Abstract
Proximal tibiofibular joint (PTFJ) pathology is an uncommon but perhaps underappreciated cause of lateral knee pain. While imaging guided therapeutic injections for diagnosis and management of joint related symptoms are now commonplace and numerous techniques for accessing most joints in the body have been documented, a technique for fluoroscopically guided injection of the PTFJ has not been yet described in the literature. We present a case of an adult patient who presented with lateral knee pain refractory to conservative management who opted for a fluoroscopically-guided therapeutic injection of her PTFJ.
Keywords: Therapeutic, Injection, Joint, Knee, Proximal, Tibiofibular
Abbreviations: PTFJ, proximal tibiofibular joint
Introduction
Lateral knee pain may be caused by a diverse range of etiologies and proximal tibiofibular joint (PTFJ) pathology should be considered in the differential diagnosis [1], [2], [3]. The utility of imaging guided intra-articular therapeutic injection for both, confirming the targeted joint as the source of symptoms as well as providing symptomatic relief has been previously described [4]. While techniques for therapeutic injection of numerous joints have been reported in the literature, description of imaging guided interventions involving the PTFJ have been scant. In this report, we present the case of a patient with lateral knee pain which was refractory to conservative management but responded to fluoroscopically guided intra-articular therapeutic injection of the PTFJ which provided both symptomatic relief and confirmation of the PTFJ as the source of her symptoms allowing for subsequent definitive management. Additionally, this report describes a suitable approach for therapeutic injection of the PTFJ under fluoroscopic guidance, discusses relevant local anatomy and procedural considerations as well as compares the relative advantages of fluoroscopic vs ultrasound guidance for this intervention.
Case Report
This report was exempt from IRB review at our institute. A 42-year-old female patient presented to Orthopedic Surgery clinic with lateral left knee pain that she attributed to a recent fall onto her left knee. The patient was able to bear weight and denied instability. Her physical examination was positive for lateral tenderness to palpation. No knee joint effusion was apparent on physical examination. Lachman and anterior/posterior drawer tests were negative. Of note, the patient had previously been diagnosed with and was undergoing treatment for chronic pain and fibromyalgia. Radiographs of the left knee demonstrated no findings to explain this patient's symptoms. One month after her initial presentation, a non-contrast MRI examination of the left knee was obtained at an outside facility (Fig. 1) that demonstrated edema-like marrow signal suggestive of a contusion vs stress reaction along the lateral tibial condyle but no discrete fracture line or apparent widening of the PTFJ. The patient's symptoms were initially managed conservatively with physical therapy, oral gabapentin, topical diclofenac sodium gel as well as saphenous nerve injection performed by her orthopedic surgeon. However, she returned to clinic approximately 6 months after initial presentation reporting persistent lateral left sided knee pain and requested further therapeutic intervention. The treating orthopedic surgeon and patient opted for imaging guided therapeutic injection of the left PTFJ given their reservations about accuracy of PTFJ targeting using only palpation.
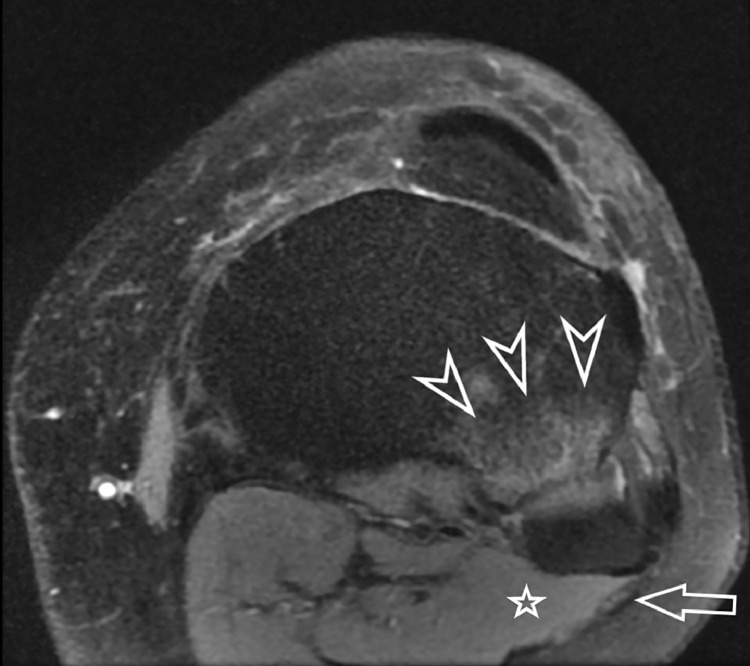
Fig. 1.
Axial fat-saturated proton density MR image of the left knee from an outside facility (obtained 1 month before initial presentation to our facility) at the level of the PTFJ demonstrated edema along the tibial margin of the PTFJ (white arrowheads) without joint space widening or effusion. Common peroneal nerve (white arrow) courses along the posterolateral aspect of the fibular head lateral to the lateral head of the gastrocnemius muscle belly (white star).
Shortly thereafter, a fluoroscopically-guided therapeutic injection of the PTFJ was performed by a board certified musculoskeletal radiologist with 7 years of postgraduate imaging-guided procedural experience. The patient reported a subjective preprocedure pain score of 8/10. The patient was positioned supine on the table of the fluoroscopy unit (Axiom Artis MP, Siemens, Erlangen, Germany) with her knee extended and stabilized in a comfortable position. The ankle was stabilized in a neutral position to maximize patient comfort for the duration of the procedure. An anterior approach was chosen to minimize risk to the common peroneal nerve. Accordingly, the image intensifier faced the anterior margin of PTFJ and the beam was oriented parallel to the medial facet of the fibular head. Using standard aseptic technique and a buffered 1% lidocaine hydrochloride solution (Hospira, Lake Forest, IL) for local anesthesia, a 2 inch 22 gauge needle was advanced into the middle third of the PTFJ. 0.5 cc of iodinated contrast (iohexol, 300 mgI/mL; Omnipaque 300, GE Healthcare, Chicago, IL) was injected to confirm intra-articular position of the needle tip (Fig. 2a). Then, 1 cc of a therapeutic cocktail comprised of 0.5 cc of 0.75% bupivacaine hydrochloride (Sensoricaine, Fresenius Kabi, Lake Zurich, IL) and 0.5 cc containing 20 mg triamcinolone acetonide (Amneal, Bridgewater, NJ) was administered into the PTFJ (Fig. 2b). The procedure needle was subsequently flushed with a small volume of 1% lidocaine and withdrawn. After a brief period of observation (approximately 15 minutes) in the holding area, the patient reported a subjective postprocedure pain score of 0/10.
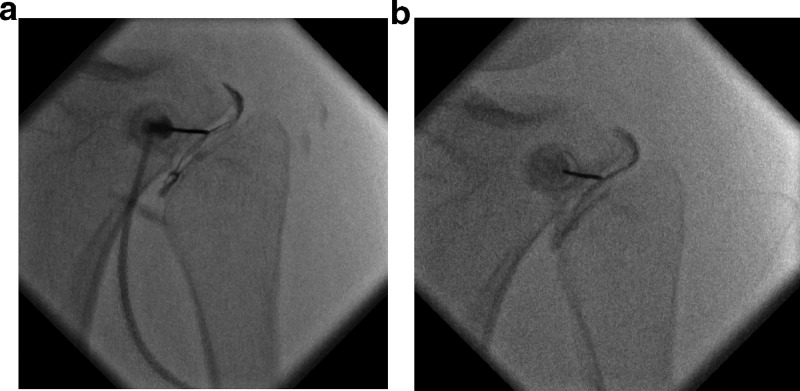
Fig. 2.
(a) shows an anterior oblique fluoroscopic image of the left PTFJ with the image intensifier oriented parallel to the articular surface of the medial facet of the fibular head with the tip of the 2 inch 22 gauge procedure needle approaching the middle third of the left PTFJ and the flow pattern of a small volume of injected iodinated contrast confirming intra articular position of the needle tip. (b) shows the opacified left PTFJ immediately after completion of therapeutic cocktail injection.
At the follow-up appointment with her orthopedic surgeon approximately 3 weeks after the fluoroscopically guided PTFJ injection, the patient reported symptomatic relief that had lasted approximately 7-10 days after the procedure, however her preinjection symptoms including lateral sided-knee pain had gradually returned thereafter. Given the refractory nature and severity of her symptoms, the patient chose to undergo surgical fusion of her left PTFJ (Fig. 3) which afforded relief from her symptoms.
Fig. 3.
AP radiograph of the left knee obtained 1 month after surgery shows postoperative changes related to PTFJ arthrodesis and proximal fibular osteotomy.
Discussion
The PTFJ is a sliding diarthrodial synovial joint between the lateral tibial condyle and medial facet of the fibular head that distributes torsional stress and lateral bending motion of the tibia as well as transmits axial loading during weight bearing [5]. The PTFJ has a fibrous capsule which is supported by the anterosuperior and posterosuperior proximal tibiofibular ligaments (Fig. 4) [5]. The configuration of the PTFJ allows for anterolateral displacement of fibular head with respect to the tibia during ankle dorsiflexion and posteromedial displacement during ankle plantarflexion [6]. Communication between the PTFJ and the knee joint has been reported in up to 64% of evaluated anatomic specimens [7]. The common peroneal nerve tracks along the lateral segment of the popliteal fossa, posterior, and medial to the biceps tendon, deep to the peroneus longus tendon and wraps around the anterolateral aspect of the fibular neck distally and gives rise to the articular, deep peroneal and superficial peroneal branches (Fig. 5) [8]. Anatomic variation in the course of the common peroneal nerve with respect to the fibular head has been described in the literature and will not be explored further here [8,9].
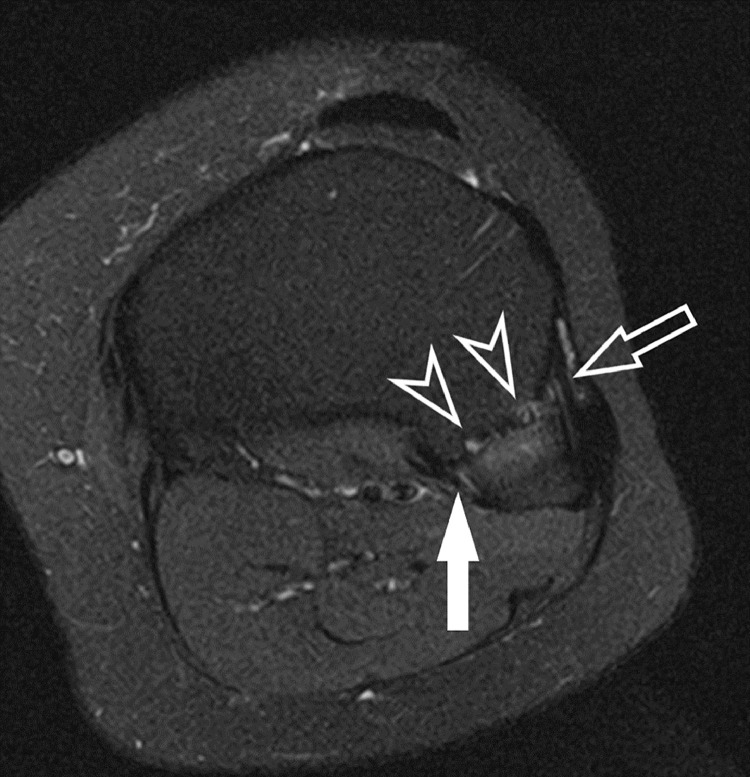
Fig. 4.
Axial intermediate-weighted fat-saturated MR image of the patient's left knee (obtained 1 month after the fluoroscopically guided PTFJ therapeutic injection) at the level of the proximal margin of the PTFJ demonstrates the relationship of the anterosuperior ligament (hollow white arrow) and posterosuperior ligament (solid white arrow) with respect to the fibrous capsule of the PTFJ (arrowheads).
Fig. 5.
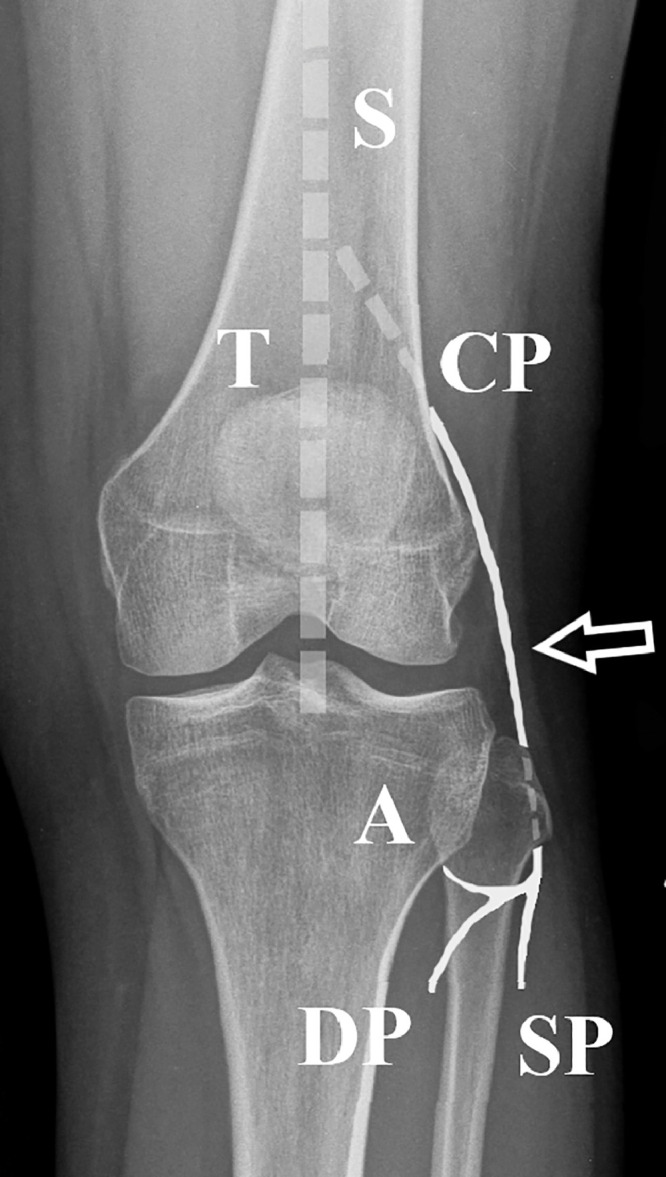
Standing AP radiograph of the patient's left knee obtained at the time of initial presentation with superimposed diagram depicting the typical course of the common peroneal nerve (CP) which arises from the sciatic nerve (S), tracks lateral to the tibial nerve (T) along the lateral margin of the popliteal fossa, posterior and medial to the biceps femoris tendon (arrow) and wraps around the anterolateral aspect of the fibular neck distally before giving rise to the articular (A), deep peroneal (DP) and superficial peroneal (SP) branches. Note: for clarity, the branches of the tibial nerve distal to the origin of the common peroneal nerve are not depicted.
In preparation for fluoroscopically guided PTFJ therapeutic intervention, it is essential to review any available cross sectional imaging to identify the optimal approach (typically parallel to the articular surface of the medial facet of the fibular head) and be familiar with the typical location and course of the common peroneal nerve and its branches. We chose an oblique anterior approach in order to minimize risk of injuring the common peroneal nerve. Cross sectional imaging studies should also be assessed for the presence of overlying fluid collection or inflammatory changes that if traversed may cause iatrogenic inoculation of the PTFJ. As with other similar imaging-guided therapeutic interventions, it is imperative to review all available clinical data to assess for: documented prior adverse reaction to iodinated contrast, local anesthetic, or components of the proposed therapeutic cocktail (intermediate-acting anesthetic and steroid) as well as coagulopathy and/or recent anticoagulation therapy and take appropriate actions as per accepted institutional/society guidelines. Additionally, we routinely assess the integrity of skin overlying the proposed needle entrance site and confirm the absence of apparent inflammatory changes to minimize the risk of iatrogenic complication. The oblique configuration of the PTFJ with respect to the conventional AP and lateral anatomic planes may require an imaging modality that can rotate to visualize the optimal approach into the joint space if the patient cannot be adequately positioned under a fixed plane fluoroscopic unit.
At the start of the procedure, it is important to counsel the patient to minimize plantar/dorsiflexion of the ankle as this may alter the orientation of the PTFJ during procedure and if necessary consider immobilization of the foot and ankle [5]. Given the small potential space, we chose to target the middle third of the PTFJ to maximize the likelihood of intra-articular needle tip placement as well as minimize the risk of injury to the terminal branches of the common peroneal nerve coursing along the anterior aspect of the fibular neck. Additionally, the small size of the PTFJ necessitates that the proceduralist minimize the volume of iodinated contrast administered during the test injection confirming intra-articular location of the needle tip in order to allow for maximum residual potential space for delivery of the therapeutic cocktail.
Although a broad range of pathology has been described about the lateral aspect of the knee, PTFJ dysfunction should be considered in the differential diagnosis of patients presenting with lateral knee pain [2,10,11]. Symptoms and clinical findings of PTFJ pathology are variable but may include: spontaneous pain referable to the PTFJ, pain upon palpation of the fibular head or pain during PTFJ mobilization [10,12]. MRI evidence of PTFJ degeneration has been described in 42% of pts presenting with lateral knee pain which supports the notion that this location should be incorporated into the formal search pattern of any radiologist evaluating an imaging study of a knee [10].
To our knowledge, there are no published formal studies documenting the effectiveness of PTFJ therapeutic injection for lateral knee pain nor any description of technique for fluoroscopically guided injection of this joint. A review of the literature does offer a single case report in the form of a poster abstract which described ultrasound guided PTFJ injection of single knees in 2 different patients using corticosteroid based therapeutic cocktails which afforded symptomatic relief for 5 and 2 months, respectively [13]. The report noted that both patients subsequently underwent additional PTFJ therapeutic interventions which included repeat corticosteroid injection in the first patient and platelet rich plasma (PRP) injections in the second. Additional interventions were not documented in the report. The utility of ultrasound guidance for joint aspiration and injection has been well described [14]. More specifically, the superiority of ultrasound guidance versus palpation only for PTFJ injection has been described in a study using cadaveric specimens which reported 100% vs 58% accuracy for each method, respectively [12]. Although to our knowledge no study has been published comparing the relative accuracies of fluoroscopic versus ultrasound guided injection of the PTFJ, it seems reasonable to infer that both forms of imaging guidance would offer superior accuracy for intra-articular delivery of injectate when compared with PTFJ injection guided by palpation alone.
When assessing the relative advantages and disadvantages of fluoroscopy versus ultrasound for imaging guided injection of the PTFJ, both techniques offer real-time visualization of needle placement with regard to adjacent anatomic structures as well as real-time monitoring of injectate delivery. Ultrasound may have additional advantages in that this modality offers the ability to: localize and avoid the anterosuperior proximal tibiofibular ligament, assess for juxta-articular ganglion formation or periarticular fluid collection, visualize and avoid local neurovascular structures, forego exposure to ionizing radiation as well as obviate the use of iodinated contrast during needle localization prior to therapeutic cocktail delivery. That being said, fluoroscopic guidance may be preferable if: ultrasound is not available, the body habitus of the patient is not amenable to PTFJ localization under ultrasound or the proceduralist is not comfortable performing an ultrasound guided therapeutic intervention of the PTFJ.
Although the patient in our case did not obtain prolonged pain relief from the fluoroscopically guided PTFJ injection, the short term symptomatic relief did support the notion that her symptoms were localized to her left PTFJ and offer justification for subsequent definitive surgical management.
Informed Consent Attestation
The patient has granted informed consent for the publication of this case report. This signed document is on file with the authors.
Footnotes
Conflicts of Interest: The authors declare that they have no conflict of interest nor financial interests to disclose.
References
- 1.McCarthy C.L., McNally E.G. The MRI appearance of cystic lesions around the knee. Skeletal Radiol. 2004;33(4):187–209. doi: 10.1007/s00256-003-0741-y. [DOI] [PubMed] [Google Scholar]
- 2.Forster B.B., Lee J.S., Kelly S., O'Dowd M., Munk P.L., Andrews G. Proximal tibiofibular joint: an often-forgotten cause of lateral knee pain. Am J Roentgenol. 2007;188(4):W359–W366. doi: 10.2214/AJR.06.0627. [DOI] [PubMed] [Google Scholar]
- 3.Pagnoux C., Lhotellier L., Marek J.J., Ballard M., Chazerain P., Ziza J.-M. Synovial cysts of the proximal tibiofibular joint: three case reports. Joint Bone Spine. 2002;69(3):331–333. doi: 10.1016/s1297-319x(02)00403-7. [DOI] [PubMed] [Google Scholar]
- 4.Berquist T. Diagnostic and therapeutic injections as an aid to musculoskeletal diagnosis. Semin Interv Radiol. 1993;10(04):326–343. [Google Scholar]
- 5.Ogden J.A. The anatomy and function of the proximal tibiofibular joint. Clin Orthop. 1974;(101):186–191. [PubMed] [Google Scholar]
- 6.Soavi R., Girolami M., Loreti I., Bragonzoni L., Monti C., Visani A. The mobility of the proximal tibio-fibular joint. A roentgen stereophotogrammetric analysis on six cadaver specimens. Foot Ankle Int. 2000;21(4):336–342. doi: 10.1177/107110070002100411. [DOI] [PubMed] [Google Scholar]
- 7.Bozkurt M., Yilmaz E., Atlihan D., Tekdemir I., Havitçioğlu H., Günal I. The proximal tibiofibular joint: an anatomic study. Clin Orthop Relat Res. 2003;5(406):136–140. doi: 10.1097/01.blo.0000030167.56585.2f. [DOI] [PubMed] [Google Scholar]
- 8.Van den Bergh F.R.A., Vanhoenacker F.M., De Smet E., Huysse W., Verstraete K.L. Peroneal nerve: Normal anatomy and pathologic findings on routine MRI of the knee. Insights Imaging. 2013;4(3):287–299. doi: 10.1007/s13244-013-0255-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim G.Y., Ryou C.H., Kim K.H., Kim D., Rhyu I.J., Kim D.H. Branching patterns and anatomical course of the common fibular nerve. Ann Rehabil Med. 2019;43(6):700–706. doi: 10.5535/arm.2019.43.6.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bozkurt M., Yılmaz E., Akseki D., Havıtcıoğlu H., Günal İ. The evaluation of the proximal tibiofibular joint for patients with lateral knee pain. Knee. 2004;11(4):307–312. doi: 10.1016/j.knee.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 11.Sekiya J.K., Kuhn J.E. Instability of the proximal tibiofibular joint. J Am Acad Orthop Surg. 2003;11(2):9. doi: 10.5435/00124635-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Smith J., Finnoff J.T., Levy B.A., Lai J.K. Sonographically guided proximal tibiofibular joint injection: technique and accuracy. J Ultrasound Med. 2010;29(5):783–789. doi: 10.7863/jum.2010.29.5.783. [DOI] [PubMed] [Google Scholar]
- 13.Diaz R., Miller J.E., Borg-Stein J., Kohler M.J. Poster 118 ultrasound-guided proximal tibiofibular joint injection in the management of proximal tibiofibular joint arthritis and instability: a case report. PM&R. 2016;8(9):S200. doi: 10.1016/j.pmrj.2016.07.161. [DOI] [PubMed] [Google Scholar]
- 14.De Smet A.A. Ultrasound-guided injections and aspirations of the extremities. Semin Roentgenol. 2004;39(1):145–154. doi: 10.1016/j.ro.2003.10.004. [DOI] [PubMed] [Google Scholar]