Abstract
Coronavirus pandemic is the most important public health event in the world currently. Patients with coronavirus disease 2019 (COVID-19) in a critical state are at risk of progressing rapidly into many serve complications; they require a high level of care from ICU nurses. How to avoid the virus to infect health care worker is also a critical issue. Based on the summarized experience of Chinese health workers, literature review and clinical practice, this article introduced donning and doffing of personal protective equipment (PPE) protocol and some keypoints of nursing critical care in patients with coronavirus disease 2019 (COVID-19): caring of patients requiring intubation and ventilation, venous thromboembolism (VTE) prevention, caring of patients on ECMO, caring for patients requiring enteral nutrition, psychological support and nursing management of COVID-19 ICU. This article introduced a useful protocol of donning and doffing personal protective equipment to protect health care workers, and provided key points for the ICU nurses how to take care of COVID-19 patients.
Keywords: device, intervention, technology
Introduction
COVID-19 is an acute infectious pneumonia whose pathogen is a new coronavirus not previously found in the population.1 2 The main symptoms of patients with COVID-19 are fever, dry cough, fatigue and muscle soreness. A patient with COVID-19 in a critical state is defined as having developed respiratory failure and requiring mechanical ventilation, or in shock or with other organ failure. They are at risk of progressing rapidly into acute respiratory distress syndrome (ARDS), septic shock, metabolic acidosis, coagulation disorders and multiple organ failure3 4 and usually transferred to intensive care unit (ICU). Therefore, critically ill patients with COVID-19 require high level of care from physicians and ICU nurses, dietitians and psychologists. We summarised our experience of providing nursing critical care to nearly 80 patients over 50 days in a 30-bed COVID-19 ICU Tongji hosptial (Guanggu Campus), which provides 800 beds for patients with COVID-19 in Wuhan. The article introduced a protocol of donning and doffing of personal protective equipment (PPE) that summarised from Chinese health workers5 and discussed six key points on nursing critical care: caring of patients with intubation and ventilation, preventing venous thromboembolism (VTE), monitoring patients with extracorporeal membrane oxygenation (ECMO), caring for patients on enteral nutrition, psychological support and nursing management of COVID-19 ICU.
Donning and doffing of PPE: the procedures to enter and exit a COVID-19 ICU
Main routes of transmission of COVID-19 included the respiratory droplet, contact and high concentration aerosol exposure,6 and it should be matched to the virus transmission mode that may occur during patient care.7 Using PPE is a must to protect the healthcare workers.7–9 Nurses should wear PPE before they contact any COVID-19 patient.10
The most recent Morbidity and Mortality Weekly Report by the Centers for Disease Control and Prevention in the USA showed that nearly 35% healthcare workers were infected from COVID-19.11 However, during the epidemic in Wuhan, there were over 400 teams with over 43 000 physicians and nurses went to help from all over China. We suggest that ICU nurses wear two layers of medical caps, two layers of masks (a 3M N95 1860 mask and a surgical mask over N95), three layers of gowns, three layers of gloves, more than two layers of shoe covers, a goggle and face shield. If the nurse needs to perform a procedure that may spread sputum or aerosol10, three layers of PPE should be donned, including two gowns and one medical protective clothing. The gown on the outer layer is to protect the medical protective clothing to avoid contamination by the patient’s body fluids and to keep the protective effect. The medical protective clothing is worn in the middle of two layers of gowns. The gown in the medical protective clothing is to prevent the nurse from being contaminated when taking off the protective clothing.5 Even with limited resources, healthcare workers have the best personal protection to reduce their anxiety and nervousness.
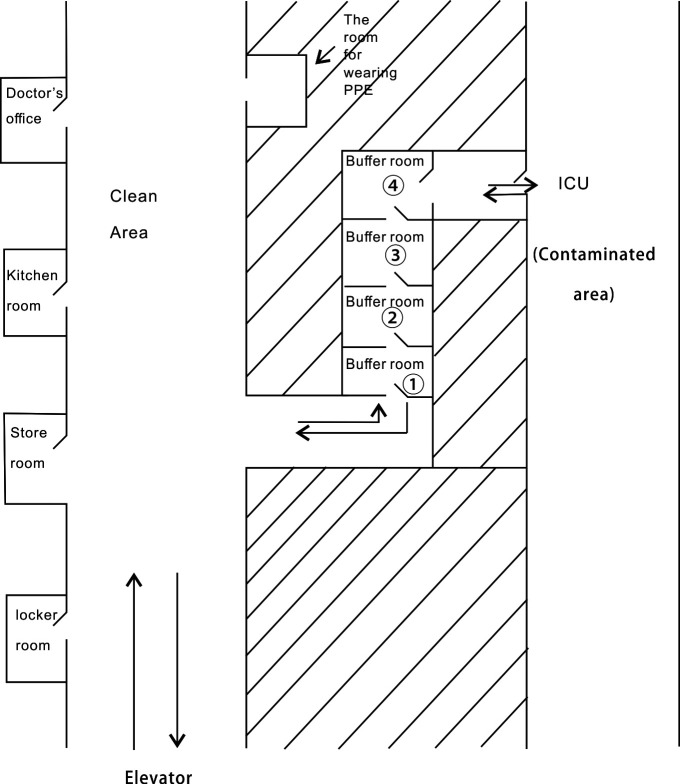
For better isolation and avoidance of cross-contamination among healthcare workers, COVID-19 ICU was divided into three separate areas: clean, buffer and contaminated zones (figure 1).12 A protocol on when and how to don PPE was established. Hand hygiene means washing hands for 20 s. The door handle should be disinfected by using hand sanitiser before the staff goes into the ICU, all healthcare workers must put on PPE according to the protocol in the clean zone following these steps: hand hygiene → putting on the first medical cap → putting on the 3M 1860/9132 medical mask → putting on the second medical cap → putting on the surgical mask → wearing the goggle → putting on the first layer of isolation gown → putting on the first layer of gloves → putting on the first layer of shoe covers → putting on the isolation protective coverall → putting on the second layer of gloves → putting on the second layer of shoe covers → putting on the second layer of gown → putting on the third layer of gloves → and finally putting on the face shield.
Figure 1.
The plan of COVID-19 ICU. ICU, intensive care unit; PPE, personal protective equipment.
After coming out of patient’s room in ICU, PPE must be removed beginning in the contaminated zone and four buffer zones step by step: hand hygiene → removing the face shield → enter the fourth buffer zone after disinfecting the door handle; while in the fourth buffer room: begin with hand hygiene → removing the first layer of shoe covers → hand hygiene → removing the next layer of gloves → hand hygiene → removing the outermost gown → hand hygiene →removing protective coverall → hand hygiene → removing the goggles → hand hygiene → removing the second medical cap → hand hygiene → removing the surgical mask → hand hygiene → entering the third buffer room after disinfecting the door handle; the process in the third buffer room: hand hygiene → removing the first shoe covers → hand hygiene → removing the second layer of gloves → removing the first gown → hand hygiene → entering the second buffer room after disinfecting the door handle; the process in the second buffer room: hand hygiene → removing the 3M 1860/9132 medical mask → hand hygiene removing the last medical cap → hand hygiene → entering the first buffer room right away after disinfecting the door handle; the process in the first buffer room: hand hygiene → put on a new surgical mask and medical cap → hand hygiene → enter the clean area after disinfecting the door handle. The process of putting on the PPE and getting ready to go into the isolation room would take about 30 min. The process of removing PPE after coming out of the isolation room would take about 30 min.
Base on the strictly execution of this protocol, when we finished the work in Guanggu campus of Tongji Hospital, staff received the test of COVID-19 antibody and nucleic acid, and the test results of all members were negative.
Providing the care to patients with invasive ventilation
According to the autopsy results, COVID-19 causes an inflammatory reaction in deep airway and damaging alveoli. Large amount of thick secretions are present in the alveoli, which may be a reason of developing atelectasis in patients with COVID-19.13 14 Therefore, it is important to use invasive ventilation treatment early for critical COVID-19 patients with severe ARDS. Using the protective ventilation strategy and timely suction could delay the progress of the disease.15
The endotracheal tube was carefully secured, and the length was checked in each shift to prevent displacement.16 In order to decrease patient’s oxygen consumption, analgesia and sedation are often used to alleviate patients’ discomfort17 and reduce patient’s irrigation; this is the routine treatment after intubation in patients with COVID-19. 18Remifentanil, midazolam and propofol could be used as the analgesic and sedative drugs. The level of sedation and pain are checked by Ramsay sedation scale and the critical care pain observation tool, and the dosage of medication is adjusted based on the result of assessment.
Suction was considered when a patient has cough with wheezing, elevated airway pressure and reduced tidal volume on the ventilator. Because the sputum is very thick and viscous, in addition to humidifying the respiratory tract through the ventilator, 3–5 mL of sterile water can be dripped into the airway before suction to help the suction. During suction, patients need to inhale pure oxygen and observe the saturation through pulse oxygen saturation (SPO2).16 19 The closed suction catheter must be used for suction, which can reduce the spread of sputum and aerosolisation during the procedure. The closed suction catheter could also keep the effectiveness of positive end expiratory pressure (PEEP) provided by the ventilator during suction to prevent alveolar collapse. The catether could be used for 1 week, and it shall be flushed with sterile water after each suction.10
It should be ensured that each part of the ventilator tubing is connected tightly, and there is space to prevent the aerosol spread into the air due to unexpected disconnect when the patient changes position. Using dual limb ventilator with virus filters placed at the ventilator outlets can reduce the exhalation of virus into the air (figure 2). The filter should be changed when the filter is completely wet or the patient’s exhalation resistance increased.10 Disposable ventilator tubing is used, and water condensation in the water trap was cleaned timely. There is no evidence if the aerosol in the ventilator tubing would not spread when the water trap is opened. Therefore, a plastic bag is used to wrap the water trap, then the trap is opened into the bag and the water was poured out.
Figure 2.
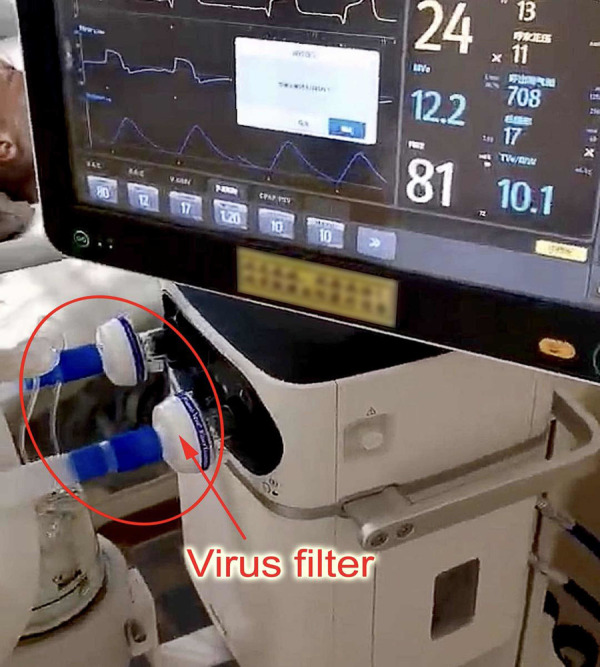
Virus filters placed at the ventilator outlets.
The nurse should watch the parameters of the ventilator and deal with the alarm of the ventilator skilfully. Lung protective ventilator strategy is often performed on COVID-19 patients with ARDS.20 The ventilator mode commonly used are pressure-controlled ventilation mode, such as pressure control-assist/control, pressure control-synchronised intermittent mandatory ventilation+pressure support ventilation and pressure control-synchronised intermittent mandatory ventilation+pressure support ventilation. Tidal volume is set low (6–8 mL/kg), and low level airway plateau pressure is maintained (≤30 cmH2O) to reduce ventilator-related lung injury. If alveolar collapse is serious, the alveolar can be reopened by increasing the PEEP while ensuring that the airway plateau pressure is less than 35 cmH2O. Generally, PEEP is set as 10 cmH20, and the maximum PEEP is no more than 15 cmH2O.
Prevention of VTE
Most of the critically ill patients with COVID-19 have coagulation disorders, and they are at high risk for VTE.21 We should notice signs of deep vein thrombosis (DVT) and pulmonary thromboembolism (PTE). Signs of DVT and PTE should be monitored. Observation for these signs that may indicate a VTE: skin temperature and colour changes, pulsation of dorsalis pedis artery weakening or missing and oedema. Signs to watch for PTE: sudden onset hypoxia, respiratory distress and blood pressure drop.22 Padua prediction tool is used to assess the VTE risk.23
Monitoring patients on ECMO
WHO interim guidelines recommended that ECMO therapy could be used for COVID-19 patients with severe ARDS. As an effective cardiopulmonary support treatment, ECMO can provide temporary support for critically ill patients to improve hypoxia and replacing lungs to do oxygen exchange.24 Five patients were treated by ECMO in our ICU, and they all survived. One was discharged, and other patients were transferred to rehabilitation ward to continue treatment.
The nurse needs to monitor and record patient’s vital signs and the usage of vasoactive drugs. The oxygenation effect of the membrane lung can be observed by monitoring SPO2. If SPO2 is less than 95%, the speed of ECMO pump or air flow can be increased. When blood pressure dropped, ECMO pump speed should be reduced and medication can be used to raise blood pressure.25
Anticoagulation is required to prevent thrombotic complications during ECMO treatment.26 27 The nurse draws blood each hour to check patient’s coagulation panel: activated clotting time and the activated partial thromboplastin time. We could use flashlight to check for any thrombosis at the end of membranous lung or in the pipeline. Adjust heparin drip according to the result of coagulation function test. The wound of puncture point should be observed; it needs to be bandaged to prevent bleeding, and the dressing on the wound should be changed every day to avoid infection.
It is essential to monitor and record ECMO parameters, such as the pump speed, air flow rate, the concentration of air–oxygen mixture and the gas flow rate each hour. When the air flow rapidly decreases, the patient’s oxygen saturation would drop immediately and lead to cardiac arrest. Therefore, this indicator is the most important one for maintaining patient oxygenation.25 27 Shaking catheter may be related to insufficient space between the catheter and blood vessel wall or insufficient volume of blood. It could be solved by adjusting the patient’s position. If it cannot be resolved, the pump speed can be adjusted down until the flow rate becomes stable.28
Keeping the vascular access parallel to the long axis of the body is important to prevent folding, twisting or pulling.27 Pressure injury is easy to form at the junction of vascular access and skin, especially near the puncture point. Double layer cotton pad could be placed between the pipeline and skin and fixed with tape. The nurse should observe the effect of sedation every hour to avoid the occurrence of unplanned extubation.
The nurse needs to check the operation of the oxygen supply device, power supply, air oxygen mixer, spare manual pump, membrane lung, arteriovenous access, and water tank every shift. It is very important to monitor and record the conditions of the puncture point, the patient’s peripheral circulation, pupils and the length of the vascular access. If there are any abnormalities, physician should be notified immediately so that the ECMO is checked for any abnormality. In our ICU, nurses could not do detailed neurological exams because patients needed sedation to be kept comfortable.
Providing care to patients requiring enteral nutrition
Nutritional support is a basic treatment and one of the core measures in comprehensive treatment plan for critically ill patients with COVID-19. Nutritional assessment is required when the patient is admitted to the ICU.29 Trained by dietitian, the intake nurse could make a nutrition plan based on the assessment and start enteral nutrition within 24–48 hours after the haemodynamics become stable. The calorie requirement of critical COVID-19 patients is about 15–30 kcal/kg/day.30 First, the ideal body weight (IBW) for the patient is calculated: IBW (kg)=patient height (cm)−105 (the result of female should multiply by 0.9). IBW (kg) × 15 kcal/kg/day is suitable for patients who have just received enteral nutrition and any patient with severe stress reaction. IBW (kg) × 20–30 kcal/kg is suitable for patients with good tolerance to enteral nutrition (no gastric retention, diarrhoea, nausea and vomiting). Critically ill patient with COVID-19 are likely to cause accelerated protein catabolism due to high fever and stress reactions, which could affect the prognosis and survival rate. Therefore, it is necessary to increase the proportion of protein intake.29
Fresubin diabetes (enteral nutritional emulsion), peptisorb liquid and enteral nutritional suspension are often used for critically ill patients with COVID-19. Fresubin diabetes (enteral nutritional emulsion) is suitable for patients with diabetes and unstable blood sugar and also for patients using glucocorticoids. Peptisorb liquid is a short peptide enteral nutrition liquid; it is easy to absorb and suitable for patients with low albumin, diarrhoea, poor intestinal absorption and elderly. Enteral nutritional suspension is suitable for patients with good recovery and better gastrointestinal function.
The autopsy results of the patient with COVID-19 showed that the small intestine of the patients had segmental dilatation and stenosis, degeneration of mucosal epithelium, necrosis and exfoliation.13 Therefore, enteral nutrition support should follow the principle gradual progression: concentration from low to high, dosage from less to more and speed from slow to fast. The formula should be pumped at a constant speed and completed within 16–24 hours.31 The nasogastric tube was used; in the process of enteral nutrition, it is essential to monitor gastric retention every 4 hours and observe for any signs of feeding intolerance, such as vomiting, bloating, diarrhoea and gastrointestinal bleeding.29 It should be noted that when using propofol for sedation, the energy provided by propofol needs to be calculated into the patient’s total daily energy. According to the literature report, propofol provides energy of 1.1 kcal/mL when administered as a 1% solution, 32 and the serum triglyceride level needs to be monitored.33
Providing psychological support
Critically ill patients with COVID-19 may have psychological issues, such as post-traumatic stress disorder, anxiety, panic, despair and depression due to respiratory distress and difficult of communication.34 Nurses should be trained by psychologist on how to access patients’ mental health by performing a psychological assessment scale. Cognitive–behavioural therapy is a structural, short-term and cognitive approach psychotherapy; it solves mental health problems by changing patients’ cognition and attitude of the disease and is helpful for critically ill patients to improve their emotion.34 Mindfulness relaxation therapy could relieve the tension and anxiety caused by disease and is useful to critically ill patients for maintain a good mental state.35
Nursing management of COVID-19 ICU
The critical condition of COVID-19 patients often accompanies with a variety of complications and causes a huge workload for nurses. We set the bed-to-care ratio in COVID-19 ICU to 1:6 according to the policy of government and 180 nurses provide nursing for 30 patients. Most of our nurses came from ICU, emergency room, departments of neurology and neurosurgery in tertiary hospital of Shanghai; there are many critically ill patients admitted in these departments. Therefore, nurses are experienced and could adapt to the work of COVID-19 ICU quickly. Each shift was set as 4 hours, nurses handed over six times a day and we found increased the incidence of near-miss when the ICU starts running. So, handover is also the key point to ensure the continuous monitoring and quality of nursing for critically ill patients with COVID-19. Based on the Joanna Briggs institute evidence summary of clinical nursing handover,36 we designed a modified version of identify, situation, observation, background, agreed plan and read back (ISOBAR)37 handover checklist. This checklist emphasises the identity verification and key points of monitoring, such as vital signs, ventilator parameters, types of catheter and skin conditions. It is suitable for nurses to hand over for critically ill patients; it could help nurses obtain more patient information from handover process.
In our ICU, the level of intubated acuity of patients is 89% (68/76), the level of not intubated acuity of patients is 11% (8/76), the level of ECMO acuity of patients is 5.6% (5/76) and the level of Continuous Renal Replacement Therapy (CRRT) acuity of patients is 61% (46/76). According to the previous report from Wuhan Jinyintan Hospital and Wuhan Pulmonary Hospital, the mortality rate of COVID-19 patients with invasive ventilation is 96% (31/32), and the mortality rate of patients on ECMO is 100% (3/3).38 During the running of our ICU (11 February 2020–31 March 2020), the mortality rate of patients receiving invasive ventilator treatment was 69.1% (47/68), and the mortality rate of patients using ECMO treatment was 0% (0/5). These results are much lower than the previous report and also reflect the effectiveness of our professional nursing of critical care. In future, we will recruit more patients to further verify the effect of key points of nursing in critically ill patients.
Conclusion
Donning and doffing of PPE protocol could help health workers to protect themselves when they are treating and caring for patients with COVID-19, especially it could reduce the risk of infection when the staff was removing PPE. The key points of nursing care could provide more information for the nurse to understand how to care and observe critical patients with COVID-19.
However, we still have some limitation in this article. First, the protocol should be performed in ICU that has four areas to set buffer room. Second, we summarised key points of nursing care patients with COVID-19 based on literature review. In future study, we should focus on how to protect staff in ICU, where there is no enough space to set buffer area, and recruit more patients to do the prospective or retrospective research to verify the effect of key points of nursing in critically ill patients with COVID-19.
Acknowledgments
Prof. D.W provided important advices to this article
Footnotes
Contributors: YX and LY are responsible for writing this paper; SC is one of the major authors from the developer team of the donning and doffing PPE protocol. YX is responsible for revising the manuscript critically for important intellectual content.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Xie M, Chen Q. Insight into 2019 novel coronavirus - an updated interim review and lessons from SARS-CoV and MERS-CoV. Int J Infect Dis 2020;94:119–24. 10.1016/j.ijid.2020.03.071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhu Y, Li C, Chen L, et al. A novel human coronavirus OC43 genotype detected in mainland China. Emerg Microbes Infect 2018;7:1–4. 10.1038/s41426-018-0171-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020. 10.1001/jama.2020.1585. [Epub ahead of print: 07 Feb 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lai C-C, Shih T-P, Ko W-C, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents 2020;55:105924. 10.1016/j.ijantimicag.2020.105924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wen X, Zhang W. COVID-19 from basics to clinical practice. Shanghai: Fudan express, 2020: 173–84. [Google Scholar]
- 6. Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun 2020;109:102433. 10.1016/j.jaut.2020.102433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cook TM. Personal protective equipment during the coronavirus disease (COVID) 2019 pandemic - a narrative review. Anaesthesia 2020;75:920–7. 10.1111/anae.15071 [DOI] [PubMed] [Google Scholar]
- 8. Honda H, Iwata K. Personal protective equipment and improving compliance among healthcare workers in high-risk settings. Curr Opin Infect Dis 2016;29:400–6. 10.1097/QCO.0000000000000280 [DOI] [PubMed] [Google Scholar]
- 9. McGoldrick M. Personal protective equipment: protecting the eyes. Home Healthc Now 2019;37:234–5. 10.1097/NHH.0000000000000804 [DOI] [PubMed] [Google Scholar]
- 10. Respiratory care committee of Chinese Thoracic Society [Expert consensus on preventing nosocomial transmission during respiratory care for critically ill patients infected by 2019 novel coronavirus pneumonia]. Zhonghua Jie He He Hu Xi Za Zhi 2020;17:E020. 10.3760/cma.j.issn.1001-0939.2020.0020 [DOI] [PubMed] [Google Scholar]
- 11. Heinzerling A, Stuckey MJ, Scheuer T, et al. Transmission of COVID-19 to Health Care Personnel During Exposures to a Hospitalized Patient - Solano County, California, February 2020. MMWR Morb Mortal Wkly Rep 2020;69:472–6. 10.15585/mmwr.mm6915e5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Liew MF, Siow WT, MacLaren G, et al. Preparing for COVID-19: early experience from an intensive care unit in Singapore. Crit Care 2020;24:83. 10.1186/s13054-020-2814-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Liu Q, Wang RS, Qu GQ, et al. Gross examination report of a COVID-19 death autopsy. Fa Yi Xue Za Zhi 2020;36:21–3. 10.12116/j.issn.1004-5619.2020.01.005 [DOI] [PubMed] [Google Scholar]
- 14. Barton LM, Duval EJ, Stroberg E, et al. COVID-19 autopsies, Oklahoma, USA. Am J Clin Pathol 2020;153:725–33. 10.1093/ajcp/aqaa062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Guo Y-R, Cao Q-D, Hong Z-S, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res 2020;7:11. 10.1186/s40779-020-00240-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Umobong EU, Mayo PH. Critical care airway management. Crit Care Clin 2018;34:313–24. 10.1016/j.ccc.2018.03.006 [DOI] [PubMed] [Google Scholar]
- 17. Danielis M, Povoli A, Mattiussi E, et al. Understanding patients' experiences of being mechanically ventilated in the intensive care unit: findings from a meta-synthesis and meta-summary. J Clin Nurs 2020;29:2107–24. 10.1111/jocn.15259 [DOI] [PubMed] [Google Scholar]
- 18. Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, Agitation/Sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med 2018;46:e825–73. 10.1097/CCM.0000000000003299 [DOI] [PubMed] [Google Scholar]
- 19. Klompas M. Prevention of intensive care unit-acquired pneumonia. Semin Respir Crit Care Med 2019;40:548–57. 10.1055/s-0039-1695783 [DOI] [PubMed] [Google Scholar]
- 20. Marini JJ, Gattinoni L. Propagation prevention: a complementary mechanism for "lung protective" ventilation in acute respiratory distress syndrome. Crit Care Med 2008;36:3252–8. 10.1097/CCM.0b013e31818f0e68 [DOI] [PubMed] [Google Scholar]
- 21. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lewis TC, Cortes J, Altshuler D, et al. Venous thromboembolism prophylaxis: a narrative review with a focus on the high-risk critically ill patient. J Intensive Care Med 2019;34:877–88. 10.1177/0885066618796486 [DOI] [PubMed] [Google Scholar]
- 23. Barbar S, Noventa F, Rossetto V, et al. A risk assessment model for the identification of hospitalized medical patients at risk for venous thromboembolism: the Padua prediction score. J Thromb Haemost 2010;8:2450–7. 10.1111/j.1538-7836.2010.04044.x [DOI] [PubMed] [Google Scholar]
- 24. Ramanathan K, Antognini D, Combes A, et al. Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases. Lancet Respir Med 2020;8:518–26. 10.1016/S2213-2600(20)30121-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Patel B, Arcaro M, Chatterjee S. Bedside troubleshooting during venovenous extracorporeal membrane oxygenation (ECMO). J Thorac Dis 2019;11:S1698–707. 10.21037/jtd.2019.04.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vieira J, Frakes M, Cohen J, et al. Extracorporeal membrane oxygenation in transport Part 2: complications and Troubleshooting. Air Med J 2020;39:124–32. 10.1016/j.amj.2019.09.009 [DOI] [PubMed] [Google Scholar]
- 27. Ratnani I, Tuazon D, Zainab A, et al. The role and impact of extracorporeal membrane oxygenation in critical care. Methodist Debakey Cardiovasc J 2018;14:110–9. 10.14797/mdcj-14-2-110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Osho AA, et al. Veno-venous extracorporeal membrane oxygenation for respiratory failure in COVID-19 patients: early experience from a major academic medical center in North America. Ann Surg 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Elke G, Hartl WH, Kreymann KG, et al. Clinical nutrition in critical care medicine - guideline of the German Society for nutritional medicine (DGEM). Clin Nutr ESPEN 2019;33:220–75. 10.1016/j.clnesp.2019.05.002 [DOI] [PubMed] [Google Scholar]
- 30. Li XY, Du B, Wang YS, et al. [The keypoints in treatment of the critical coronavirus disease 2019 patient(2)]. Zhonghua Jie He He Hu Xi Za Zhi 2020;43:277–81. 10.3760/cma.j.cn112147-20200224-00159 [DOI] [PubMed] [Google Scholar]
- 31. McNelly AS, Bear DE, Connolly BA, et al. Effect of intermittent or continuous feed on muscle wasting in critical illness: a phase 2 clinical trial. Chest 2020;158:183–94. 10.1016/j.chest.2020.03.045 [DOI] [PubMed] [Google Scholar]
- 32. Hastings J, Ridley EJ, Bianchet O, et al. Does propofol sedation contribute to overall energy provision in mechanically ventilated critically ill adults? A retrospective observational study. JPEN J Parenter Enteral Nutr 2018;42:748–57. 10.1177/0148607117721917 [DOI] [PubMed] [Google Scholar]
- 33. Kaur H, Nattanamai P, Qualls KE. Propofol and clevidipine-induced hypertriglyceridemia. Cureus 2018;10:e3165. 10.7759/cureus.3165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Richards-Belle A, Mouncey PR, Wade D, et al. Psychological outcomes following a nurse-led preventative psychological intervention for critically ill patients (POPPI): protocol for a cluster-randomised clinical trial of a complex intervention. BMJ Open 2018;8:e020908. 10.1136/bmjopen-2017-020908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Steinberg BA, Klatt M, Duchemin A-M. Feasibility of a mindfulness-based intervention for surgical intensive care unit personnel. Am J Crit Care 2016;26:10–18. 10.4037/ajcc2017444 [DOI] [PubMed] [Google Scholar]
- 36. Marin T. Nursing: clinical handover, 2019. [Google Scholar]
- 37. Porteous JM, Stewart-Wynne EG, Connolly M, et al. iSoBAR--a concept and handover checklist: the National Clinical Handover Initiative. Med J Aust 2009;190:S152–6. 10.5694/j.1326-5377.2009.tb02625.x [DOI] [PubMed] [Google Scholar]
- 38. Zhou F. Clinical course and risk factors for mortality of adult inpatients with COVID-19. Lancet 2020;395:1054–62. [DOI] [PMC free article] [PubMed] [Google Scholar]