Abstract
Patient: Female, 79-year-old
Final Diagnosis: Cervical spinal epidural hematoma
Symptoms: Neck pain • unilateral weakness
Medication: —
Clinical Procedure: —
Specialty: Neurosurgery • Orthopedics and Traumatology
Objective:
Rare disease
Background:
This report presents the case of a woman with no known coagulopathy, use of anticoagulants, or history of trauma who spontaneously developed an epidural hematoma of the spine. This is an uncommon condition, with the potential for missed diagnosis and potential harm to the patient.
Case Report:
The patient was an elderly woman with a history of Type 2 diabetes mellitus and hyperlipidemia. Of note, she had recently recovered from COVID-19. Because the woman presented with right-sided weakness and pain in the back of her neck, the stroke team was activated. A computed tomography (CT) scan of her neck revealed a very subtle hyperdensity, which on further investigation was found to be an acute epidural hematoma at C2–C3 space through the C6 vertebra. While awaiting surgery, the patient had spontaneous improvement of her right-sided weakness and her condition eventually was managed conservatively.
Conclusions:
Spontaneous spinal epidural hematoma is an uncommon condition, and a high index of suspicion is required to accurately diagnose and appropriately manage it. In the case presented here, the hematoma was subtle on the CT scan, and the patient’s weakness easily could have been misdiagnosed as an ischemic stroke. That may have resulted in administration of thrombolytics, potentially causing significant harm. In addition, the patient had recently recovered from COVID-19 disease, which may or may not be incidental. Further observation will be required to determine if there is a spike in similar cases, which may be temporally associated with the novel coronavirus.
MeSH Keywords: COVID-19; Hematoma, Epidural, Spinal; Spinal Stenosis
Background
Emergency physicians commonly encounter patients who present with unilateral weakness. The most common cause is an ischemic stroke; intracranial hemorrhage is less common. In the presence of neck pain, however, other less common differential diagnoses should be considered, and relevant imaging ordered to identify the underlying pathology.
Case Report
The patient was a 79-year-old woman with a history of Type 2 diabetes mellitus and hyperlipidemia. She had no significant history of tobacco smoking, alcohol use, or substance abuse.
Of note, the patient had recovered from a mild case of pneumonia caused by the 2019 novel coronavirus disease (COVID-19) 2 1/2 months prior to presentation. The woman was diagnosed with COVID-19 based on results of nasopharyngeal swab testing. At that time, she was asymptomatic and the testing was done as part of contact tracing and active surveillance when one of her family members was diagnosed with the disease. The diagnosis was confirmed with reverse transcription polymerase chain reaction. When a subsequent chest X-ray revealed slight haziness in the woman’s lungs, she was diagnosed with mild pneumonia. Based on national policy at the time for patients with COVID-19, she was admitted to the hospital and isolated for 14 days, from the middle to the end of February 2020. During that stay, she had only mild upper respiratory tract symptoms and the only medication she required was for them. She was never intubated, did not require ventilatory assistance, and did not receive any antiviral drugs or other specific therapy for COVID-19, such as hydroxychloroquine or plasma therapy. After 2 further swab tests returned negative results, she was discharged.
In mid-May 2020, the patient was brought by ambulance to the Emergency Department (ED) with a complaint of right-sided weakness and pain in the back of her neck. Twelve hours before, she had gone to sleep. She noted the symptoms when she woke up 9 hours after that.
The woman had weakness in her right upper and lower limbs but not in her face. She had no radicular symptoms and no history of recent trauma or neck manipulation.
On examination, the patient appeared lethargic but her Glasgow Coma Scale score was 15. She was able to answer questions and follow simple commands.
Examination of the woman’s cranial nerves was unremarkable and her face looked symmetrical. On a scale from 0 to 5, neurological examination of her limbs revealed a power of 3 in her right upper limb, 2 in her right lower limb, and 4 in her left upper and lower limbs. Sensation was preserved in her limbs. The woman had an extensor plantar reflex on her right side and a flexor plantar reflex on her left side. The results of examinations of her heart, lungs, and abdomen were unremarkable.
In view of the patient’s unilateral weakness, the Stroke Team had been activated upon her arrival in the ED, and she was sent for urgent imaging scans. In addition to a computed tomography (CT) scan of her brain, a CT scan of her cervical spine and CT angiography were ordered. The latter was performed to rule out a carotid or vertebral artery dissection, given the patient’s neck pain.
The CT scans revealed a subtle hyperdensity (Figure 1) within the posterior aspect of the spinal canal from the C3–4 through C6 vertebrae, raising suspicion for an acute epidural/subdural hematoma. The patient’s cervical spine was otherwise unremarkable, and there was no evidence of dissection or significant stenosis in the carotid, vertebrobasilar, or intracranial arteries. Apart from chronic microvascular ischemic changes, no significant abnormalities were noted in the brain.
Figure 1.
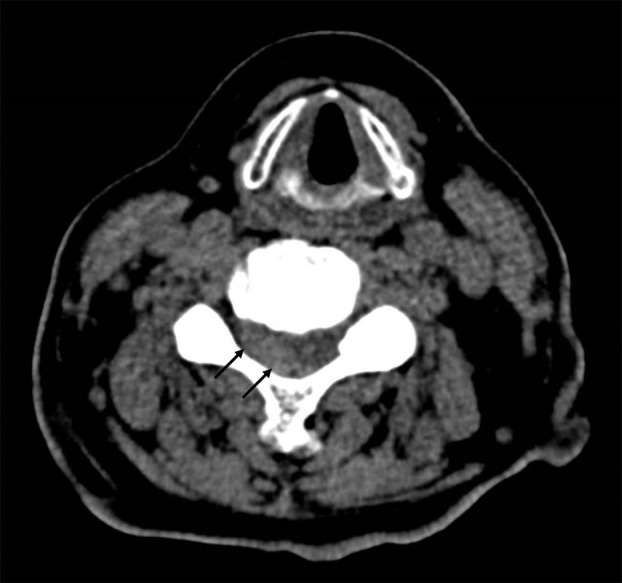
Transverse view of non-contrast computed tomography scan of the cervical spine at the C4 vertebra. The image shows subtle hyperdensity (arrows) in the posterior aspect of the spinal canal, which could easily have been missed. This raised suspicion for an acute epidural/subdural hematoma and prompted magnetic resonance imaging.
A magnetic resonance imaging (MRI) scan of the brain and cervical spine done immediately thereafter revealed an acute epidural hematoma that spanned the right posterior aspect of the C2–C3 space through the C6 vertebra. There was associated moderate to severe spinal canal stenosis with spinal cord deviation anteriorly and to the left side, which was worst at the C4–C5 vertebrae (Figure 2, 3). There was no signal change in the spinal cord, nor was there evidence of a large arteriovenous malformation in the woman’s cervical spine. The MRI of the brain showed no acute infarct or intracranial hemorrhage, and no significant stenosis or aneurysm was seen on MR angiography.
Figure 2.

Sagittal magnetic resonance image of the cervical spine (T2-weighted). The image shows an acute epidural hematoma (arrows) spanning the C2–C3 space to the C6 vertebra.
Figure 3.
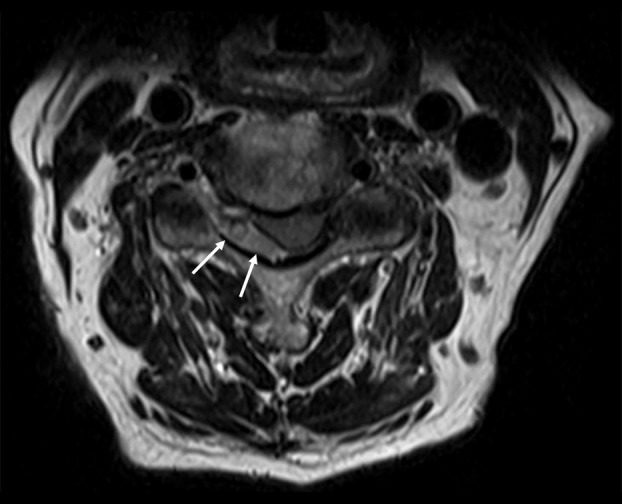
A transverse magnetic resonance image of the C4 vertebra (T2-weighted). The image shows the acute epidural hematoma (arrows). There is associated spinal canal stenosis with spinal cord deviation anteriorly and on the left side.
The patient was admitted to the High-Dependency ward in the Orthopedic Surgery Department. She was given intravenous dexamethasone for 3 days (8 mg TID), followed by oral dexamethasone for another 3 days (4 mg TID) and decompression surgery was planned. While awaiting the procedure, however, the patient had spontaneous improvement in her right-sided weakness; therefore, the treatment plan was changed to conservative management with close monitoring.
Results of blood testing revealed that the patient had normal prothrombin and activated partial thromboplastin times and a normal platelet count. A subsequent work-up by specialists from the Hematology Department revealed no blood clotting disorder.
The woman was discharged 6 days after presentation, by which time, her symptoms had improved significantly and she had only mild residual weakness in her right upper limb. She was scheduled for further outpatient rehabilitation and occupational therapy. No repeat imaging was done prior to discharge to confirm that her hematoma had improved.
Discussion
In a patient who has unilateral weakness, it is important to think broadly about the differential diagnosis, especially when symptoms are present that are atypical for an ischemic stroke (such as the neck pain in the case described here). In patients with neck pain and neurological signs, we often include carotid/vertebral artery dissection in the differential diagnosis. However, the present case illustrates an uncommon cause of such symptoms that also should be considered. Failure to recognize the significance of neck pain and to order imaging scans of the neck could have resulted in misdiagnosis of ischemic stroke. If such a misdiagnosis had occurred within a specific window of time, it might have resulted in administration of thrombolytics, which could have caused the patient significant harm.
Spontaneous spinal epidural hematoma is uncommon, with an estimated incidence of 0.1 per 100 000 patients per year [1]. It is even rarer in patients with no known coagulopathy, who are not on anticoagulants or antiplatelets, and have no history of trauma or prior spinal instrumentation or manipulation. Spontaneous spinal epidural hematoma is associated with significant morbidity, because it can cause disabling neurological deficits, and approximately 50% of patients do not recover fully [2].
According to the available literature, most patients with the condition present with back or neck pain, often with a radicular component, followed by motor and/or sensory deficits [3]. In such cases, a CT scan should be done, as it is an easily available initial imaging modality, whereas MRI is valuable for better defining the location and extent of a hematoma [4]. Emergent decompression surgery is generally the mainstay of treatment for this condition, with earlier surgery providing better neurological outcomes [5–7]. The patient in the present case report, however, had no radicular symptoms, and her symptoms resolved spontaneously.
A review of the literature revealed several other reports of spontaneous improvement and studies of conservative management for spinal epidural hematoma. Initial neurologic function is a strong predictor of neurologic recovery (in patients managed surgically or conservatively), and conservative management can be considered in patients who present with milder neurologic deficit, or in those who show early signs of functional recovery [8–10]. Patient age and sex [8] and hematoma length (i.e. number of vertebral segments affected) [11] do not appear to have any prognostic significance.
The present case also is interesting, in that the patient had recently recovered from a mild pneumonia caused by COVID-19, which may or may not be incidental, and raises the question if the hematoma could be an unexpected association with the disease. Because COVID-19 is new, there is much that is still unknown about its possible complications. For example, it is now known that COVID-19 may be associated with a hyper-coagulable state, leading to venous or arterial thromboses, and an increased incidence of acute ischemic strokes [12]. More recently, there have also been reports of the virus causing a multisystem inflammatory syndrome in children [13].
It may be worthwhile to be alert for reports of cases similar to the one we have reported as the global medical community strives to gain a better understanding of COVID-19 and its potential sequelae.
Conclusions
Spontaneous spinal epidural hematoma is uncommon, and a high index of suspicion is required to accurately diagnose and appropriately manage it. Although decompression surgery is generally the mainstay of treatment for this condition, conservative management can be used in carefully selected patients. The patient in the present case report had recently recovered from COVID-19. Further observation will be required to determine if there is a spike in other similar cases that may be temporally associated with the novel coronavirus.
Acknowledgments
The authors would like to thank our colleagues who helped to care for this patient and our department for supporting the writing of this report. We would also like to thank the patient for allowing us to use her medical records, results of her tests, and images in the writing of this case report.
Footnotes
Conflict of interests
None.
References:
- 1.Holtas S, Heiling M, Lönntoft M. Spontaneous spinal epidural hematoma: Findings at MR imaging and clinical correlation. Radiology. 1996;199:409–13. doi: 10.1148/radiology.199.2.8668786. [DOI] [PubMed] [Google Scholar]
- 2.Raasck K, Habis A, Aoude A, et al. Spontaneous spinal epidural hematoma management: A case series and literature review. Spinal Cord Ser Cases. 2017;3:16043. doi: 10.1038/scsandc.2016.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thiele RH, Hage ZA, Surdell DL, et al. Spontaneous spinal epidural hematoma of unknown etiology: Case report and literature review. Neurocrit Care. 2008;9(2):242–46. doi: 10.1007/s12028-008-9083-x. [DOI] [PubMed] [Google Scholar]
- 4.Braun P, Kazmi K, Nogués-Meléndez P, et al. MRI findings in spinal subdural and epidural hematomas. Eur J Radiol. 2007;64(1):119–25. doi: 10.1016/j.ejrad.2007.02.014. [DOI] [PubMed] [Google Scholar]
- 5.Liu WH, Hsieh CT, Chiang YH, Chen GJ. Spontaneous spinal epidural hematoma of thoracic spine: A rare case report and review of literature. Am J Emerg Med. 2008;26(3):384.e1–2. doi: 10.1016/j.ajem.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 6.Lawton MT, Porter RW, Heiserman JE, et al. Surgical management of spinal epidural hematoma: Relationship between surgical timing and neurological outcome. J Neurosurg. 1995;83(1):1–7. doi: 10.3171/jns.1995.83.1.0001. [DOI] [PubMed] [Google Scholar]
- 7.Groen RJ, van Alphen HA. Operative treatment of spontaneous spinal epidural hematomas: A study of the factors determining postoperative outcome. Neurosurgery. 1996;39(3):494–509. doi: 10.1097/00006123-199609000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Kim T, Lee CH, Hyun SJ, et al. Clinical outcomes of spontaneous spinal epidural hematoma: A comparative study between conservative and surgical treatment. J Korean Neurosurg Soc. 2012;52(6):523–27. doi: 10.3340/jkns.2012.52.6.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.SreeHarsha CK, Rajasekaran S, Dhanasekararaja P. Spontaneous complete recovery of paraplegia caused by epidural hematoma complicating epidural anesthesia: A case report and review of literature. Spinal Cord. 2006;44(8):514–17. doi: 10.1038/sj.sc.3101869. [DOI] [PubMed] [Google Scholar]
- 10.Jang JW, Lee JK, Seo BR, et al. Spontaneous resolution of a traumatic cervicothoracic epidural hematoma presenting with transient paraplegia: A case report. Spine (Phila Pa 1976) 2010;35(12):E564–67. doi: 10.1097/BRS.0b013e3181cd2de8. [DOI] [PubMed] [Google Scholar]
- 11.Groen RJ. Non-operative treatment of spontaneous spinal epidural hematomas: A review of the literature and a comparison with operative cases. Acta Neurochir. 2004;146:103–10. doi: 10.1007/s00701-003-0160-9. [DOI] [PubMed] [Google Scholar]
- 12.Cuker A, Peyvandi F. Coronavirus disease 2019 (COVID-19): Hypercoagulability. UpToDate https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19-hypercoagulability.
- 13.World Health Organization Scientific Brief Multisystem inflammatory syndrome in children and adolescents with COVID-19. https://www.who.int/publications-detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19.


