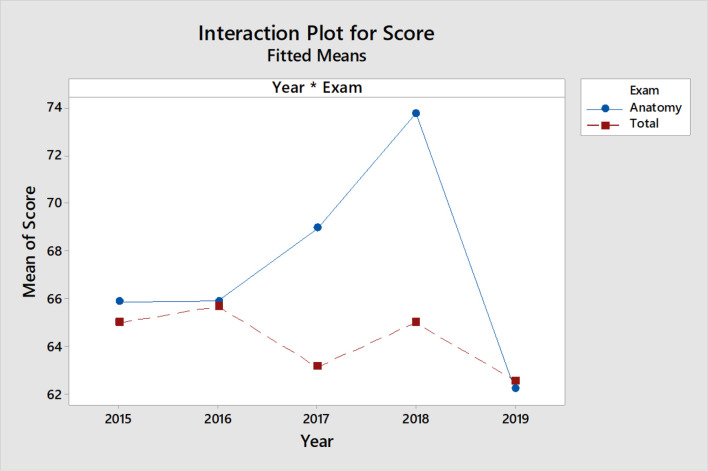
There was no significant difference in mean Anatomy and mean Total examination scores for 2015, 2016 and 2019. However, mean (SD) Anatomy scores were significantly higher than the Total examination scores for the trial period of 2017 and 2018 [68.97 (17.32) vs 63.12 (11.51) and 73.77 (17.85) vs 64.99 (10.31) (p < 0.001)]. This is illustrated in the interactive plot (Figure 2).
Figure 2.
Interaction plot for Anatomy and Total examination score
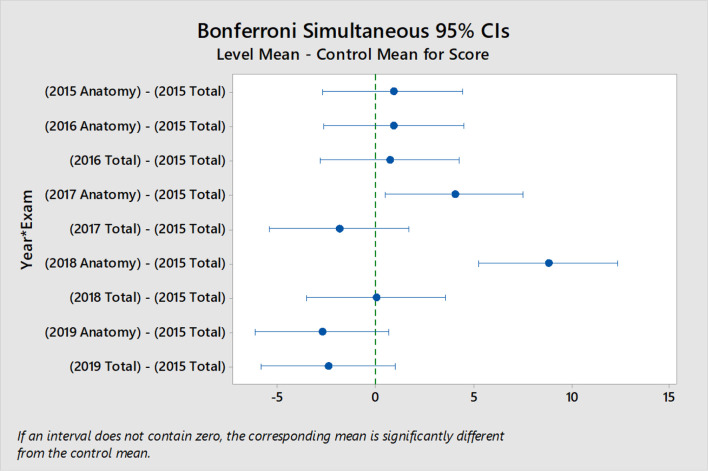
Although the Total examination score varied over time (Table 3), taking 2015 as a baseline, there was no significant difference between the 5 years studied. In contrast, Anatomy scores for 2017 and 2018 were significantly higher than the baseline (p = 0.016 for 2017 and p < 0.001 for 2018 - Figure 3). In addition, combined Anatomy scores for 2017 and 2018 were significantly higher than scores of 2015 and 2016, difference 5.50 (95% C.I 3.31–7.70, p < 0.001).
Figure 3.
Bonferroni simultaneous tests for level mean – control mean (2015 total score). Values are mean and 95% CI. CI, confidence interval
Discussion
This study shows that small group teaching in Radiology to first year medical students significantly improved Anatomy MCQ scores at the end of year examination. This comprised of lectures as well as quizzes pertaining to that week’s Anatomy topic using Radiologic images and common clinical scenarios. Radiology had no impact on overall examination scores – this is not surprising as MCQ in Anatomy represented around 6% of the total possible score in end of year examinations. Anatomy was also examined as part of SAQ, but as stated in the methods, it was not possible to determine the anatomy only component of each student’s summative score from the way data were collated and was therefore omitted from this evaluation. Anatomy MCQ scores in 2019 returned to pre-small group Radiology teaching levels after the study period.
Small group teaching has previously been shown to be beneficial to students.4 One of the drawbacks of small group teaching, however, is the labour intensive nature of this approach. In this study, the ratio of student exposure to tutor time was 1:18. In other words, every 1 min of student teaching required 18 min of tutor time; this did not include the time taken to prepare for what is being taught (Figure 1and Table 1). One way medical schools have dealt with this for problem based learning has been to employ non-medical trained personnel to deliver pre-prepared teaching. This may not work in an area where the expertise of the Radiologist may be the key to improved outcome. In our study, students in the small groups were given the opportunity to freely ask clinically relevant questions to an experienced clinician, which may help in the way they processed and retained information.
While many studies have demonstrated high student satisfaction with using Radiology to teach Anatomy, there are limited data to objectively demonstrate Radiology teaching having a direct and measureable impact on Anatomy performance in asummative examination.3,5 Studies have also shown that just having radiological images – without accompanying clinical contact and context – did not help students learn.6
Radiology, using real clinical scenarios and images, bridges the gap between Anatomy and Clinical Medicine. It allows for “authentic learning” – bringing clinical meaning to what the student is learning in Anatomy.7 Our small group instruction with quiz model also allows for deep, active learning through close interaction with a practicing Clinical Radiologist. Small group learning is associated with increased student interest, retention of knowledge and skills, enhances transfer of concepts to innovative issues and improves self-directed learning.7 It also facilitates an adult style of learning and acceptance of personal responsibility for own progress. Moreover, it enhances student–faculty and peer–peer interaction and allows clarification on points of bafflement.8 The prolonged (14 week), close weekly student–faculty contact in our study could promote successful student integration at this early stage of University life, improving student well-being and academic outcome – as described by Tinto, Astin and Umbach et al.9–12
Potential limitations of the study
This study was done evaluating only MCQ – the anatomy contribution to the written questions and students’ performance there was not evaluated. This was because written questions assessed multiple subjects per question and marked on the overall response, making it impossible to single out the anatomy component. Anatomy MCQ allowed a clean data set to be evaluated and correlated to the final total score. Although the number of questions which related to Anatomy was not standardised, it did not differ significantly between the years. Furthermore, it was made statistically unimportant by the large sample of students in each year of the study period.
No control group was included or possible in this retrospective observational study. The overall ability of each student year cohort is also not controlled for. However, charting the Anatomy score against the overall total examination score of the cohort year in the interaction plot mitigated against this.
There is of course no evidence that the findings from this study will translate into improved clinical knowledge when these students start to practice as clinicians. Trials are required in this area where medical students studying anatomy are randomly allocated to small group teaching in radiology versus standard anatomy teaching. The early end points could include independent assessment of student satisfaction and score outcomes across all examinations. Further assessment could evaluate if this translates in better clinical performance.13 Until this happens, and direct correlational longitudinal information is available, it would be unrealistic to expect radiology small group teaching to be implemented by medical schools based on our findings alone.
Conclusions
This is the first study, to the best of our knowledge, to objectively demonstrate Radiology small group teaching significantly improving Anatomy scores for medical students in the MCQ component of the summative end of year examination. Further studies are required in this area to establish whether these findings are reproducible, as it could have significant implications for Anatomy teaching of medical students in the future.
Footnotes
Acknowledgment: Dr Nigel Raby for his years of support and his work in Radiology teaching to medical students, and Ms Suzanne McDowall for her help in getting the students’ anonymised scores.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
C Chew, Email: chewszewan@aol.com.
David Young, Email: david.young@strath.ac.uk.
REFERENCES
- 1.Bardeen CR. The use of radiology in teaching anatomy. Radiology 1927; 8: 384–6. doi: 10.1148/8.5.384 [DOI] [Google Scholar]
- 2.Smart G. The place of radiodiagnosis in the undergraduate medical curriculum. Proc R Soc Med 1970; 63: 837–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Chew C, Cannon P, O’Dwyer PJ. Radiology for medical students (1925–2018): an overview. BJR Open 2020; 1: 20190050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferris H. The use of small group tutorials as an educational strategy in medical education. Int J of Higher Ed 2015; 4: 225–8. [Google Scholar]
- 5.Marker DR, Bansal AK, Juluru K, Magid D. Developing a Radiology-Based teaching approach for gross anatomy in the digital era. Acad Radiol 2010; 17: 1057–65. doi: 10.1016/j.acra.2010.02.016 [DOI] [PubMed] [Google Scholar]
- 6.Boon JM, Meiring JH, Richards PA. Clinical anatomy as the basis for clinical examination: development and evaluation of an introduction to clinical examination in a problem-oriented medical curriculum. Clin Anat 2002; 15: 45–50. doi: 10.1002/ca.1091 [DOI] [PubMed] [Google Scholar]
- 7.Pawlina W, Drake RL. Authentic learning in anatomy: a primer on pragmatism. Anat Sci Educ 2016; 9: 5–7. doi: 10.1002/ase.1592 [DOI] [PubMed] [Google Scholar]
- 8.Meo SA. Basic steps in establishing effective small group teaching sessions in medical schools. Pak J Med Sci 2013; 29: 1071–6. doi: 10.12669/pjms.294.3609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tinto V. ed.Rethinking the causes and cures of student attrition. 2nd. Chicago: University of Chicago Press; 1993. [Google Scholar]
- 10.Tinto V. Linking the learning and leaving: Exploring the role of the college classroom in student departure. In: Braxton J. M, ed.Reworking the student departure puzzle . Nashville: Vanderbuilt University Press; 2000(pp81-94).. [Google Scholar]
- 11.Astin A. What matters in college: Four critical years revisited. San Francisco: Jossey Bass Higher and Adult Education Series; 1993. [Google Scholar]
- 12.Umbach PD, Wawrzynski MR. Faculty do matter: the role of college faculty in student learning and engagement. Res High Educ 2005; 46: 153–84. doi: 10.1007/s11162-004-1598-1 [DOI] [Google Scholar]
- 13.McManus IC, Harborne AC, Horsfall HL, Joseph T, Smith DT, Marshall-Andon T, et al. Exploring UK medical school differences: the MedDifs study of selection, teaching, student and F1 perceptions, postgraduate outcomes and fitness to practise. BMC Med 2020; 18: 136. doi: 10.1186/s12916-020-01572-3 [DOI] [PMC free article] [PubMed] [Google Scholar]