Abstract
Objectives:
Patients with acute respiratory failure due to coronavirus disease 2019 (COVID-19) have a high likelihood of needing prolonged intubation and may subsequently require tracheotomy. Indications and timing for performing tracheotomy in patients affected by severe COVID-19 pneumonia are still elusive. The aim of this study is to analyze the role of tracheotomy in the context of this pandemic. Moreover, we report the timing of the procedure and the time needed to complete weaning and decannulation in our center.
Methods:
This retrospective, observational cohort study included adults (≥18 years) with severe COVID-19 pneumonia who were admitted to the intensive care unit (ICU) of the tertiary care center of Reggio Emilia (Italy). All patients underwent orotracheal intubation with invasive mechanical ventilation, followed by percutaneous or open surgical tracheotomy. Indications, timing of the procedure, and time needed to complete weaning and decannulation were reported.
Results:
Forty-four patients were included in the analysis. Median time from orotracheal intubation to surgery was 7 (range 2-17) days. Fifteen (34.1%) patients died during the follow-up period (median 22 days, range 8-68) after the intubation. Weaning from the ventilator was first attempted on median 25th day (range 13-43) from orotracheal intubation. A median of 35 (range 18-79) days was required to complete weaning. Median duration of ICU stay was 22 (range 10-67) days. Mean decannulation time was 36 (range 10-77) days from surgery.
Conclusions:
Since it is not possible to establish an optimal timing for performing tracheotomy, decision-making should be made on case-by-case basis. It should be adapted to the context of the pandemic, taking into account the availability of intensive care resources, potential risks for health care workers, and benefits for the individual patient.
Keywords: COVID-19, COVID, SARS-CoV-2, tracheotomy, tracheostomy, weaning
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) disease (COVID-19) pandemic is a major public health emergency. 1 Coronavirus disease 2019 results in a clinical picture of atypical pneumonia, with different degree of severity. About 5% of patients present an acute respiratory distress syndrome (ARDS) requiring admission to the intensive care unit (ICU). 2 About 2.3% patients positive for COVID-19 require invasive mechanical ventilation (IMV) via an endotracheal tube, 2 but the percentage rises to 42% among critically ill patients. 3 Many of these patients with acute respiratory failure have a high likelihood of needing prolonged intubation and IMV and may subsequently require tracheotomy. The role of tracheotomy in COVID-19-affected patients is still hazy: few data are reported about the indications, timing, clinical results, and percentage of complications. Some authors agree that tracheotomy should be performed after at least 14 days from intubation. These data come from recommendations and guidelines that describe the surgical steps to achieve maximum protection of the involved medical/nursing staff, but data on this subject are still lacking. 4 Herein, we report the clinical outcome in 44 consecutive patients, treated in our tertiary referral center, affected by severe COVID-19 pneumonia requiring intubation and tracheotomy. The role of tracheotomy, timing of weaning from the ventilator, and decannulation are reported.
Patients and Methods
A retrospective analysis was performed of the clinical records of consecutive patients affected by severe ARDS due to SARS-CoV-2 infection, treated with IMV and tracheotomy at the ICU of a tertiary referral center (Azienda USL-IRCCS of Reggio Emilia, Italy) in March to April 2020. All tracheotomies were performed with either percutaneous or open technique and bedside approach in negative pressure rooms inside the ICU. In order to minimize the risk of infection in medical/nursing staff, a protocol for performing safe tracheotomy was adopted. 5 A cuffed tracheal cannula was positioned at the end of surgery.
The patients were included in the study according to the following criteria. Inclusion criteria were any age and sex, diagnosis of COVID-19 confirmed by nasopharyngeal/oropharyngeal swab, severe ARDS due to COVID-19 infection, treated by intubation and IMV, and subsequent tracheotomy. Exclusion criteria were presence of previous tracheostoma, history of radiotherapy on the neck.
Statistical Analysis
Categorical variables were presented as percentages. Continuous variables were summarized as mean ± standard deviation or median and range. Comparisons between groups were performed by Pearson χ2 test or Fischer exact test for discrete variables as appropriate, and t test for continuous variables. Statistical significance was presented as P value, with observed differences considered statistically significant at a P ≤ .05.
Results
Forty-seven patients affected by severe ARDS due to SARS-CoV-2 infection underwent IMV and subsequent tracheotomy at the ICU of our hospital in March and April 2020. Three patients were excluded from the study because they were transferred to other cities before complete weaning. Forty-four patients met the inclusion criteria and were included in the analysis. Median age was 64 years (range 34-79); male to female ratio was 2.7. Past medical history was relevant for ≥2, 1, or 0 comorbidities in 32/44 (72.7%), 8/44 (18.2%) and 4/44 (9.1%) patients, respectively. The clinical summary of the patients is reported in Table 1. All patients underwent elective tracheotomy; 29 patients underwent open surgical tracheotomy, while 15 patients underwent percutaneous dilatational tracheotomy. Median time from orotracheal intubation to surgery was 7 days (range 2-17). At the time when surgical indication to tracheotomy was given, mean respiratory values were as follows: positive end-expiratory pressure (PEEP) 13.5 cm H2O (±2.6), FiO2 58.4% (±12.7), respiratory rate 17.6 breaths per minute (±2.8). The tracheotomy was performed within 24 hours from the indication. No intraoperative complications occurred. Twenty-five (56.8%) patients had postoperative complications: mild hemorrhage (8/44, 18.2%), local infection (15/44, 34.1%), and subcutaneous emphysema (4/44, 9.1%). None of the patients required revision surgery. The type of surgical technique didn’t affect the outcome in terms of complication rate, with 16/29 (55.2%) patients with postoperative complications in case of open surgical tracheotomy (OST) and 8/15 (53.3%) in percutaneous dilatational tracheotomy (PDT) (P = .84). Fifteen patients (34.1%) died during the follow-up period, after a median period of 22 (range 8-68) days after the intubation. The risk of mortality was not correlated with the timing of tracheotomy (P = .82) or with the type of surgical technique (P = .28). All those 15 patients died before any attempt of weaning. Weaning from the ventilator and decannulation timing were analyzed in the 29 survivors. Weaning from the ventilator was first attempted on median 25th day (range 13-43) from the orotracheal intubation. A median of 35 (range 18-79) days was required from orotracheal intubation to complete weaning. The surgical technique didn’t affect weaning: Median time was 33.0 (range 24-79) days for OST and 43.5 days for PDT (range 18-95; P = .74). Median duration of ICU stay was 22 days (range 10-67). Considering weaning timing, it was estimated that thanks to tracheotomy, the length of ICU’s stay was shortened by 14 days per patient. Mean decannulation time was 36 (range 10-77) days from surgery. A timetable is reported in Figure 1. None of the medical and nursing staff was infected in both groups.
Table 1.
Clinical Summary of the Cohort.
| Clinical summary | |||
|---|---|---|---|
| All patients | F | M | |
| Demographics | |||
| Age (median, range) | 64 (34-79) | 68 (38-77) | 64 (34-79) |
| Sex (male/female, ratio) | 32/12 (2.7) | – | – |
| Comorbidity (%) | |||
| Arterial hypertension | 27/44 (61.4%) | 7/12 (58.3%) | 20/32 (62.5%) |
| BMI > 25 | 17/44 (38.6%) | 8/12 (66.7%) | 9/32 (28.1%) |
| Diabetes mellitus | 9/44 (20.5%) | 1/12 (8.3%) | 8/32 (25.0%) |
| Other | 28/44 (63.6%) | 8/12 (66.7%) | 20/32 (62.5%) |
| Smoking habits (%) | 8/44 (18.2%) | 3/12 (25.0%) | 5/32 (15.6%) |
Figure 1.
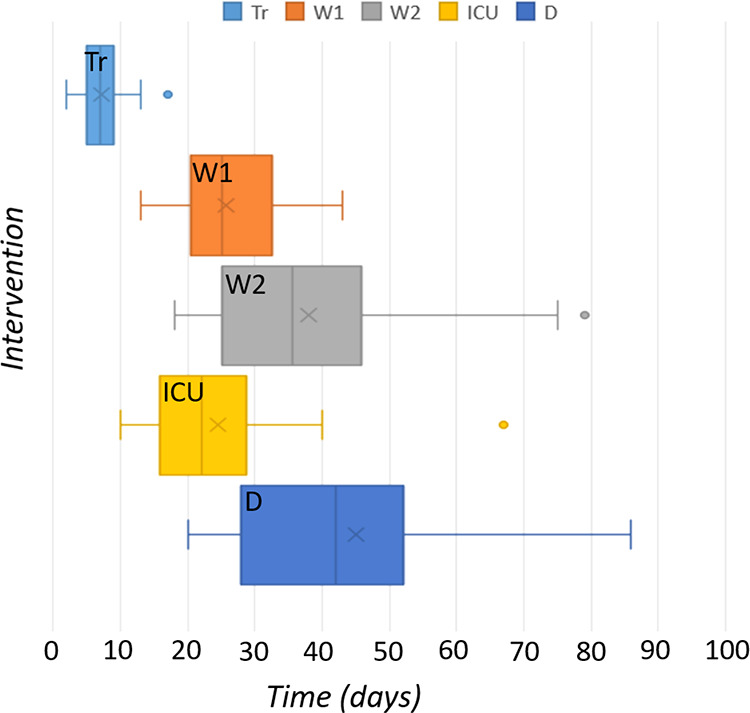
Timeline. Time 0 is the day of ICU admission. D, decannulation (dark blue); ICU, dismission from ICU (yellow); Tr, time from intubation to tracheotomy (clear blue); W1, first attempt of weaning from the ventilator (orange); W2, complete weaning (grey). ICU indicates intensive care unit.
Discussion
We decided to consider previous radiotherapy on the neck an exclusion criterion because we though it could affect outcome: After radiation therapy, surgery is often more challenging because of the presence of fibrotic tissue, and it is therefore associated with higher risk of complications in our experience.
In our cohort of patients, there was a complication rate of almost 57%. This high-complication rate could be explained by 2 reasons. First of all, we analyzed the complication rates in a group of critically ill patients, that can’t be compared to the general population. Secondly, we considered the complications of any severity in the analysis, including also mild infections and minor hemorrhages not requiring surgical reintervention. Previous studies that included only major complications, reported in fact lower complication rates; instead, those studies who collected also mild complications in the analysis, reported higher complication rates, reporting minor hemorrhage for 100% of critically ill patients. 6
Indications
Traditionally, in critically ill patients with need for prolonged intubation, tracheotomy is performed to facilitate weaning and to ease airway toilet, therefore improving the management of these patients. Moreover, tracheotomy decreases the risk of complications related to prolonged intubation, such as subglottic or tracheal stenosis and arytenoid anchyloses. Coronavirus disease 2019–related ARDS often requires prolonged intubation. In addition, early extubating attempts frequently require a re-intubation procedure. According to Meng et al, 7 these should be considered difficult and complicated intubations for different reasons (ie, no respiratory reserve, strict infection control and urgency, personal protective equipment, psychological pressure). Therefore, in this kind of patients, the presence of tracheostomy offers several advantages, as it allows safer attempt of weaning from the ventilator, both for the patient and for medical staff. During the epidemic crisis, 2 attempts of weaning during orotracheal intubation were attempted in our ICU. The first patient was able to perform weaning successfully, being extubated 6 days after admission. The second patient was extubated without performing tracheostomy, but 36 hours after the orotracheal tube removal, it became necessary to proceed to re-intubation because of progressive respiratory fatigue occurring despite face mask optimization; the following day, he underwent tracheotomy in order to manage his weaning more easily and safely. Aside from those 2 patients, all the others admitted to the ICU underwent tracheotomy.
In this context of the COVID-19 pandemic, tracheotomy had a new role that had not been reported before: The rapidly increasing need for ICU admissions due to severe COVID-19 caused an imbalance between the number of patients requiring intensive care and availability of ICU’s beds and resources. Thus, the tracheostomy represented an important measure for early discharge of patients from ICU to lower intensity care wards. In fact, patients with a tracheotomy still needing IMV can be managed with minimal sedation and they can be managed in lower-intensity wards.
Timing
Even though data regarding this topic are lacking and timing has yet to be defined, some authors have addressed the issue of when to perform the procedure, and practices vary widely. 8 Only small cohorts of patients have been reported; therefore, it is inappropriate to draw conclusions with such small numbers. One has to balance between the advantages of tracheotomy and the possibility of viral transmission to medical/nursing staff involved in surgical and decannulation procedure or taking care for the patients. Some authors have proposed that viral load should be considered and incorporated within recommendations. 4 The American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) issued a position statement on March 27, 2020 (revised April 2), recommending performing a tracheostomy no earlier than 2 weeks after intubation. Recommendations of the ENT UK and British Laryngological Association suggest to wait a minimum of 14 days of intubation to allow prognostic information to become clear and for viral load to potentially decrease. 9 In contrast, other authors 10 proposed a timing of 7 days if patients are far from reaching weaning targets. One of the first case series of 32 patients from Italy reported a mean intubation period of 15 days (range, 9-21 days) before performing tracheotomy. Ferri et al 8 suggested that tracheostomy should be performed in stable or clinically improved patients affected by COVID-19, not before the 20th day after orotracheal intubation. They argue that the subgroup of patients with shorter duration of intubation has a negative prognostic trend. We didn’t find a different prognosis, as the risk of death during the first 60 days was not related to the duration of the orotracheal intubation. Indeed, we performed early tracheotomies, with a median time of 7 days. Our choice to perform early tracheotomy was due in part to the need to increase the ICU’s capacity for additional patients. Moreover, in some cases, tracheotomy was needed early because the orotracheal tube was frequently blocked with secretions. In fact, since the tracheal cannula is shorter than the orotracheal tube and because of the presence of an inner cannula, the toilet of the tracheal cannula is much easier. A recent systematic review published by Adly et al 11 in 2018 showed that early tracheostomy, performed within 7 days from intubation, reduces the complications’ rate (ie, aspiration pneumonia, septic shock, multi-organ failure), the mortality rate and the length of stay in ICU.
In our experience with ARDS-like pattern, we have attempted to lower the risk of ventilator-induced lung injury in COVID-19 patients by individualizing modalities with protective ventilation criteria, as tidal volume below 8 mL/kg of predicted body weight, respiratory rate below 25 bpm and plateau pressure below 30 to 35 cmH2O. 12 In addition, especially in long-term patients with poor lung compliance, we performed frequent PEEP trials in order to reduce driving pressure or increase tidal volume in conjunction with a pressure-controlled modality with constant inspiratory pressure over PEEP. 13,14
Conclusions
Since it is not possible to establish an optimal timing for performing tracheotomy, decision-making should be made on case-by-case basis. It should be adapted for the pandemic, taking into account the availability of ICU’s resources, the potential risks for health care workers and the benefits for the individual patient.
Footnotes
Authors’ Note: This research has been conducted in accordance with ethical principles, including the World Medical Association Declaration of Helsinki (2002). The local ethical committee Area Vasta Emilia Nord approved this research.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Cecilia Botti  https://orcid.org/0000-0002-0136-141X
https://orcid.org/0000-0002-0136-141X
Francesca Lusetti  https://orcid.org/0000-0003-0153-9641
https://orcid.org/0000-0003-0153-9641
References
- 1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in china. N Engl J Med. 2020;382(8):727–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in china. N Engl J Med. 2020;382(18):1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARSCoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. [published correction appears in Lancet Respir Med. 2020 Apr;8(4): e26]. Lancet Respir Med. 2020;8(5):475–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Delides A, Maragoudakis P, Nikolopoulos T. Timing of tracheotomy in intubated patients with COVID-19. Otolaryngol Head Neck Surg. 2020;163(2):328–329. [DOI] [PubMed] [Google Scholar]
- 5. Botti C, Lusetti F, Castellucci A, Costantini M, Ghidini A. Safe tracheotomy for patients with COVID-19. Am J Otolaryngol. 2020;41(4):102533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Johnson-Obaseki S, Veljkovic A, Javidnia H. Complication rates of open surgical versus percutaneous tracheostomy in critically ill patients. Laryngoscope. 2016;126(11):2459–2467. doi:10.1002/lary.26019 [DOI] [PubMed] [Google Scholar]
- 7. Meng L, Qiu H, Wan L, et al. Intubation and ventilation amid the COVID-19 outbreak: Wuhan’s experience. Anesthesiology. 2020;132(6):1317–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ferri E, Boscolo Nata F, Pedruzzi B, et al. Indications and timing for tracheostomy in patients with SARS CoV2-related. Eur Arch Otorhinolaryngol. 2020;277(8):2403–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jacob T, Walker A, Mantelakis A, Gibbins N, Keane O. A framework for open tracheostomy in COVID-19 patients. Clin Otolaryngol. 2020;45(4):649–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mattioli F, Fermi M, Ghirelli M, et al. Tracheostomy in the COVID-19 pandemic. Eur Arch Otorhinolaryngol. 2020;277(7):2133–2135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Adly A, Youssef TA, El-Begermy MM, Younis HM. Timing of tracheostomy in patients with prolonged endotracheal intubation: a systematic review. Eur Arch Otorhinolaryngol. 2018;275(3):679–690. [DOI] [PubMed] [Google Scholar]
- 12. Marini JJ. Evolving concepts for safer ventilation. Crit Care. 2019;23(1):114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gattinoni L, Marini JJ, Collino F, et al. The future of mechanical ventilation: lessons from the present and the past. Crit Care. 2017;21(1):183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. De Jong A, Cossic J, Verzilli D, et al. Impact of the driving pressure on mortality in obese and non-obese ARDS patients: a retrospective study of 362 cases. Intensive Care Med. 2018;44(7):1106–1114. [DOI] [PubMed] [Google Scholar]


